Treatment of Pseudoaneurysm of Internal Maxillary Artery: A Case Report
Abstract
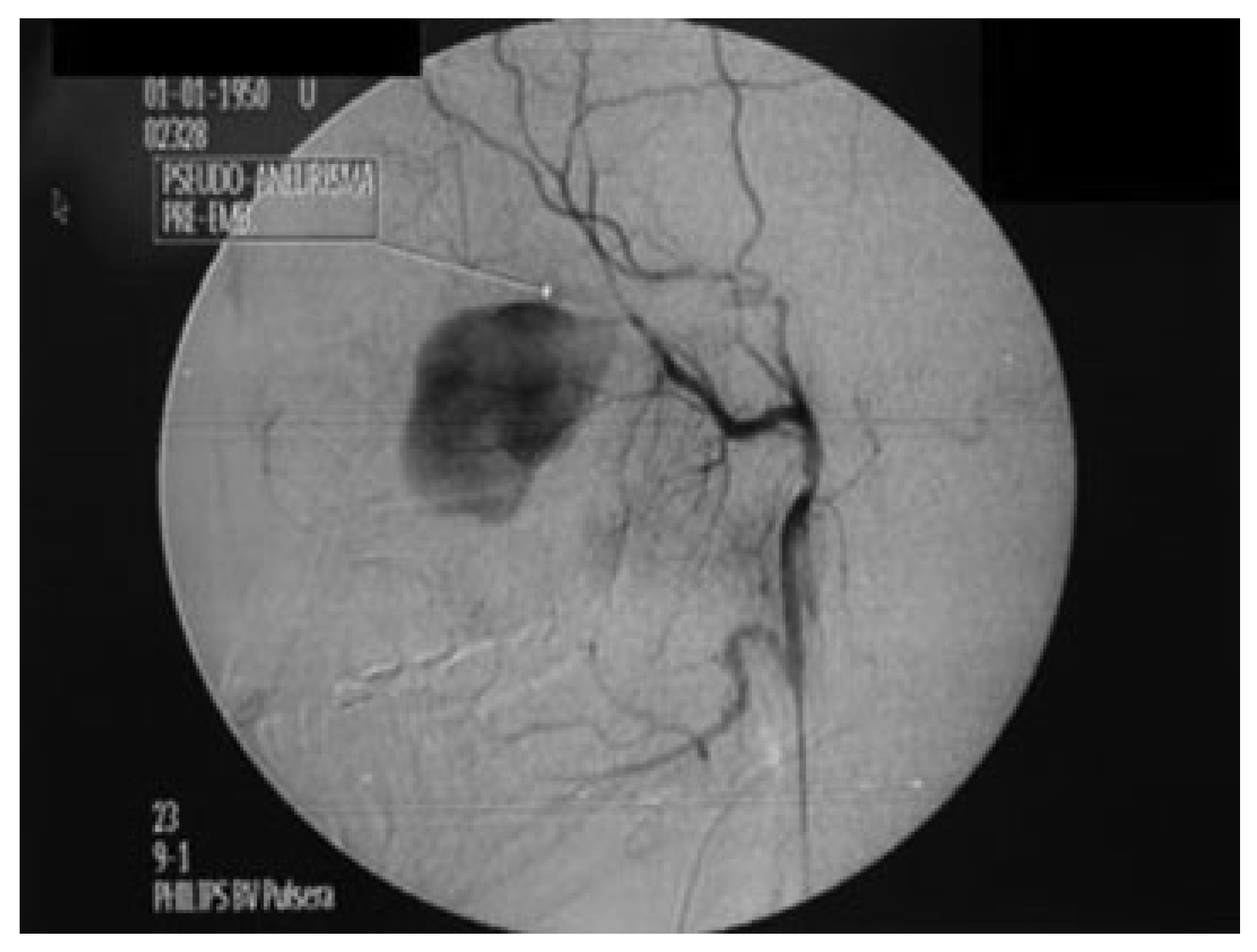
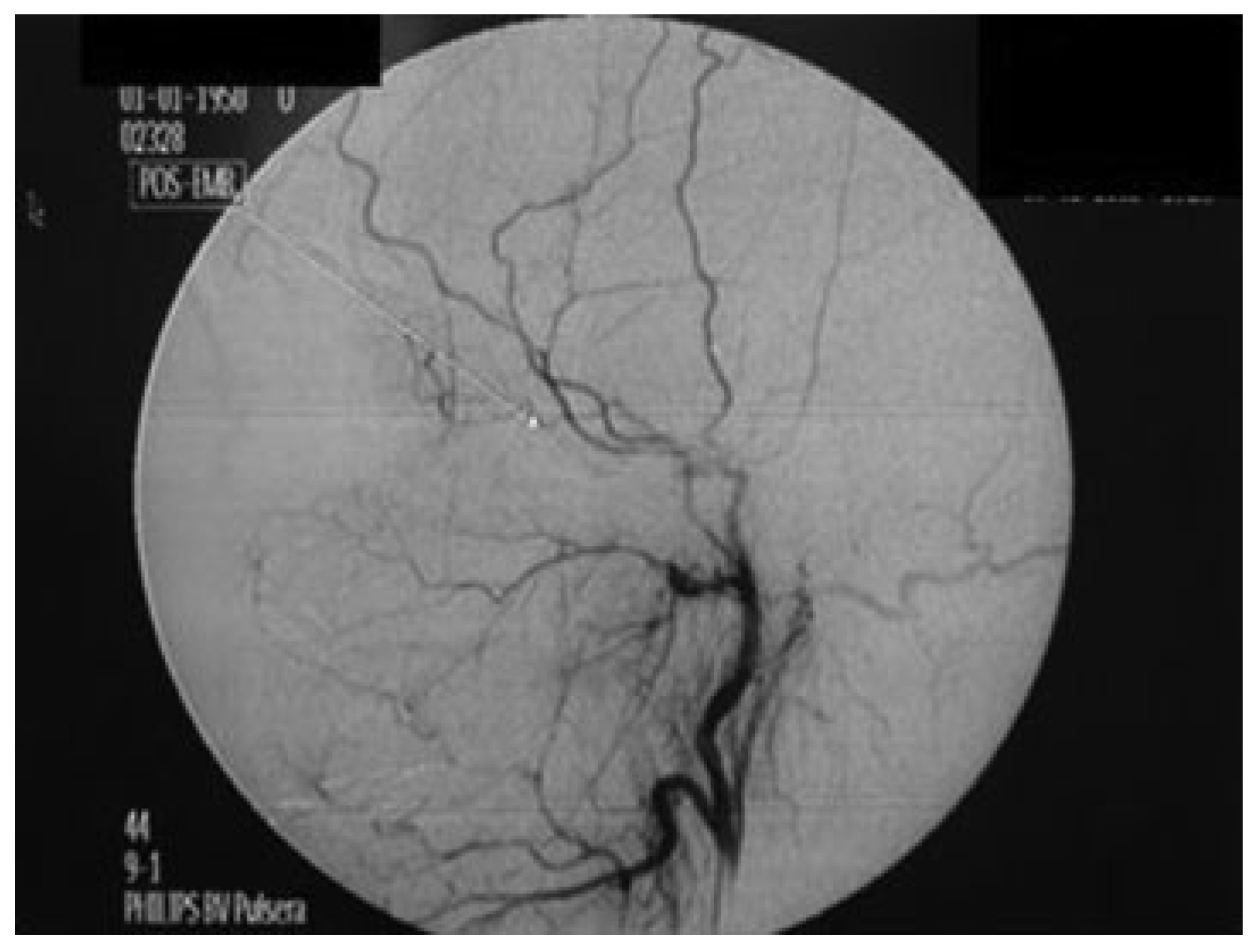
:Case Report
Discussion
Conclusions
References
- Zachariades, N.; Skoura, C.; Mezitis, M.; Marouan, S. Pseudoaneurysm after a routine transbuccal approach for bone screw placement. J Oral Maxillofac Surg 2000, 58, 671–673. [Google Scholar] [PubMed]
- Krishnan, D.G.; Marashi, A.; Malik, A. Pseudoaneurysm of internal maxillary artery secondary to gunshot wound managed by endovascular technique. J Oral Maxillofac Surg 2004, 62, 500–502. [Google Scholar] [PubMed]
- Zachariades, N.; Rallis, G.; Papademetriou, G.; Papakosta, V.; Spanomichos, G.; Souelem, M. Embolization for the treatment of pseudoaneurysm and transection of facial vessels. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001, 92, 491–494. [Google Scholar] [CrossRef] [PubMed]
- Procopio, O.; Fusetti, S.; Liessi, G.; Ferronato, G. False aneurysm of the sphenopalatine artery after a Le Fort I osteotomy: Report of 2 cases. J Oral Maxillofac Surg 2003, 61, 520–524, discussion 524–525. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.L.; Chou, A.S.B.; Wong, H.F.; Wu, S.H.; Wan, Y.L. Pseudoaneurysm of the internal maxillary artery. Available online: http://www.eurorad.org/case.php?id=1627 (accessed on 30 November 2005).
- D’Orta, J.A.; Shatney, C.H. Post-traumatic pseudoaneurysm of the internal maxillary artery. J Trauma 1982, 22, 161–164. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, H.C.; Kendrick, R.W.; Pogorel, B.S. False aneurysm of the maxillary artery. An unusual complication of closed facial trauma. Arch Otolaryngol 1983, 109, 616–618. [Google Scholar] [PubMed]
- Rogers, S.N.; Patel, M.; Beirne, J.C.; Nixon, T.E. Traumatic aneurysm of the maxillary artery: The role of interventional radiology. A report of two cases. Int J Oral Maxillofac Surg 1995, 24, 336–339. [Google Scholar] [CrossRef] [PubMed]
- De Sál, P.M.; Machado, M.C.; Da Silva, D.A.; Brito, L.L.; El Hassan, S. Delayed epistaxis secondary to intracavernous pseudoaneurysm of internal carotid artery. Rev Bras Otorrinolaringol 2003, 69, 715–718. [Google Scholar]
- Fan, X.; Mao, Q. Life-threatening oral haemorrhage of a pseudoaneurysm after raising of a fractured zygoma. Br J Oral Maxillofac Surg 2002, 40, 508–509. [Google Scholar] [CrossRef] [PubMed]
- Kish, J.W.; Katz, M.D.; Marx, M.V.; Harrell, D.S.; Hanks, S.E. N-butyl cyanoacrylate embolization for control of acute arterial hemorrhage. J Vasc Interv Radiol 2004, 15, 689–695. [Google Scholar] [CrossRef] [PubMed]
- Jordan, O.; Doelker, E.; Rüfenacht, D.A. Biomaterials used in injectable implants (liquid embolics) for percutaneous filling of vascular spaces. Cardiovasc Intervent Radiol 2005, 28, 561–569. [Google Scholar] [PubMed]
- Vinters, H.V.; Galil, K.A.; Lundie, M.J.; Kaufmann, J.C. The histotoxicity of cyanoacrylates. A selective review. Neuroradiology 1985, 27, 279–291. [Google Scholar] [PubMed]
- Hirohata, M.; Abe, T.; Morimitsu, H.; Fujimura, N.; Shigemori, M.; Norbash, A.M. Preoperative selective internal carotid artery dural branch embolisation for petroclival meningiomas. Neuroradiology 2003, 45, 656–660. [Google Scholar] [CrossRef] [PubMed]
- Nakstad, P.H.; Bakke, S.J.; Hald, J.K. Embolization of intracranial arteriovenous malformations and fistulas with polyvinyl alcohol particles and platinum fibre coils. Neuroradiology 1992, 34, 348–351. [Google Scholar] [PubMed]
- Selcuk, H.; Soylu, N.; Albayram, S.; et al. Endovascular treatment of persistent epistaxis due to pseudoaneurysm formation of the ophthalmic artery secondary to nasogastric tube. Cardiovasc Intervent Radiol 2005, 28, 242–245. [Google Scholar] [PubMed]
© 2010 by the author. The Author(s) 2010.
Share and Cite
Barbalho, J.C.M.; Santos, E.S.; Menezes, J.M.S.; Gonçalves, F.R.; Chagas, O.L. Treatment of Pseudoaneurysm of Internal Maxillary Artery: A Case Report. Craniomaxillofac. Trauma Reconstr. 2010, 3, 87-89. https://doi.org/10.1055/s-0030-1254378
Barbalho JCM, Santos ES, Menezes JMS, Gonçalves FR, Chagas OL. Treatment of Pseudoaneurysm of Internal Maxillary Artery: A Case Report. Craniomaxillofacial Trauma & Reconstruction. 2010; 3(2):87-89. https://doi.org/10.1055/s-0030-1254378
Chicago/Turabian StyleBarbalho, Jimmy Charles Melo, Eliardo Silveira Santos, José Maria Sampaio Menezes, Fabricio Rocha Gonçalves, and Otacilio Luiz Chagas. 2010. "Treatment of Pseudoaneurysm of Internal Maxillary Artery: A Case Report" Craniomaxillofacial Trauma & Reconstruction 3, no. 2: 87-89. https://doi.org/10.1055/s-0030-1254378
APA StyleBarbalho, J. C. M., Santos, E. S., Menezes, J. M. S., Gonçalves, F. R., & Chagas, O. L. (2010). Treatment of Pseudoaneurysm of Internal Maxillary Artery: A Case Report. Craniomaxillofacial Trauma & Reconstruction, 3(2), 87-89. https://doi.org/10.1055/s-0030-1254378


