Virtual Surgical Planning for Management of Acute Maxillofacial Trauma
Abstract
1. Background
- Provide an overview of useful VSP services for patients with complex maxillofacial trauma.
- Describe a case series of ten patients with severe maxillofacial trauma for which commercial VSP services were successfully implemented during their initial hospital admission.
- Propose indications to consider VSP when treating acute maxillofacial trauma.
2. VSP Services for Maxillofacial Trauma
2.1. Virtual Fracture Reduction
2.2. Occlusal Splints
2.3. Patient Models
2.4. Patient-Specific Plates and Other Anatomic Implants
3. Patients and Methods
4. Selected Illustrative Cases
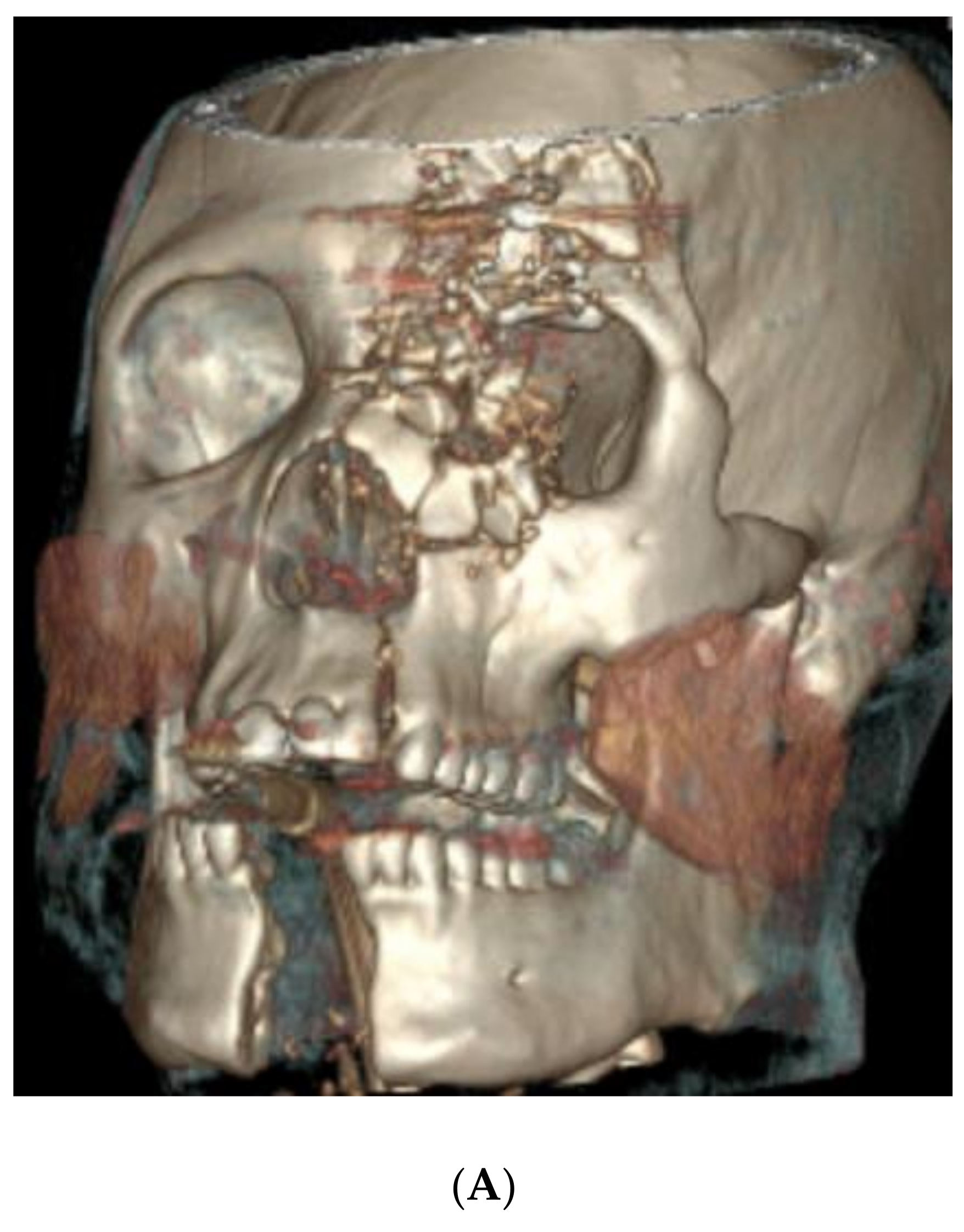
4.1. Case 1 (Occlusal Splint)
- An extensive calvarial fracture involving the left frontal sinus and left cribriform plate;
- Comminuted fractures of the left medial, superior, and inferior orbital walls;
- Left Le Fort I/II maxillary fractures;
- A comminuted transverse palatal fracture;
- A left mandibular symphyseal fracture (with 2.4 cm diastasis between the fracture segments);
- A comminuted nasal bone fracture.
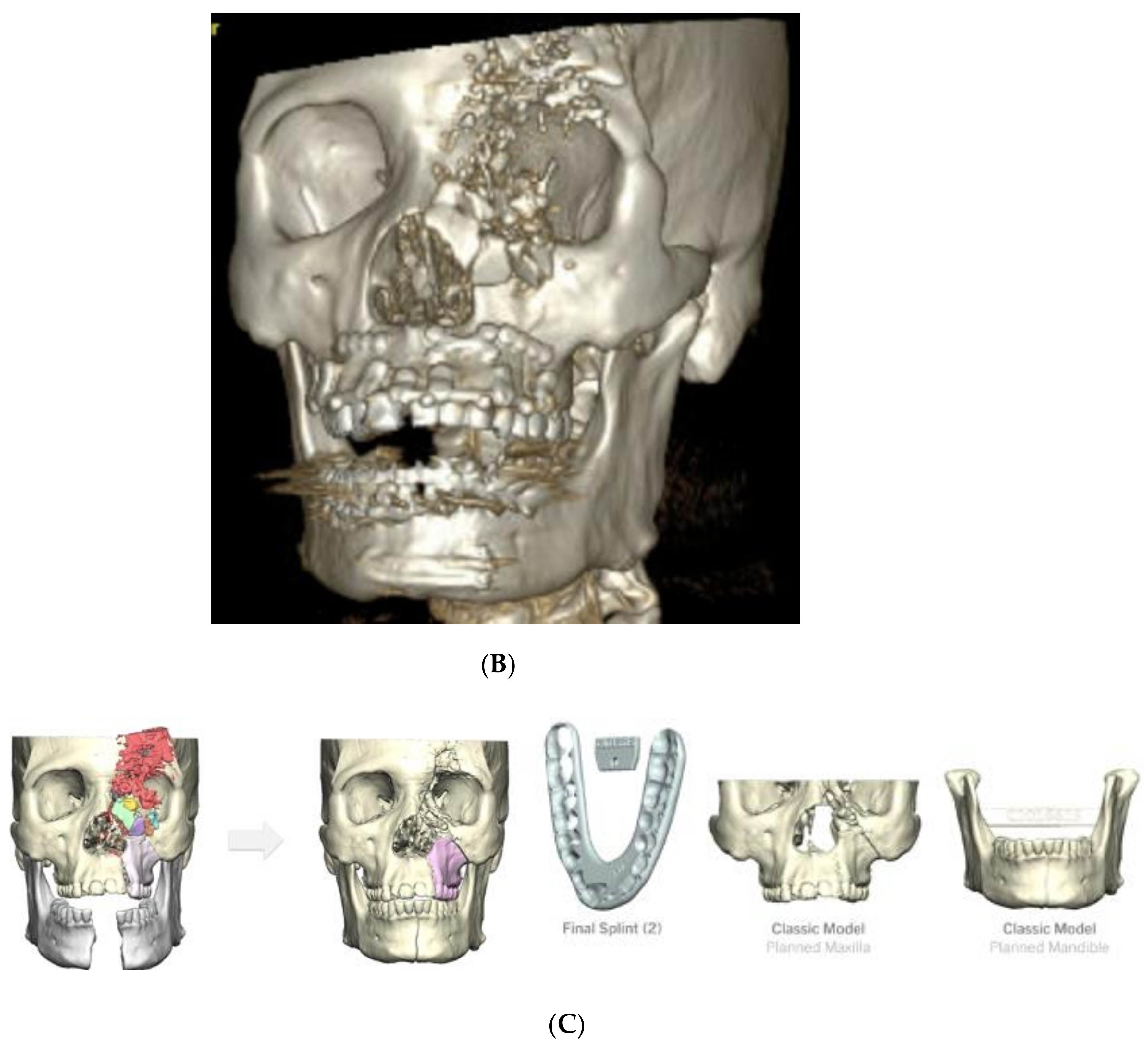
4.2. Case 2 (Occlusal Splint, 3D Model)
- Bilateral calvarial and skull base fractures;
- Comminuted left orbital fractures;
- Left Le Fort I/II/III maxillary fractures;
- A comminuted left maxillary fracture involving the left and right hard palate with a mobile palate segment;
- Bilateral comminuted, displaced, open mandibular body fractures;
- Bilateral comminuted nasal fractures.
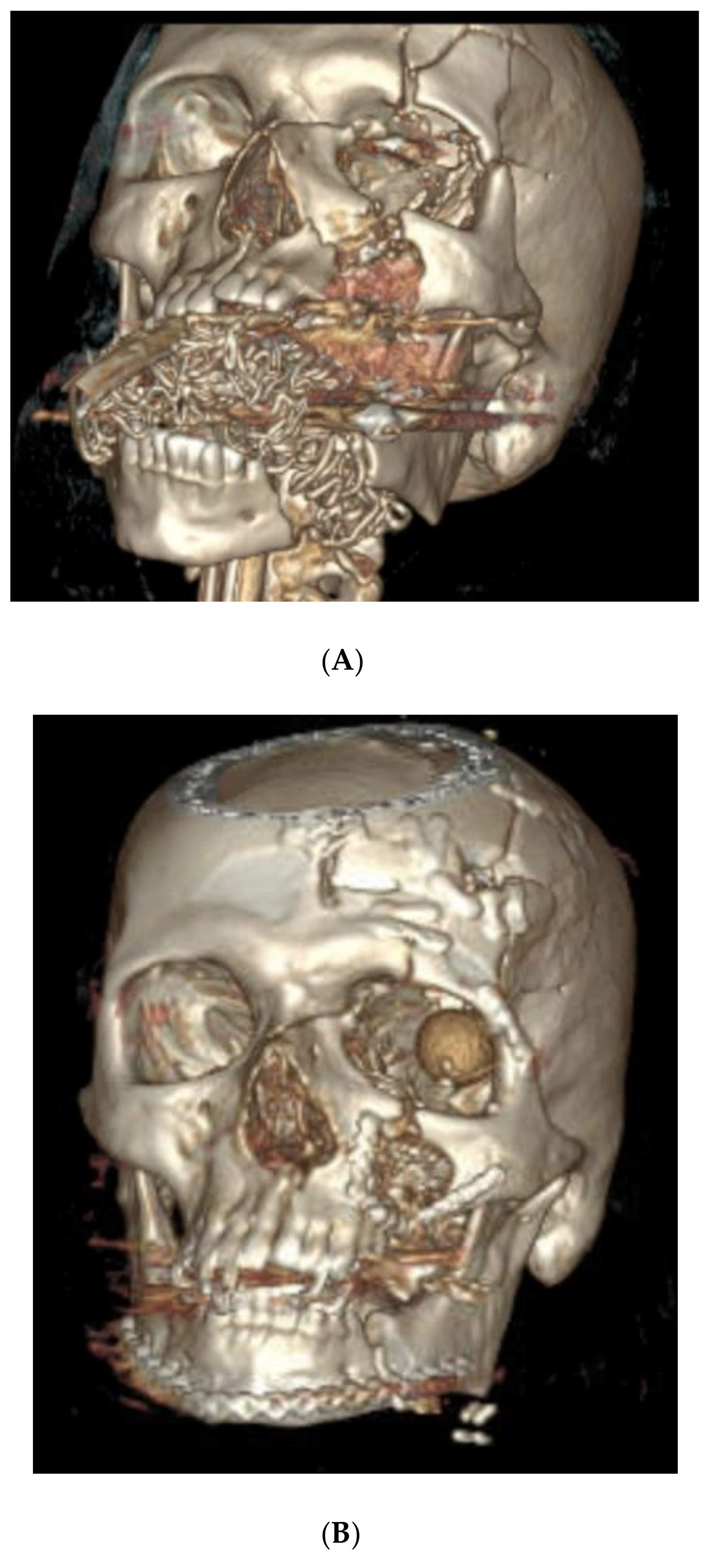
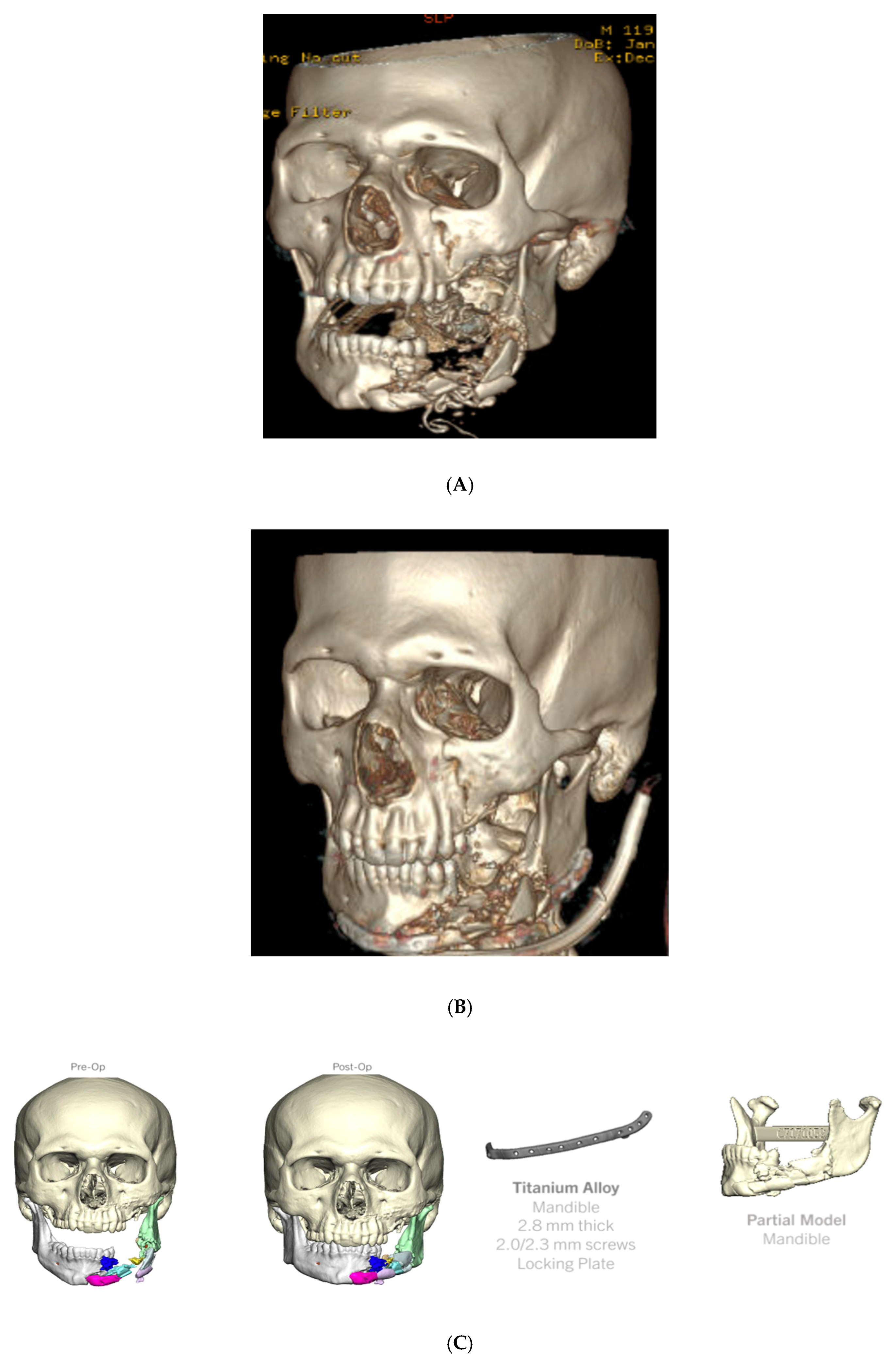
4.3. Case 3 (Patient 3D Model, Occlusal Splint, 3D Printed Plate)
- Left orbital floor and lateral orbital rim fractures;
- Comminuted maxillary fractures with involvement of the hard palate and retained bullet fragments in the maxillary sinus;
- An extensively comminuted open fracture of the left mandibular body extending to the parasymphysis;
- Extensive soft tissue and dental injuries with retained ballistic fragments.
5. Indications to Consider VSP When Treating Acute Facial Trauma
- VSP can be used to virtually assess and restore occlusion when comminuted panfacial injuries involve both the midface and mandible, especially when a symphyseal mandible fracture is present that can lead to unintentional facial widening during fracture reduction. Three-dimensional models will assist with plate bending and fracture reduction. Occlusal splints can help the surgeon achieve stable maxillomandibular fixation in these patients intraoperatively to guide fracture reduction.
- Palatal split fractures make restoration of stable occlusion extremely difficult. VSP-derived occlusal splints can be used both intraoperatively and, if needed, postoperatively to help reduce and/or stabilize these fractures.
- When ballistic trauma results in excessive comminution and pulverization of bone, VSP can be used to assist with fracture reduction and, if needed, for the production of custom implants that span the areas of bone loss.
- Limited or poor dentition makes traditional maxillomandibular fixation techniques ineffective as a guide to fracture reduction. The virtual assessment of both occlusion and fracture reduction using VSP is valuable in this setting. An occlusal split can also make stable maxillomandibular fixation possible in many cases.
6. Discussion
- Following a virtual planning session, surgeons may have a better understanding of how bone fragments will be reduced prior to surgery.
- Custom occlusal splints and plates may guide bony reduction insofar as the surgeon will not be relying solely on the alignment of partially visible fracture lines and/or sometimes unstable occlusion during the procedure.
- Bending plates to a 3D model produced with VSP is easier than trying to bend plates to the patient via the limited access provided by surgical approaches.
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tang, N.S.J.; Ahmadi, I.; Ramakrishnan, A. Virtual surgical planning in fibula free flap head and neck reconstruction: A systematic review and meta-analysis. J. Plast. Reconstr. Aesthetic Surg. 2019, 72, 1465–1477. [Google Scholar] [CrossRef] [PubMed]
- Barr, M.L.; Haveles, C.S.; Rezzadeh, K.S.; Nolan, I.T.; Castro, R.; Lee, J.C.; Steinbacher, D.; Pfaff, M.J. Virtual Surgical Planning for Mandibular Reconstruction With the Fibula Free Flap: A Systematic Review and Meta-analysis. Ann. Plast. Surg. 2020, 84, 117–122. [Google Scholar] [CrossRef]
- Gray, R.; Gougoutas, A.; Nguyen, V.; Taylor, J.; Bastidas, N. Use of three-dimensional, CAD/CAM-assisted, virtual surgical simulation and planning in the pediatric craniofacial population. Int. J. Pediatr. Otorhinolaryngol. 2017, 97, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Saad, A.; Winters, R.; Wise, M.W.; Dupin, C.L.; St Hilaire, H. Virtual surgical planning in complex composite maxillofacial reconstruction. Plast. Reconstr. Surg. 2013, 132, 626–633. [Google Scholar] [CrossRef]
- Alkaabi, S.; Maningky, M.; Helder, M.N.; Alsabri, G. Virtual and traditional surgical planning in orthognathic surgery—Systematic review and meta-analysis. Br. J. Oral. Maxillofac. Surg. 2022, 60, 1184–1191. [Google Scholar] [CrossRef]
- Alkhayer, A.; Piffkó, J.; Lippold, C.; Segatto, E. Accuracy of virtual planning in orthognathic surgery: A systematic review. Head Face Med. 2020, 16, 34. [Google Scholar] [CrossRef] [PubMed]
- Starch-Jensen, T.; Hernández-Alfaro, F.; Kesmez, Ö.; Gorgis, R.; Valls-Ontañón, A. Accuracy of Orthognathic Surgical Planning using Three-dimensional Virtual Techniques compared with Conventional Two-dimensional Techniques: A Systematic Review. J. Oral Maxillofac. Res. 2023, 14, e1. [Google Scholar] [CrossRef] [PubMed]
- Farrell, B.B.; Franco, P.B.; Tucker, M.R. Virtual surgical planning in orthognathic surgery. Oral Maxillofac. Surg. Clin. N. Am. 2014, 26, 459–473. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.; Vanderbeek, C.; Herford, A.S.; Thakker, J.S. Use of Virtual Surgical Planning and Virtual Dataset With Intraoperative Navigation to Guide Revision of Complex Facial Fractures: A Case Report. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2019, 77, 790.e1–790.e17. [Google Scholar] [CrossRef] [PubMed]
- Thakker, J.S.; Pace, M.; Lowe, I.; Jung, P.; Herford, A.S. Virtual Surgical Planning in Maxillofacial Trauma. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2019, 27, 143–155. [Google Scholar] [CrossRef]
- Castro-Núñez, J.; Van Sickels, J.E. Secondary reconstruction of maxillofacial trauma. Curr. Opin. Otolaryngol. Head Neck Surg. 2017, 25, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Ding, Q.; Fu, Z.Z.; Yue, J.; Xu, Y.X.; Xue, L.F.; Xiao, W.L. Virtual Surgical Planning and Three-Dimensional Printing to Aid the Anatomical Reduction of an Old Malunited Fracture of the Mandible. J. Craniofacial Surg. 2021, 32, e647–e649. [Google Scholar] [CrossRef] [PubMed]
- Day, K.M.; Phillips, P.M.; Sargent, L.A. Correction of a Posttraumatic Orbital Deformity Using Three-Dimensional Modeling, Virtual Surgical Planning with Computer-Assisted Design, and Three-Dimensional Printing of Custom Implants. Craniomaxillofacial Trauma Reconstr. 2018, 11, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Liokatis, P.; Malenova, Y.; Fegg, F.; Haidari, S.; Probst, M.; Boskov, M.; Cornelius, C.; Troeltzsch, M.; Probst, F. Digital planning and individual implants for secondary reconstruction of midfacial deformities: A pilot study. Laryngoscope Investig. Otolaryngol. 2022, 7, 369–379. [Google Scholar] [CrossRef] [PubMed]
- Hussein, M.A.; Besher, A.; Saad, M.A.; Wilson, A.M. Versatility of Hard Occlusal Splints in Optimizing Outcomes in Patients with Old Pan-facial Fractures. Plast. Reconstr. Surg. Glob. Open 2021, 9, E3855. [Google Scholar] [CrossRef]
- Longeac, M.; Depeyre, A.; Pereira, B.; Barthelemy, I.; Pham Dang, N. Virtual surgical planning and three-dimensional printing for the treatment of comminuted zygomaticomaxillary complex fracture. J. Stomatol. Oral Maxillofac. Surg. 2021, 122, 386–390. [Google Scholar] [CrossRef] [PubMed]
- Dubron, K.; Van Camp, P.; Jacobs, R.; Politis, C.; Shaheen, E. Accuracy of virtual planning and intraoperative navigation in zygomaticomaxillary complex fractures: A systematic review. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, e841–e848. [Google Scholar] [CrossRef]
- Abdul Lateef Hassan, T.; Abbood Mohammed, D. Virtual Surgical Planning and 3-Dimensional Printing for the Treatment of Zygomaticomaxillary Complex and/or Orbital Fracture. J. Craniofacial Surg. 2023, 34, e218–e222. [Google Scholar] [CrossRef] [PubMed]
- Novelli, G.; Tonellini, G.; Mazzoleni, F.; Bozzetti, A.; Sozzi, D. Virtual surgery simulation in orbital wall reconstruction: Integration of surgical navigation and stereolithographic models. J. Cranio-Maxillofacial Surg. 2014, 42, 2025–2034. [Google Scholar] [CrossRef] [PubMed]
- Brito, N.M.d.S.O.; Soares, R.d.S.C.; Monteiro, E.L.T.; Martins, S.C.R.; Cavalcante, J.R.; Grempel, R.G.; Neto, J.A.d.O. Additive Manufacturing for Surgical Planning of Mandibular Fracture. Acta Stomatol. Croat. 2016, 50, 348–353. [Google Scholar] [CrossRef]
- Maloney, K.D.; Rutner, T. Virtual Surgical Planning and Hardware Fabrication Prior to Open Reduction and Internal Fixation of Atrophic Edentulous Mandible Fractures. Craniomaxillofacial Trauma Reconstr. 2019, 12, 156–162. [Google Scholar] [CrossRef]
- Castro-Núñez, J.; Shelton, J.M.; Snyder, S.; Sickels, J.V. Virtual Surgical Planning for the Management of Severe Atrophic Mandible Fractures. Craniomaxillofacial Trauma Reconstr. 2018, 11, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Egger, J.; Wallner, J.; Gall, M.; Chen, X.; Schwenzer-Zimmerer, K.; Reinbacher, K.; Schmalstieg, D. Computer-aided position planning of miniplates to treat facial bone defects. PLoS ONE 2017, 12, e0182839. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.; Lock, I.B.; Fan, C.K.B.; Maduekwe, U.; Ha, M.M.M.; Rasko, Y.; Grant, M.P.; Nam, A.J.; Steinberg, J.P.; Liang, F. Many Moving Pieces: Virtual Preoperative Surgical Planning for Traumatic Occlusal Splints. J. Craniofacial Surg. 2022, 33, 1037–1041. [Google Scholar] [CrossRef]
- Koenig, Z.A.; Lokant, B.T.; Weaver, S.; Brooke, S.M.; Uygur, H.S. Surgical Guide Splint Fabrication via Virtual Surgical Planning for Complex Mandible Fractures in the Trauma Setting. J. Craniofacial Surg. 2023, 35, 649–651. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Zhang, C.; Wu, J.; Xu, X.; Zhang, Y.; Zhang, S. Three-Dimensional Printed Customized Surgical Guides for the Precise Correction of Complex Midfacial Post-Traumatic Deformities. J. Craniofacial Surg. 2022, 33, 1150–1153. [Google Scholar] [CrossRef] [PubMed]
- Velarde, K.; Cafino, R.; Isla, A.; Ty, K.M.; Palmer, X.-L.; Potter, L.; Nadorra, L.; Pueblos, L.V.; Velasco, L.C. Virtual surgical planning in craniomaxillofacial surgery: A structured review. Comput. Assist. Surg. 2023, 28, 2271160. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.; Botros, A.; Henriquez, O.A. Applications of Preoperative and Intraoperative Technologies for Complex Primary and Secondary Facial Trauma Reconstruction. Otolaryngol. Clin. N. Am. 2023, 56, 1125–1136. [Google Scholar] [CrossRef] [PubMed]
- Zeiderman, M.R.; Pu, L.L.Q. Contemporary reconstruction after complex facial trauma. Burns Trauma 2020, 8, tkaa003. [Google Scholar] [CrossRef]
- Marschall, J.S.; Dutra, V.; Flint, R.L.; Kushner, G.M.; Alpert, B.; Scarfe, W.; Azevedo, B. In-House Digital Workflow for the Management of Acute Mandible Fractures. J. Oral. Maxillofac. Surg. 2019, 77, 2084.e1–2084.e9. [Google Scholar] [CrossRef]
- Knudson, S.A.; Day, K.M.; Kelley, P.; Padilla, P.; Collier, I.X.; Henry, S.; Harshbarger, R.; Combs, P. Same-Admission Microvascular Maxillofacial Ballistic Trauma Reconstruction Using Virtual Surgical Planning: A Case Series and Systematic Review. Craniomaxillofacial Trauma Reconstr. 2022, 15, 206–218. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.C.; Yang, C.H.; Chang, Y.J.; Wu, C.C.; Chang, L.R.; Lai, J.P. Repairing Facial Fractures with Interrupted Maxillary-mandibular Arches by Computer-assisted Reverse Planning Model Surgery. Plast. Reconstr. Surg. Glob. Open 2022, 10, e4149. [Google Scholar] [CrossRef]
- Wu, B.; Lv, K. Control of Mandibular Width With 3D Printed Occlusal Splint in Children With Multiple Mandibular Fractures. J. Craniofacial Surg. 2023, 34, e582–e584. [Google Scholar] [CrossRef]
- Sharaf, B.A.; Morris, J.M.; Kuruoglu, D. EPPOCRATIS: A Point-of-Care Utilization of Virtual Surgical Planning and Three-Dimensional Printing for the Management of Acute Craniomaxillofacial Trauma. J. Clin. Med. 2021, 10, 5640. [Google Scholar] [CrossRef] [PubMed]
- Khatib, B.; Gelesko, S.; Amundson, M.; Cheng, A.; Patel, A.; Bui, T.; Dierks, E.J.; Bell, R.B. Updates in Management of Craniomaxillofacial Gunshot Wounds and Reconstruction of the Mandible. Oral Maxillofac. Surg. Clin. N. Am. 2021, 33, 359–372. [Google Scholar] [CrossRef] [PubMed]
- Cho, R.Y.; Byun, S.H.; Park, S.Y.; On, S.W.; Kim, J.C.; Yang, B.E. Patient-specific plates for facial fracture surgery: A retrospective case series. J. Dent. 2023, 137, 104650. [Google Scholar] [CrossRef] [PubMed]
- Kozakiewicz, M.; Elgalal, M.; Loba, P.; Komuński, P.; Arkuszewski, P.; Broniarczyk-Loba, A.; Stefańczyk, L. Clinical application of 3D pre-bent titanium implants for orbital floor fractures. J. Cranio-Maxillofacial Surg. 2009, 37, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.T.; Chen, C.H.; Wang, P.F.; Lin, C.L. Development of a novel anatomical thin titanium mesh plate with reduction guidance and fixation function for Asian zygomatic-orbitomaxillary complex fracture. J. Cranio-Maxillofacial Surg. 2018, 46, 547–557. [Google Scholar] [CrossRef]
- Ha, S.H.; Choi, J.Y. Restoration of Facial Bone Defect using Patient-Specific Implant. J. Craniofacial Surg. 2022, 33, 2063–2066. [Google Scholar] [CrossRef]
- Lim, H.K.; Choi, Y.J.; Choi, W.C.; Song, I.S.; Lee, U.L. Reconstruction of maxillofacial bone defects using patient-specific long-lasting titanium implants. Sci. Rep. 2022, 12, 7538. [Google Scholar] [CrossRef] [PubMed]
- Schreurs, R.; Klop, C.; Gooris, P.J.J.; Maal, T.J.J.; Becking, A.G.; Dubois, L. Critical appraisal of patient-specific implants for secondary post-traumatic orbital reconstruction. Int. J. Oral Maxillofac. Surg. 2022, 51, 790–798. [Google Scholar] [CrossRef] [PubMed]
- Mendez, B.M.; Chiodo, M.V.; Patel, P.A. Customized “In-Office” Three-Dimensional Printing for Virtual Surgical Planning in Craniofacial Surgery. J. Craniofacial Surg. 2015, 26, 1584–1586. [Google Scholar] [CrossRef] [PubMed]
- Maglitto, F.; Orabona, G.D.; Committeri, U.; Salzano, G.; De Fazio, G.R.; Vaira, L.A.; Abbate, V.; Bonavolontà, P.; Piombino, P.; Califano, L. Virtual Surgical Planning and the “In-House” Rapid Prototyping Technique in Maxillofacial Surgery: The Current Situation and Future Perspectives. Appl. Sci. 2021, 11, 1009. [Google Scholar] [CrossRef]
- Radabaugh, J.P.; Zhang, P.; Wang, D.; Lin, P.L.Y.; Shelton, J.; Liau, J.Y.; CunninghamJr, L.L.; Gal, T.J. Barriers to Repair in Maxillofacial Trauma. JAMA Facial Plast. Surg. 2016, 18, 177–182. [Google Scholar] [CrossRef]
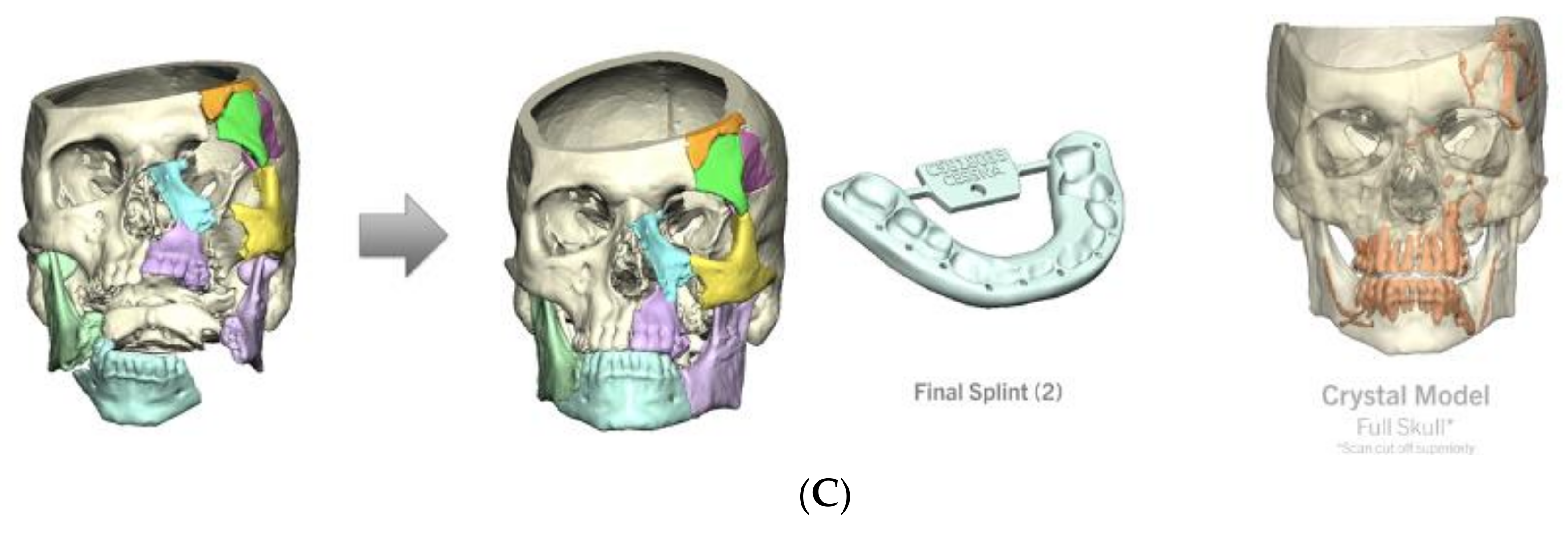
| Age at Surgery * (Years). | 38 (range 18–72) |
| Male Gender (n) | 10 |
| Mechanism (n) | |
| GSW | 6 |
| MVC | 2 |
| GLF | 1 |
| Occupational | 1 |
| VSP Used (n) | |
| Occlusal splint | 7 |
| 3D printed surgical plate | 4 |
| Patient 3D model | 4 |
| Injuries (n) | |
| Mandibular fracture | 8 |
| Palatal fracture | 6 |
| LeFort I | 4 |
| LeFort II | 2 |
| LeFort III | 2 |
| Orbital fracture | 4 |
| NOE | 3 |
| ZMC fracture | 2 |
| Frontal sinus fracture | 2 |
| Consult to OR Time * (days) | 8.6 (range 5–13) |
| Length of Surgery * (minutes) | 276 (range 130–450) |
| Complication Rate | 70% |
| Length of Follow-up & (days) | 370 (range 33–1171) |
| Age | Etiology | Facial Fractures | Other Injuries | VSP Services | Consult to OR Time (Days) | Length of Surgery (Minutes) | Postoperative Complications and Interventions | Length of Follow-Up (Days) |
|---|---|---|---|---|---|---|---|---|
| 27 | GSW | Mandibular fracture (complex) LeFort II LeFort III Left orbital fracture (two-wall) Bilateral NOE | None | Pre-contoured plate (left mandibular ramus) | 9 | 450 | Oroantral fistula Necrotic maxillary and mandibular bone Midface reconstruction with fibula free flap | 1171 |
| 69 | Occupational | LeFort I Maxillary fracture (palate split) | Globe rupture | Occlusal splint Pre-contoured plate (maxillary spine) | 8 | 281 | Nasal obstruction due to synechiae and bone fragment To be addressed in OR | 296 |
| 34 | GSW | Mandibular fracture Maxillary fracture (complex) LeFort I Frontal sinus fracture | Orbital foreign body Eyelid lacerations | Occlusal splint 3D model (mandible and maxilla) | 7 | 209 | None | 33 |
| 33 | GSW | Mandibular fracture (complex) Maxillary fracture (complex, palate split) Left orbital fracture (two-wall) Left NOE Left ZMC | Eyelid lacerations | Occlusal splint | 7 | 299 | Osteonecrosis of maxilla Attempted fibula free flap, failed intraoperatively due to carotid injury; treated with obturator | 500 |
| 38 | MVC | LeFort I LeFort II LeFort III Bilateral orbital fractures (three-wall) Left NOE | Severe intracranial injury Left retrobulbar hematoma Rib fractures and pulmonary contusions Right hip fracture Multiple extremity fractures | Pre-contoured plates (zygomatico-frontal, infraorbital rim, LeFort I) | 11 | 349 | None | 400 |
| 31 | MVC | Mandibular fracture (complex) | Rib fractures and pulmonary contusions Femur fracture Spinal process fracture | Occlusal splint 3D model (mandible) | 9 | 209 | Orocutaneous fistula (intraoral to submental) Necrotic exposed mandible Bone and soft tissue debrided in OR | 417 |
| 72 | GSW | Mandibular fracture (complex) Maxillary fracture (complex, palate split) Left orbital fracture Left ZMC | Severe intracranial injury Left globe injury | Occlusal splint | 9 | 433 | None | 48 |
| 23 | GSW | Mandibular fracture (complex) Maxillary fracture (complex, palate split) | None | Occlusal splint Pre-contoured plate (mandible) 3D model (mandible) | 13 | 130 | Palpable bony overgrowth Loose screws All hardware removed in OR, prominent areas of bone drilled down; postoperative wound infection, treated medically | 571 |
| 41 | GSW | Mandibular fracture (complex) | None | 3D model (mandible) | 8 | 221 | Orocutaneous fistula Treated medically | 341 |
| 18 | GLF | Mandibular fracture (simple) Maxillary fracture (palatal split) LeFort I | None | Occlusal splint | 5 | 175 | Loose plate (palate) Removed in OR | 110 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singerman, K.W.; Morisada, M.V.; Kriet, J.D.; Flynn, J.P.; Humphrey, C.D. Virtual Surgical Planning for Management of Acute Maxillofacial Trauma. Craniomaxillofac. Trauma Reconstr. 2025, 18, 18. https://doi.org/10.3390/cmtr18010018
Singerman KW, Morisada MV, Kriet JD, Flynn JP, Humphrey CD. Virtual Surgical Planning for Management of Acute Maxillofacial Trauma. Craniomaxillofacial Trauma & Reconstruction. 2025; 18(1):18. https://doi.org/10.3390/cmtr18010018
Chicago/Turabian StyleSingerman, Kyle W., Megan V. Morisada, J. David Kriet, John P. Flynn, and Clinton D. Humphrey. 2025. "Virtual Surgical Planning for Management of Acute Maxillofacial Trauma" Craniomaxillofacial Trauma & Reconstruction 18, no. 1: 18. https://doi.org/10.3390/cmtr18010018
APA StyleSingerman, K. W., Morisada, M. V., Kriet, J. D., Flynn, J. P., & Humphrey, C. D. (2025). Virtual Surgical Planning for Management of Acute Maxillofacial Trauma. Craniomaxillofacial Trauma & Reconstruction, 18(1), 18. https://doi.org/10.3390/cmtr18010018






