Complications of Frontal Sinus Fractures
Abstract
:SKULL-BASE COMPLICATIONS
INTRACRANIAL COMPLICATIONS
OPHTHALMOLOGIC
MAXILLOFACIAL
CONCLUSION
- Frontal sinus fractures represent only 5 to 12% of all maxillofacial fractures but due to the anatomic location of the sinus can have devastating sequelae. These can be skull base, intracranial, ophthalmologic or maxillofacial. They can involve brain, eye, bone, dura, muscle, or the skin–soft tissue envelope. These complications can be insidious and involve multiple organ systems.
- We must recognize that frontal sinus fractures regardless of age, gender, fracture pattern, or method of repair are going to develop complications. With this knowledge, early detection and constant vigilance is our best defense. This means lifelong follow-up to include routine imaging, endoscopy, neurologic examination, and ophthalmologic evaluation.
- Management of complications of frontal sinus fractures is often multidisciplinary. Involvement of plastic surgery, neurologic surgery, ophthalmology, otolaryngology, oral surgery, infectious disease, and critical care is often necessary for optimal outcomes.
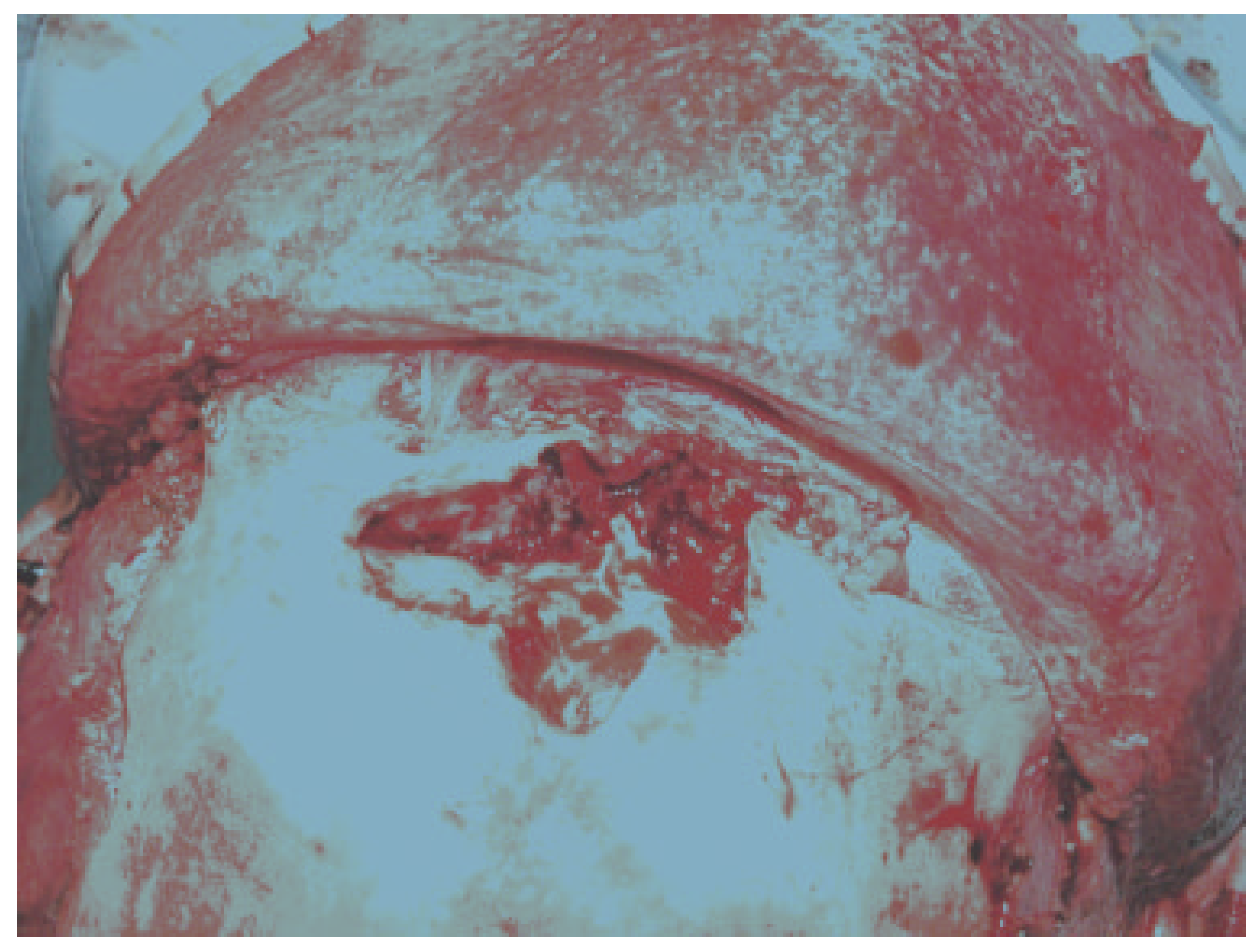
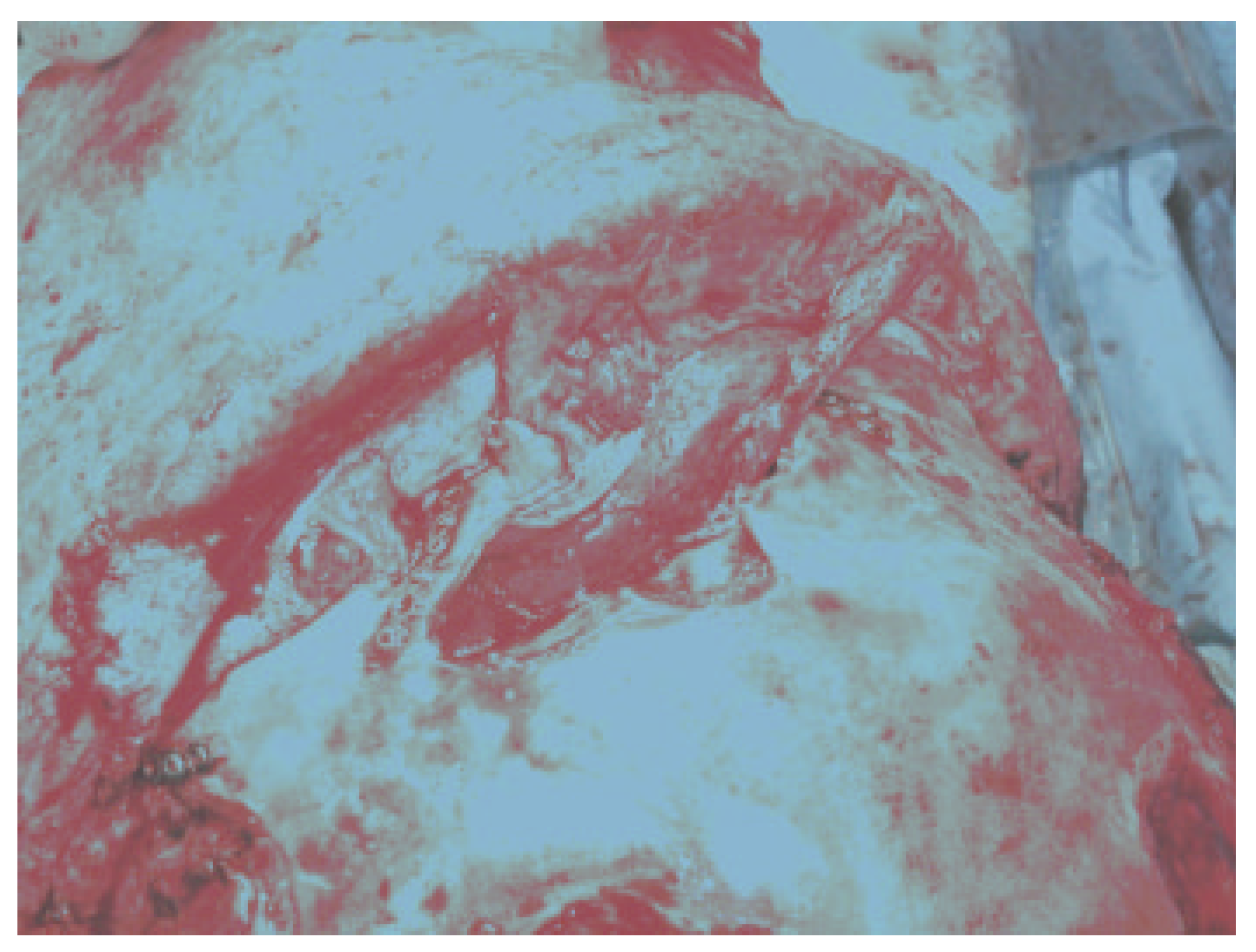
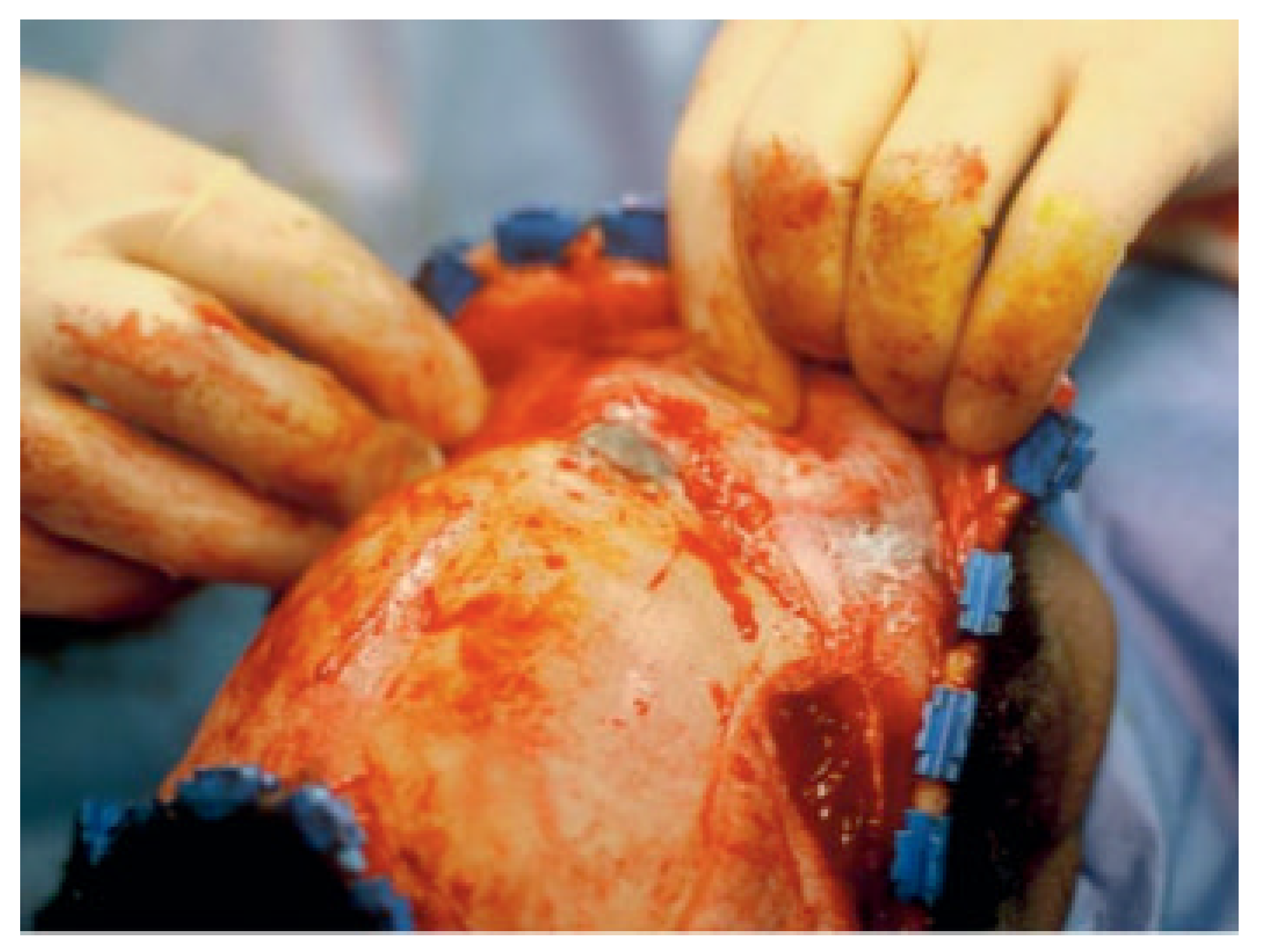
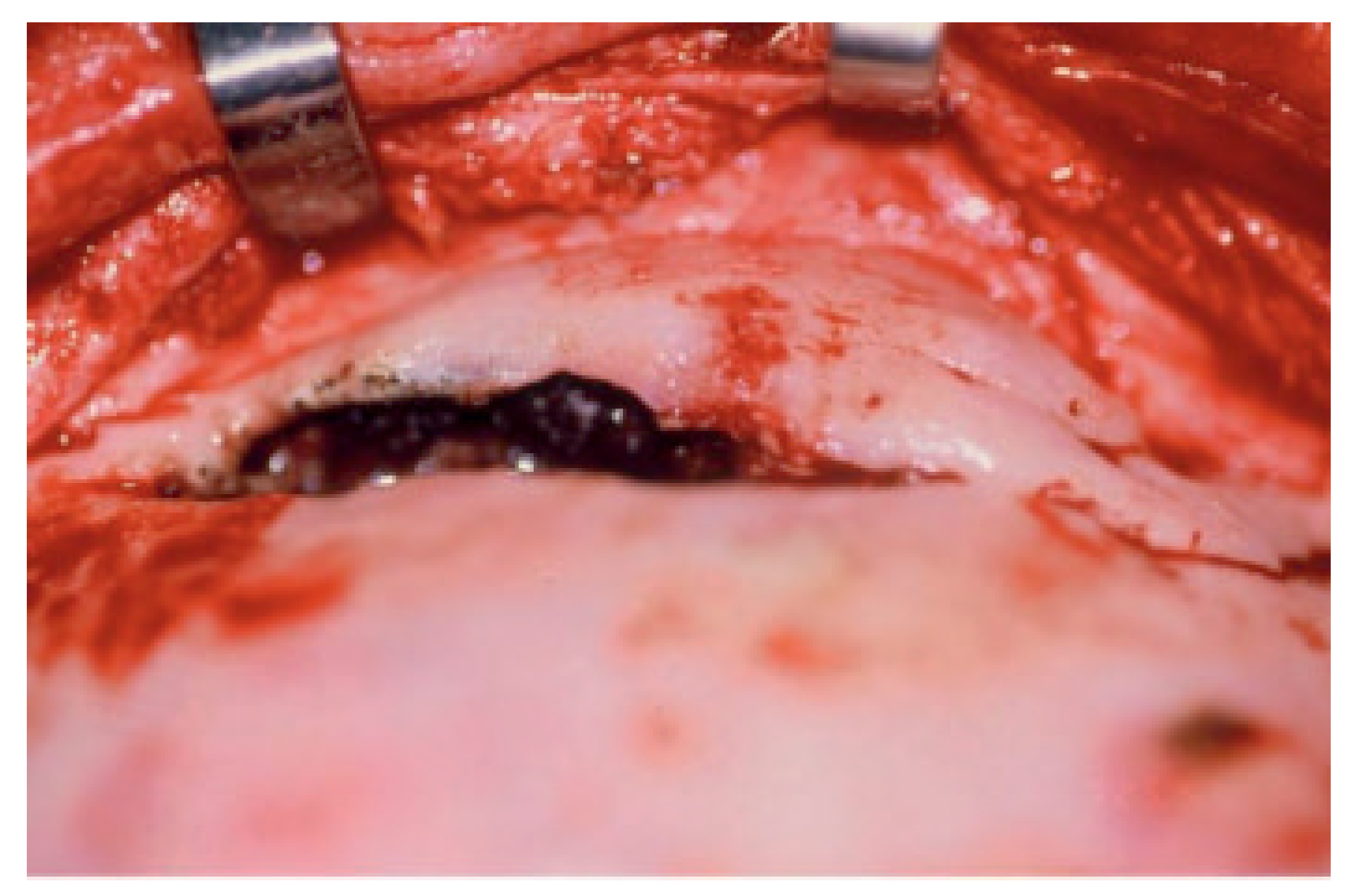
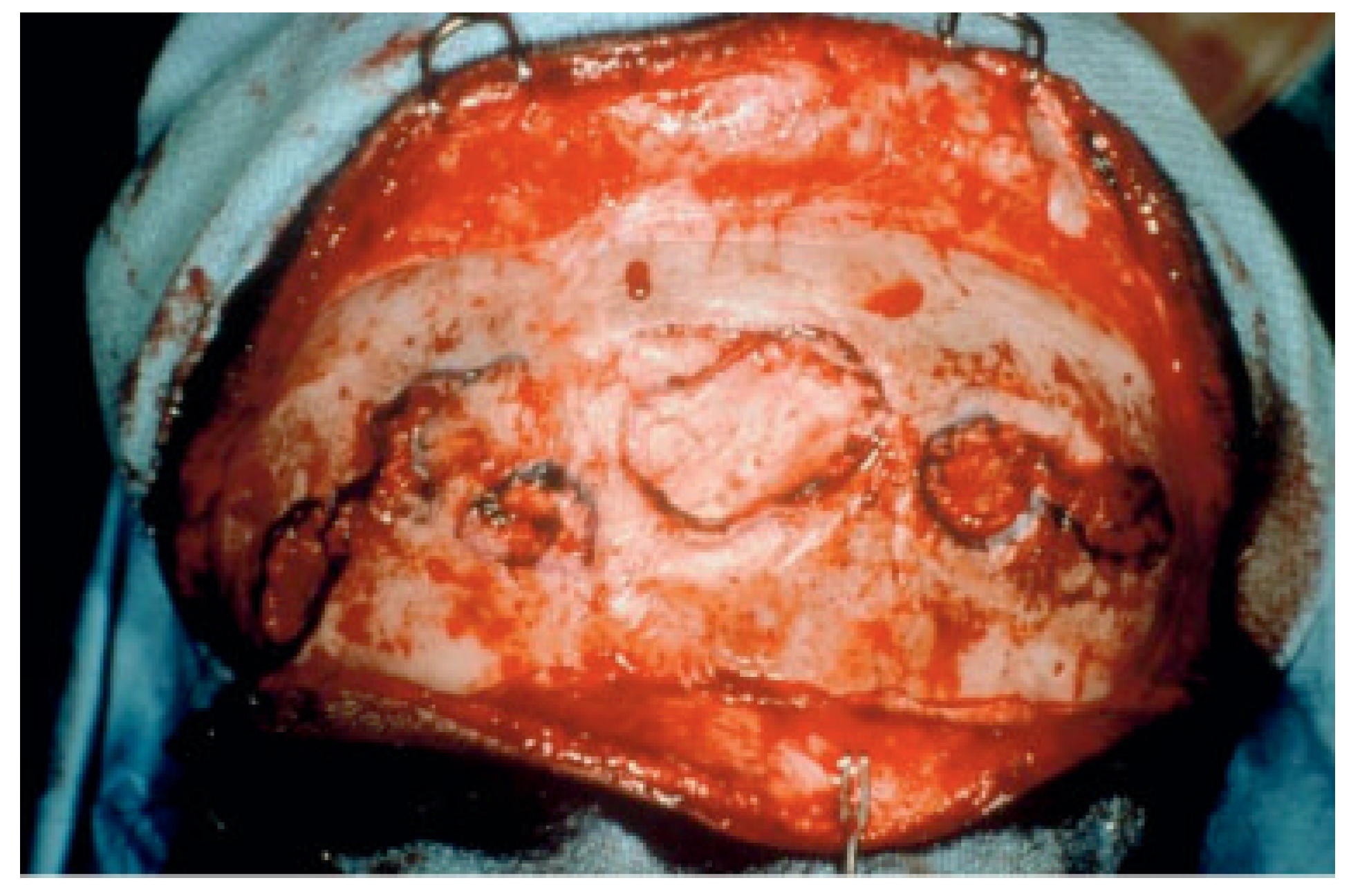
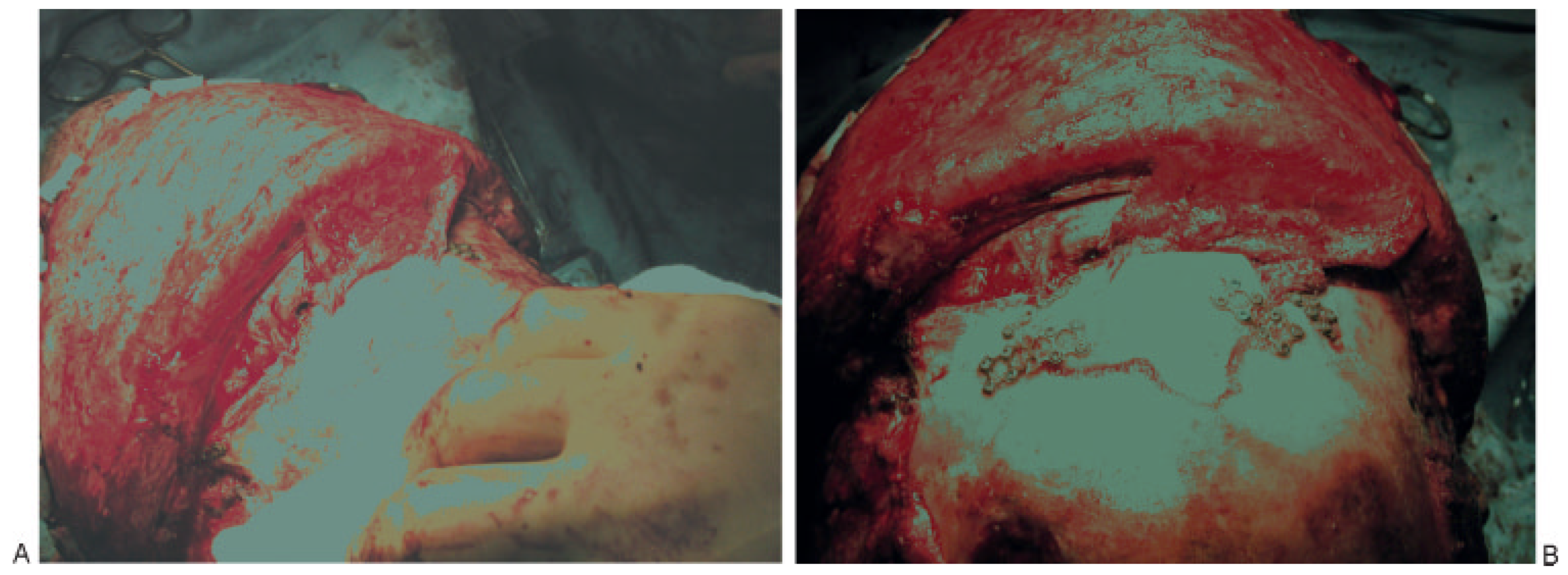
- Complications related to previous reconstruction of the frontal sinus can be extremely difficult. Principles to guide revision surgery include separation of the anterior cranial base from the nasal cavity preferably with vascularized tissue, thorough and complete mucosal removal, and use of autologous material for obliteration if necessary. If obliteration is required in an infected field, then cancellous bone is the material of choice (Figure 10A,B).
- Posterior table fractures with severe comminution, CSF leak, or nasofrontal ostia involvement should be treated with cranialization. If the posterior table is intact and the nasofrontal ostia are damaged, obliteration is the best treatment. If the anterior table is displaced and the nasofrontal ostia are intact, then reconstruction is the best option.
References
- Manolidis, S.; Hollier, L.H., Jr. Management of frontal sinus fractures. Plast Reconstr Surg 2007, 120 (Suppl 2), 32s–48s. [Google Scholar] [CrossRef] [PubMed]
- Metzinger, S.E.; Guerra, A.B.; Garcia, R.E. Frontal sinus fractures: management guidelines. Facial Plast Surg 2005, 21, 199–206. [Google Scholar]
- Xie, C.; Mehendale, N.; Barrett, D.; Bui, C.J.; Metzinger, S.E. 30-year retrospective review of frontal sinus fractures: the Charity Hospital experience. J Craniomaxillofac Trauma 2000, 6, 7–15. [Google Scholar]
- Strong, E.B.; Pahlavan, N.; Saito, D. Frontal sinus fractures: a 28-year retrospective review. Otolaryngol Head Neck Surg 2006, 135, 774–779. [Google Scholar]
- Piccolino, P.; Vetrano, S.; Mundula, P.; Di Lella, G.; Tedaldi, M.; Poladas, G. Frontal bone fractures: new technique of closed reduction. J Craniofac Surg 2007, 18, 695–698. [Google Scholar] [PubMed]
- Stanley, R.B., Jr. Fractures of the frontal sinus. Clin Plast Surg 1989, 16, 115–123. [Google Scholar]
- Stanley, R.B., Jr. Management of frontal sinus fractures. Facial Plast Surg 1988, 5, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Stanley, R.B., Jr. Management of severe frontobasilar skull fractures. Otolaryngol Clin North Am 1991, 24, 139–150. [Google Scholar]
- Manolidis, S. Frontal sinus injuries: associated injuries and surgical management of 93 patients. J Oral Maxillofac Surg 2004, 62, 882–898. [Google Scholar]
- Luce, E.A. Frontal sinus fractures: guidelines to management. Plast Reconstr Surg 1987, 80, 500–510. [Google Scholar]
- Heller, E.M.; Jacobs, J.B.; Holliday, R.A. Evaluation of the frontonasal duct in frontal sinus fractures. Head Neck 1989, 11, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Schick, B.; Draf, W.; Kahle, G.; Weber, R.; Wallenfang, T. Occult malformations of the skull base. Arch Otolaryngol Head Neck Surg 1997, 123, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Disa, J.J.; Robertson, B.C.; Metzinger, S.E.; Manson, P.N. Transverse glabellar flap for obliteration/isolation of the nasofrontal duct from the anterior cranial base. Ann Plast Surg 1996, 36, 453–457. [Google Scholar] [CrossRef]
- Thaller, S.R.; Donald, P. The use of pericranial flaps in frontal sinus fractures. Ann Plast Surg 1994, 32, 284–287. [Google Scholar] [CrossRef]
- Bourguet, J.; Bourdiniere, J.; Subileau, C.; Le Clech, G. [Otorhinolaryngology and ethmoido-frontal injuries]. J Fr Otorhinolaryngol Audiophonol Chir Maxillofac 1977, 26, 95–105. [Google Scholar]
- Le Clech, G.; Bourdinie`re, J.; Rivron, A.; Demoulin, P.Y.; Inigues, J.P.; Marechal, V. [Post-traumatic infections of the frontal sinus.]. Rev Laryngol Otol Rhinol (Bord) 1990, 111, 103–105. [Google Scholar] [PubMed]
- Klotch, D.W. Frontal sinus fractures: anterior skull base. Facial Plast Surg 2000, 16, 127–134. [Google Scholar] [CrossRef]
- Wallis, A.; Donald, P.J. Frontal sinus fractures: a review of 72 cases. Laryngoscope 1988, 98 Pt 1 Pt 1, 593–598. [Google Scholar] [CrossRef]
- Donald, P.J. The tenacity of the frontal sinus mucosa. Otolaryngol Head Neck Surg 1979, 87, 557–566. [Google Scholar] [CrossRef]
- Fain, J.; Chabannes, J.; Peri, G.; Jourde, J. [Frontobasal injuries and CSF fistulas: attempt at an anatomoclinical classification. Therapeutic incidence. ]. Neurochirurgie 1975, 21, 493–506. [Google Scholar]
- Rohrich, R.J.; Hollier, L.H. Management of frontal sinus fractures: changing concepts. Clin Plast Surg 1992, 19, 219–232. [Google Scholar] [CrossRef] [PubMed]
- Donald, P.J.; Bernstein, L. Compound frontal sinus injuries with intracranial penetration. Laryngoscope 1978, 88 Pt 1, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Rice, D.H. Management of frontal sinus fractures. Curr Opin Otolaryngol Head Neck Surg 2004, 12, 46–48. [Google Scholar] [PubMed]
- Rice, D.H. Cerebrospinal fluid rhinorrhea: diagnosis and treatment. Curr Opin Otolaryngol Head Neck Surg 2003, 11, 19–22. [Google Scholar]
- Piek, J. Surgical treatment of complex traumatic frontobasal lesions: personal experience in 74 patients. Neurosurg Focus 2000, 9, e2. [Google Scholar]
- Rice, D.H. The microbiology of paranasal sinus infections: diagnosis and management. CRC Crit Rev Clin Lab Sci 1978, 9, 105–121. [Google Scholar]
- Maniglia, A.J.; Goodwin, W.J.; Arnold, J.E.; Ganz, E. Intracranial abscesses secondary to nasal, sinus, and orbital infections in adults and children. Arch Otolaryngol Head Neck Surg 1989, 115, 1424–1429. [Google Scholar] [CrossRef]
- Hargrove, R.N.; Wesley, R.E.; Klippenstein, K.A.; Fleming, J.C.; Haik, B.G. Indications for orbital exenteration in mucormycosis. Ophthal Plast Reconstr Surg 2006, 22, 286–291. [Google Scholar]
- Whatley, W.S.; Allison, D.W.; Chandra, R.K.; Thompson, J.W.; Boop, F.A. Frontal sinus fractures in children. Laryngoscope 2005, 115, 1741–1745. [Google Scholar]
- Wright, D.L.; Hoffman, H.T.; Hoyt, D.B. Frontal sinus fractures in the pediatric population. Laryngoscope 1992, 102, 1215–1219. [Google Scholar]
- Day, T.A.; Meehan, R.; Stucker, F.J.; Nanda, A. Management of frontal sinus fractures with posterior table involvement: a retrospective study. J Craniomaxillofac Trauma 1998, 4, 6–9. [Google Scholar] [PubMed]
- Gerbino, G.; Roccia, F.; Benech, A.; Caldarelli, C. Analysis of 158 frontal sinus fractures: current surgical management and complications. J Craniomaxillofac Surg 2000, 28, 133–139. [Google Scholar] [PubMed]
- Vrankovic´, D.; Glavina, K. Classification of frontal fossa fractures associated with cerebrospinal fluid rhinorrhea, pneumocephalus or meningitis: indications and time for surgical treatment. Neurochirurgia (Stuttg) 1993, 36, 44–50. [Google Scholar]
- El Khatib, K.; Danino, A.; Malka, G. The frontal sinus: a culprit or a victim? A review of 40 cases. J Craniomaxillofac Surg 2004, 32, 314–317. [Google Scholar] [CrossRef]
- Lewine, J.D.; Davis, J.T.; Bigler, E.D.; et al. Objective documentation of traumatic brain injury subsequent to mild head trauma: multimodal brain imaging with MEG, SPECT, and MRI. J Head Trauma Rehabil 2007, 22, 141–155. [Google Scholar] [CrossRef]
- Tokisato, K.; Inatomi, Y.; Yonehara, T.; Fujioka, S.; Uchino, M. [A case with bacterial meningitis caused by cerebrospinal fluid rhinorrhea 22 years after head trauma.]. Rinsho Shinkeigaku 2001, 41, 435–437. [Google Scholar] [PubMed]
- Aletsee, C.; Konopik, V.; Dazert, S.; Dieler, R. [Surgery of anterior skull base fractures.]. Laryngorhinootologie 2003, 82, 626–631. [Google Scholar]
- Martello, J.Y.; Vasconez, H.C. Supraorbital roof fractures: a formidable entity with which to contend. Ann Plast Surg 1997, 38, 223–227. [Google Scholar]
- Haug, R.H.; Van Sickels, J.E.; Jenkins, W.S. Demographics and treatment options for orbital roof fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002, 93, 238–246. [Google Scholar]
- Holt, G.R.; Holt, J.E. Incidence of eye injuries in facial fractures: an analysis of 727 cases. Otolaryngol Head Neck Surg 1983, 91, 276–279. [Google Scholar] [CrossRef]
- Manfredi, S.J.; Raji, M.R.; Sprinkle, P.M.; Weinstein, G.W.; Minardi, L.M.; Swanson, T.J. Computerized tomographic scan findings in facial fractures associated with blindness. Plast Reconstr Surg 1981, 68, 479–490. [Google Scholar] [PubMed]
- Ey, W. [Orbital involvement in frontobasal injuries.]. Laryngol Rhinol Otol (Stuttg) 1981, 60, 162–167. [Google Scholar] [PubMed]
- Chen, K.T.; Chen, C.T.; Mardini, S.; Tsay, P.K.; Chen, Y.R. Frontal sinus fractures: a treatment algorithm and assessment of outcomes based on 78 clinical cases. Plast Reconstr Surg 2006, 118, 457–468. [Google Scholar] [PubMed]
- Merville, L. [Fronto-orbito-nasal dislocations: initial total reconstruction. Tactics, Advantages, Conditions.]. Rev Stomatol Chir Maxillofac 1977, 78, 1–17. [Google Scholar] [CrossRef]
- Raveh, J.; Laedrach, K.; Vuillemin, T.; Zingg, M. Management of combined frontonaso-orbital/skull base fractures and telecanthus in 355 cases. Arch Otolaryngol Head Neck Surg 1992, 118, 605–614. [Google Scholar]



© 2008 by the author. The Author(s) 2008.
Share and Cite
Metzinger, S.E.; Metzinger, R.C. Complications of Frontal Sinus Fractures. Craniomaxillofac. Trauma Reconstr. 2009, 2, 27-34. https://doi.org/10.1055/s-0029-1202597
Metzinger SE, Metzinger RC. Complications of Frontal Sinus Fractures. Craniomaxillofacial Trauma & Reconstruction. 2009; 2(1):27-34. https://doi.org/10.1055/s-0029-1202597
Chicago/Turabian StyleMetzinger, Stephen E., and Rebecca C. Metzinger. 2009. "Complications of Frontal Sinus Fractures" Craniomaxillofacial Trauma & Reconstruction 2, no. 1: 27-34. https://doi.org/10.1055/s-0029-1202597
APA StyleMetzinger, S. E., & Metzinger, R. C. (2009). Complications of Frontal Sinus Fractures. Craniomaxillofacial Trauma & Reconstruction, 2(1), 27-34. https://doi.org/10.1055/s-0029-1202597


