Advanced Simulation System for Orbitozygomatic Fracture Reconstruction: Multicenter Validation of a Novel Training and Objective Assessment Platform
Abstract
1. Introduction
2. Materials and Methods
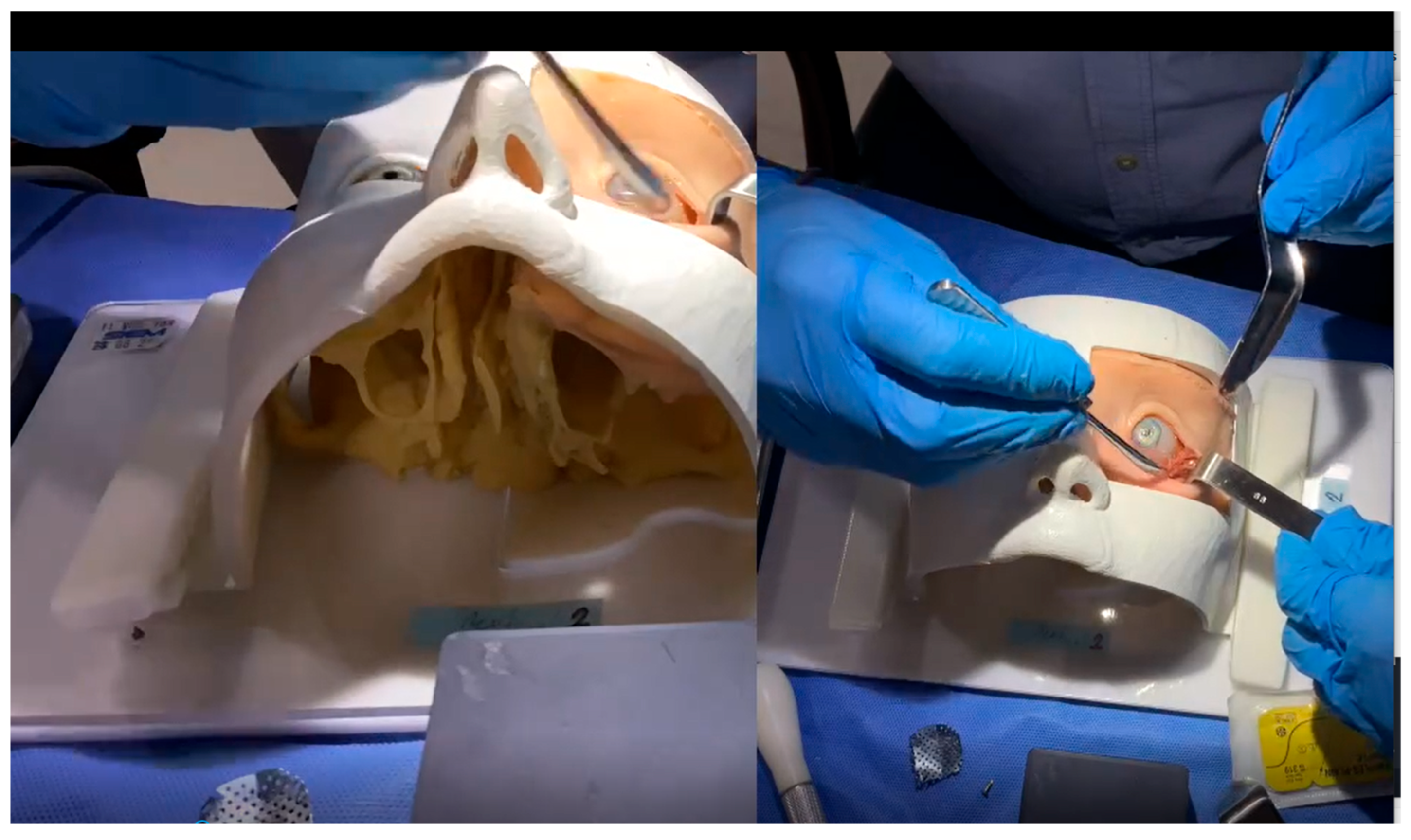
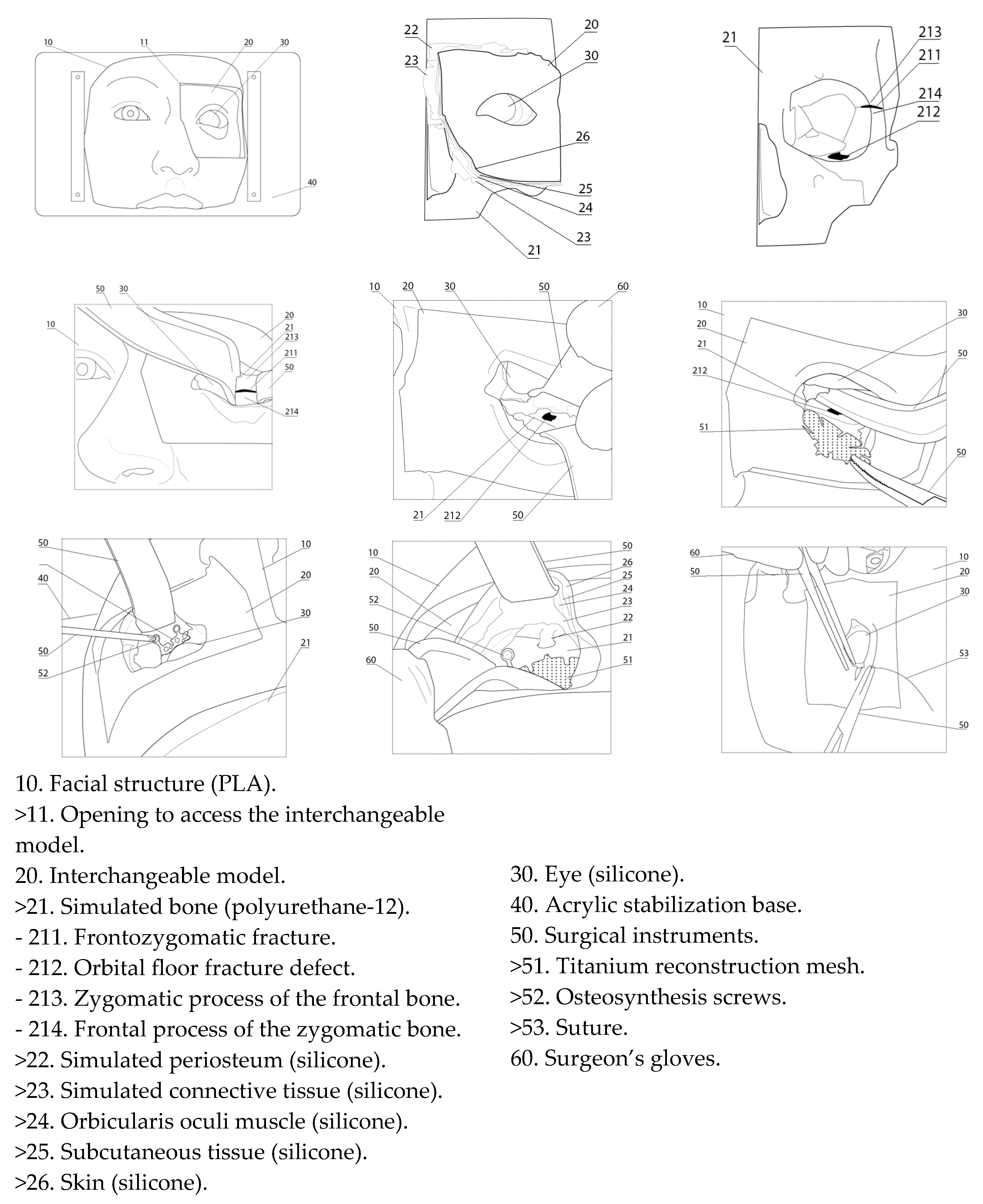
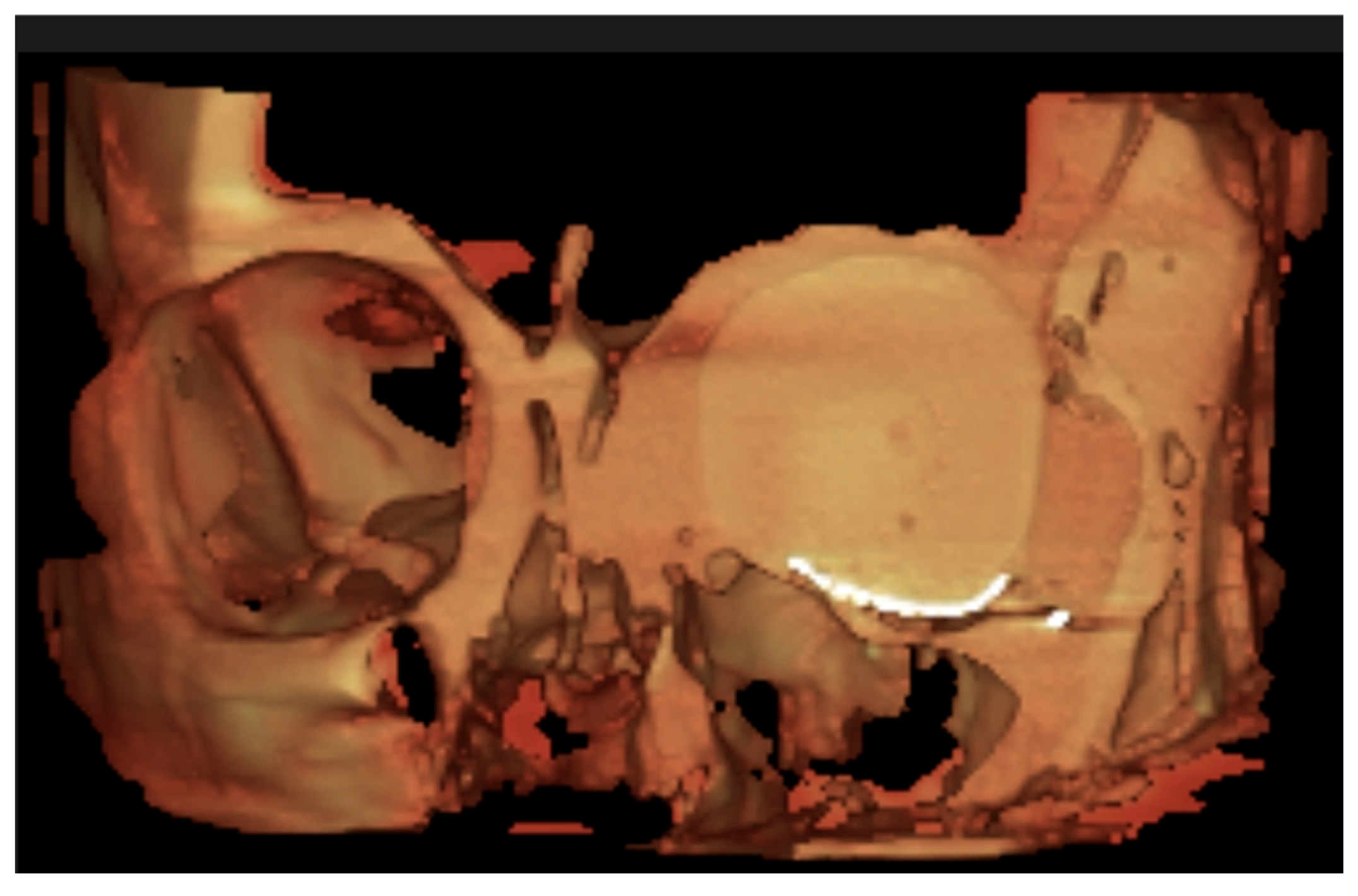
2.1. Simulation Model Construction
2.2. Ethics and Participants
2.3. Simulation Assessment
- Simulated surgeries were performed, during which performance data was collected for each participant. Procedures were video-recorded and assessed with ICSAD to measure performance metrics and evaluate construct validity through motion analysis.
- Immediately following the procedures, participants completed structured satisfaction surveys aimed at evaluating the face and content validity of the simulation model.
- Postoperative CBCT evaluation by a blinded radiologist assessed six key aspects using standardized criteria.
- In the fourth stage, two expert surgeon evaluators, blinded to participant identity and group allocation, reviewed the performance data collected during the first stage. Each participant was assessed using both a global rating scale (OSATS) and a specific objective, fault-based scale (Specific Fault Measurement, SFM) to evaluate technical performance.
- In the final phase, statistical comparisons were conducted between groups to determine whether significant differences in performance outcomes could be identified.
2.3.1. First Stage: Simulated Surgeries
2.3.2. Second Stage: Structured Satisfaction Surveys
Face and Content Validity
- The Face Validity Survey (Table 2) evaluated the anatomical accuracy and realism of the simulator, assessing whether it provided a convincing surgical environment.
- The Content Validity Survey (Table 3) assessed the simulator’s ability to effectively convey the procedural knowledge and technical skills necessary for a successful orbitozygomatic fracture reconstruction.
2.3.3. Third Stage: Cone-Beam Tomography Ancillary Assessment (CBCT)
2.3.4. Fourth Stage: Evaluation by Expert Surgeons
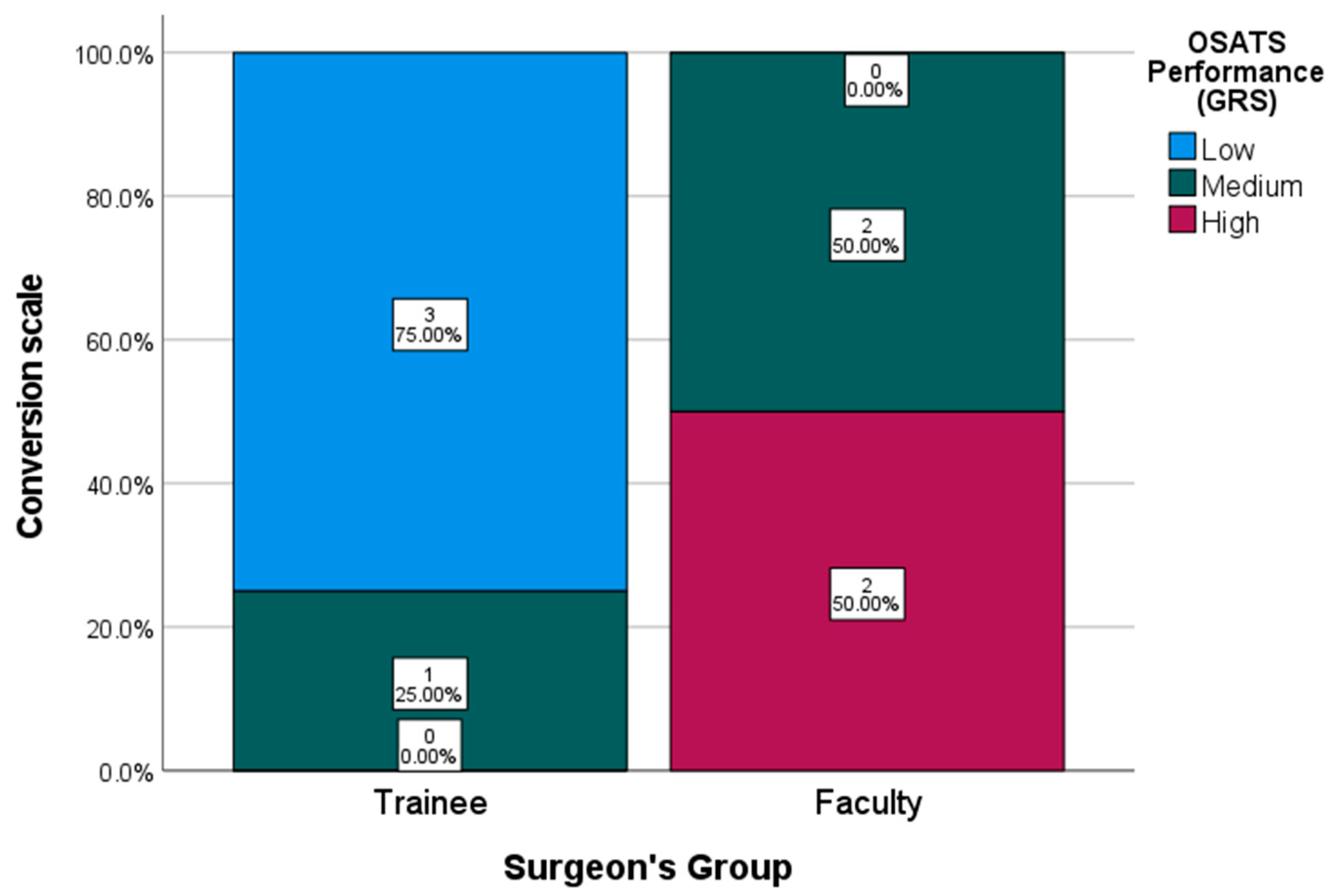
- The OSATS (Objective Structured Assessment of Technical Skills) scale, a 5-point Likert scale evaluating overall surgical competence.
- The Specific Fault Measurement (SFM) system records and quantifies each procedural error throughout the entire surgery, within the same five defined domains evaluated globally by the OSATS framework.
OSATS Global Rating Scale (GRS)
- Respect for tissue integrity.
- Avoidance of unnecessary movements.
- Absence of hesitant or awkward movements.
- Maintenance of a steady operative flow.
- Demonstrated procedural knowledge.
Specific Fault Measurement (SFM) Scale
2.3.5. Fifth Stage: Statistical Comparisons
3. Results
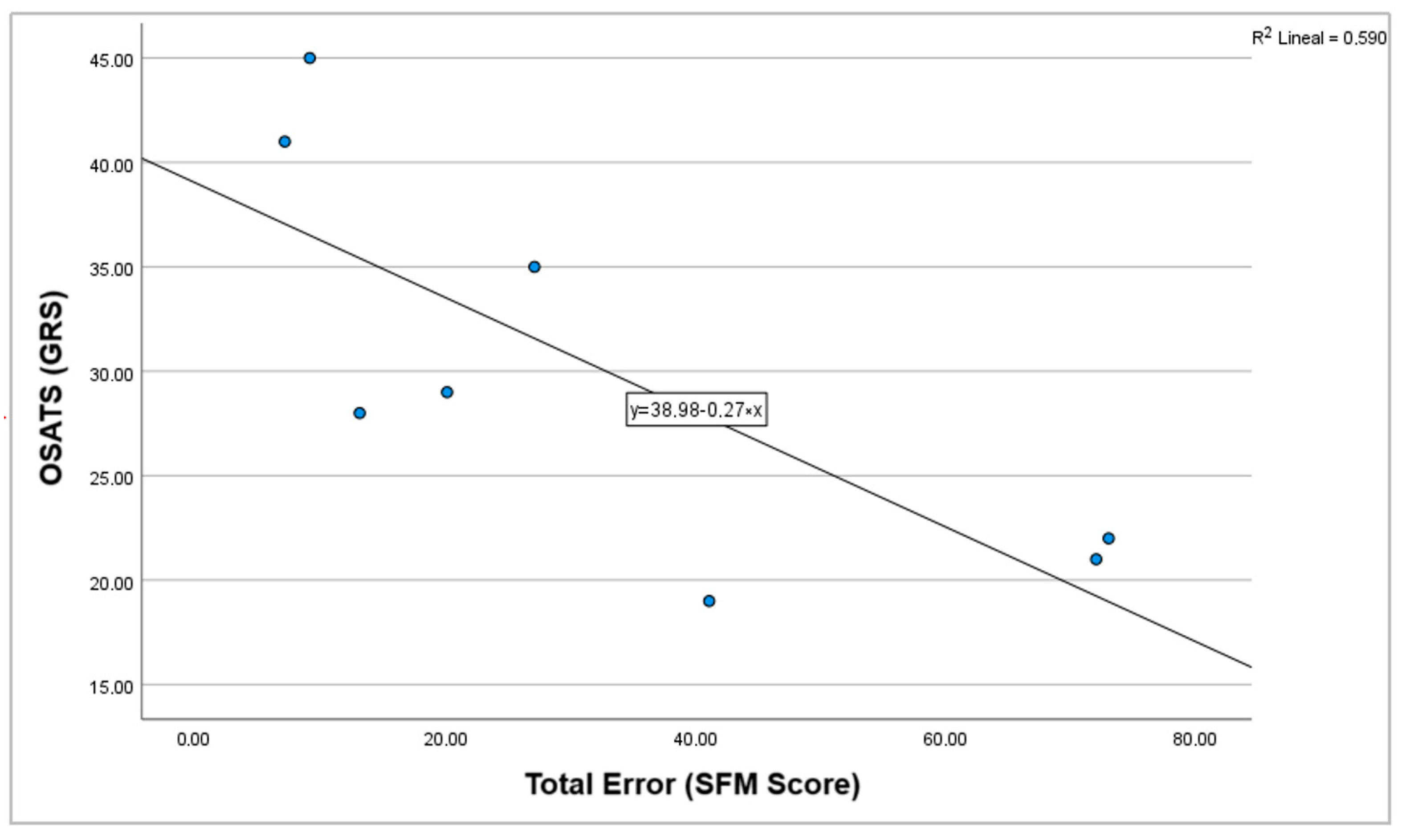
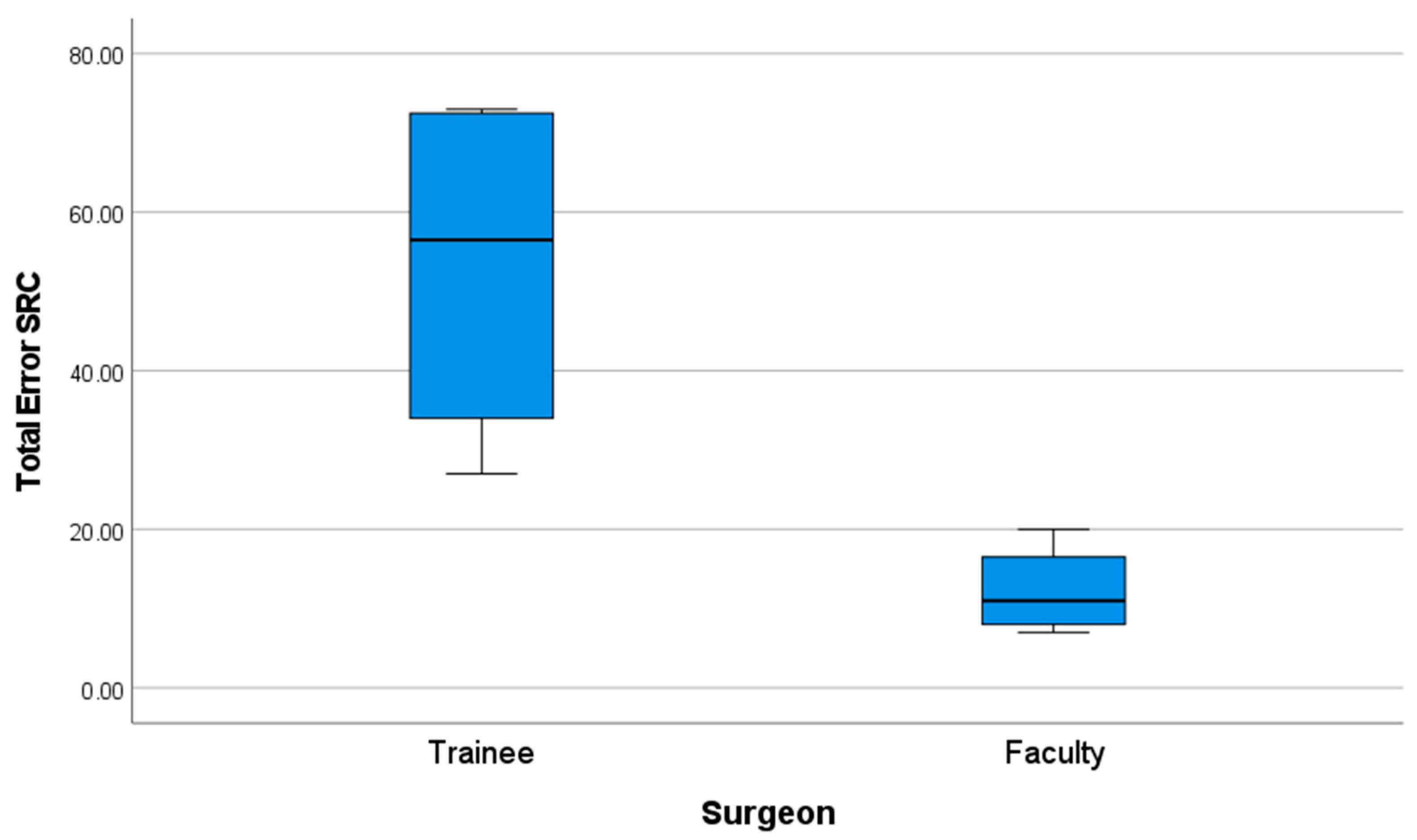
3.1. Construct Validity
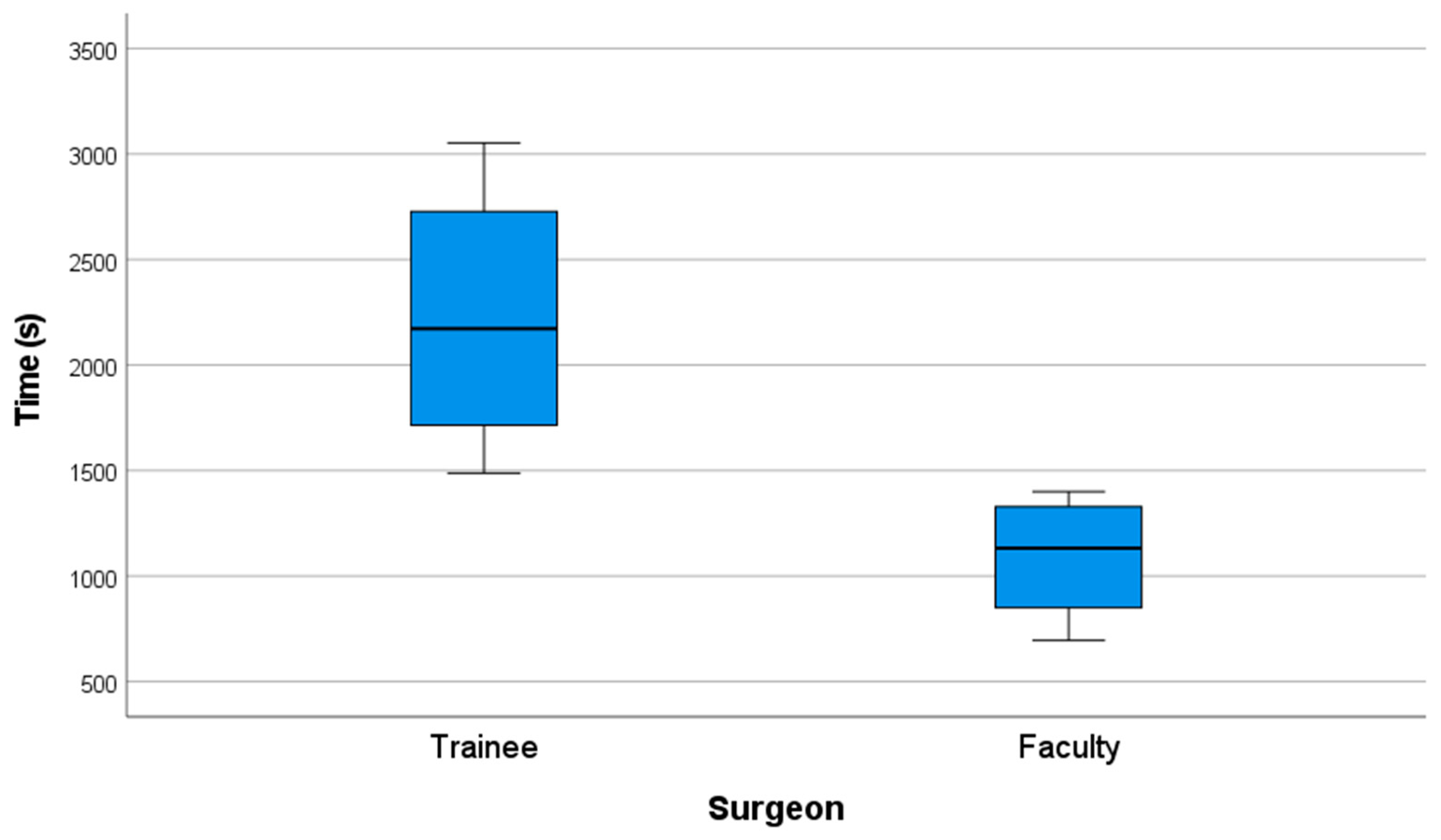
3.2. Operative Time Comparison
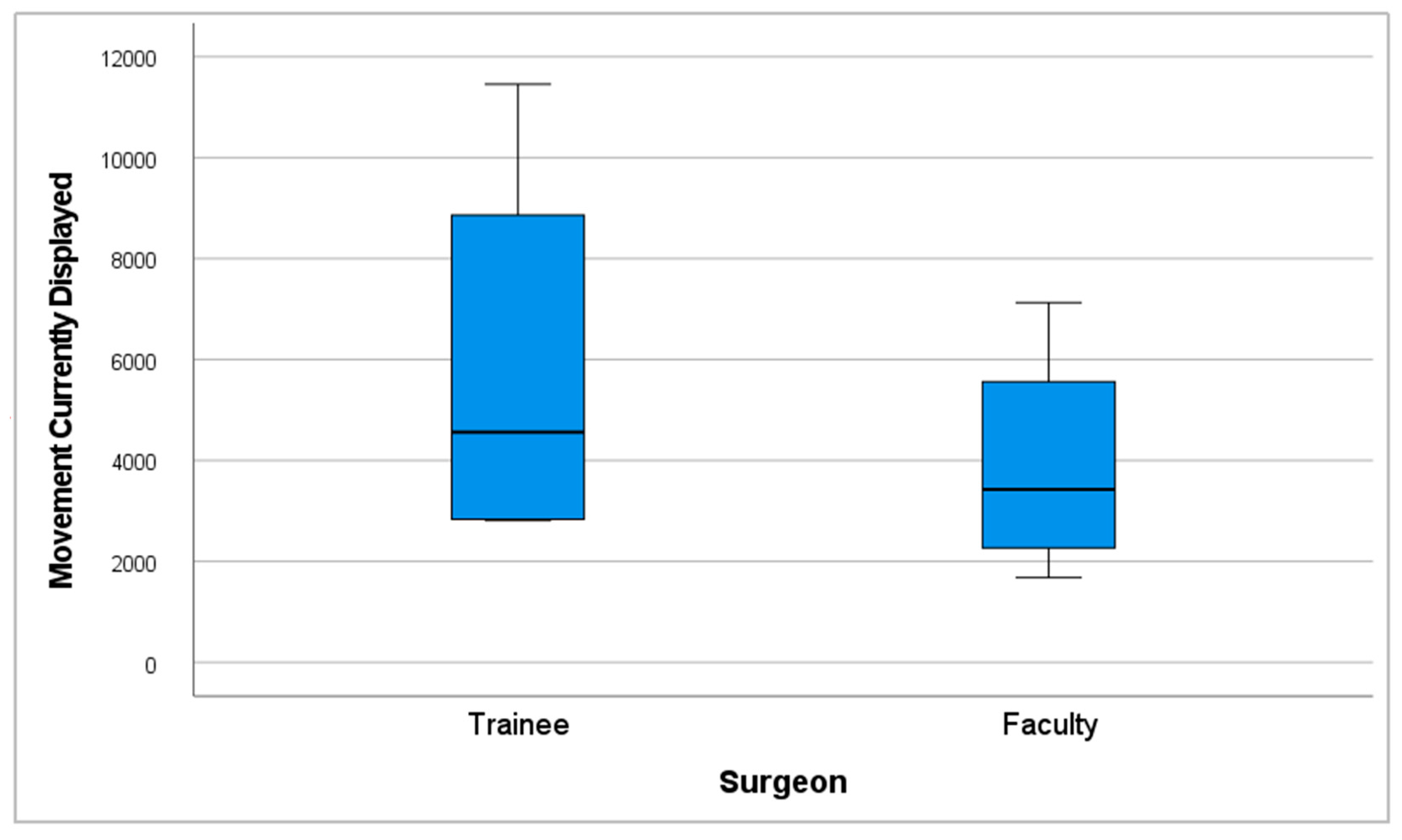
3.3. Hand Movement and Path Length Analysis
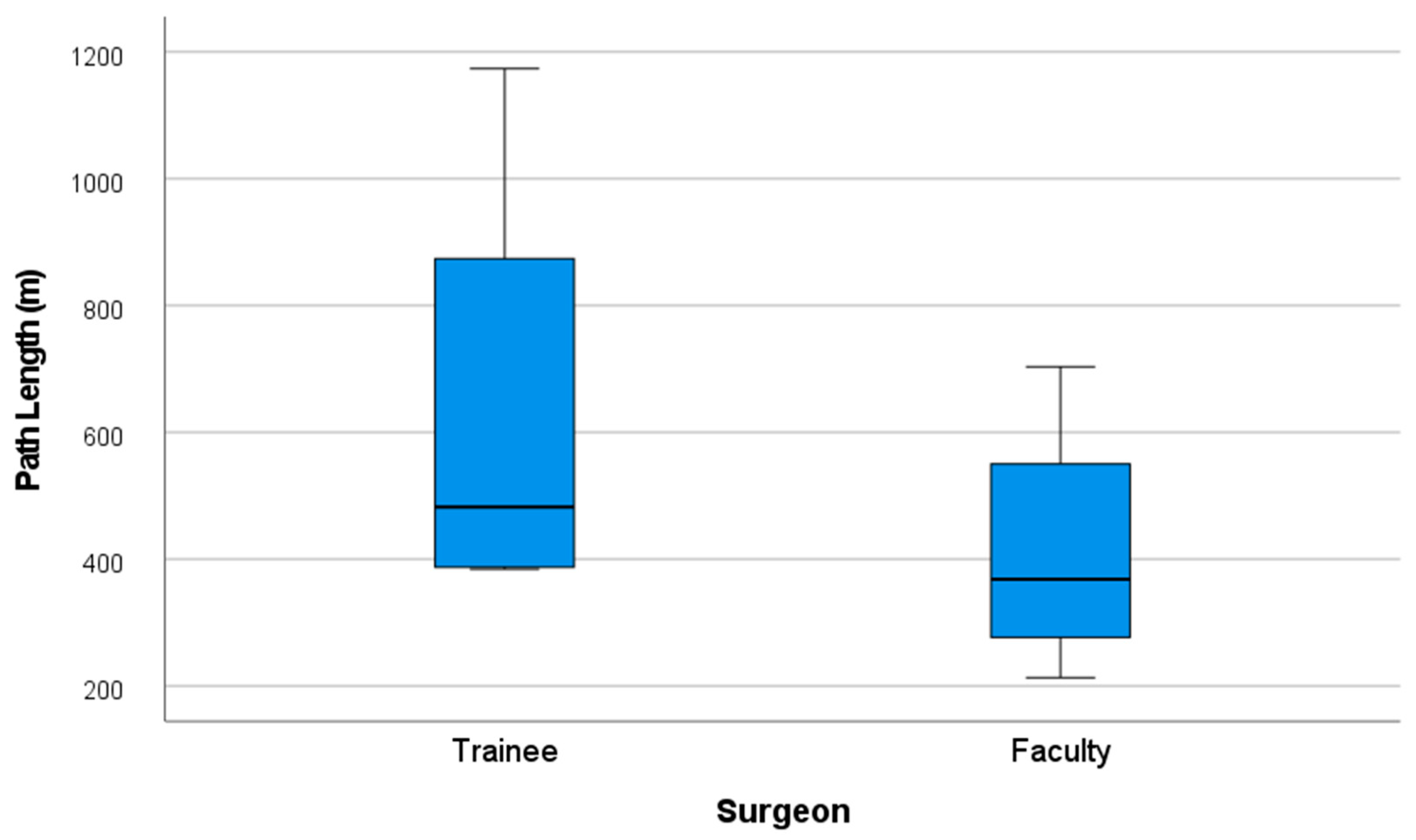
3.4. Content and Face Validity
3.4.1. Content Validity
- In terms of surgical approach training, 100% of respondents agreed that the simulator could be effectively used to teach access to orbitozygomatic fractures (mean = 4.7 out of 5; SD = 0.48).
- When asked about its applicability to real clinical settings, all participants (100%) agreed that the simulator could be effectively implemented as a training model in maxillofacial surgery residency programs, with the highest possible score in this item (mean = 4.8 out of 5; SD = 0.42).
- A total of 70% of respondents strongly agreed that the simulator achieved an appropriate level of realism for practicing fracture reduction, reconstruction, and fixation in this anatomical region (mean of 4.2 out of 5; SD = 0.92).
- Furthermore, 80% of participants agreed or strongly agreed that the simulator was suitable for learning the application of specific fixation systems, such as screws, plates, and meshes, relevant to the treatment of orbitozygomatic fractures (mean = 4.3 out of 5; SD = 1.34).
- Regarding its educational utility, 80% of participants strongly agreed that the simulator represents a valuable tool for training residents in performing reconstruction, reduction, and fixation procedures for orbitozygomatic fractures (mean = 4.7 out of 5; SD = 0.48).
- Lastly, 70% agreed or strongly agreed that the model is also useful for training surgeons with prior experience in maxillofacial trauma, highlighting its potential for continuing surgical education (mean = 3.7 out of 5; SD = 1.34).
3.4.2. Face Validity
- A total of 90% of respondents agreed or strongly agreed that the visual appearance of the blow-out fracture was realistic, with a mean score of 4.3 out of 5 (SD = 0.95).
- Similarly, 80% of participants agreed or strongly agreed that the visual representation of the frontozygomatic fracture appeared realistic, with a mean score of 4.3 out of 5 (SD = 0.82).
- Regarding anatomical representation, 100% of participants agreed or strongly agreed that the phantom accurately simulated the depth and anatomy of the orbitozygomatic region, achieving a mean score of 4.6 out of 5 (SD = 0.52).
- For soft tissue realism, 70% of participants reported that soft tissues felt realistic during the minimally invasive surgical approach, with a mean score of 3.7 out of 5 (SD = 0.82).
- In terms of bone structure simulation, 60% of respondents strongly agreed that both cortical and cancellous bone provided a realistic tactile experience during drilling and screw placement, with a mean score of 4.1 out of 5 (SD = 1.29).
3.5. Cone-Beam Tomography Ancillary Assessment (CBCT)
4. Discussion
4.1. Specific Rating Scale Validation
4.2. Future Directions
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ICSAD | Imperial College Surgical Assessment Device |
| OSATS | Objective Structured Assessment of Technical Skills |
| CONSORT | Consolidated Standards of Reporting Trials |
| STROBE | Strengthening the Reporting of Observational studies in Epidemiology |
| PLA | Polylactic Acid |
| CChC | Hospital Clínico Mutual de Seguridad |
| HOSCAR | Hospital de Carabineros |
| PUC | Pontificia Universidad Católica de Chile |
| SFM | Specific Fault Measurement |
| GRS | Global Rating Scale |
| SD | Standard Deviation |
References
- Carl-Peter, C.; Nils, G.; Søren, H.; Kenji, K.; Warren, S. Surgery Reference CMF Trauma Midface Introduction. Surgery Reference AO Fundation. 2025. Available online: https://surgeryreference.aofoundation.org/cmf/trauma/midface/further-reading/introduction?searchurl=/searchresults (accessed on 18 March 2025).
- Dhar, P.; Jones, J. Electric scooter-related oral and maxillofacial injuries in Oxfordshire. Br. J. Oral Maxillofac. Surg. 2024, 62, 826–830. [Google Scholar] [CrossRef]
- Azarmehr, I.; Stokbro, K.; Bell, R.B.; Thygesen, T. Contemporary Techniques in Orbital Reconstruction: A Review of the Literature and Report of a Case Combining Surgical Navigation, Computer-Aided Surgical Simulation, and a Patient-Specific Implant. J. Oral Maxillofac. Surg. 2020, 78, 594–609. [Google Scholar] [CrossRef] [PubMed]
- Christophel, J.J.; Park, S.S.; Nogan, S.J.; Essig, G.F. A Facial Trauma Simulation Course for Evaluation and Treatment of Facial Fractures. JAMA Facial Plast. Surg. 2017, 19, 464–467. [Google Scholar] [CrossRef] [PubMed]
- Pérez, S.V.; Correa, D.B.; Fuentes, C.C.; Mori, F.A.; Troncoso, G.S.; Sirandoni, R.F. Transconjunctival Approach Using Lateral Skin Extension for Reconstruction of Orbit Zygomatic Complex Fractures: Technique Description and a Case Series Analysis. Craniomaxillofacial Trauma Reconstr. 2021, 14, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Dhupar, V.; Akkara, F.; Gavhane, S.S.; Chodankar, N.U. ‘Y’ Modification of the cutaneous incision of the preseptal transconjunctival approach for the management of zygomatico-maxillary complex fractures: A prospective clinical study. J. Stomatol. Oral Maxillofac. Surg. 2024, 125, 101927. [Google Scholar] [CrossRef]
- Alshalah, M.E.; Enezei, H.H.; Aldaghir, O.M.; Khalil, A.A.; Aldelaimi, T.N.; Al-Ani, R.M. Direct or Indirect Surgical Approach of Zygomatic Complex Fracture: A Comparative Study. J Craniofac Surg. 2023, 34, 2433–2436. [Google Scholar] [CrossRef]
- Lee, R.; Raison, N.; Lau, W.Y.; Aydin, A.; Dasgupta, P.; Ahmed, K. A systematic review of simulation-based training tools for technical and non-technical skills in ophthalmology. Eye 2020, 34, 1737–1759. [Google Scholar] [CrossRef]
- Meara, D.J.; Coffey Zern, S. Simulation in craniomaxillofacial training. Curr. Opin. Otolaryngol. Head Neck Surg. 2016, 24, 376–380. [Google Scholar] [CrossRef]
- Borgersen, N.J.; Naur, T.M.H.; Sørensen, S.M.D.; Bjerrum, F.; Konge, L.; Subhi, Y. Gathering Validity Evidence for Surgical Simulation. Ann. Surg. 2018, 267, 1063–1068. [Google Scholar] [CrossRef]
- Zargaran, A.; Hirniak, J.; Zargaran, D. Oral and Maxillofacial Surgical simulation: Efficacy for medical students. Br. J. Oral Maxillofac. Surg. 2020, 58, 1251–1254. [Google Scholar] [CrossRef]
- Rojas, F.; Tapia, S.; Campolo, A.; Vargas, A.; Ramírez, H.; Benitez, B.K.; Teuber, C.E. Simulating A Subcondylar Mandibular Fracture With Intraoral Open Reduction and Internal Fixation: A Novel Education Tool for Residents. Craniomaxillofacial Trauma Reconstr. 2023, 16, 275–280. [Google Scholar] [CrossRef]
- Adams, J.W.; Paxton, L.; Dawes, K.; Burlak, K.; Quayle, M.; McMenamin, P.G. 3D printed reproductions of orbital dissections: A novel mode of visualising anatomy for trainees in ophthalmology or optometry. Br. J. Ophthalmol. 2015, 99, 1162–1167. [Google Scholar] [CrossRef]
- Segall, S.C.; Lavell, K.; Brody, A. Lateral Canthotomy and Cantholysis Simulation Device. United States; US11710425B2. 2023. Available online: https://patentimages.storage.googleapis.com/c2/f6/2d/23169e4478b8cb/US11710425.pdf (accessed on 23 May 2025).
- Ottensmeyer, M.P.; de Novi, G.; Loan, G.J.; Scott Bardsley, R.; Cho Moore, J. Trauma Training Simulator with Event-Based Gesture Detection and Instrument-Motion Tracking. United States; US9595208B2. 2017. Available online: https://patentimages.storage.googleapis.com/03/ee/d6/2f3604d2d8fad7/US9595208.pdf (accessed on 23 May 2025).
- Hine, J.F. Anatomical Head and Neck Simulator Apparatus. United States; US20240233579A9. 2024. Available online: https://patentimages.storage.googleapis.com/44/9f/6c/d2064605250ada/US20240233579A9.pdf (accessed on 23 May 2025).
- Gada, S.M.; Liacouras, P.C.; Wyn, M.J.; Garnes, J.A. Ophthalmic Training Simulator. United States; US10410543B2. 2019. Available online: https://patentimages.storage.googleapis.com/60/46/01/8027a0979b8fba/US10410543.pdf (accessed on 23 May 2025).
- Marson, B.A.; Sutton, L.J. The Newport eye: Design and initial evaluation of a novel foreign body training phantom. Emerg. Med. J. 2014, 31, 329–330. [Google Scholar] [CrossRef]
- Scawn, R.L.; Foster, A.; Lee, B.W.; Kikkawa, D.O.; Korn, B.S. Customised 3D Printing: An Innovative Training Tool for the Next Generation of Orbital Surgeons. Orbit 2015, 34, 216–269. [Google Scholar] [CrossRef] [PubMed]
- Jacobo, O.M.; Giachero, V.E.; Hartwig, D.K.; Mantrana, G.A. Three-dimensional printing modeling: Application in maxillofacial and hand fractures and resident training. Eur. J. Plast. Surg. 2018, 41, 137–146. [Google Scholar] [CrossRef]
- Cheng, A.; Kessler, D.; Mackinnon, R.; Chang, T.P.; Nadkarni, V.M.; Hunt, E.A. Reporting guidelines for health care simulation research: Extensions to the CONSORT and STROBE statements. Adv. Simul. 2016, 1, 25. [Google Scholar] [CrossRef] [PubMed]
- Santander, M.J.; Sepúlveda, V.; Iribarren, J.; Rosenbaum, A.; Albrich, D.; Varas, J.; Napolitano, C. Development and Validation of a Laryngeal Microsurgery Simulation Training System for Otolaryngology Residents. Otolaryngol. Head Neck Surg. 2023, 169, 971–987. [Google Scholar] [CrossRef]
- Kazan, R.; Viezel-Mathieu, A.; Cyr, S.; Hemmerling, T.M.; Gilardino, M.S. The Montreal Augmentation Mammaplasty Operation (MAMO) Simulator: An Alternative Method to Train and Assess Competence in Breast Augmentation Procedures. Aesthetic Surg. J. 2018, 38, 835–849. [Google Scholar] [CrossRef]
- Ayub, S.M. “See one, do one, teach one”: Balancing patient care and surgical training in an emergency trauma department. J. Glob. Health 2022, 12, 03051. [Google Scholar] [CrossRef]
- Datta, V.; Mackay, S.; Mandalia, M.; Darzi, A. The Use of Electromagnetic Motion Tracking Analysis to Objectively Measure Open Surgical Skill in The Laboratory-Based Model. J. Am. Coll. Surg. 2001, 193, 479–485. [Google Scholar] [CrossRef]
- Corvetto, M.A.; Fuentes, C.; Araneda, A.; Achurra, P.; Miranda, P.; Viviani, P.; Altermatt, F.R. Validation of the imperial college surgical assessment device for spinal anesthesia. BMC Anesthesiol. 2017, 17, 131. [Google Scholar] [CrossRef] [PubMed]
- Johnston, S.; Coyer, F.M.; Nash, R. Kirkpatrick’s Evaluation of Simulation and Debriefing in Health Care Education: A Systematic Review. J. Nurs. Educ. 2018, 57, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Niitsu, H.; Hirabayashi, N.; Yoshimitsu, M.; Mimura, T.; Taomoto, J.; Sugiyama, Y.; Takiyama, W. Using the Objective Structured Assessment of Technical Skills (OSATS) global rating scale to evaluate the skills of surgical trainees in the operating room. Surg. Today 2013, 43, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.A.; Regehr, G.; Reznick, R.; Macrae, H.; Murnaghan, J.; Hutchison, C.; Brown, M. Objective structured assessment of technical skill (OSATS) for surgical residents. Br. J. Surg. 1997, 84, 273–278. [Google Scholar] [CrossRef]
- Consorti, G.; Paglianiti, M.; Monarchi, G.; de Tomaso, S.; Cirignaco, G.; Gasperoni, M.; Gennaro, P. New test for systematic skills enhancement and improvement in maxillofacial surgery training: Multicentre pilot study. Br. J. Oral Maxillofac. Surg. 2024, 2, 716–721. [Google Scholar] [CrossRef]
- Boza, C.; León, F.; Buckel, E.; Riquelme, A.; Crovari, F.; Martínez, J.; Gennaro, P. Simulation-trained junior residents perform better than general surgeons on advanced laparoscopic cases. Surg. Endosc. 2017, 31, 135–141. [Google Scholar] [CrossRef]
- Kolozsvari, N.O.; Feldman, L.S.; Vassiliou, M.C.; Demyttenaere, S.; Hoover, M.L. Sim One, Do One, Teach One: Considerations in Designing Training Curricula for Surgical Simulation. J. Surg. Educ. 2011, 68, 421–427. [Google Scholar] [CrossRef]
- Cohen, E.R.; Feinglass, J.; Barsuk, J.H.; Barnard, C.; O’Donnell, A.; McGaghie, W.C.; Wayne, D.B. Cost Savings from Reduced Catheter-Related Bloodstream Infection After Simulation-Based Education for Residents in a Medical Intensive Care Unit. Simul. Healthc. J. Soc. Simul. Healthc. 2010, 5, 98–102. [Google Scholar] [CrossRef]
- Bae, D.S.; Lynch, H.; Jamieson, K.; Yu-Moe, C.W.; Roussin, C. Improved Safety and Cost Savings from Reductions in Cast-Saw Burns After Simulation-Based Education for Orthopaedic Surgery Residents. J. Bone Jt. Surg. 2017, 99, e94. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, R.; Darzi, A. Simulation to Enhance Patient Safety. Chest 2011, 140, 854–858. [Google Scholar] [CrossRef]
- Vargas, E. Fantoma Personalizable de Tercio Medio Facial Para Simulación de Reconstrucción de Fracturas Orbito Cigomáticas; Díaz, F.A.P., Ed.; CVE 2609714; Diario Oficial de la República de Chile, Ministerio del Interior: Santiago, Chile, 2025; p. 1. [Google Scholar]
- Coronel, B.V.; Álvarez, R.I.S.; Riveros, F.B.; Schilling, M.M.; Espinoza, V.D.; Jaras, I.M.; Cohen, J.V. Minor surgery course using remote and asynchronous feedback: Training wherever, whenever. Glob. Surg. Educ. J. Assoc. Surg. Educ. 2023, 2, 109. [Google Scholar] [CrossRef]
- Morales, S.; Lam, P.; Cerrato, R.; Mococain, P.; Ruz, C.; Filippi, J.; Villa, A.; Varas, J. A novel simulation model and training program for minimally invasive surgery of hallux valgus. J. Am. Acad. Orthop. Surg. 2024, 32, e816–e825. [Google Scholar] [CrossRef] [PubMed]
- Jarry, C.; Varas, J.; Inzunza, M.; Escalona, G.; Machuca, E.; Vela, J.; Bellolio, F.; Larach, J.T. Design and validation of a simulation-based training module for ileo-transverse intracorporeal anastomosis. Surg Endosc. 2025, 39. [Google Scholar] [CrossRef]
- Rojas, M.F.; Torres, J.; Figueroa, U.; Varas, J.; Achurra, P.; Navia, A.; Cuadra, A.; Searle, S. Validation of a synthetic simulation model of endoscopic rectus sheath plication. Hernia 2024, 28, 1381–1390. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, C.; Vela, J.; Contreras, C.; Belmar, F.; Paul, I.; Zinco, A.; Ramos, J.P.; Ottolino, P.; Achurra-Tirado, P.A.; Jarufe, N.; et al. A new approach for the acquisition of trauma surgical skills: An OSCE type of simulation training program. Surg. Endosc. 2022, 36, 8441–8550. [Google Scholar] [CrossRef]
- Varas, J.; Belmar, F.; Fuentes, J.; Vela, J.; Contreras, C.; Letelier, L.M.; Riquelme, A.; Asbun, D.; Abbott, E.F.; Escalona, G.; et al. Improving medical student performance with unsupervised simulation and remote asynchronous feedback. J. Surg. Educ. 2024, 81. [Google Scholar] [CrossRef] [PubMed]
- Fried, G.M.; Varas, J.; Telem, D.A.; Greenberg, C.C.; Hashimoto, D.A.; Paige, J.T.; Pugh, C. Opportunities and applications of educational technologies in surgical education and assessment. Ann. Surg. 2025, 281, 34–39. [Google Scholar] [CrossRef]
- Trujillo, C.J.; Ulloa, J.V.; Vivas, G.E.; Escobar, E.G.; Gutiérrez, I.V.; Tirado, P.A.; Cohen, J.V. Surgeons vs ChatGPT: Assessment and feedback performance based on real surgical scenarios. J. Surg. Educ. 2024, 81, 960–966. [Google Scholar] [CrossRef]
- Coffey-Zern, S.; Calvi, R.M.D.; Vorrasi, J.S.; Meara, D.J. Incorporating Simulation into Oral and Maxillofacial Surgery Residency Education and Training: Christiana Care’s Method. J. Oral Maxillofac. Surg. 2015, 73, 1244–1245. [Google Scholar] [CrossRef]
- Peserico-DalFarra, P.; Gagliardi-Lugo, A.F. Training simulation for oral and maxillofacial surgeons based on the techniques of arthroscopy in the temporomandibular joint. Br. J. Oral Maxillofac. Surg. 2019, 57, 929–931. [Google Scholar] [CrossRef]
- Bertin, H.; Huon, J.F.; Praud, M.; Fauvel, F.; Salagnac, J.M.; Perrin, J.P.; Corre, P. Bilateral sagittal split osteotomy training on mandibular 3-dimensional printed models for maxillofacial surgical residents. Br. J. Oral Maxillofac. Surg. 2020, 58, 953–958. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, A.; Faba, G.; Varas, J.; Andrade, T. Septoplasty Training During the COVID-19 Era: Development and Validation of a Novel Low-Cost Simulation Model. OTO Open 2022, 6. [Google Scholar] [CrossRef] [PubMed]

| Initial Survey—Assessment of Surgical Experience 1. Level of Training in Oral and Maxillofacial Surgery and Traumatology: ☐ Resident ☐ Specialist 2. Years of Experience: How many years have you been practicing as a Resident or Specialist? ______ years. 3. Current Areas of Professional Practice: Mark with an X all the areas in which you are currently active: ☐ Teaching activities ☐ Non-surgical clinical practice ☐ Operating room activities ☐ Administrative duties 4. Career Interruptions: Please indicate whether you have had to suspend your clinical or surgical activities for a period longer than 6 months during your career: ☐ I have never suspended activities for more than 6 months ☐ I have suspended clinical/surgical activities for more than 6 months Reason: _______________________________ 5. Experience with Surgical Simulation: Have you previously performed surgical simulation using high-fidelity mannequins (phantoms)? ☐ Yes ☐ No 6. Knowledge of the Surgical Procedures to Be Simulated: Are you familiar with the surgical procedures that will be simulated during the practical session? ☐ Yes, I am familiar with them and have practiced them before ☐ Yes, I am familiar with them, but I have not had the opportunity to practice them ☐ No, I am not familiar with them 7. Practical Experience in Surgical Procedures: If you had to estimate the number of surgeries in which you have performed these procedures on real patients during your career, what would that number be? Number of surgeries: ______ |
| Face Validity Statement | Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| 1. The visual appearance of the blow-out fracture looks realistic. | |||||
| 2. The visual appearance of the frontozygomatic fracture looks realistic. | |||||
| 3. The phantom accurately simulates the depth and shape of the orbitozygomatic anatomy. | |||||
| 4. The soft tissues of the orbitozygomatic complex feel realistic when performing the minimally invasive surgical approach. | |||||
| 5. The cortical bone and cancellous bone feel realistic when drilling and inserting screws. | |||||
| 6. I believe I would practice with this simulator before performing an actual orbitozygomatic fracture surgery. |
| Content Validity Statement | Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| 7. The simulator achieves overall realism for practicing reconstruction, reduction, and fixation of orbitozygomatic complex fractures. | |||||
| 8. This simulator is a useful tool for residents to learn how to perform reconstruction, reduction, and fixation of orbitozygomatic complex fractures. | |||||
| 9. This simulator is a useful tool for training surgeons with prior experience in maxillofacial trauma. | |||||
| 10. You would consider implementing this simulator as a training model for maxillofacial surgery residents. | |||||
| 11. This simulator can be used to learn how to perform surgical access to orbitozygomatic complex fractures. | |||||
| 12. This simulator is suitable for learning how to use the screw, plate, and mesh systems specific to orbitozygomatic complex fractures. |
| Category | Evaluated Aspect |
|---|---|
| 1. Mesh–bone interface. | Presence or absence of soft tissue at the mesh–bone interface. |
| 2. Mesh/function. | Mesh position preventing or allowing orbital fat protrusion into the maxillary sinus. |
| 3. Mesh/position. | Complete coverage of the orbital floor |
| 4. Mesh adaptation. | Proper anatomical adaptation to the orbital cavity. |
| 5. Mesh positional integrity. | Evidence of displacement, deformation, or rotation. |
| 6. Relationship with maxillary sinus. | Presence or absence of sinus invasion. |
| Performance Level | Score Range |
|---|---|
| Low | 10–23 |
| Intermediate | 24–37 |
| High | 38–50 |
| Category | Type of Error Committed | Number of Errors Observed |
|---|---|---|
| 1. Respect for Tissue | Violation of appropriate tissue handling. | |
| 2. Unnecessary Movements | Performs unnecessary or non-purposeful movements. | |
| 3. Hesitant or Clumsy Movements | Exhibits hesitation or clumsiness during any part of the procedure. | |
| 4. Operative Flow | Interrupts or disrupts the surgical workflow. | |
| 5. Procedural Knowledge | Demonstrates lack of procedural knowledge by making an error, expressing uncertainty, or requiring clarification on the next steps. | |
| Total Errors (SFM Score) | Sum of all errors committed across categories. |
| Group | n | Age, Mean (Range) | Years in Practice, Mean (Range) | No. of Orbitozygomatic Surgeries, Mean (Range) | No. of Surgeries per Year, Mean (Range) |
|---|---|---|---|---|---|
| Trainees | 4 | 33 (29–36) | 2.5 (2–4) | 0.75 (0–3) | 0.19 (0–0.75) |
| Faculty | 6 | 47 (39–63) | 14.8 (7–26) | 351.67 (30–1600) | 17.12 (4–61.53) |
| Statistics | ||||
|---|---|---|---|---|
| Specific Fault Measurement (SFM) | ||||
| Trainees | N | Valid | 4 | |
| Missing | 0 | |||
| Mean | 53.25 | |||
| Std. Deviation | 22.955 | |||
| Minimum | 27 | |||
| Maximum | 73 | |||
| Percentiles | 25 | 30.50 | ||
| 50 | 56.50 | |||
| 75 | 72.75 | |||
| Faculty | N | Valid | 4 | |
| Missing | 0 | |||
| Mean | 12.25 | |||
| Std. Deviation | 5.737 | |||
| Minimum | 7 | |||
| Maximum | 20 | |||
| Percentiles | 25 | 7.50 | ||
| 50 | 11.00 | |||
| 75 | 18.25 | |||
| Test Statistics a | ||||
| Specific Fault Measurement (SFM) | ||||
| Mann–Whitney U | 0.000 | |||
| Wilcoxon W | 10.000 | |||
| Z | −2.309 | |||
| Asymp. Sig. (2-tailed) | 0.021 | |||
| Exact Sig. [2(1-tailed Sig.)] | 0.029 b | |||
| Statistics | |||
|---|---|---|---|
| Time | |||
| Trainees | N | Valid | 4 |
| Missing | 0 | ||
| Mean | 2221.25 | ||
| Std. Deviation | 668.360 | ||
| Minimum | 1488 | ||
| Maximum | 3053 | ||
| Percentiles | 25 | 1601.50 | |
| 50 | 2172.00 | ||
| 75 | 2890.25 | ||
| Faculty | N | Valid | 4 |
| Missing | 0 | ||
| Mean | 1089.75 | ||
| Std. Deviation | 309.518 | ||
| Minimum | 695 | ||
| Maximum | 1400 | ||
| Percentiles | 25 | 772.75 | |
| 50 | 1132.00 | ||
| 75 | 1364.50 | ||
| Test Statistics a | |||
| Time | |||
| Mann–Whitney U | 0.000 | ||
| Wilcoxon W | 10.000 | ||
| Z | −2.309 | ||
| Asymp. Sig. (2-tailed) | 0.021 | ||
| Exact Sig. [2(1-tailed Sig.)] | 0.029 b | ||
| Content Validity Questions Statement/Answers (N = 10) | Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| This simulator can be used to learn how to perform surgical access to fractures of the orbitozygomatic complex. | 7 (70%) | 3 (30%) | 0 (0%) | 0 (0%) | 0 (0%) |
| I would consider it appropriate to implement this simulator as a training model for maxillofacial surgery residents. | 8 (80%) | 2 (20%) | 0 (0%) | 0 (0%) | 0 (0%) |
| The simulator achieves general realism for practicing reconstruction, reduction, and fixation of fractures of the orbitozygomatic complex. | 5 (50%) | 2 (20%) | 3 (30%) | 0 (0%) | 0 (0%) |
| This simulator is suitable for learning how to use the screw, plate, and mesh system specific for fractures of the orbitozygomatic complex. | 7 (70%) | 1 (10%) | 1 (10%) | 0 (0%) | 1 (10%) |
| This simulator is a useful tool for residents to learn how to perform reconstruction, reduction, and fixation of orbitozygomatic complex fractures. | 8 (80%) | 2 (20%) | 0 (0%) | 0 (0%) | 0 (0%) |
| This simulator is a useful tool for training surgeons with previous experience in maxillofacial trauma. | 3 (30%) | 4 (40%) | 1 (10%) | 1 (10%) | 1 (10%) |
| Face Validity Questions Statement/Answers (N = 10) | Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| The visual appearance of the Blow out Fracture looks realistic | 5 (50%) | 4 (40%) | 0 (0%) | 1 (10%) | 0 (0%) |
| The visual appearance of the frontozygomatic fracture looks realistic. | 5 (50%) | 3 (30%) | 2 (20%) | 0 (0%) | 0 (0%) |
| The model adequately simulates the depth and shape of the orbitozygomatic anatomy | 6 (60%) | 4 (40%) | 0 (0%) | 0 (0%) | 0 (0%) |
| The soft tissues of the Zygomatic-orbital complex feel realistic when performing minimally invasive surgical access. | 1 (10%) | 6 (60%) | 2 (20%) | 1 (10%) | 0 (0%) |
| Realistic cortical bone and cancellous bone feel when drilling and inserting screws | 6 (60%) | 1 (10%) | 1 (10%) | 2 (20%) | 0 (0%) |
| Do you think you would practice with this simulator before an actual orbitozygomatic complex fracture surgery? | 6 (60%) | 4 (40%) | 0 (0%) | 0 (0%) | 0 (0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vargas, E.; Díaz, R.; Vargas, J.P.; Campolo, A.; Villanueva, R.; Cortéz, C.; Valladares-Pérez, S. Advanced Simulation System for Orbitozygomatic Fracture Reconstruction: Multicenter Validation of a Novel Training and Objective Assessment Platform. Craniomaxillofac. Trauma Reconstr. 2025, 18, 34. https://doi.org/10.3390/cmtr18030034
Vargas E, Díaz R, Vargas JP, Campolo A, Villanueva R, Cortéz C, Valladares-Pérez S. Advanced Simulation System for Orbitozygomatic Fracture Reconstruction: Multicenter Validation of a Novel Training and Objective Assessment Platform. Craniomaxillofacial Trauma & Reconstruction. 2025; 18(3):34. https://doi.org/10.3390/cmtr18030034
Chicago/Turabian StyleVargas, Enrique, Rodrigo Díaz, Juan Pablo Vargas, Andrés Campolo, Rodrigo Villanueva, Carlos Cortéz, and Salvador Valladares-Pérez. 2025. "Advanced Simulation System for Orbitozygomatic Fracture Reconstruction: Multicenter Validation of a Novel Training and Objective Assessment Platform" Craniomaxillofacial Trauma & Reconstruction 18, no. 3: 34. https://doi.org/10.3390/cmtr18030034
APA StyleVargas, E., Díaz, R., Vargas, J. P., Campolo, A., Villanueva, R., Cortéz, C., & Valladares-Pérez, S. (2025). Advanced Simulation System for Orbitozygomatic Fracture Reconstruction: Multicenter Validation of a Novel Training and Objective Assessment Platform. Craniomaxillofacial Trauma & Reconstruction, 18(3), 34. https://doi.org/10.3390/cmtr18030034






