Teeth in the Line of Fracture: To Retain or Remove?
Abstract
:Materials and Methods
- a.
- Involving lateral and apical fibers completely
- b.
- Involving three-quarters of the lateral fibers
- c.
- Involving apical fibers completely
- d.
- Involving apical one-third of lateral fibers bilaterally
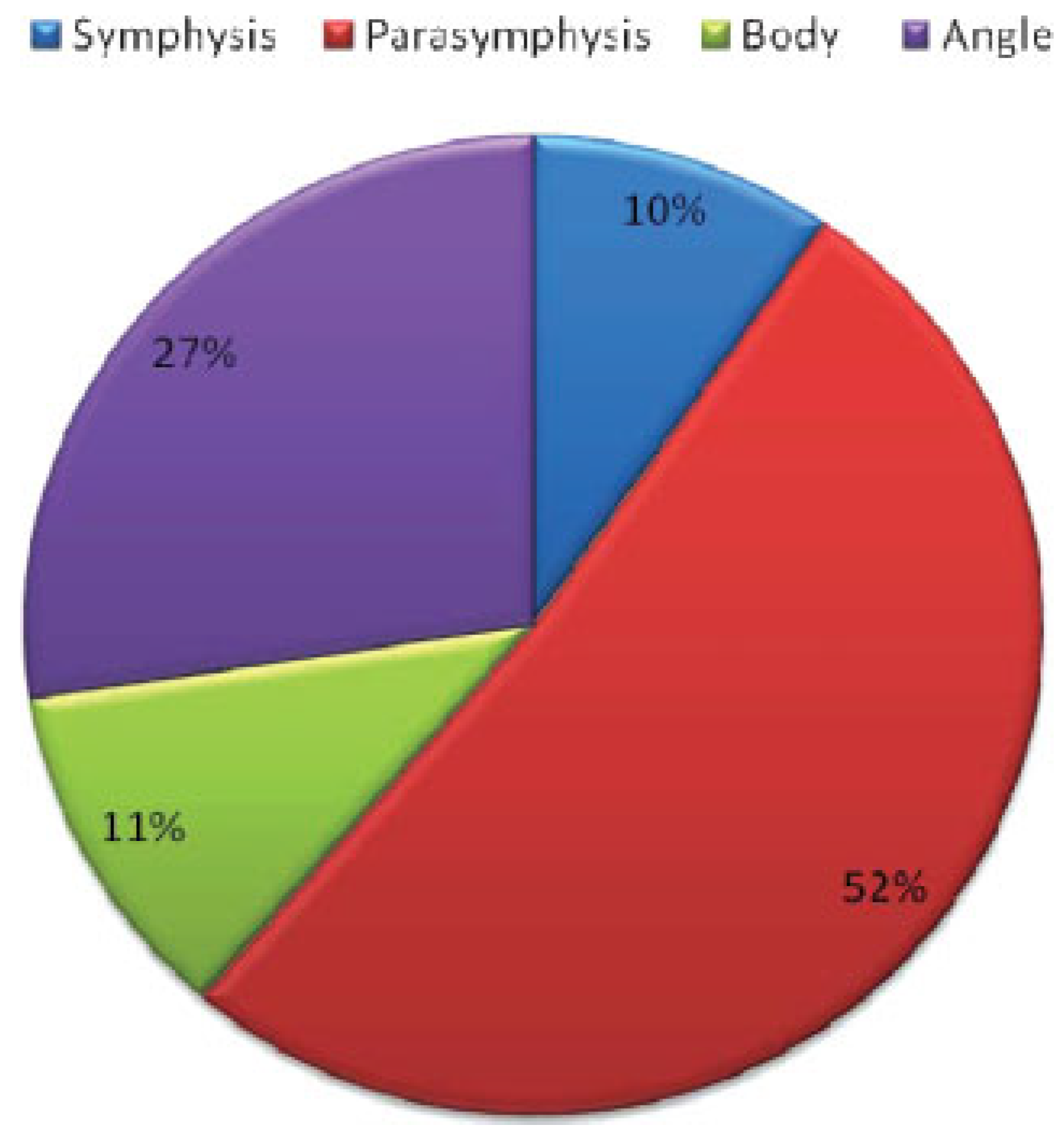
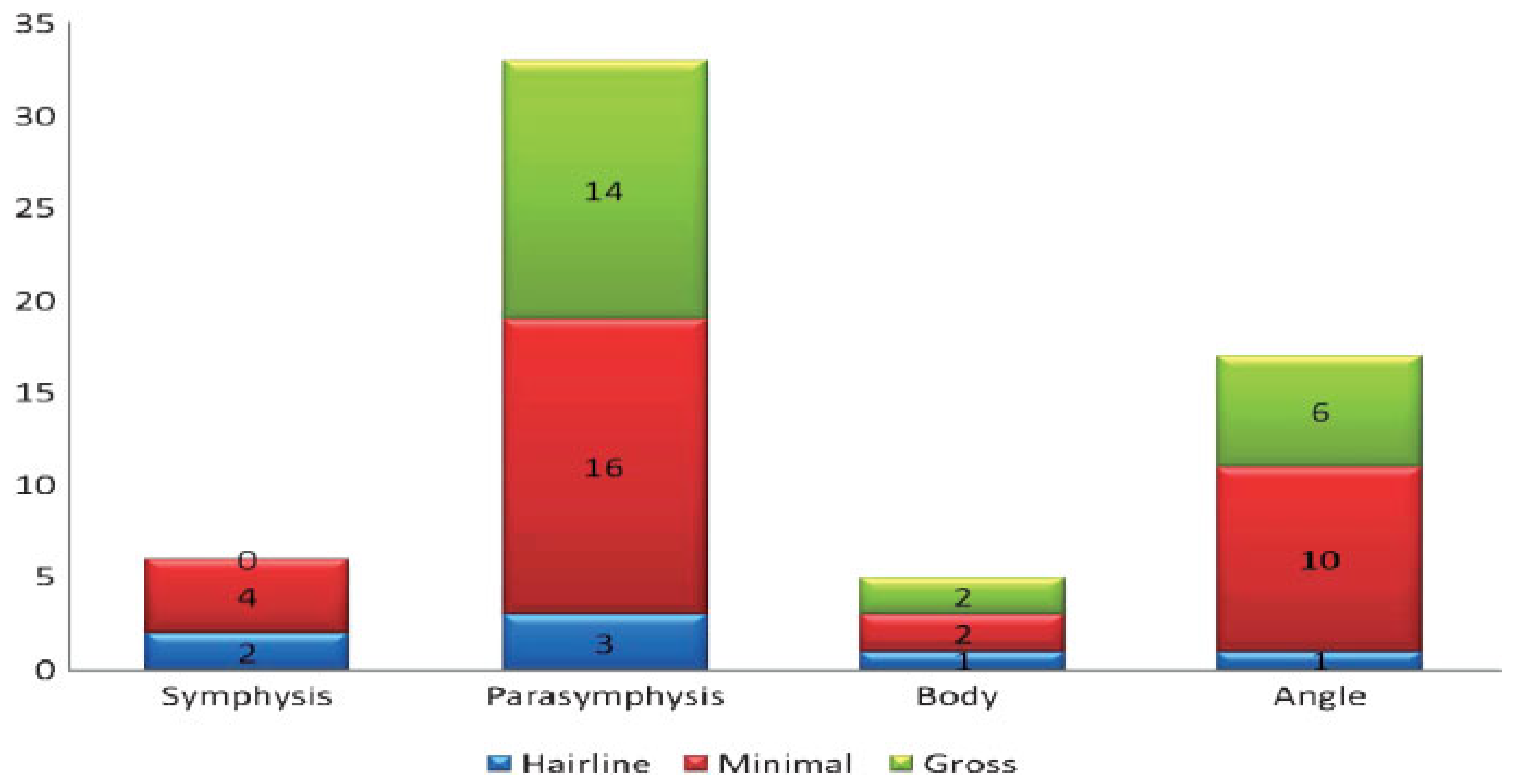
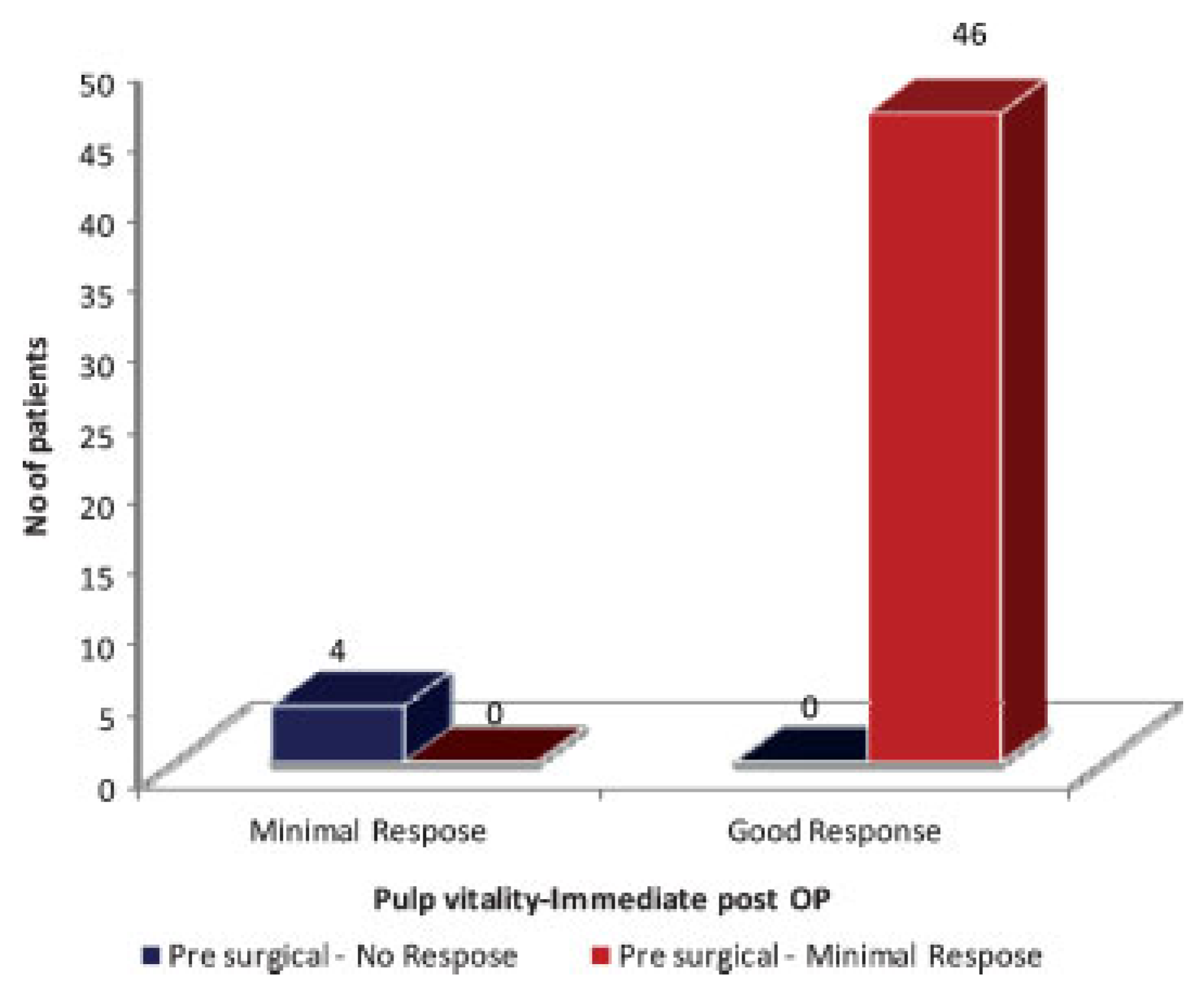
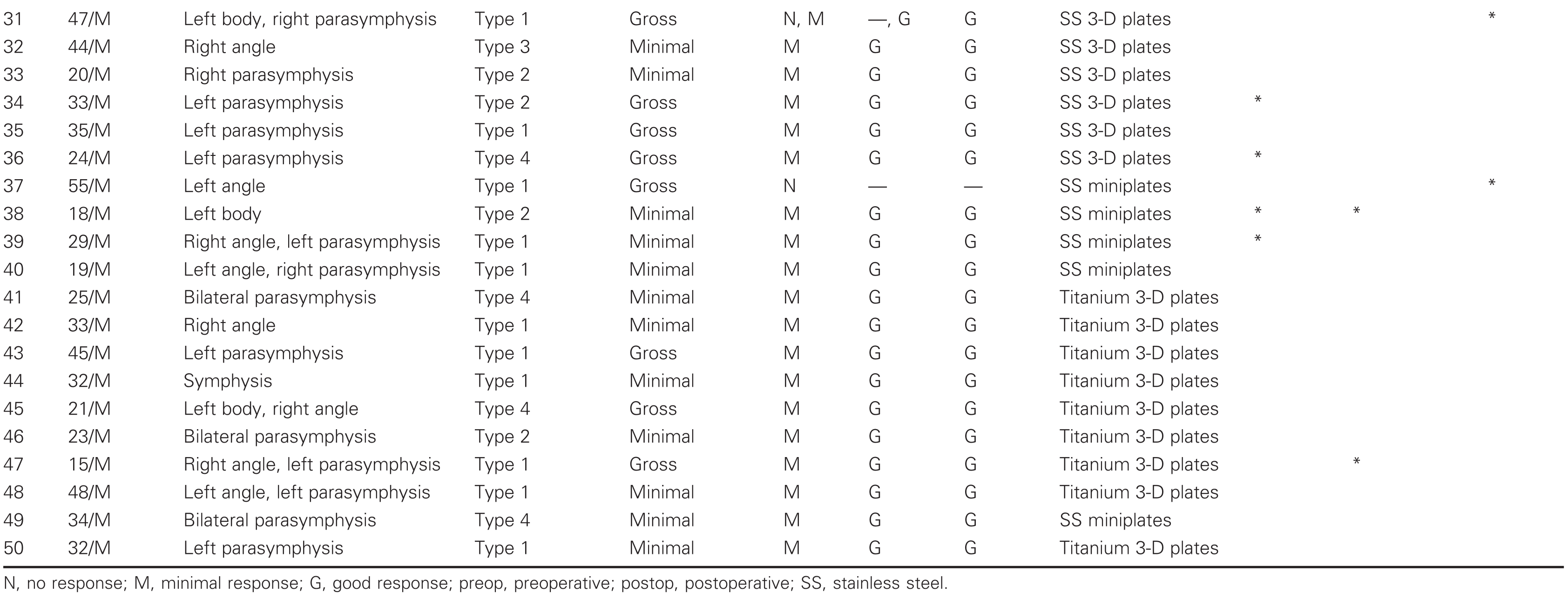
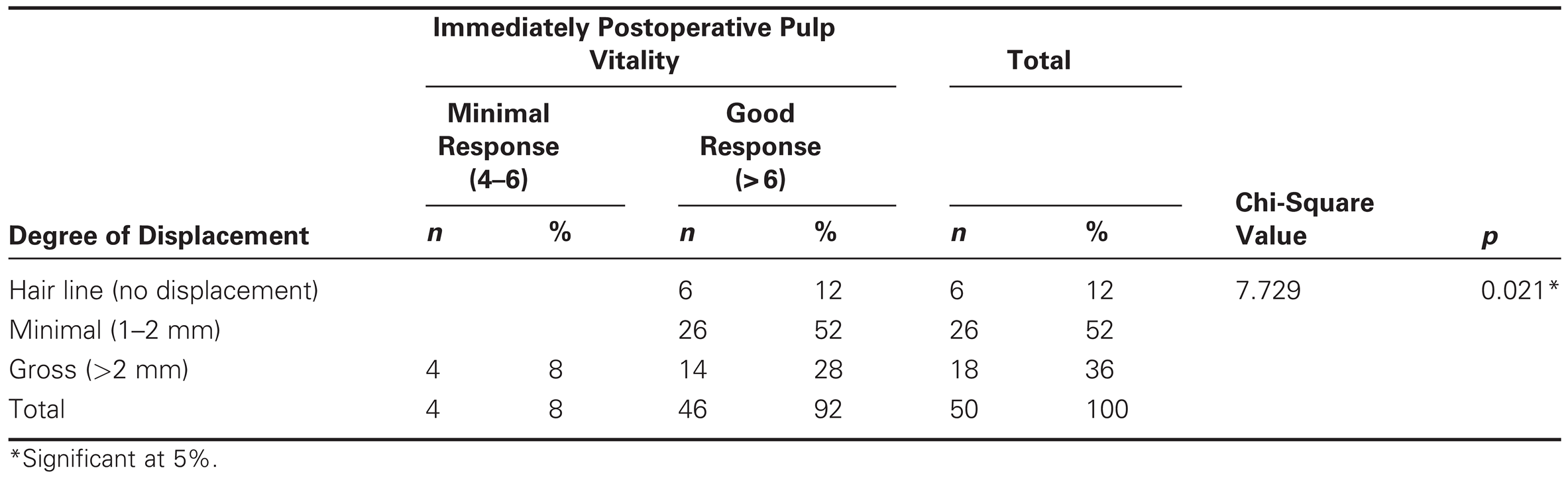
Results
Discussion
Conclusion
References
- Patrocınio, L.G.; Patrocınio, J.A.; Borba, B.H.C. , et al. Mandibular fracture: analysis of 293 patients treated in the Hospital of Clinics, Federal University of Uberlandia. Braz J Otorhinolaryngol 2005, 71, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Metin, M.; Sener, I.; Tek, M. Impacted teeth and mandibular fracture. Eur J Dent 2007, 1, 18–20. [Google Scholar] [CrossRef] [PubMed]
- Thapliyal, G.K.; Sinha, R.; Menon, P.S.; Chakranarayan, A. Management of mandibular fractures. MJAFI 2008, 64, 218–220. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E.I.I.I.; Muniz, O.; Anand, K. Treatment considerations for comminuted mandibular fractures. J Oral Maxillofac Surg 2003, 61, 861–870. [Google Scholar] [CrossRef] [PubMed]
- Abreu, M.E.R.; Viegas, V.N.; Ibrahim, D.; et al. Treatment of comminuted mandibular fractures: a critical review. Med Oral Patol Oral Cir Bucal 2009, 14, E247–E251. [Google Scholar] [PubMed]
- Smith, B.R.; Johnson, J.V. Rigid fixation of comminuted mandibular fractures. J Oral Maxillofac Surg 1993, 51, 1320–1326. [Google Scholar] [CrossRef] [PubMed]
- Kamboozia, A.H.; Punnia-Moorthy, A. The fate of teeth in mandibular fracture lines. A clinical and radiographic follow up study. Int J Oral Maxillofac Surg 1993, 22, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Cabrini Gabrielli, M.A.; Real Gabrielli, M.F.; Marcantonio, E.; Hochuli-Vieira, E. Fixation of mandibular fractures with 2.0-mm miniplates: review of 191 cases. J Oral Maxillofac Surg 2003, 61, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Ajmal, S.; Khan, M.A.; Jadoon, H.; Malik, S.A. Management protocol of mandibular fractures at Pakistan Institute of Medical Sciences, Islamabad, Pakistan. J Ayub Med Coll Abbottabad 2007, 19, 51–55. [Google Scholar] [PubMed]
- Renton, T.F.; Wiesenfeld, D. Mandibular fracture osteosynthesis: a comparison of three techniques. Br J Oral Maxillofac Surg 1996, 34, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Tams, J.; van Loon, J.P.; Rozema, F.R.; Otten, E.; Bos, R.R. A three-dimensional study of loads across the fracture for different fracture sites of the mandible. Br J Oral Maxillofac Surg 1996, 34, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Jimson, S.; Sankar, A.; Prasad, R. Comparative study of stainless steel miniplate, three-dimensional plate and titanium threedimensional plate for fixation of mandibular fractures. Int J Oral Maxillofac Surg 2009, 38, 502–503. [Google Scholar] [CrossRef]
- Shinohara, E.H.; Mitsuda, S.T.; Miyagusko, J.M.; Horikawa, F.K. Mandibular fracture reduction without intraoperative intermaxillary fixation: a technique using two modified reduction forceps. J Contemp Dent Pract 2006, 7, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Fordyce, A.M.; Lalani, Z.; Songra, A.K.; Hildreth, A.J.; Carton, A.T.; Hawkesford, J.E. Intermaxillary fixation is not usually necessary to reduce mandibular fractures. Br J Oral Maxillofac Surg 1999, 37, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Zachariades, N.; Mezitis, M.; Rallis, G. An audit of mandibular fractures treated by intermaxillary fixation, intraosseous wiring and compression plating. Br J Oral Maxillofac Surg 1996, 34, 293–297. [Google Scholar] [CrossRef] [PubMed]
- Gerbino, G.; Tarello, F.; Fasolis, M.; De Gioanni, P.P. Rigid fixation with teeth in the line of mandibular fractures. Int J Oral Maxillofac Surg 1997, 26, 182–186. [Google Scholar] [CrossRef] [PubMed]
- Fox, A.J.; Kellman, R.M. Mandibular angle fractures: twominiplate fixation and complications. Arch Facial Plast Surg 2003, 5, 464–469. [Google Scholar] [CrossRef] [PubMed]




 |
 |
 |
 |
 |
© 2010 by the author. The Author(s) 2010.
Share and Cite
Samson, J.; John, R.; Jayakumar, S. Teeth in the Line of Fracture: To Retain or Remove? Craniomaxillofac. Trauma Reconstr. 2010, 3, 177-184. https://doi.org/10.1055/s-0030-1268512
Samson J, John R, Jayakumar S. Teeth in the Line of Fracture: To Retain or Remove? Craniomaxillofacial Trauma & Reconstruction. 2010; 3(4):177-184. https://doi.org/10.1055/s-0030-1268512
Chicago/Turabian StyleSamson, Jimson, Reena John, and Shalini Jayakumar. 2010. "Teeth in the Line of Fracture: To Retain or Remove?" Craniomaxillofacial Trauma & Reconstruction 3, no. 4: 177-184. https://doi.org/10.1055/s-0030-1268512
APA StyleSamson, J., John, R., & Jayakumar, S. (2010). Teeth in the Line of Fracture: To Retain or Remove? Craniomaxillofacial Trauma & Reconstruction, 3(4), 177-184. https://doi.org/10.1055/s-0030-1268512



