Extended Transcaruncular Approach Using Detachment and Repositioning of the Inferior Oblique Muscle for the Traumatic Repair of the Medial Orbital Wall
Abstract
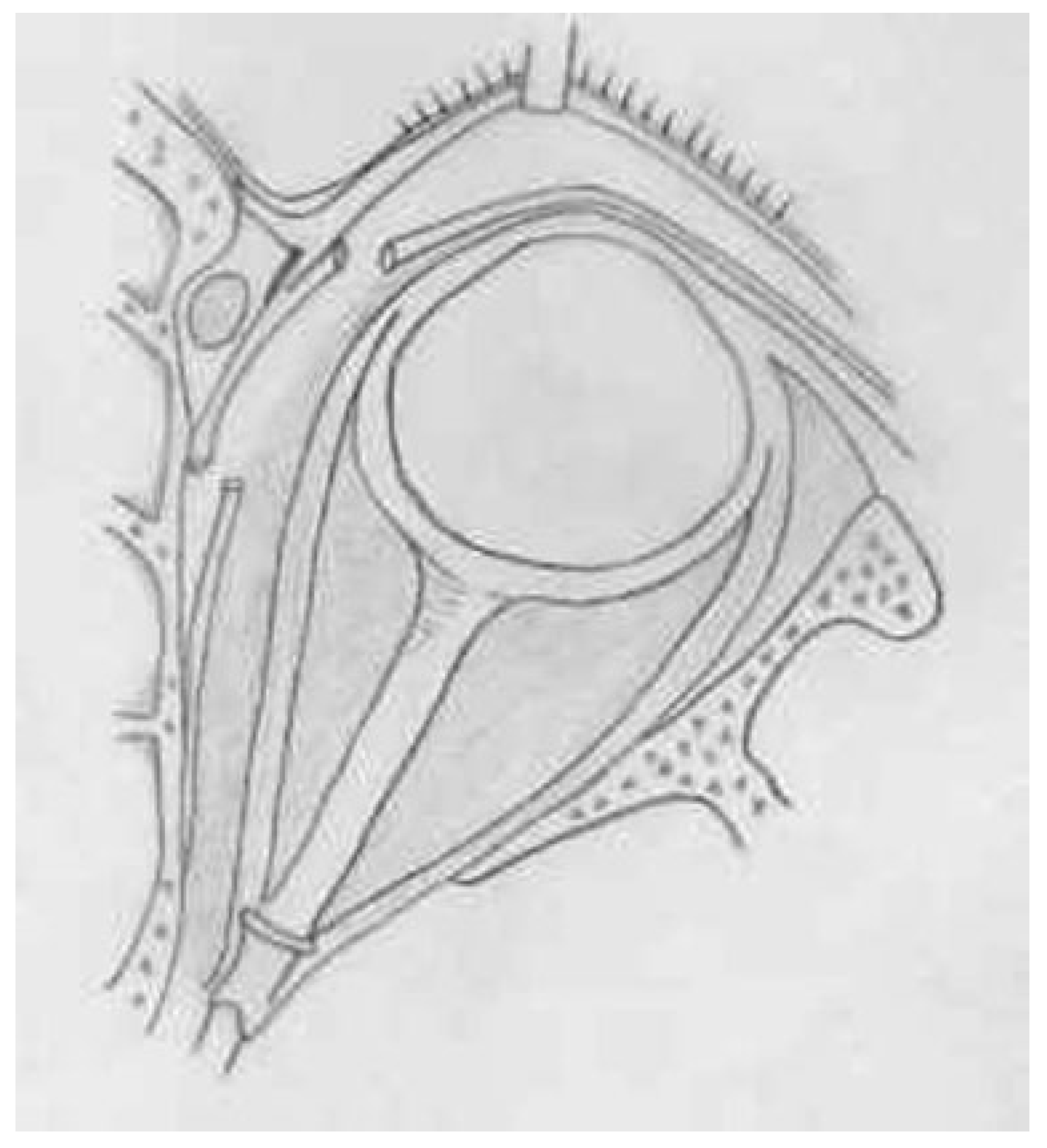
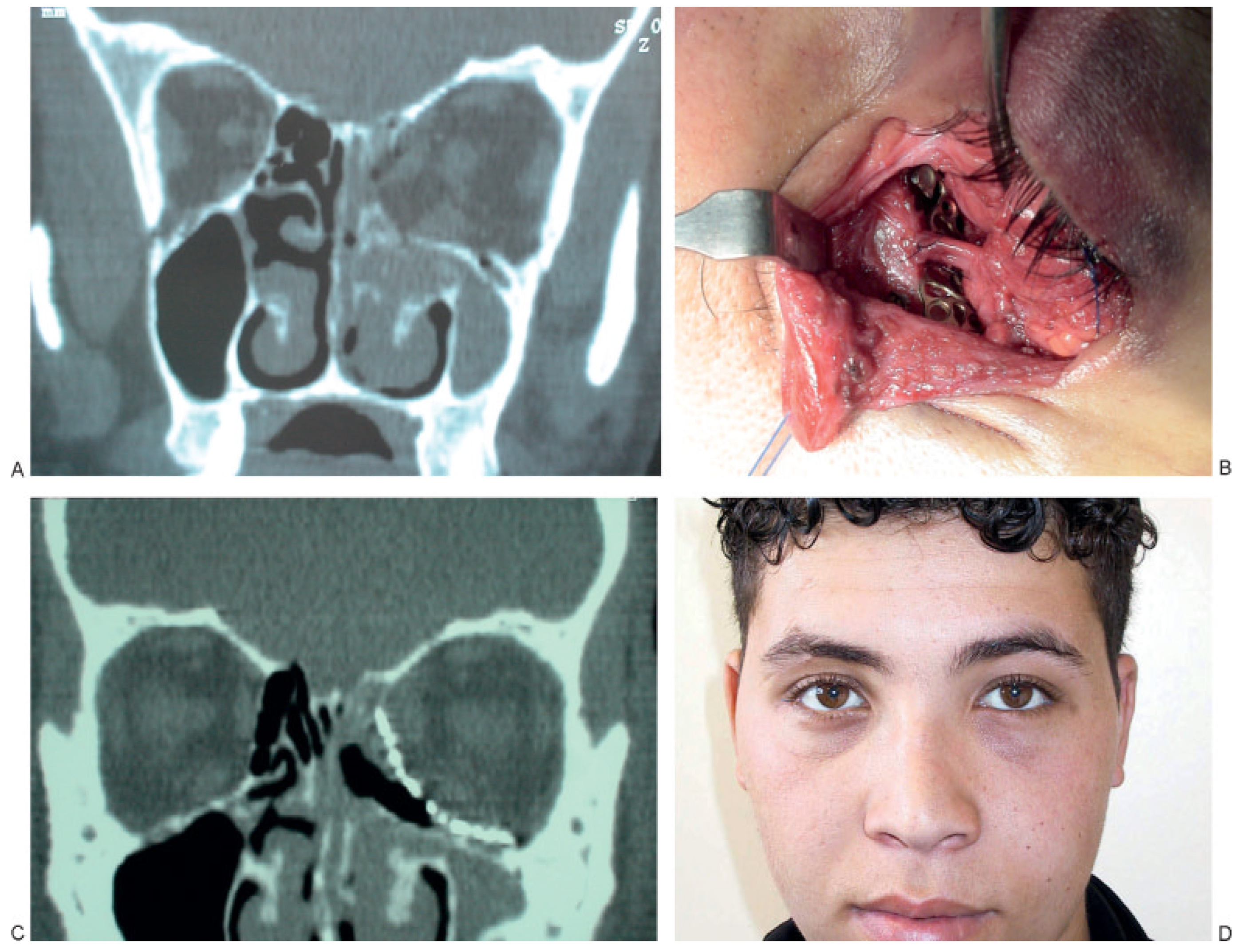
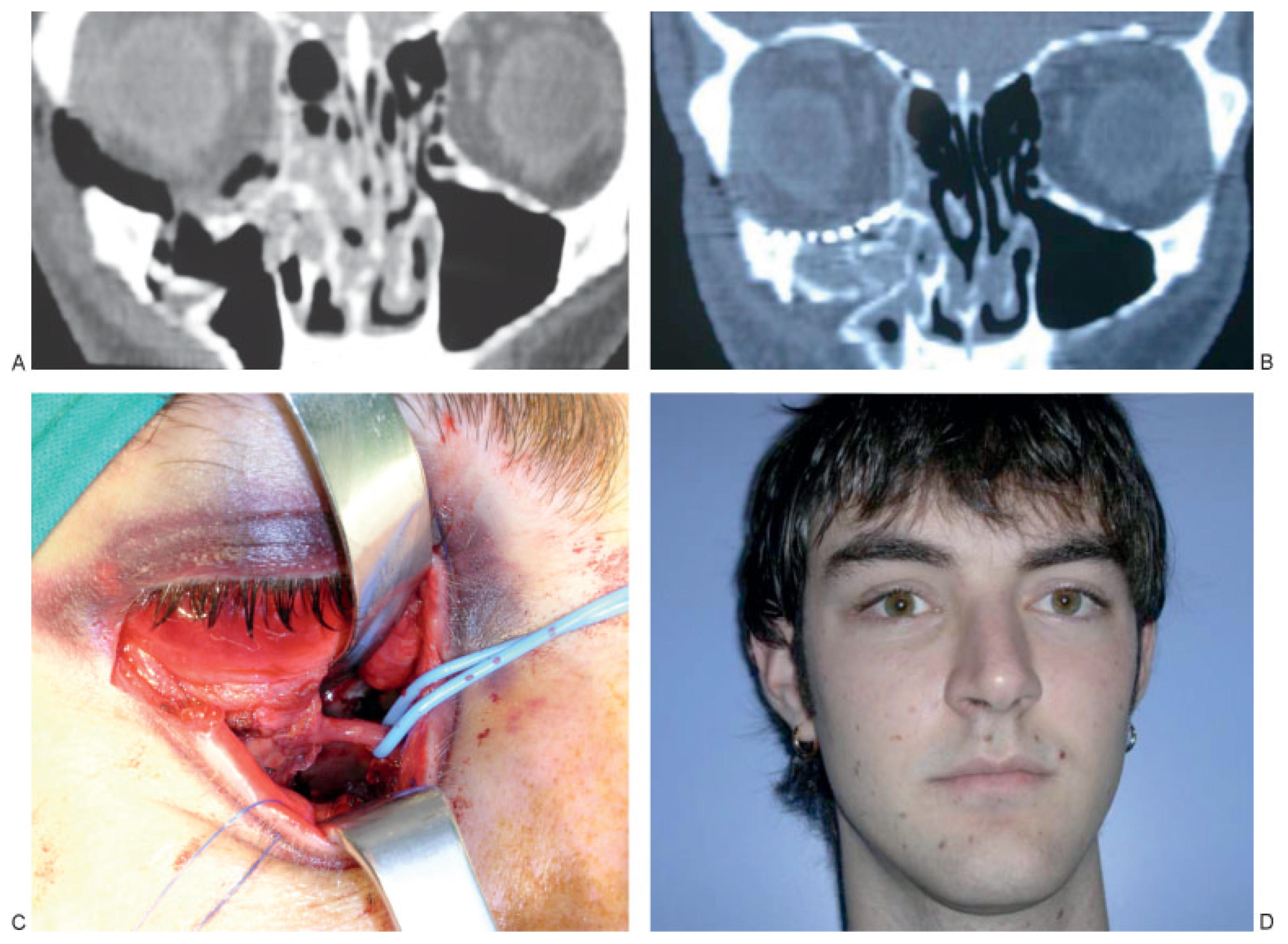
:SURGICAL TECHNIQUE
RESULTS
DISCUSSION
CONCLUSION
References
- Lynch, R.C. The technique of radical frontal sinus operation which has given me the best results. Laryngoscope 1921, 31, 1–5. [Google Scholar] [CrossRef]
- McCord, C.D. Orbital decompression for Graves’ disease exposure through lateral canthal and inferior fornix incision. Ophthalmology 1981, 88, 533–541. [Google Scholar] [CrossRef]
- Anderson, R.L.; Lindberg, J.V. Transorbital approach to decompression in Graves’ disease. Arch Ophthalmol 1981, 99, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Graham, S.M. The transcaruncular approach to the medial orbital wall. Laryngoscope 2002, 112, 986–989. [Google Scholar] [PubMed]
- Francis, I.C. Transcaruncular medial orbitotomy for stabilization of the posterior limb of the medial canthal tendon. Clin Experiment Ophthalmol 2001, 29, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Fante, R.G. Transcaruncular approach to the medial canthal tendon-application for lower eyelid laxity. Ophthal Plast Reconstr Surg 2001, 17, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Demirci, H.; Hassan, A.S.; Elner, S.G.; Boehkle, C.; Elner, V.M. Comprehensive, combined anterior and transcaruncular orbital approach to medial canthal ligament plication. Ophthal Plast Reconstr Surg 2007, 23, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S. The treatment of the lacrimal apparatus obstruction with the use of an inner canthal Jones tube insertion via a transcaruncular approach. Ophthalmic Surg Lasers 2001, 32, 48–54. [Google Scholar] [PubMed]
- Kennedy, D.W.; Goodstein, M.L.; Miller, N.R.; et al. Endoscopic transnasal orbital decompression. Arch Otolaryngol Head Neck Surg 1990, 116, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Graham, S.M.; Carter, K.D. Combined-approach orbital decompression for thyroid-related orbitopathy. Clin Otolaryngol Allied Sci 1999, 24, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Shorr, N.; Baylis, H.I.; Goldberg, R.A.; et al. Transcaruncular approach to the medial orbit and apex. Ophthalmology 2000, 107, 1459–1463. [Google Scholar] [CrossRef] [PubMed]
- Manning, S.C. Endoscopic management of medial subperiosteal orbital abcess. Arch Otolaryngol Head Neck Surg 1993, 119, 789–791. [Google Scholar] [CrossRef] [PubMed]
- de Chalain, T.M.; Cohen, S.R.; Burstein, F.D. Modification of the transconjunctival lower lid approach to the orbital floor; lateral paracanthal incision. Plast Reconstr Surg 1994, 94, 877–880. [Google Scholar] [CrossRef] [PubMed]
- Shorr, N.; Baylis, H.I.; Goldberg, R.A.; Perry, J.D. Transcaruncular approach to the medial orbit and orbital apex. Ophthalmology 2000, 107, 1459–1463. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.L.; Bernardino, C.R.; Rubin, P.A. Transcaruncular orbital decompression for management of compressive optic neuropathy in thyroid-related orbitopathy. Plast Reconstr Surg 2003, 112, 739–747. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, R.A.; Mancini, R.; Demer, J.L. The transcaruncular approach: surgical anatomy and technique. Arch Facial Plast Surg 2007, 9, 443–447. [Google Scholar] [PubMed]
- Su, G.W.; Harris, G.J. Combined inferior and medial surgical approaches and overlapping thin implants for orbital floor and medial wall fractures. Ophthal Plast Reconstr Surg 2006, 22, 420–423. [Google Scholar] [CrossRef] [PubMed]
- Warwik, R. Eugene Wolff’s Anatomy of the Eye and Orbit, 7th ed.HK Lewis: London, England, 1976. [Google Scholar]
- Ellis, E., III; Tan, Y. Assessment of internal orbit reconstructions for pure blowout fractures: cranial bone grafts versus titanium mesh. J Oral Maxillofac Surg 2003, 61, 442–453. [Google Scholar] [CrossRef] [PubMed]
- Tyers, A.G. Colour Atlas of Ophthalmic Plastic Surgery; Churchill Livingstone: Edinburgh, Scotland, 1995. [Google Scholar]
- Chen, C.T.; Huang, F.; Tsay, P.K.; et al. Endoscopically assisted transconjunctival decompression of traumatic optic neuropathy. J Craniofac Surg 2007, 18, 19–26. [Google Scholar] [CrossRef] [PubMed]
| Age | Transconjunctival | Detachment Inferior | Enophthalmos (Preoperative/ | Postoperative | Follow-Up | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Sex | (Years) | Diagnosis | Dissection | Endoscope | Oblique Muscle | Reconstruction | Postoperative) | Diplopia | (Months) |
| 1 | F | 25 | Medial wall and floor fracture | Preseptal | No | Yes | 1.5-mm plate and PDS | –1.6/0.0 | No | 23 |
| 2 | F | 21 | Medial wall and floor fracture | Retroseptal | No | No | Titanium mesh and PDS | –1.5/–0.3 | No | 36 |
| 3 | F | 23 | Medial wall and floor fracture | Preseptal | No | Yes | Titanium mesh | –0.4/–0.2 | No | 12 |
| 4 | F | 15 | Medial wall and floor fracture | Retroseptal | No | No | PDS | –1.1/–0.1 | No | 15 |
| 5 | M | 48 | Orbital apex syndrome | Retroseptal | Yes | Yes | Ethmoidectomy | Not assessed | Yes | 6 |
| 6 | F | 27 | Panfacial wall and floor fracture | Preseptal | No | Yes | Titanium mesh | –0.7/0.0 | No | 20 |
| 7 | M | 36 | Medial wall fracture | Retroseptal | No | No | Titanium mesh | –1.1/–0.2 | No | 36 |
| 8 | F | 34 | Strut fracture trapdoor | Preseptal | No | No | Resorbable mesh | –0.5/+0.5 | Yes | 13 |
| 9 | F | 25 | Strut fracture trapdoor | Retroseptal | No | No | Resorbable mesh | –0.7/0.0 | No | 30 |
| 10 | F | 33 | Medial wall and floor fracture | Retroseptal | No | Yes | Titanium mesh | –1.7/–0.2 | ? | 5 |
© 2008 by the author. The Author(s) 2008.
Share and Cite
Rodriguez, J.; Galan, R.; Forteza, G.; Mateos, M.; Mommsen, J.; Bouso, O.V.; Piera, V. Extended Transcaruncular Approach Using Detachment and Repositioning of the Inferior Oblique Muscle for the Traumatic Repair of the Medial Orbital Wall. Craniomaxillofac. Trauma Reconstr. 2009, 2, 35-40. https://doi.org/10.1055/s-0029-1202598
Rodriguez J, Galan R, Forteza G, Mateos M, Mommsen J, Bouso OV, Piera V. Extended Transcaruncular Approach Using Detachment and Repositioning of the Inferior Oblique Muscle for the Traumatic Repair of the Medial Orbital Wall. Craniomaxillofacial Trauma & Reconstruction. 2009; 2(1):35-40. https://doi.org/10.1055/s-0029-1202598
Chicago/Turabian StyleRodriguez, Javier, Ramon Galan, Gabriel Forteza, Mario Mateos, Jens Mommsen, Olga Vazquez Bouso, and Veronica Piera. 2009. "Extended Transcaruncular Approach Using Detachment and Repositioning of the Inferior Oblique Muscle for the Traumatic Repair of the Medial Orbital Wall" Craniomaxillofacial Trauma & Reconstruction 2, no. 1: 35-40. https://doi.org/10.1055/s-0029-1202598
APA StyleRodriguez, J., Galan, R., Forteza, G., Mateos, M., Mommsen, J., Bouso, O. V., & Piera, V. (2009). Extended Transcaruncular Approach Using Detachment and Repositioning of the Inferior Oblique Muscle for the Traumatic Repair of the Medial Orbital Wall. Craniomaxillofacial Trauma & Reconstruction, 2(1), 35-40. https://doi.org/10.1055/s-0029-1202598



