Blindness is an uncommon, yet documented complication of facial trauma. Numerous case studies, series, and retrospective analyses have been published, with a reported incidence around 3%. Hippocrates first noted the association between maxillofacial trauma and
blindness; millennia later, this was expounded upon by Berlin, who discovered such trauma may directly lead to fracturing of the optic canal [
1]
. As diagnostic modalities such as computed tomographic scanning evolved, par- ticularly over the past few decades, more specific, in-depth reports analyzing maxillofacial trauma and subsequent sequelae have emerged. It is the goal of this article to examine the current literature for those publications that have addressed the issue of blindness following facial trauma (including operative interven- tions) and create a concise review for maxillofacial surgeons.
Incidence of Blindness
One of the earliest analysis of maxillofacial trauma out- comes was published in the
Journal of Trauma by Cruse et al in 1980 [
2]. In this article, the authors reported on 33 patients noted to have naso-orbito-ethmoid fractures, 10 of whom were found to suffer severe ocular injury with initial or subsequent loss of sight. Three years later, Holt et al published one of the largest such series to date, which analyzed 727 facial fractures with a blindness incidence of ~3%, laying the groundwork for today’s incidence reporting [
3].
Many groups have confirmed these numbers. Al- Qurainy et al describe 363 patients with a total of 438 midfacial fractures with loss of vision of 2.2% when analyzed per patient [
4]. Similar figures were described by Kallela et al in 1994. Here, retrospective analysis of 614 patients presenting with midfacial fractures (four as isolated zygomatic fractures and six with LeFort frac- tures) revealed 10 patients with a total of 14 blind eyes: a blindness rate of 2.3% [
5]. Higher rates of blindness sec- ondary to traumatic midfacial fractures have been pub- lished: Ashar et al noted 22% of midfacial fractures involving the orbit resulted in permanent blindness [
6]. This high incidence seems to be isolated. Even when focused attention is paid to orbital fractures, blindness rates of ~2.9% are reoprted [
7].
In more recent years, several very large retrospec- tive analyses have been completed. MacKinnon et al described in eloquent detail a retrospective review of a total of 2516 patients with facial fractures that required operative intervention. Of these patients, 19 were noted to have severe visual impairment or blindness, largely secondary to laterally directed forces of impact [
8]. Inter- estingly, MacKinnon et al demonstrated that the lateral orbital wall along with the zygomaticomaxillary buttress were the most commonly fractured areas in the patients with significant ocular sequelae. These substantiate sim- ilar reports in the literature [
9,
10]. It should be noted that MacKinnon et al’s blindness rate of 0.8% of patients sustaining facial fractures is significantly lower than previously published reports.
This reduced rate of blindness has also been documented in other very large series, including Zachariades et al in their review of 5936 facial trauma patients, in which 19 cases of blindness occurred, yielding a rate of 0.32% [
11]. The authors found vision loss was most commonly seen in Le Fort III level fractures.
A retrospective chart review undertaken by Ansari in 2005 revealed 30 cases of blindness following facial trauma and subsequent facial fractures requiring oper- ative intervention in 2503 patients [
12]. Their analysis revealed the vast majority of cases were secondary to zygoma or zygomaxillary complex fractures with retro- bulbar hemorrhage or severe damage to the eye as a whole being present in most.
Mechanism of Injury Leading to Blindness
Numerous case reports and case series have added to our understanding of this phenomenon in the setting of maxillofacial trauma. These span a range of mechanisms, clinical courses, and ultimate outcomes ranging from traumatic blindness following a displaced lateral orbital wall fracture to traumatic retrobulbar hemorrhages and malar fractures [
13,
14,
15,
16]. Other interesting yet rare compli- cations have been published in the form of transient complete blindness following nose blowing after an orbital floor fracture and orbital cellulitis secondary to fracture with subsequent subperiosteal abscess formation and permanent blindness [
17,
18,
19].
The facial skeleton is designed to withstand large force loads, with directed energy resistance in the form of elasticity, surrounding periosteum, and affect of soft tissues. Rene LeFort [
20] originally described the common fracture patterns associated with maxillofacial trauma and laid the groundwork for our understanding of facial trauma patterns. When one directs attention specifically to the globe and ocular periorbit, other factors protecting the globe include the prominence of the orbital bones themselves, as well as natural reflexes such as blinking and head aversion [
21]. Cushioning of the contents of the orbit in the form of orbital fat and the extraocular muscles also protect the ocular mecha- nism from injury secondary to blunt external forces.
Injury to the optic nerve itself is the most com- mon cause of blindness following traumatic fracture. It should be noted, however, that, secondary to a bony ring and relative laxity of the optic nerve within the optic canal, the optic nerve itself is not commonly injured during traumatic facial fracture. The transmitted force from frontal impact through the orbital wall and apex deforms the optic canal, leading to secondary ischemic necrosis from damage to the vasonervorum [
22]. In addi- tion to the mechanism of compression, shearing forces on the optic nerve itself may damage the nerve’s intimate blood supply, which is not as resilient as the nerve, resulting in ischemic neuropathy. Furthermore, the long and short posterior ciliary arteries lie unprotected in the muscle cone and may be more susceptible to injury following blunt trauma than the optic nerve itself [
12].
Ophthalmologic examination of patients with blindness or severe visual impairment secondary to ischemic neuropathy reveals a pupil that constricts with accommodation, but not to light. Notably, these pa- tients, if not suffering other ocular injuries, will have a normal fundoscopic exam.
Patients with ocular abnormalities following max- illofacial trauma most commonly present with immediate deficits; however, delayed presentations have also been described. Ansari outlined in detail those pathogeneses associated with immediate versus delayed visual loss and surmised the causes of immediate loss of vision in the posttraumatic blind patient, which include indirect optic nerve contusion, necrosis, concussion, laceration, vaso nervorum disruption, or intraneural/intrasheath hemorrhage, as well as intracerebral bleeding, vascular insufficiency, or compressive local edema [
12]. These are contrasted to those factors associated with delayed post- traumatic blindness: optic nerve edema, optic nerve necrosis, infarction, intraneural hemorrhage, visual tract injuries, optic chiasm hemorrhages, and callus formation into the optic canal/foramen.
Other than direct injury to the optic nerve itself, blindness secondary to maxillofacial fractures in the trauma patient may also be seen secondary to retrobulbar hemorrhage [
23]. These hemorrhages are commonly arte- rial in nature, often arising from the infraorbital artery or the anterior/posterior ethmoidal arteries. Brisk, high- pressure bleeding into the closed confines of the orbit results in ischemic injury, compartment syndrome, and subsequent atrophy of the optic nerve [
14].
It is also important to emphasize that iatrogenic fractures in the form of operative osteotomy are not without risk and complication. Naturally, in the con- trolled atmosphere of the operative theater, these rates are substantially lower than scar in traumatic facial fracture, but the risk exists nonetheless. Such factors were inves- tigated by Girotto et al, who documented three cases of ophthalmic complications secondary to LeFort I osteot- omies ranging from diplopia to permanent blindness [
24].
They hypothesized that the uncontrolled nature of pter- ygomaxillary disjunction may result in the extension of this fracture to the skull base or optic canal, resulting in optic nerve compromise. Their subsequent investigation utilizing a cadaveric model examining pressure trans- duction through the optic canal during maxillary down fracture revealed both increases of pressure and propaga- tion of fracture lines through the pterygoid bones. Such reports of blindness or severe visual impairment following maxillary down fracture have also previously been noted in the literature [
25,
26].
Iatrogenic causes of severe ocular impairment secondary to maxillofacial surgery are not limited to LeFort I osteotomies, as this has also been published in the literature. Pigadas and Lloyd reported such a case following Gilles repair of a displaced zygomaticomaxil- lary complex fracture in 2005 [
27].
Treatments and Outcomes
For decades, debate has surrounded the treatment mo- dality of choice for patients sustaining traumatic optic neuropathy. Although the management of traumatic optic neuropathy and posttraumatic blindness has re- mained controversial, observation, megadose corticoste- roid therapy, and surgical decompression of the optic nerve canal have all been investigated. The results of these studies are varied and often contradictory.
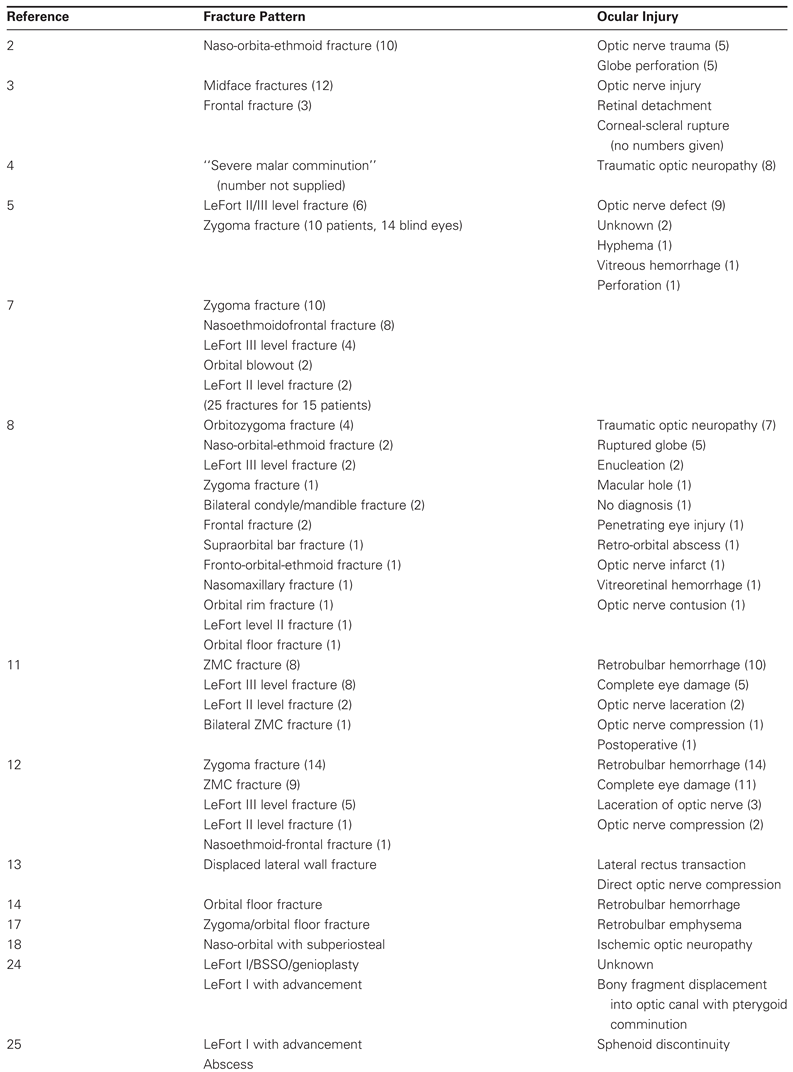
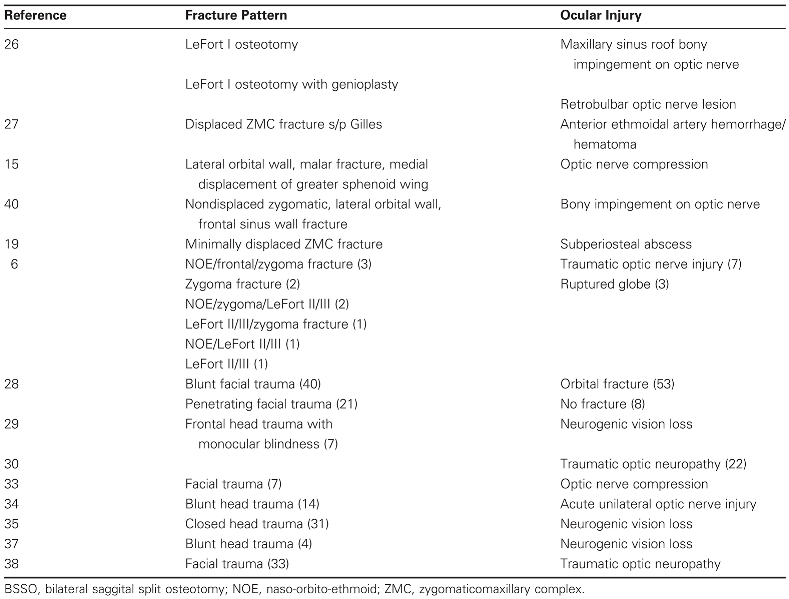
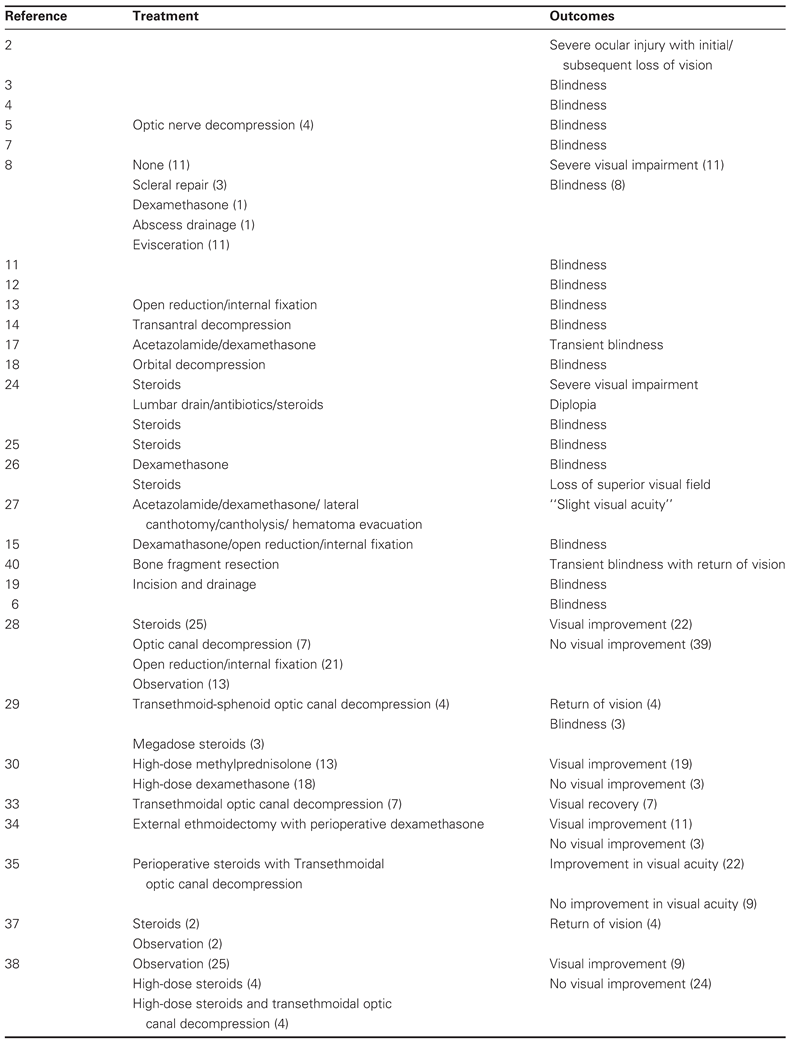
Table 2 summarizes the reported treatment modalities and out- comes.
Recently, Wang et al conducted a retrospective review of 61 consecutive patients presenting with a visual acuity deficit following facial trauma to their institution in Baltimore over a 12-year time period [
28]. These pa- tients were managed both operatively and nonopera- tively, with 41% receiving steroids alone, 11% undergoing optic nerve decompression, 34% undergoing open reduction and internal fixation of facial fractures, and observation in the remaining 21%. The authors found no significant difference in posttreatment visual acuities across the varying treatment modalities. How- ever, it was noted that patients who had suffered blunt trauma demonstrated a significantly higher rate of im- provement in visual acuity when compared with those who had received penetrating periocular trauma. Post- treatment improvement was also significantly higher in those patients who had some degree of light perception at their time of presentation versus those who had presented with total blindness. In all, 45% of patients in this series demonstrated some improvement in visual acuity following blunt facial trauma after observation or medical or surgical intervention.
Anderson et al first advocated for the use of megadose steroid therapy for treatment of blindness following facial trauma in 1982 [
29]. The authors published a case series of seven patients who presented with abrupt-onset monocular blindness following frontal head trauma. Four of these patients underwent surgical decompression of the optic canal, with only one patient achieving minor return of vision. Three of the seven patients demonstrated return of vision after receiving a course of megadose steroid therapy. The authors recom- mended that a 12-hour trial of megadose steroid treat- ment be employed prior to consideration of surgical optic nerve canal decompression.
Steroid therapy was further investigated by Spoor et al [
30]. These authors investigated 21 patients who had some visual impairment in 22 eyes following facial trauma and who were treated with megadose methyl- prednisolone (13 patients) or dexamethasone (18 pa- tients). Notably, there was a wide range of time to presentation, from 4 hours to 15 days. No significant difference in outcome was noted between these two treatment groups, with seven of nine eyes and 12 of 13 eyes demonstrating visual improvement in the dex- amethasone and methylprednisolone groups, respectively. However, those patients treated with methylprednisolone were noted to demonstrate improvement in visual acuity significantly faster than those who had received dexamethasone.
If one considers that indirect optic trauma is a focal central nervous system insult, the treatment of such may be supported by evidence for appropriate treatment modalities for other traumatic central nervous system events. In 1995, the Brain Trauma Foundation published their “Guidelines for the Management of Severe Head Injury”, which recommended against glucocorticoid ther- apy in the severely head injured patient [
31]. These recom- mendations were contradictory to those published by the National Spinal Cord Injury Study (NASCIS) group, which advocated for utilization of glucocorticoid therapy in the setting of acute spinal cord injury [
32]. However, following the NASCIS 2 and NASCIS 3 investigations, only modest benefit was noted in post hoc analyses. The findings of these two investigations have yet to be independently confirmed, thus confounding treatment recommendations for the patient sustaining acute trau- matic central nervous system injury. The most current recommendations for the management of acute cervical spine and spinal cord injuries are guided by the American Association of Neurological Surgeons, Spine Section and the Congress of Neurological Surgeons. With respect to acute spinal cord trauma, the available medical evidence does not support a significant clinical benefit from the administration of methylprednisolone in the treatment of patients for either 24 or 48 hours’ duration. The neuro- logical recovery benefit of methylprednisolone when administered within 8 hours has been suggested but not convincingly proven. However, administration of methyl- prednisolone for 24 hours has been associated with a significant increase in severe medical complications. This is even more significant when given for 48 hours. Because clinical trials failed to convincingly demonstrate a sig- nificant clinical benefit of high-dose steroids when given in the face of acute spinal cord trauma, and with the increased risks of medical complications asso- ciated with its use, high-dose methylprednisolone in the treatment of acute traumatic optic neuropathy should only be undertaken with the knowledge that the evidence suggesting harmful side effects is more consistent than the evidence suggesting clinical benefit. This cannot be overemphasized.
Other treatment modalities have been described for the management of posttraumatic optic neuropathy. The transethmoidal approach to surgically decompress- ing the optic canal was first described by Niho et al in 1961 [
33]. Prior to this publication, surgical decompression of the optic canal was undertaken via a frontal approach, which unroofed the canal but failed to excise the medial wall. Niho and colleagues’ description of the procedure noted it to be undertaken under local anesthesia, as subjective responses in terms of return of vision guide subsequent steps of the operation. Their first case series was comprised of seven patients, all of whom were reported to enjoy visual recovery. Similar outcomes have been described by Joseph et al following ipsilateral external ethmoidectomy. They noted visual improve- ment in 11 of 14 patients following blunt head trauma [
34]. However, these authors utilized perioperative dexame- thasone as part of their treatment regimen. Levin et al in 1994 performed a retrospective analysis of 31 cases of neurogenic vision loss following closed head trauma for which transethmoidal decompression of the optic canal was undertaken [
35]. Again, all patients had received a perioperative course of steroid therapy. The authors noted that 71% of these patients had improvement in visual acuity, with 19% achieving an acuity of 20/40 or better. They also found vision was significantly improved in those patients less than 40 years of age.
These case numbers, however, pale in comparison to those published by Fukado in 1975 [
36]. The author presented 400 cases of surgical decompression of the optic canal with excellent results. However, these num- bers have been called into question due to a lack of clear patient selection criteria.
Observation of such injuries has been described but is not strongly supported in the current literature. Wolin and Lavin described four cases of spontaneous return of vision after blunt head trauma that had initially caused blindness [
37]. They noted that two of these pa- tients did indeed receive steroids, but the authors stated that visual improvement had begun prior to their in- stitution. They went on to advocate for surgical decom- pression of the optic canal when visual loss initially improves with corticosteroid therapy but repeatedly deteriorates with tapered doses.
Lessell investigated 33 cases of posttraumatic optic neuropathy in which 25 patients were observed and only five of whom had improvement in visual acuity [
38]. Four patients received high-dose corticoste- roids with one patient improving; the remaining four patients received both steroid therapy and transeth- moidal decompression, and three improved. This fail- ure of observation alone was substantiated by Cook et al, who published their results of a meta-analysis of 45 articles involving 244 cases of traumatic optic neuropathy [
39]. In it, they found no significant differ- ence in visual outcomes following treatment with steroids, surgical decompression, or a combination of these two modalities. Significance was demonstrated, however, in those patients treated with any of the above-mentioned modalities who improved more than those observed.
The appropriate treatment modality for patients suffering blindness or severe optic neuropathy secondary to blunt head trauma continues to be debated. Support exists for both megadose corticosteroid therapy as well as surgical decompression of the optic canal. The relatively small number of such cases precludes a large, prospective randomized trial to aid in the elucidation of the appro- priate management plan. It must also be emphasized that the administration of high-dose steroids has been asso- ciated with a significant increase in severe medical complications. Therefore, its use in the treatment of acute traumatic optic neuropathy should only be under- taken with the knowledge that the evidence suggesting harmful side effects is more consistent than the sugges- tion of clinical benefit.
Conclusions
Blindness following facial fracture, either traumatic or iatrogenic, is a rare yet documented complication of injury or surgery in the orbital region. Although there are multiple mechanisms, the common pathway of direct or indirect optic nerve compromise is most common. It should be noted many fracture patterns may result in such a devastating complication, although high lateral loads seem to carry the highest correlation. Intraoper- atively, care should be taken during osteotomies, partic- ularly those of the LeFort I variety, to avoid uncontrolled fracturing and pressure transduction as these have been documented to lead to severe ocular complications. Management of the patient suffering blindness or severe visual impairment secondary to traumatic optic neuro- pathy is complex and disputed. Megadose corticosteroid therapy, as well as surgical decompression of the optic canal via a transethmoidal approach, is supported in the published literature, whereas observation alone is not. However, steroid use in the treatment of acute traumatic optic neuropathy should only be undertaken with the knowledge that the evidence suggesting harmful side effects is more consistent than the suggestion of clinical benefit. The debate over the proper management of these patients will likely continue until a large, prospec- tive randomized trial can be undertaken.