Frontal Sinus Fractures and Traumatic Brain Injury: Predictors of Mortality in Surgical Management
Abstract
Introduction
Methods
Study Design
Variables
Sample Size
Statistical Analysis
Results
Sociodemographic Characteristics
Trauma Characteristics
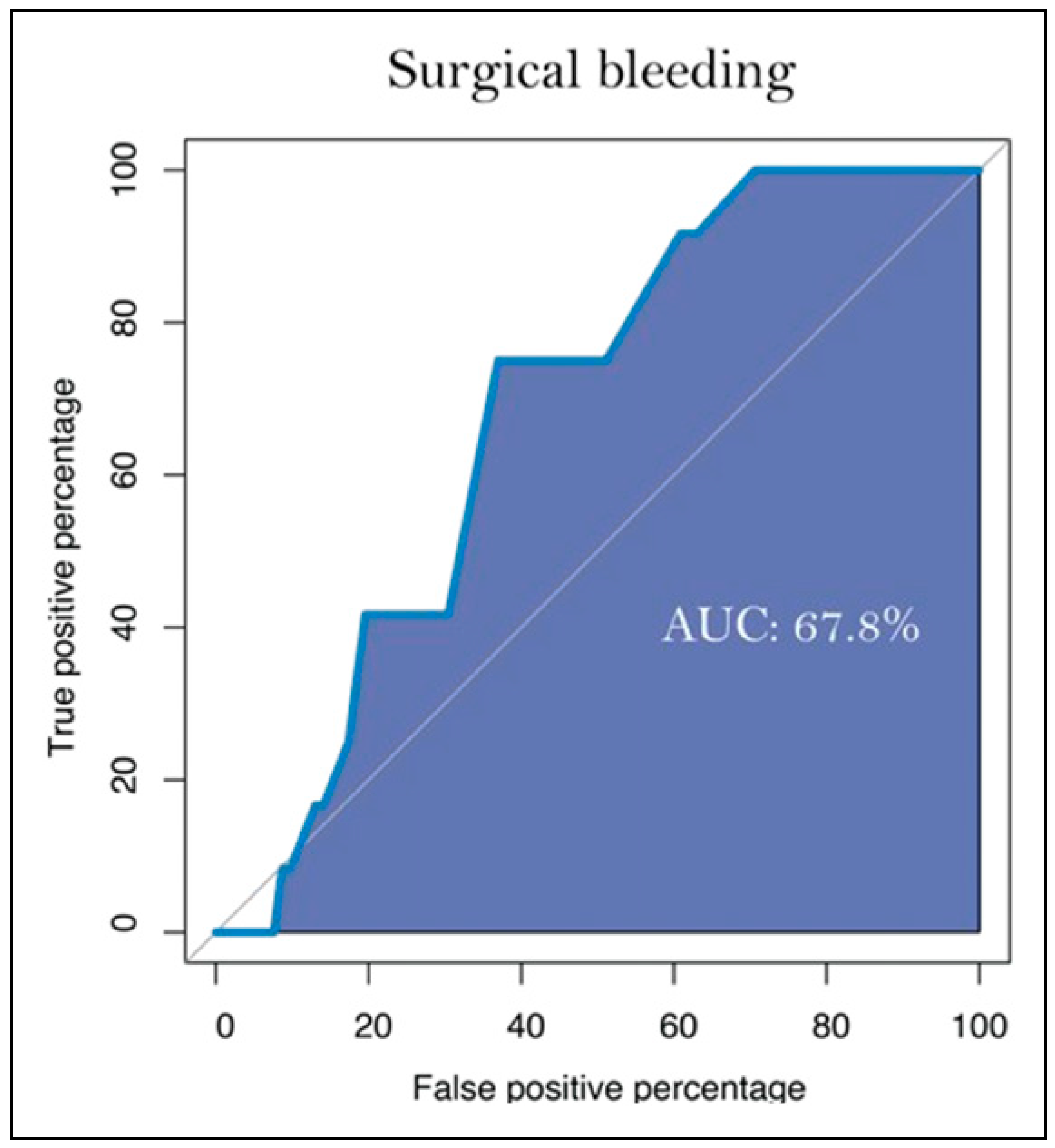
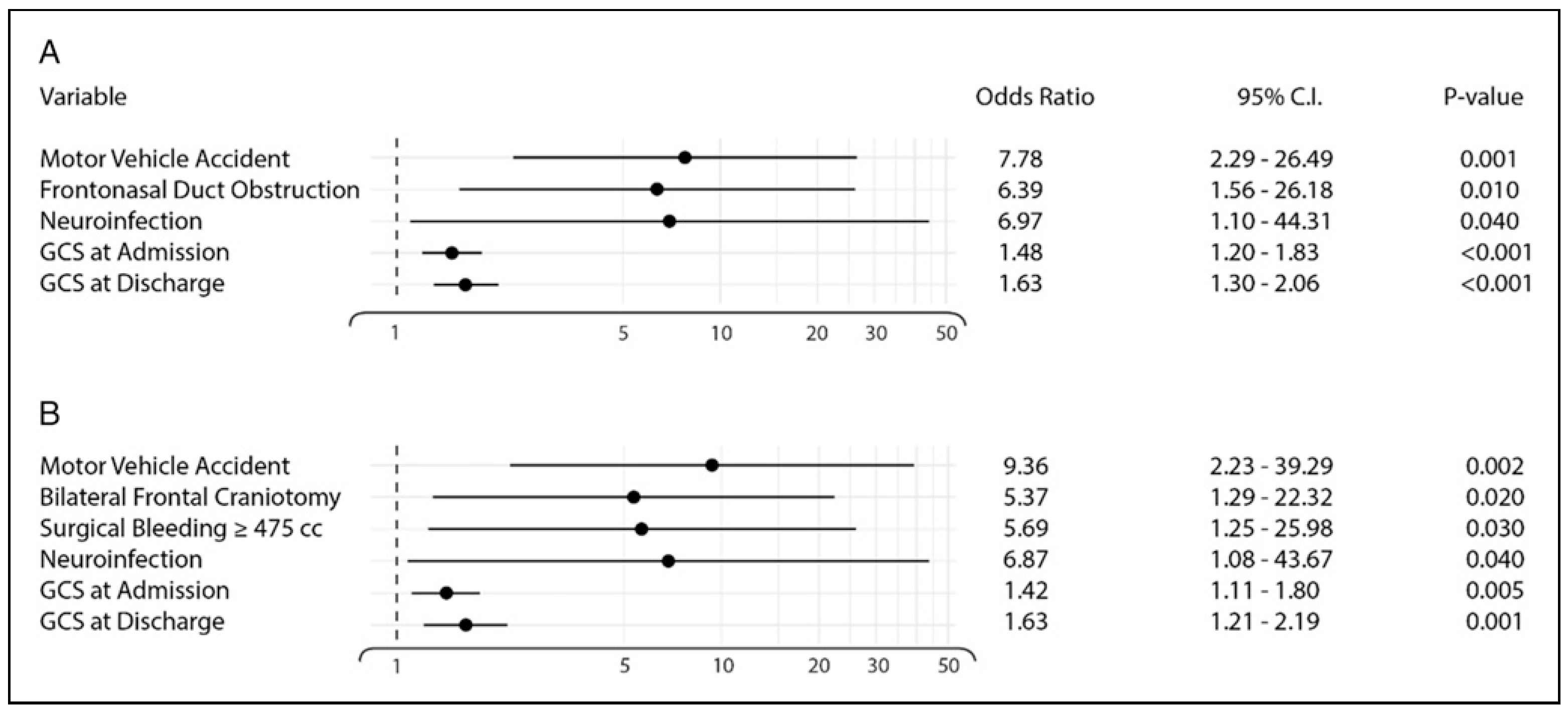
Intervention Characteristics
Discussion
Conclusions
Author’s Notes
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Avello Canisto, F.; Avello Peragallo, A. Nueva clasificación de las fracturas del tercio superior facial: Consideraciones anatomo-quiru’rgicas. An. Fac. Med. 2013, 4, 272–277. [Google Scholar] [CrossRef][Green Version]
- Brasileiro, B.F.; Passeri, L.A. Epidemiological analysis of maxillofacial fractures in Brazil: A 5-year prospective study. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2006, 1, 28–34. [Google Scholar] [CrossRef] [PubMed]
- MarKnez-Villalobos Castillo, S. Osteos’ıntesis Craniomaxilofacial; Ergon: Madrid, Spain, 2002. [Google Scholar]
- El Khatib, K.; Danino, A.; Malka, G. The frontal sinus: A culprit or a victim. A review of 40 cases. J. Cranio-Maxillo-Fac. Surg. 2004, 5, 314–317. [Google Scholar] [CrossRef]
- Morales-Olivera Mart’ın, J.; Herna’ndez-Ordoñez, R.; Pacheco-López, R. “Estudio epidemiológico del trauma facial en el servicio de cirug’ıa pla’stica y reconstructiva del hospital general «Dr. Rube’n Leñero» en la Ciudad de Me’xico. Incidencia de 5 años”. Cirug’ıa Pla’stica. 2017, 3, 119–124. [Google Scholar]
- Avello Canisto, F.; Saavedra Leveau, J.; Pasache Jua’rez, L.; Iwaki Cha’vez, R.; Nu’ñez Castañeda, J.; Robles Hermenegildo, M. Fracturas del tercio superior facial: Experiencia en el Servicio de Cirug’ıa de Cabeza, Cuello y Ma’xilo-Facial del Hospital Nacional Dos de Mayo, 1999–2009. An Fac Med. 2014, 75, 319–322. [Google Scholar] [CrossRef][Green Version]
- Avello, F. Epidemiolog’ıa y clasificación de las fracturas ma’xilo-faciales. Hosp. Nac. Dos de Mayo. Tesis de especialidad en Cirug’ıa de Cabeza, Cuello y Ma’xilo-Facial; Universidad Nacional Mayor de San Marcos, Facultad de Medicina: Lima, Peru, 2002. [Google Scholar]
- Manolidis, S.; Hollier, L.H., Jr. Management of frontal sinus fractures. Plast. Reconstr. Surg. 2007, 120 (Suppl. 7), 32S–48S. [Google Scholar] [CrossRef]
- Lin, S.; Levin, L.; Goldman, S.; Peled, M. Dento-alveolar and maxillofacial injuries-a retrospective study from a level 1 trauma center in Israel. Dent. Traumatol. 2007, 23, 155–157. [Google Scholar] [CrossRef]
- Canisto, F.A. Clasificación de las Fracturas Faciales en el Servicio de Cirug’ıa de Cabeza, Cuello y Ma’xilo-Facial del Hospital Nacional “Dos de Mayo”, 1999–2014. Revista Me’dica Carriónica. 2019, 5. [Google Scholar]
- World Health Organization. In Fractures of Skull and Facial Bone. International Statistical Classification of Diseases and Related Health Problems 10th Revision; Available online: https://icd.who.int/browse10/2019/en; World Health Organization: Geneva, Switzerland, 2019.
- IBM Corp. IBM SPSS Statistics for Windows, Version 23.0; IBM Corp: Armonk, NY, USA, 2015. [Google Scholar]
- Stephen, E.; Metzinger, M.; Guerra, A.; Eloy, R. Frontal sinus fractures: Management guidelines. Facial Plast. Surg. 2005, 21, 199–205. [Google Scholar]
- Hachl, O.; Tuli, T.; Schwabegger, A.; Gassner, R. Maxillofacial trauma due to work-related accidents. Nt J. Oral. Maxillofac. Surg. 2002, 31, 90–93. [Google Scholar] [CrossRef]
- Chan, J.; Putnam, M.; Feustel, P.; Koltai, P. The age dependent relationship between facial fractures and Skull fractures. Int. J. Ped Orl. 2004, 68, 877–881. [Google Scholar] [CrossRef]
- Gonza’lez, E.; Pedemonte, C.; Vargas, I.; et al. Fracturas facialesen un centro de referencia de traumatismos nivel I: Estudio descriptivo. Rev. Española Cirug’ıa Oral. Maxilofac. 2015, 37, 65–70. [Google Scholar] [CrossRef]
- Torres-Criollo, L.; Diaz, P.; Mancheno-Benalcazar, K.; et al. Management of cranial fractures with sinking Manejo de fracturas creaneales con hundimiento. Arch. Venez. Farmacol. Ter. 2021, 39, 760–765. [Google Scholar]
- Ioannides, C.; Freihofer, H.P.; Vrieus, J.; Friens, J. Fractures of the frontal sinus: A rationale of treatment. Br. J. Plast. Surg. 1993, 3, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Sataloff, R.T.; Sariego, J.; Myers, D.L.; Richter, H.J. Surgical management of the frontal sinus. Neurosurgery. 1984, 15, 593–596. [Google Scholar] [CrossRef]
- Swinson, B.D.; Jerjes, W.; Thompson, G. Current practice in the management of frontal sinus fractures. J. Laryngol. Otol. 2004, 12, 927–932. [Google Scholar] [CrossRef]
- Owens, M.; Klotch, D.W. Use of bone for obliteration of the nasofrontal duct with the osteoplastic flap: A cat model. Laryngoscope 1993, 103, 883–889. [Google Scholar] [CrossRef] [PubMed]
- Bell, R.B.; Dierks, E.J.; Brar, P.; Potter, J.K.; Potter, B.E. A protocol for the management of frontal sinus fractures emphasizing sinus preservation. J. Oral. Maxillofac. Surg. 2007, 5, 825–839. [Google Scholar] [CrossRef]
- Bhavana, K.; Kumar, R.; Keshri, A.; Aggarwal, S. Minimally invasive technique for repairing CSF leaks due to defects of posterior table of frontal sinus. J. Neurol. Surg. B Skull Base. 2014, 3, 183–186. [Google Scholar]
- Bellamy, J.L.; Molendijk, J.; Reddy, S.K.; et al. Severe infectious complications following frontal sinus fracture: The impact of operative delay and perioperative antibiotic use. Plast. Reconstr. Surg. 2013, 1, 154–162. [Google Scholar] [CrossRef]
- Pollock, R.A.; Hill JLJr Davenport, D.L.; Snow, D.C.; Vasconez, H.C. Cranialization in a cohort of 154 consecutive patients with frontal sinus fractures (1987–2007): Review and update of a compelling procedure in the selected patient. Ann. Plast. Surg. 2013, 1, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.A.; Tatum, S.A. Frontal sinus fractures: Evolving clinical considerations and surgical approaches. Craniomaxillofacial Trauma. Reconstr. 2019, 2, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Jing, X.L.; Luce, E. Frontal sinus fractures: Management and complications. Craniomaxillofacial Trauma. Reconstr. 2019, 3, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Montovani, J.C.; Nogueira, E.A.; Ferreira, F.D.; Lima Neto, A.C.; Nakajima, V. Surgery of frontal sinus fractures. Epidemiologic study and evaluation of techniques. Braz. J. Otorhinolaryngol. 2006, 2, 204–209. [Google Scholar] [CrossRef]
- Villafa’n-Quiroga, R.; Cienfuegos-Monroy, R.; Sierra-Mart’ınez, E. Fractures of the posterior wall of the frontal sinus: Nonsurgical management and complications. Cir. Cir. 2010, 5, 387–392. [Google Scholar]
- Rodr’ıguez-Perales, M.A.; Canul-Andrade, L.P.; Villagra-Siles, E. (Eds.) Tratamiento Quiru’rgico de las Fracturas del Seno Frontal; Anales de Otorrinolaringolog’ıa Mexicana: Merida, Mexico, 2004. [Google Scholar]
| Population Characteristics | Total Study Population (N = 150) |
|---|---|
| Age in years | 28.58 ± 16.55 |
| Gender | |
| Female | 25 (16.7%) |
| Male | 125 (83.3%) |
| Comorbidities | |
| Alcoholism | 78 (52%) |
| Smoking | 62 (41.3%) |
| Drug addiction | 31 (20.6%) |
| Obesity | 25 (16.6%) |
| Diabetes mellitus type 2 | 17 (11.3%) |
| Arterial hypertension | 20 (13.3%) |
| Others | 16 (10.6%) |
| Surgery characteristics | |
| Presurgical CSF fistula | 21 (14%) |
| Post-surgical CSF fistula | 6 (4%) |
| Type of intervention | |
| Conservative treatment | 45 (30%) |
| Bilateral frontal craniotomy | 52 (34.7%) |
| Unilateral frontal craniotomy | 17 (11.3%) |
| Squirlectomy and osteosynthesis | 33 (22%) |
| Material used | |
| Pericranium | 48 (30.9%) |
| Gelfoam | 32 (20.6%) |
| Bone wax | 32 (20.6%) |
| Muscle | 29 (18.7%) |
| Surgicel | 12 (7.7%) |
| Fascia | 1 (0.6%) |
| Fat | 1 (0.6%) |
| Glasgow at admission a | 14 (12–15) |
| Glasgow at discharge a | 15 (14–15) |
| Waiting days for surgery a | 1 (0–2) |
| Surgery waiting time (hours) a | 8 (4–17) |
| Operative bleeding (cc) a | 390 (155–600) |
| Duration of surgery (min) a | 240 (151.5–300) |
| Type of surgical wound performed | |
| Souter | 51 (48.6%) |
| Trauma flap | 15 (14%) |
| Bicoronal | 14 (13.3%) |
| Through original traumatic injury | 7 (6.6%) |
| Wound reopening | 6 (5.3%) |
| Italic S-shaped wound | 5 (4.6%) |
| Hemisauter | 5 (4.6%) |
| Horseshoe wound | 2 (2%) |
| Prophylactic antibiotics | |
| Amoxicillin | 80 (53.3%) |
| Cephalothin | 60 (40%) |
| Ceftriaxone | 41 (27.3%) |
| Clindamycin | 21 (14%) |
| Vancomycin | 1 (0.6%) |
| Prophylactic antimycotic | |
| Metronidazole | 1 (0.6%) |
| Complications | |
| Neuroinfection | 7 (4.6%) |
| Local wound infection | 5 (3.3%) |
| Soft tissue infection | 2 (1.3%) |
| Onset of infection after admission (days) a | 2.5 (2–3.75) |
| Fever after admission | 18 (12%) |
| Cisternostomy | 12 (8%) |
| Death | 15 (10%) |
| Days of hospital stay a | 9 (6–13.25) |
| Outpatient follow-up | 119 (79.3%) |
| Surgery Group | Control Group | |||
|---|---|---|---|---|
| Variable | N = 105 | N = 45 | p | |
| Male | 92 (87.6%) | 33 (73.3%) | 0.717 | |
| Age in years | 28.64 ± 15.8 | 28.45 ± 18.4 | 0.951 | |
| Comorbidities | ||||
| Diabetes mellitus type 2 | 13 (12.4%) | 4 (8.9%) | 0.536 | |
| High blood pressure | 11 (10.5%) | 9 (20%) | 0.116 | |
| Obesity | 20 (19%) | 5 (11.1%) | 0.232 | |
| Smoking | 51 (48.6%) | 11 (24.4%) | 0.006 | |
| Alcoholism | 57 (54.3%) | 20 (44.4%) | 0.269 | |
| Drug addiction | 26 (24.8%) | 5 (11.1%) | 0.058 | |
| Trauma mechanism | ||||
| Direct assault | 36 (34.3%) | 7 (15.6%) | 0.020 | |
| Automobile accident | 26 (24.8%) | 7 (15.6%) | 0.090 | |
| Motorcycle accident | 12 (11.4%) | 3 (6.7%) | 0.554 | |
| Fall from height | 12 (11.4%) | 17 (37.8%) | <0.001 | |
| Firearm | 3 (2.9%) | 2 (4.4%) | 1.00 | |
| Other | 16 (15.2%) | 9 (20%) | 0.473 | |
| CSF fistula pre-surgery | 17 (16.2%) | 4 (8.9%) | 0.238 | |
| Neurological focalization | 48 (45.7%) | 23 (52.3%) | 0.465 | |
| Glasgow | ||||
| Admission | 14 (12–15) | 14 (12.5–15) | 0.733 | |
| Discharge | 15 (14–15) | 15 (14.5–15) | 0.877 | |
| Involvement of tables | 0.129 | |||
| Internal | 6 (5.7%) | 6 (13.3%) | ||
| External | 34 (32.4%) | 18 (40%) | ||
| Both | 65 (61.9%) | 21 (46.7%) | ||
| Nasofrontal duct obstruction | 6 (5.7%) | 7 (15.6%) | 0.062 | |
| Type of hematoma | ||||
| Epidural | 36 (34.3%) | 10 (22.2%) | 0.142 | |
| Subdural | 18 (17.1%) | 10 (22.2%) | 0.464 | |
| Subarachnoid | 14 (13.3%) | 12 (26.7%) | 0.048 | |
| Parenchymal | 14 (13.3%) | 3 (6.7%) | 0.238 | |
| Contusion | 16 (15.2%) | 9 (20%) | 0.473 | |
| Pneumocephalus | 16 (15.2%) | 2 (4.4%) | 0.062 | |
| Complete displacement | 32 (30.8%) | 11 (26.2%) | 0.583 | |
| Laterality | 0.316 | |||
| Left | 45 (43.3%) | 16 (35.6%) | ||
| Right | 44 (42.3%) | 18 (40%) | ||
| Bilateral | 15 (14.4%) | 11 (24.4%) | ||
| Type of fracture | ||||
| Depressed | 62 (59.6%) | 6 (13.3%) | <0.001 | |
| Linear | 42 (40.4%) | 39 (86.7%) | <0.001 | |
| Labs at admission | ||||
| Hemoglobin | 14.1 (12.3–15.2) | 13.4 (12.1–14.4) | 0.165 | |
| Leukocytes | 14.6 (11.3–18) | 14.8 (11.7–18.5) | 0.626 | |
| Neutrophils | 11.4 (7.5–14.7) | 11 (8–15.4) | 0.916 | |
| Lymphocytes | 1.89 (1.14–2.89) | 1.8 (1.1–3.3) | 0.667 | |
| Platelets | 234 (183.5–285) | 245 (214.5–271.5) | 0.264 | |
| MPV | 7.87 (6.89–9) | 7.43 (6.6–8.3) | 0.075 | |
| Labs at discharge | ||||
| Hemoglobin | 11.9 (10.3–13.7) | 12.7 (11.4–13.9) | 0.062 | |
| Leukocytes | 12.1 (10–15.5) | 12.6 (10.9–16.2) | 0.448 | |
| Neutrophils | 9.8 (7.14–13.3) | 10.5 (7.68–13.8) | 0.409 | |
| Lymphocytes | 1.42 (1.1–2.16) | 1.3 (.8–1.8) | 0.143 | |
| Platelets | 223 (167–280) | 220 (183–254) | 0.936 | |
| MPV | 7.38 (6.57–8.29) | 7.29 (6.7–8.2) | 0.785 | |
| Days of hospital stay | 9 (7–14) | 6 (5–13) | 0.008 | |
© 2024 by the authors. The Author(s) 2024.
Share and Cite
Trejo, E.; García, P.; Ortega, D.A.; González, K.C.; Botello, E.; Hernández, G.; Morales, J.A.; Martínez, Á.R. Frontal Sinus Fractures and Traumatic Brain Injury: Predictors of Mortality in Surgical Management. Craniomaxillofac. Trauma Reconstr. 2024, 17, 314-323. https://doi.org/10.1177/19433875241229882
Trejo E, García P, Ortega DA, González KC, Botello E, Hernández G, Morales JA, Martínez ÁR. Frontal Sinus Fractures and Traumatic Brain Injury: Predictors of Mortality in Surgical Management. Craniomaxillofacial Trauma & Reconstruction. 2024; 17(4):314-323. https://doi.org/10.1177/19433875241229882
Chicago/Turabian StyleTrejo, Eduardo, Patricio García, Diego A. Ortega, Karla C. González, Edgar Botello, Gamaliel Hernández, Jesús A. Morales, and Ángel R. Martínez. 2024. "Frontal Sinus Fractures and Traumatic Brain Injury: Predictors of Mortality in Surgical Management" Craniomaxillofacial Trauma & Reconstruction 17, no. 4: 314-323. https://doi.org/10.1177/19433875241229882
APA StyleTrejo, E., García, P., Ortega, D. A., González, K. C., Botello, E., Hernández, G., Morales, J. A., & Martínez, Á. R. (2024). Frontal Sinus Fractures and Traumatic Brain Injury: Predictors of Mortality in Surgical Management. Craniomaxillofacial Trauma & Reconstruction, 17(4), 314-323. https://doi.org/10.1177/19433875241229882




