Due to the prominent, midface location of the cheek, fractures of the zygomatic-maxillary complex (ZMC) represent the second most common type of facial fracture [
1,
2]. Traditionally referred to as a ‘‘tripod’’ fracture, an ZMC fracture actually involves disruption at four sites: the lateral orbital rim, the inferior orbital rim, the zygomaticomaxillary buttress, and the zygomatic arch [
3]. The majority of ZMC fractures are closed, displaced, and noncomminuted [
4]. Although the typical resultant deformity is a midface depression, with posterior positioning of the malar prominence, a range of displacements, including anterior projection of the zygoma, may occur, depending on the mechanism of trauma [
5]. In addition to malar asymmetry and other aesthetic sequelae, fractures of the ZMC may have substantial functional consequences, including concomitant orbital injury with ophthalmologic impairment, facial hypesthesia, and trismus, and are often associated with concomitant injuries to the other parts of the craniofacial skeleton or spine [
2,
6,
7].
Although it has been suggested that all displaced ZMC fractures require surgical intervention, conservative management is frequently employed in cases of minimal displacement, asymptomatic injury, patient noncompliance, or medical contraindication to surgery [
8,
9]. No standard classification scheme currently exists to assist in the assessment of ZMC fracture severity and need for surgical treatment. Although classification methods and treatment algorithms have been suggested, all are based on location of fracture lines rather than the degree and direction of displacement [
5,
10,
11,
12]. Similarly, radiographic evaluation of ZMC fractures is complicated by difficulties in translating a three-dimensional rotation and displacement into a two-dimensional imaging modality. In particular, the location of the malar eminence, which is critical to establishing facial symmetry, is challenging to pinpoint in two dimensions. The assessment of fracture severity from an aesthetic standpoint therefore remains a clinical judgment.
In the present study, we present a novel method of ZMC fracture assessment, which utilizes a threedimensional imaging modality to visualize and quantify malar eminence displacement in the anterior-posterior, medial-lateral, and superior-inferior dimensions. The pattern of displacement is then correlated with the recommended intervention, representing the clinical assessment of fracture severity, as well as the eventual outcome.
Methods
Patient Selection
A retrospective chart review was conducted of all patients treated at Stanford University School of Medicine, Department of Otolaryngology–Head and Neck Surgery from January 2002 to April 2008 with an
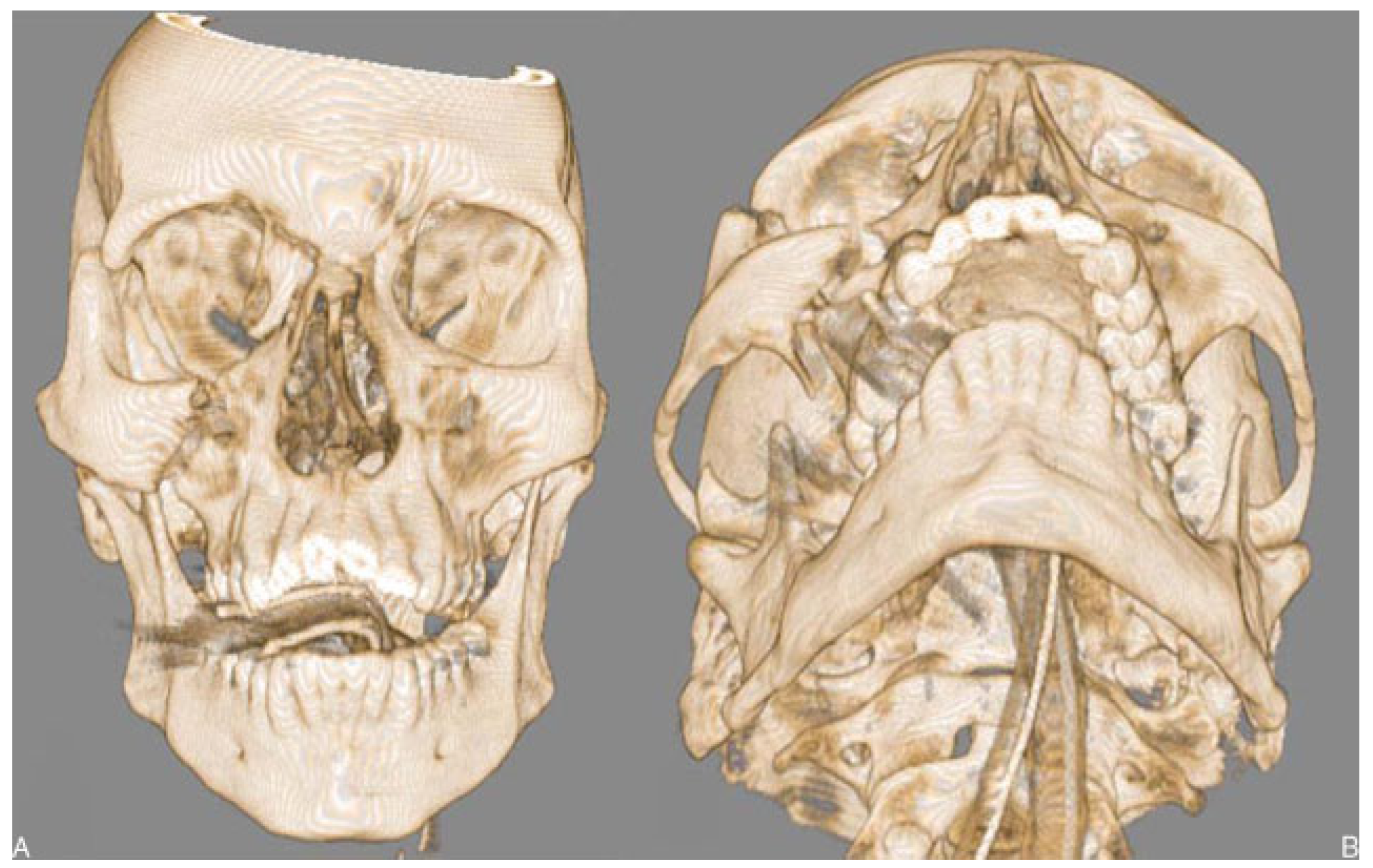
International Classification of Diseases, Ninth Revision diagnosis code corresponding to fracture of face bones (code 802). The protocols were approved by the Stanford Human Subjects Committee. Two hundred twelve patients were identified with a diagnosis of facial fracture. The radiological records of these patients were then reviewed, and 59 patients were determined to have ZMC fractures, defined as concomitant disruption of the zygomaticofrontal suture, the zygomaticomaxillary buttress, and the infraorbital rim, resulting in the complete detachment of a ‘‘tripod’’ fragment containing the malar eminence (
Figure 1). Of these, 35 patients were considered eligible for the study. Exclusion criteria were bilateral midface fractures (an isolated contralateral mandibular fracture was considered acceptable), nondisplaced fractures, and nonacute or partially healed fractures (as determined on computed tomography [CT]). An additional six patients were excluded due to lack of treatment and/or follow-up data or inability to obtain CT images. A total of 29 patients with ZMC fractures were analyzed in this study.
An age- and gender-matched cohort of 30 nonfracture patients was selected from records of patients at Stanford University School of Medicine, Department of Otolaryngology–Head and Neck Surgery who underwent a facial CT scan between the dates of July 2006 and March 2008 for a diagnosis of chronic rhinosinusitis. Radiological records and patient charts were reviewed to exclude any subjects with prior documentation of facial trauma.
Three-Dimensional Analysis
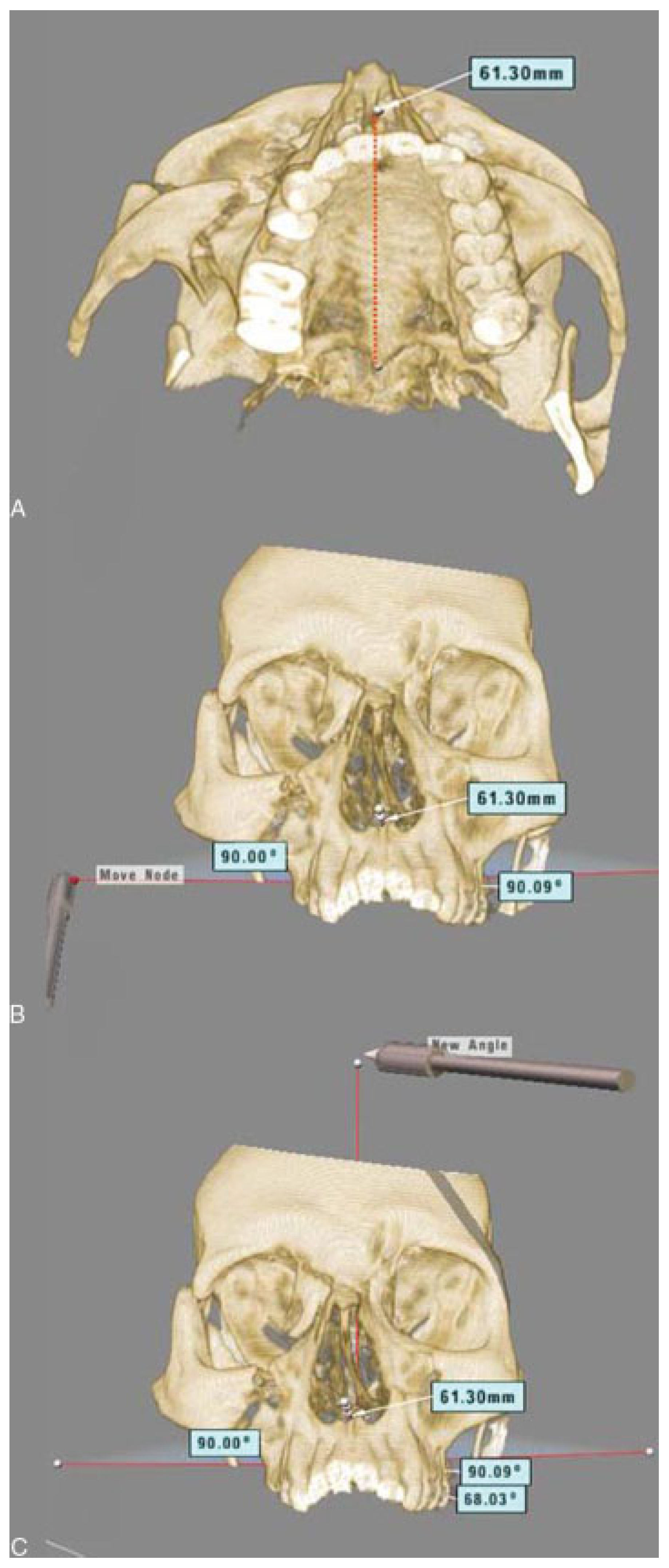
Facial CT images of fracture and nonfracture patients were imported into the Dextroscope, a virtual reality, three-dimensional image analysis modality (Volume Interactions Ltd., Singapore). Following three-dimensional reconstruction of the skull, the anteroposterior (A-P), mediolateral (M-L), and superoinferior (S-I) axes were established to facilitate a standardized measurement of malar eminence displacement. The A-P axis was first delineated along the palatine plane by creating a line from the anterior nasal spine (ANS) to the posterior nasal spine (PNS;
Figure 2A). The ANS-PNS axis has been shown to roughly approximate the Frankfurt plane within 1.0 ± 3.5 degrees [
13]. The M-L axis was next established by creating two lines perpendicular to the A-P axis, extending laterally in either direction from the PNS (
Figure 2B). Finally, the S-I axis was established by creating another line perpendicular to the A-P axis, extending superiorly from the PNS in the midline (
Figure 2C).
The malar eminences were located bilaterally as the point of intersection between a vertical arc from the zygomatic process of the frontal bone to the maxilla superior to the first molar, and a horizontal arc from the inferior orbital rim along the superior aspect of the zygomatic arch (
Figure 3) [
14]. In fracture patients, the malar eminence on the fractured side was designated by inferring the location of the intersecting arcs on the displaced zygoma.
A series of measurements was made to compare the positions of the right and left malar eminences in the nonfracture subjects and the positions of malar eminences on the fractured and nonfractured sides in the ZMC fracture patients. The measurements, performed in each of the three axes, were calculated from compressed, two-dimensional snapshot images captured with the Dextroscope and analyzed using image analysis software (Digimizer, MedCalc Software, Mariakerke, Belgium). The detailed measurement methodology is depicted in
Figure 4. All measurements were performed twice by the same investigator, with at least 48 hours separating the trials, for internal validation. In the event of nonagreement between the two trials, defined as sets of values that would result in assignment to different displacement categories (see Statistical Analysis below), a third trial was performed, with the final displacement category assigned being that obtained from two of the three trials.
Additionally, the Euclidean distance of malar eminence displacement was measured in the ZMC fracture group but not in the nonfracture subjects. This measurement is defined as the linear distance between the superimposed malar eminences after cloning and reflection of the nonfractured half of the skull on to the fractured half.
Statistical Analysis
The discrepancy between the position of the left and right malar eminences was determined in each axis (AP, M-L, and S-I) for each of the 30 nonfracture subjects. The absolute value mean of these discrepancies was calculated for each axis and used as the baseline anatomic asymmetry. A value of two standard deviations above this baseline for each axis was then set as the threshold for ‘‘mild displacement,’’ and a value of three standard deviations above the baseline for each axis was set as the threshold for ‘‘severe displacement’’ when analyzing the fracture subjects. Each fracture subject was then assigned a designation of ‘‘severe negative,’’ ‘‘mild negative,’’ ‘‘neutral,’’ ‘‘mild positive,’’ or ‘‘severe positive’’ for each axis, based upon the amount of displacement relative to the baseline. A cumulative point score was determined by assigning a value of 0 to the neutral category, a value of 1 to mild displacement (in either direction), and a value of 2 to severe displacement (in either direction), for a total score across all three axes ranging from 0 (neutral displacement in all three axes) to 6 (severe displacement in all three axes). Fisher exact test was then used to compare rates of surgical intervention (ZMC repair alone and orbital floor repair) among patients grouped by pattern of displacement, cumulative point score, and Euclidean distance of displacement. A logistic regression was also performed with surgical intervention versus no surgical intervention as the outcome measure and displacement in the A-P, M-L, and S-I directions, as well as cumulative point score and Euclidean distance of displacement as predictor variables.
Results
Demographic and epidemiological characteristics of the fracture and nonfracture subjects are presented in
Table 1. The fracture subjects ranged in age from 18 to 85 years, with a mean age of 33.4 years, and were predominantly male, with a male:female ratio of 22:7. Nonfracture subjects were age- and gender-matched to the fracture group, with ages ranging from 18 to 73 years, a mean age of 33.4 years, and a male:female ratio of 23:7. Of the fracture patients, 12 sustained left-sided ZMC fractures and 17 sustained right-sided fractures. Mechanisms of injury included fall (27.6%), blunt trauma (27.6%), motor vehicle collision (24.1%), bicycle collision (13.8%), and pedestrian-vehicle accident (6.9%). Eight patients were noted to have ophthalmologic symptoms (e.g., diplopia, gaze restriction/entrapment, proptosis, globe rupture), six were reported as having facial hypesthesia or anesthesia, and six had trismus. Eleven patients had no documentation of any ocular or neurological findings, and two patients could not be evaluated for symptoms due to mental status at the time of admission. Of the 29 fracture subjects, 19 were treated with open reduction and internal fixation (ORIF) of the ZMC fracture alone and 11 underwent concomitant orbital floor repair. There was only one orbital floor repair patient who did not require concomitant ZMC repair.
Comparison of the left and right malar eminence positions in nonfracture subjects revealed a baseline anatomic variance in symmetry of 1.10 ± 0.74 mm in the M-L direction, 1.07 ± 0.90 mm in the S-I direction, and 1.83 ± 1.55 mm in the A-P direction. Using these values, thresholds for mild and severe displacement were established for each axis (
Table 2). Each fracture patient was then assigned a displacement category for each of the three axes as well as a cumulative point score based on these categories (
Table 3).
Two of the fracture patients had neutral displacements in all three axes (cumulative score = 0), 10 patients had only mild or neutral displacements, 13 patients exhibited severe displacement in one dimension, and six patients exhibited severe displacement in two dimensions. There were no patients who exhibited severe displacement along all three axes (cumulative score = 6). Of the patients with severe displacement in at least one dimension, 78.9% underwent ZMC repair, whereas only 40.0% of patients without severe displacement in any dimension underwent ZMC repair (
p = 0.05). However, presence of severe displacement did not appear to be associated with orbital floor repair, which was performed in 30.0% of patients without severe displacement and 42.1% of patients with severe displacement in at least one dimension (
Figure 5).
Fifteen patients were severely displaced in the M-L direction, six exhibited severe S-I displacement, and four exhibited severe A-P displacement. The incidence of ZMC and concomitant orbital floor repair did not differ significantly according to direction of displacement; ZMC repair rates were 86.7%, 83.3%, and 75.0% in patients with severe M-L displacement, severe S-I displacement, and severe A-P displacement, respectively. Concomitant orbital floor repair rates were 46.7%, 50%, and 50% in patients with severe M-L displacement, severe S-I displacement, and severe A-P displacement, respectively.
Seven of the 29 fracture patients had a cumulative point score of 0 or 1, eight had a score of 2, eight had a score of 3, three had a score of 4, and three had a score of 5. When divided into scores of 2 or less versus 3 or more, 46.7% of patients with a ‘‘low’’ score of 0, 1, or 2 underwent ZMC repair, whereas 85.7% of patients with a ‘‘high’’ score of 3, 4, or 5 underwent ZMC repair (p = 0.05). A similar trend was noted for orbital floor repair, with patients scoring 0, 1, 2, or 3 having a 30.4% rate of orbital floor repair, as compared with a rate of 66.7% for patients scoring 4 or 5.
Analyses by each individual dimension are presented in
Figure 6,
Figure 7 and
Figure 8. In the M-L dimension, nine patients were neutral, two had a mild medial displacement, three had a mild lateral displacement, 11 had a severe medial displacement, and four had a severe lateral displacement. Patients with a severe displacement along the M-L axis (regardless of directionality) were found to have higher rates of ORIF than patients with neutral or mild displacements in the M-L dimension (86.7% versus 42.9%;
p = 0.02). Medial displacements also trended toward higher rates of ORIF than lateral displacements, although this did not reach statistical significance in our sample (84.6% versus 57.1%). Rates of orbital floor repair did not differ significantly among patients with neutral, mild, and severe M-L displacement (22.2%, 40.0%, and 46.7%, respectively) or among patients with medial versus lateral displacements (46.2% versus 42.9%).
In the S-I dimension, 14 patients were neutral, four had a mild superior displacement, five had a mild inferior displacement, three had a severe superior displacement, and three had a severe inferior displacement. Severity of displacement along the S-I axis was not correlated with rates of ZMC alone or orbital floor repair, although patients with severe displacement did have the highest rates of both procedures. Rates of ZMC repair in patients with neutral, mild, and severe S-I displacement (regardless of directionality) were 64.3%, 55.6%, and 83.3%, respectively. Rates of orbital floor repair in patients with neutral, mild, and severe S-I displacement (regardless of directionality) were 35.7%, 33.3%, and 50%, respectively. Inferior displacements also trended toward higher rates of ZMC and orbital floor repair than superior displacements, although not statistically significant (75.0% versus 57.1% for ZMC repair, 62.5% versus 14.3% for orbital floor repair).
In the A-P dimension, 17 patients were neutral, eight had a mild posterior displacement, and four had a severe posterior displacement. None of the patients had an anterior displacement significant enough to qualify as mild or severe. Patients with any posterior displacement (mild or severe) trended toward higher rates of both ZMC and orbital floor repair than patients who were neutral in along the A-P axis. The rate of ZMC repair in patients with mild or severe A-P displacement was 83.3%, as compared with 52.9% in patients with neutral A-P displacement. The rate of orbital floor repair in patients with mild or severe A-P displacement was 50.0%, as compared with 29.4% in patients with neutral A-P displacement.
Patients who required orbital floor repair had a greater mean Euclidean distance of displacement (5.04 ± 2.36) than patients who did not require orbital floor repair (3.36 ± 1.26; p = 0.02). However, patients who required ZMC repair did not have a significantly different Euclidean distance of displacement (4.35 ± 2.06) compared with patients who did not require ZMC repair (3.32 ± 1.44). Patients requiring ZMC repair did have significantly larger absolute cumulative displacements (calculated as the sum of the absolute values of the displacements in each of the three directions, in millimeters) than patients who did not require ZMC repair (8.28 ± 3.63 versus 5.11 ± 2.68; p = 0.02). The absolute cumulative displacement did not differ significantly between patients requiring orbital floor repair and those who did not (8.78 ± 4.86 versus 6.37 ± 3.00).
Discussion
In this study, we present a novel method of analyzing ZMC fractures based on assessment of fracture displacement in three-dimensional space. The demographic characteristics of the subjects in this study are similar to those of facial trauma patient populations that have been previously reported [
7,
15]. Our results suggest that patients with greater cumulative malar eminence displacements, higher fracture scores, and/or severe displacement in one or more dimensions were more likely to require repair. Severe displacement in the medial-lateral (x) dimension was most strongly correlated with need for surgical repair. In addition, patients with greater Euclidean malar eminence displacements were more likely to require orbital floor repair. Although it is generally understood that greater displacement will more likely require repair, this is (to the authors’ knowledge) the first study to analyze this specifically. Furthermore, analysis of the axes of displacement is a novel approach to this problem.
Although several groups have published classification schemes for categorizing facial fractures, none have quantified ZMC fracture displacement in three dimensions. The use of two-dimensional imaging in the assessment of fracture severity presents several problems. In unilateral fractures, the fractured and unfractured side cannot be compared in their entirety in one image slice, and, depending on the gantry angle and/or orientation of the patient in the CT scanner, a given image slice may be at different levels in the two sides. This poses significant challenges when attempting to quantify the amount of displacement. As a result, previously published classification schemes have been limited to qualitative categorical distinctions, which do not account for differences in the pattern or extent of displacement. For example, the algorithm proposed by Özyazgan et al. recommends no repair of the zygomatic arch for single or nondisplaced fractures, whereas all displaced plural fractures of the zygomatic arch should be treated with ORIF, regardless of amount of displacement [
11]. In our investigation, we demonstrate that mild displacements may not necessarily require surgical intervention.
Although we believe that three-dimensional assessment is superior to evaluation based on twodimensional imaging, there are limitations to the current investigation. As a retrospective study, the correlation with intervention and outcomes data presumes accurate clinical judgment of the treating surgeon. To establish a truly effective algorithm based on three-dimensional fracture displacement pattern would require a prospective, randomized controlled study, in which patients in each displacement category would be assigned to surgical intervention or nonsurgical intervention and then assessed for outcome parameters. Additionally, the current study assumes baseline facial symmetry in assessing fracture displacement. To the extent that there is slight normal anatomic variation between the positions of the malar eminence on the left versus the right, we have factored this value in when establishing thresholds for displacement. Of note, more asymmetry in the control subjects was noted in the A-P dimension than the other two dimensions. Because of this greater amount of variation, the sensitivity of A-P fracture displacement measurements may have been diminished, in that the threshold for calling a fracture displaced was increased. A larger-scale study with a greater number of control subjects is indicated to determine whether the A-P variation represents a true difference in symmetry in the general population.
The current study is a first step toward establishing a scientific, quantitative system for classifying ZMC fractures. The use of three-dimensional evaluation has many potential applications, not only for diagnosis and determination of appropriate interventional strategy, but also for peri- and intraoperative planning. Because of the complex nature of ZMC fractures, which may be comminuted, involve multiple bones, and/or complicated by soft tissue edema, surgical repair is often challenging. The use of intraoperative CT, with or without three-dimensional reconstruction, has been attempted with satisfactory results in small numbers of patients with these fractures; however, its utility has not been assessed in a prospective trial [
16,
17]. The ability to visualize fracture displacement, as well as to quantify the amount of correction necessary in each plane, would be potentially invaluable in ensuring adequate surgical repair and reducing the need for secondary intervention, which is associated with poorer outcomes. Further trials are warranted to fully evaluate the diagnostic, prognostic, and intraoperative guidance potential of three-dimensional fracture assessment.