Introduction
Zygomaticomaxillary complex (ZMC) fractures are among the most common facial fracture patterns resulting from trauma to the craniofacial skeleton. Due to its prominent position at the center of the face, the zygoma is particularly vulnerable to injury, accounting for up to 40% of presenting maxillofacial fracture cases [
1]. The most common mechanisms are motor vehicle collisions and assault, with these injuries resulting in a spectrum of clinical severity [
2]. While obvious deformity of the cheek is the symptom most commonly cited by patients, ZMC fractures can also lead to diplopia secondary to enophthalmos and/or hypoglobus, trismus resulting from zygomatic arch impaction on the temporalis insertion at the mandibular coronoid process, and even possible entropion and epiphora from lower eyelid retraction in the setting of severe infraorbital rim displacement [
3,
4].
Although ZMC fractures are common and carry potentially significant clinical consequences, the management of these injuries can be murky at times. When the zygoma is severely displaced, patients demonstrate obvious facial deformity and the decision to operate is clear [
5,
6]. Unfortunately, these are the minority of cases, and patients most often present with moderately or even minimally displaced ZMC fractures. In these instances, a careful clinical exam combined with outpatient monitoring for symptom development are crucial in determining the need for surgery. However, facial swelling at initial presentation and during the first office visit can obscure subtle but critical changes in facial structure and may even account for patient-reported symptoms like trismus [
7,
8]. As a result, for patients with less clear-cut findings, the decision to operate is complex and is made based on the totality of information, which invariably leads to significant subjectivity and variability among surgeons.
CT scans remain the standard of care for the evaluation of ZMC fractures, and 3D rendering of the facial skeleton has been further shown to be useful in characterizing fracture topography [
7,
9]. However, little has been done to assess how CT findings relate to symptoms of ZMC fractures and subsequent need for surgery. In this study, the authors aim to identify key patient and imaging characteristics that are reliably associated with symptomatic ZMC fractures, with the goal of better understanding how degree and vector of fracture displacement relate to need for operative intervention.
Methods
Study Design
This study received approval from and complied with all policies and procedures outlined by the Institutional Review Board. A retrospective review of an institutional database (Research Electronic Data Capture) was performed on all patients who presented with zygomaticomaxillary complex fractures at a Level I Trauma Center between May 2015 and September 2020. Inclusion criteria included all patients presenting with CT-confirmed zygoma fractures.
Subjects for the study were defined as patients who experienced facial trauma with fractures along the zygomaticosphenoid (ZS), zygomaticofrontal (ZF), zygomaticomaxillary (ZM) and zygomaticotemporal (ZT) sutures. All included patients underwent high-quality CT imaging containing axial, sagittal, and coronal cross-sections with 3D facial skeletal reconstruction. Patients with concomitant midfacial fractures (eg, naso-orbitoethmoid and Le Fort pattern injuries) or inadequate imaging data were excluded from the study.
Data Collection
Clinical data was collected from the electronic medical record (EMR) for each patient. Relevant patient demographics, including age, gender, and primary insurance, were noted. Physical exam findings at initial presentation and at follow-up after either surgical intervention or 2 weeks from initial presentation were also recorded. Possible symptoms included: diplopia, enophthalmos, orbital dystopia, malar changes, facial asymmetry, trismus, palpable infraorbital rim step-off, infraorbital nerve paresthesia or anesthesia, and malocclusion. The decision to operate based on clinical findings at initial presentation was also determined from the clinical record.
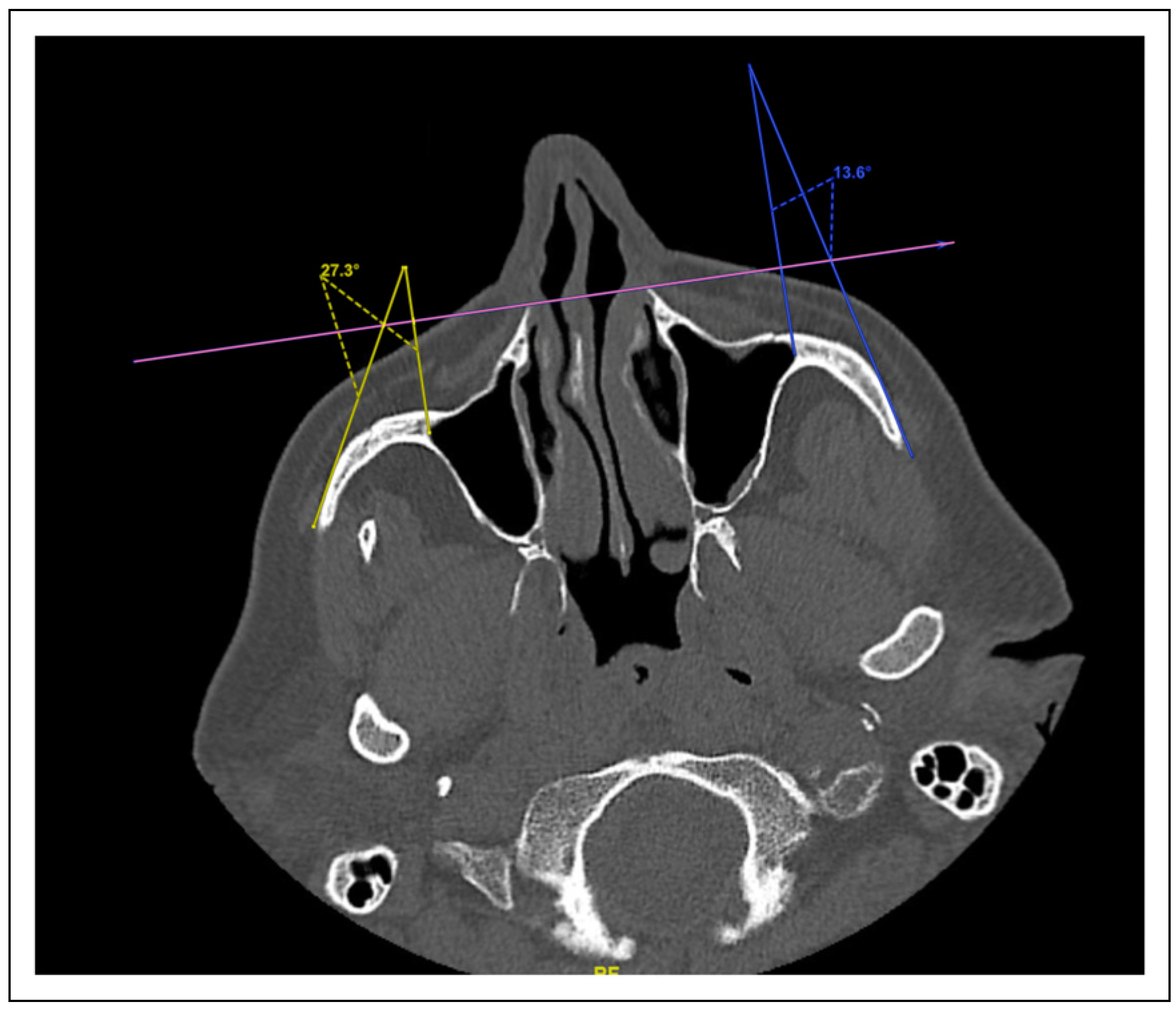
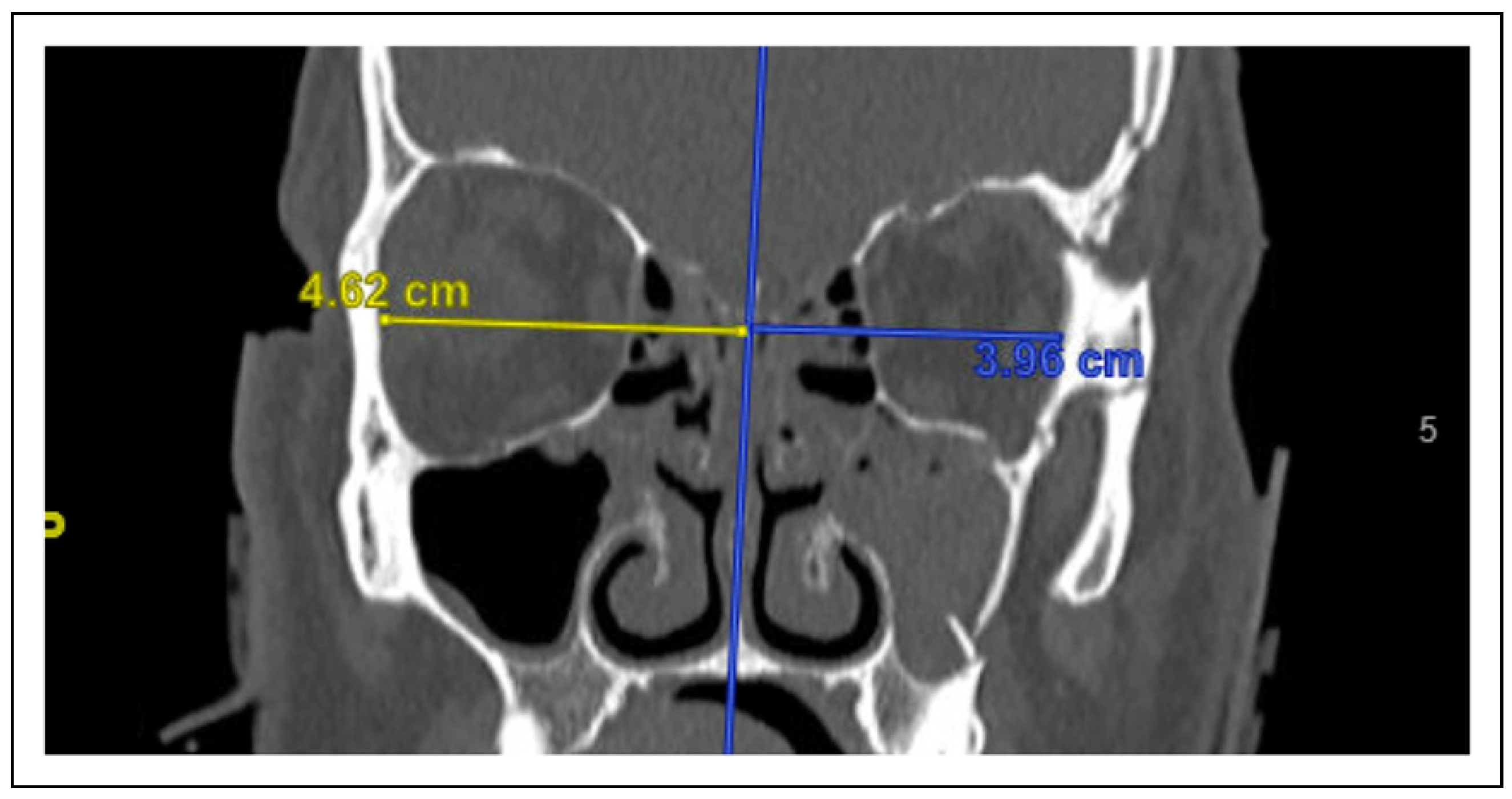
Computed tomography imaging characteristics of the fractures at initial presentation were similarly documented. Data elements measured in this study were (1) medial displacement or impaction of the lateral wall of the maxillary sinus (
Figure 1), (2) zygoma angle of rotation (
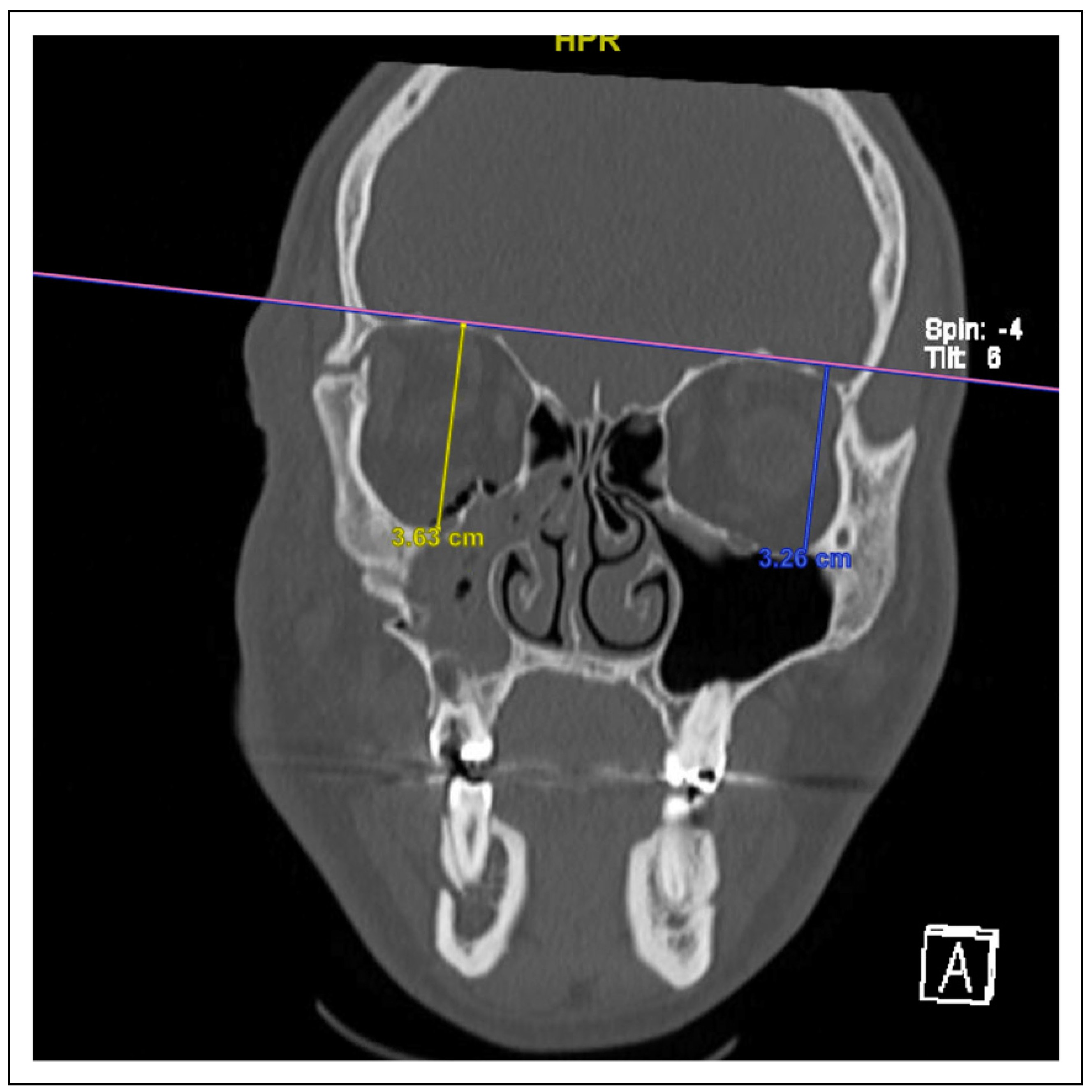
Figure 2), (3) anterior-posterior (AP) displacement of the zygoma (
Figure 3), (3) cranial-caudal or vertical displacement of the zygoma (
Figure 4), and (4) lateral-medial displacement (LM) of the zygoma (
Figure 5). For all vector measurements, the uninjured side served as an internal control.
Additionally, total absolute fracture displacement was taken as the sum of absolute displacements of each linear vector (lateral maxillary wall impaction, anterior-posterior displacement, vertical displacement, and lateral-medial displacement).
Statistical Analysis
Patient demographics and clinical symptomatology were reported using descriptive statistics. Chi-square tests were used to analyze statistical differences in operative indications among patients with various demographics, symptom presentations, and radiographic features. Logistic regression analysis was performed to determine relationships between radiographic characteristics and clinical symptomatology. Statistical significance was determined by a P-value of <.05. All statistical analyses were performed in R (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient Demographics
A total of 135 patients with ZMC fractures were initially identified using our institutional database. After individual chart review, 11 patients were excluded due to the presence of other midfacial fractures or excess trauma obscuring the ZMC fracture. An additional 29 patients were excluded due to poor image quality or missing CT scans.
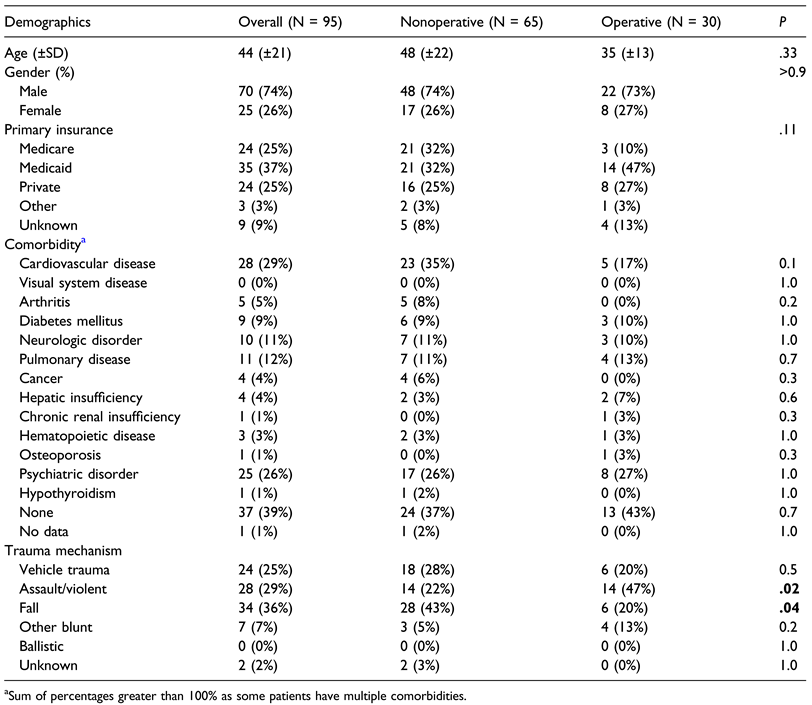
After this selection process, a total of 95 patients were included in our analysis. 65 patients (68%) had injuries that were deemed non-operative, while 30 patients (32%) were offered operative intervention. The average age of patients was 44 (±21) years old. The average age of patients with injuries deemed nonoperative was 48 (±22) years old, compared to 35 (±13) years old among patients deemed as operative. This difference was not statistically significant after controlling for various displacement vectors (
P = .33). Additionally, males comprised 74% and females 26% of the overall cohort. Males and females displayed no significant differences in proportions of fractures considered operative (
P > .90). Primary insurance also did not significantly influence indications for operation (
P = .11). Cardiovascular disease (29%), psychiatric disorders (26%), pulmonary disease (12%), and neurologic disorders (11%) were the most frequently noted comorbidities; notably, 39% of patients had no comorbidities. The most common trauma mechanisms were: vehicle trauma; assault or violence; falls; and other blunt objects. Assault or violent trauma mechanism was significantly more likely to be associated with indication for operative intervention (
P = .02), while falls were significantly more likely to result in non-operative injuries (
P = .04) (
Table 1).
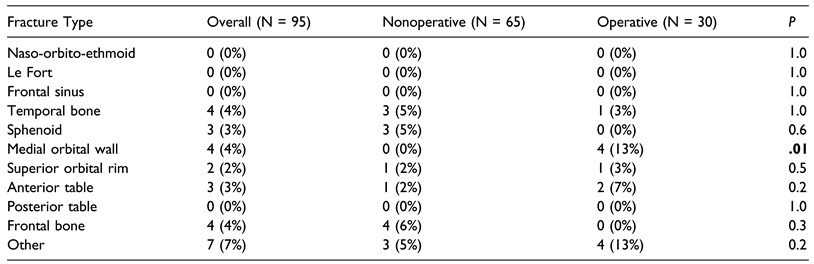
Thirteen patients with operative ZMC fractures presented with associated facial fractures, while 8 non-operative patients had associated facial fractures, including those of the: temporal bone; sphenoid; medial orbital wall; superior orbital rim; anterior table; posterior table, and frontal bone. Medial orbital wall fractures were significantly more likely to occur in patients with ZMC fractures indicating operative intervention (
P = .01). Of note, patients with concomitant midfacial fractures (eg, naso-orbito-ethmoid and Le Fort pattern injuries) were excluded from this study (
Table 2).
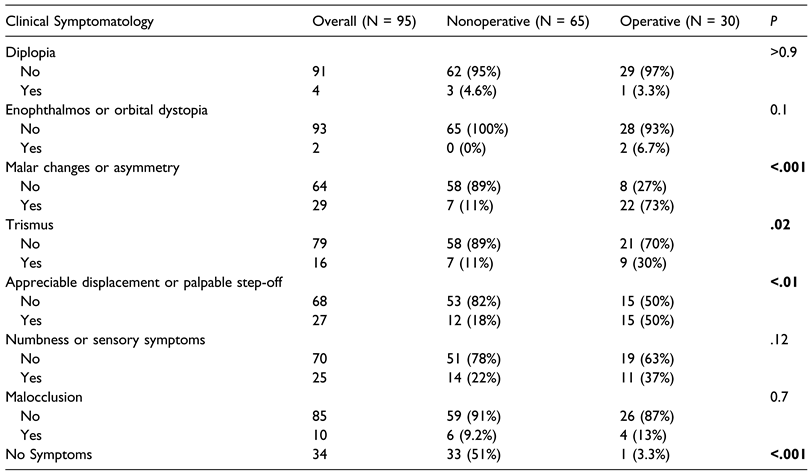
Clinical Symptomatology at Presentation
Sixty-four (67%) patients experienced symptoms that are commonly considered in the evaluation of operative status. These symptoms included: malar displacement (31%), infraorbital step-off (28%), numbness or other sensory symptoms (26%), trismus (17%), malocclusion (11%), diplopia (4%), and enophthalmos or orbital dystopia (2%). Malar changes (
P < .001), step-off at the infraorbital rim (
P < .01), and trismus (
P = .02) were significantly associated with indication for operation. Meanwhile, lack of symptomatology was notably associated with a non-operative status (
P < .001). Symptoms such as temporary diplopia at presentation (
P > .90), enophthalmos or orbital dystopia (
P = .10), numbness or other sensory symptoms (
P = .12), and malocclusion (
P = .70) were not significantly associated with operative status (
Table 3).
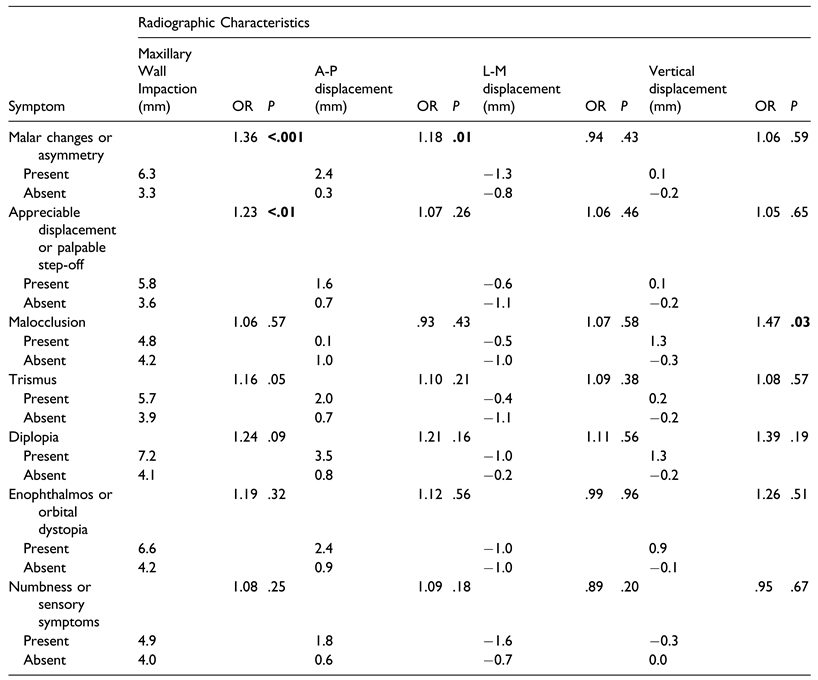
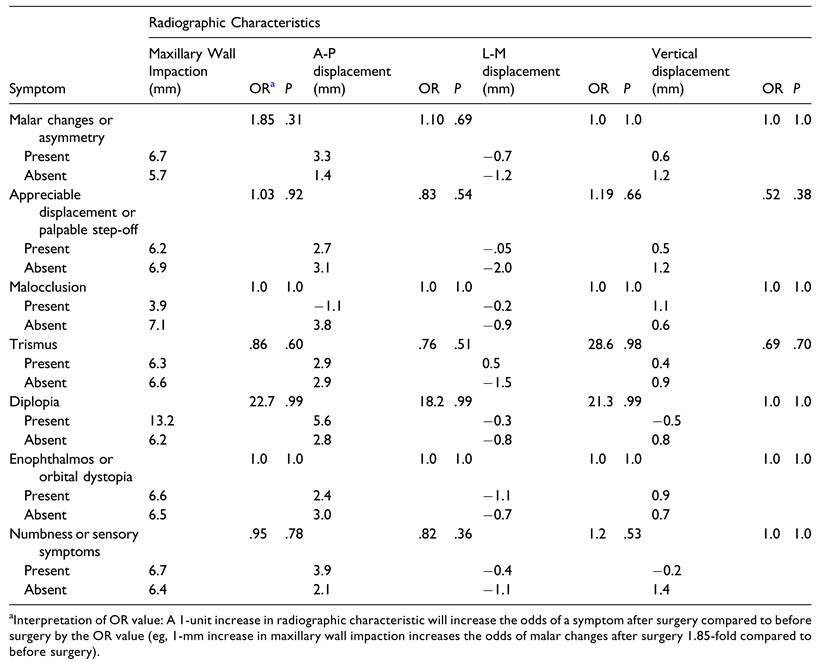
Relationships Between Radiographic Characteristics and Symptomatology of ZMC Fractures
Logistic regression analysis was used to assess relationships between radiographic characteristics of ZMC fractures and initial symptomatic presentation. Radiographic characteristics consisted of displacement measurements in various vectors: lateral maxillary wall impaction, zygoma body rotation, vertical displacement, anterior-posterior displacement, and lateral-medial displacement (
Figure 1,
Figure 2,
Figure 3,
Figure 4 and
Figure 5). These displacement measures were analyzed as they related to clinical malar changes, step-off of the infraorbital rim, malocclusion, trismus, diplopia, enophthalmos or orbital dystopia, and numbness or sensory symptoms (
Table 4).
Lateral Maxillary Wall Impaction
Lateral maxillary wall impaction on radiographic imaging most significantly predicted malar changes (OR = 1.36,P < .001) and appreciable displacement or step-off of the infraorbital rim (OR = 1.23, P < .01). Specifically, for every 1-mm increase in maxillary wall impaction, patients experienced a 1.36-fold or 1.23-fold increase in the odds of symptomatic malar changes or step-off, respectively. Patients with malar flattening on examination experienced an average of 6.3 mm of lateral maxillary wall impaction, compared to 3.3 mm in those who did not present with obvious malar changes. Meanwhile, patients with infraorbital step-off experienced an average 5.8 mm of lateral maxillary wall impaction, and those without step-off experienced an average 3.6 mm of impaction. Other symptomatology, including malocclusion, trismus, diplopia, enophthalmos or orbital dystopia, and sensory symptoms, were not predicted by lateral maxillary wall impaction.
Anterior-Posterior Displacement
AP displacement on radiographic imaging significantly predicted malar changes (OR = 1.18, P = .01). For every 1-mm increase in AP displacement, patients experienced a 1.18-fold increase in the odds of symptomatic malar changes. Patients with obvious malar flattening displayed an average of 2.4 mm of posterior displacement, in comparison to .3 mm in those without malar changes. AP displacement did not predict initial presentation with infraorbital rim step-off, malocclusion, trismus, diplopia, enophthalmos or orbital dystopia, or sensory symptoms.
Vertical Displacement
Vertical displacement on CT imaging significantly predicted the presence of malocclusion (OR = 1.47, P = .03). For every millimeter increase in vertical displacement, patients were 1.47 times more likely to experience malocclusion. Patients with subjective malocclusion exhibited an average of 1.3 mm of inferior displacement; meanwhile, patients without malocclusion exhibited an average of —.3 mm of inferior displacement, or .3 mm of superior displacement. Vertical displacement did not predict any other symptomatology addressed by this study.
Zygoma Body Rotation
Degree of zygoma body rotation, as assessed by angle of rotation, was not associated with clinical symptomatology.
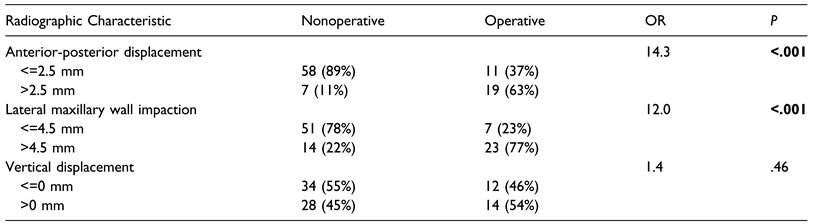
Key Radiographic Characteristics as Predictors of Operative Intervention
Scatter-plot analysis of the radiographic characteristics found to significantly predict symptomatology (ie, lateral maxillary wall impaction, anterior-posterior displacement, and vertical displacement) vs operative indication revealed approximate displacement measurement cut-offs for subsequent analysis (
Figure 6).
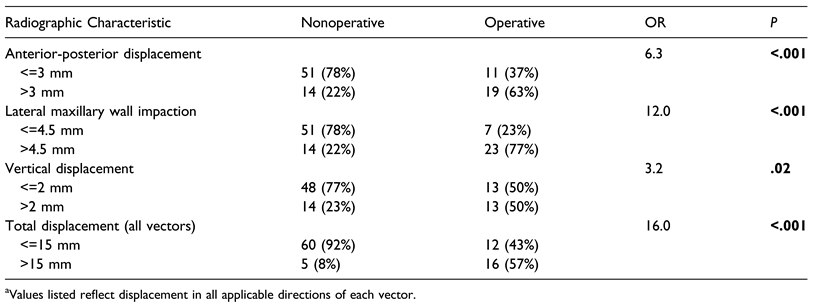
Fisher’s exact tests were then used to assess relationships between the severity of radiographic displacement measurements and need for operative management. ZMC fractures with a lateral maxillary wall impaction greater than 4.5 mm were significantly more likely to be considered operative than those impacted less than or equal to this value (OR = 12.0,
P < .001). Similarly, fractures with an AP displacement greater than 2.5 mm in the posterior direction were significantly more likely to require operative intervention than those displaced less than or equal to this value (OR = 14.3,
P < .001). Meanwhile, no threshold of vertical displacement significantly predicted need for operative intervention (
Table 5).
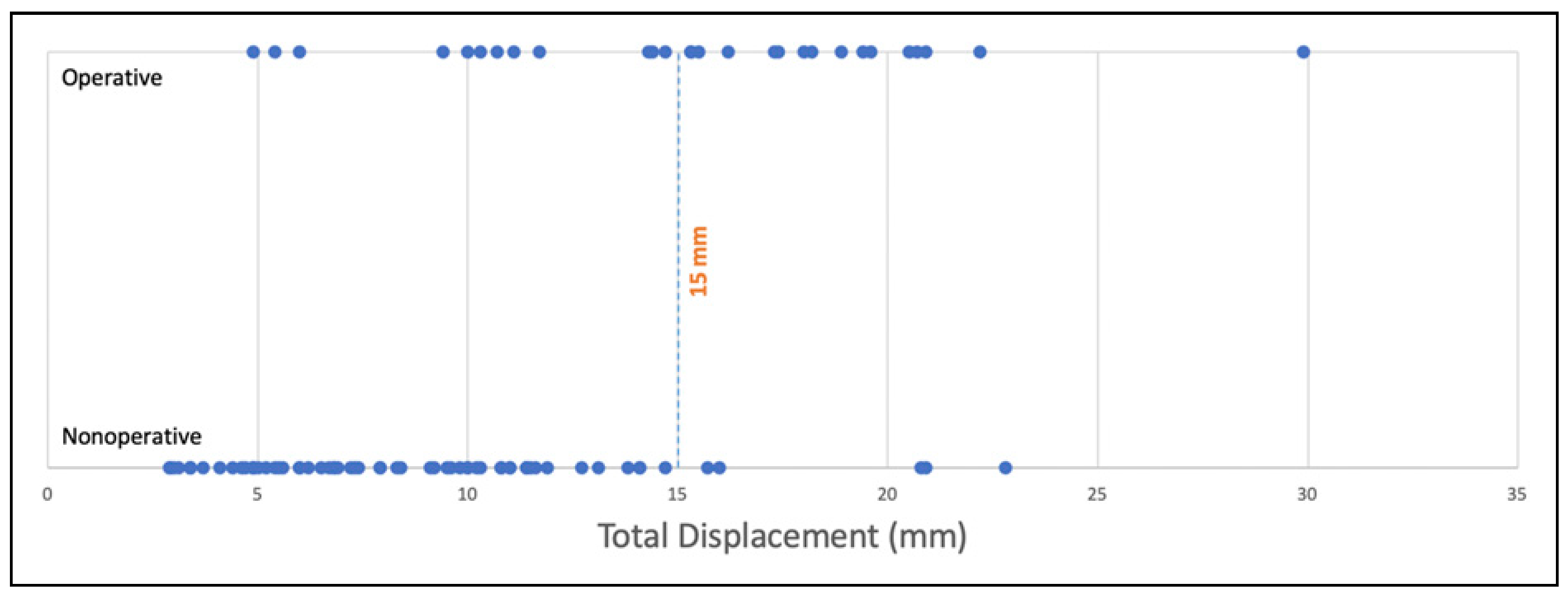
The same approach was applied to determine absolute-value displacement cut-offs that predicted
non-operative status. For those with an AP displacement less than 3 mm either anteriorly or posteriorly, the chance of needing surgery was low (OR = 6.3,
P < .001). Similarly, vertical displacement less than 2 mm either superiorly or inferiorly was unlikely to require surgery (OR = 3.4,
P = .02) (
Table 6). Moreover, fractures with a total absolute displacement less than 15 mm total had a very low risk of requiring surgery (OR = 16.0,
P < .001) (
Figure 7).
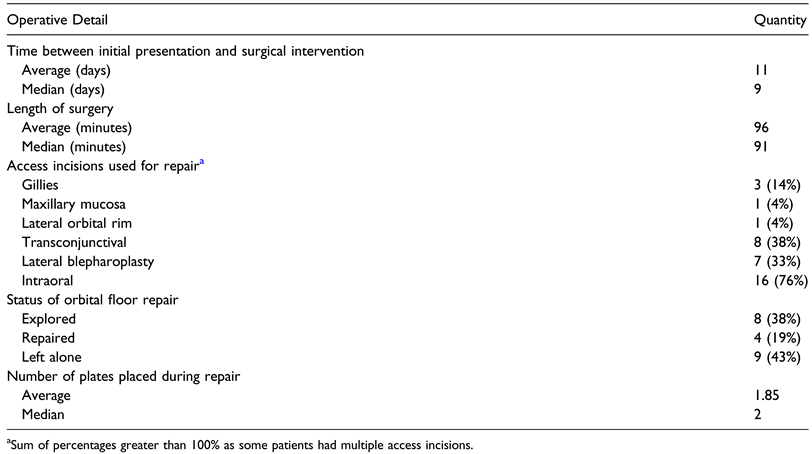
Operative Details
Of the 30 patients whose ZMC fractures were deemed to be operative, 21 underwent surgical intervention with open reduction. The average time between initial presentation and surgery was 11 days, and the average length of surgery was 96 minutes. The access incisions most commonly used for repair were: intraoral (76%), transconjunctival (38%), lateral blepharoplasty (33%), and Gillies (14%). Of the 30 cases, the orbital floor was explored in 8 (38%) cases, repaired in 4 (19%), and left alone in 9 (43%). An average of 1.85 plates and median of 2 plates were placed during repair (
Table 7).
Symptomatology on Follow-Up: Non-Operative and Operative Patients. Of the 65 patients whose ZMC fractures were considered non-operative, 32 (49%) received follow-up for their injury with an ophthalmologist or plastic surgeon after their initial presentation, compared with 21 (70%) patients with operative injuries who received follow-up (P = .08). The 9 remaining surgical candidates did not receive follow-up—and, by extension, surgery—after initial presentation for various reasons: lack of reliable transportation (11%), patient preference (33%), and other/unknown (56%). Among patients who followed up, non-operative patients received an average total length of follow-up of 92 days, while operative patients who underwent surgery received an average of 101 days of follow-up (P = .84).
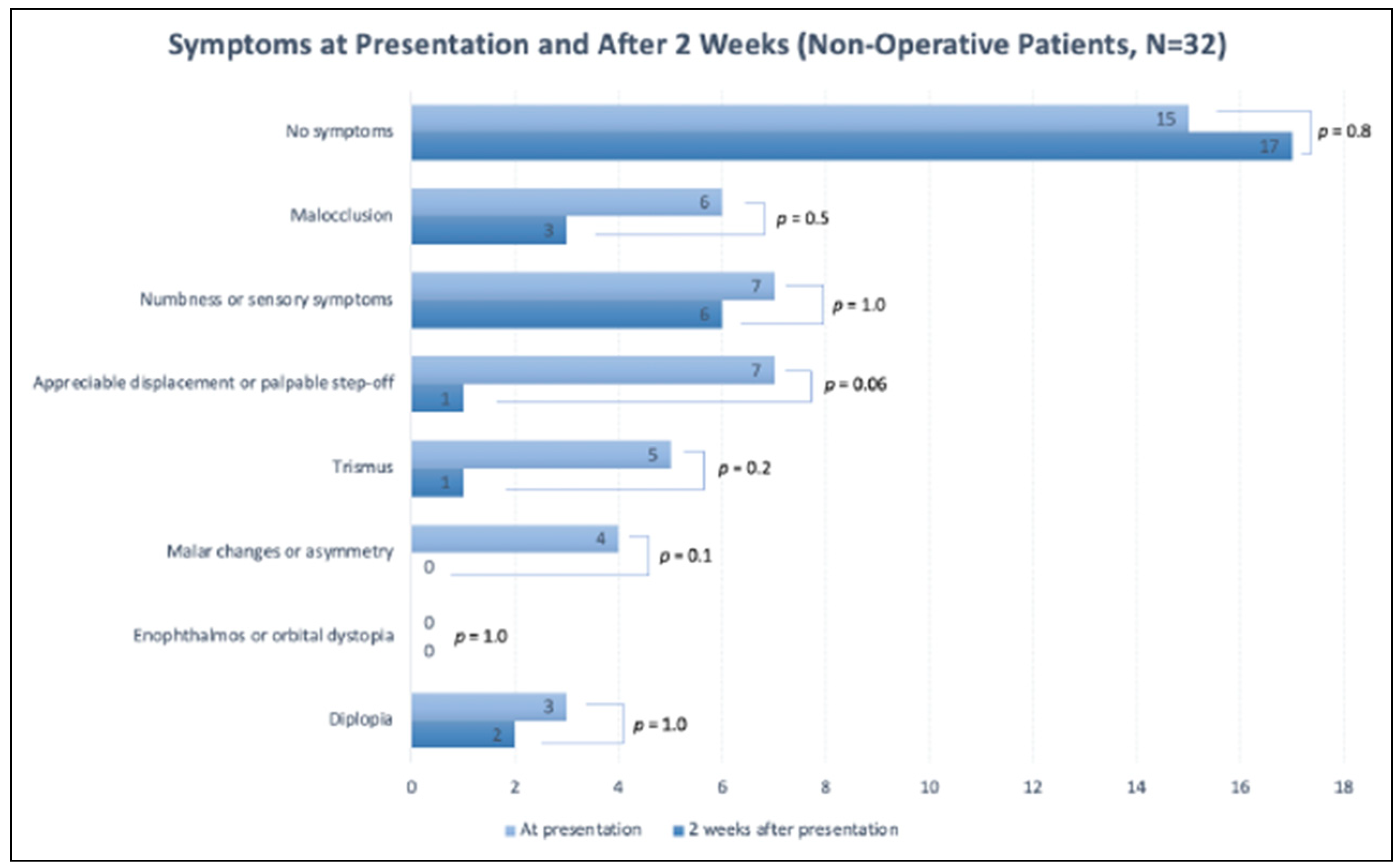
Chart review was conducted to evaluate symptom progression for non-operative patients who received at least 2 weeks of post-injury follow-up. Among non-operative patients who received follow-up, the number of patients endorsing no symptoms increased from 47% at initial presentation to 53% after 2 weeks (
P = .8). All symptoms noted by this study also remained stable or decreased in frequency by 2 weeks after initial presentation. Of note, the frequency of enophthalmos remained stable (
P = 1.0), while diplopia and malar changes decreased over the follow-up period (
P = 1.0 and
P = .1, respectively) (
Figure 8).
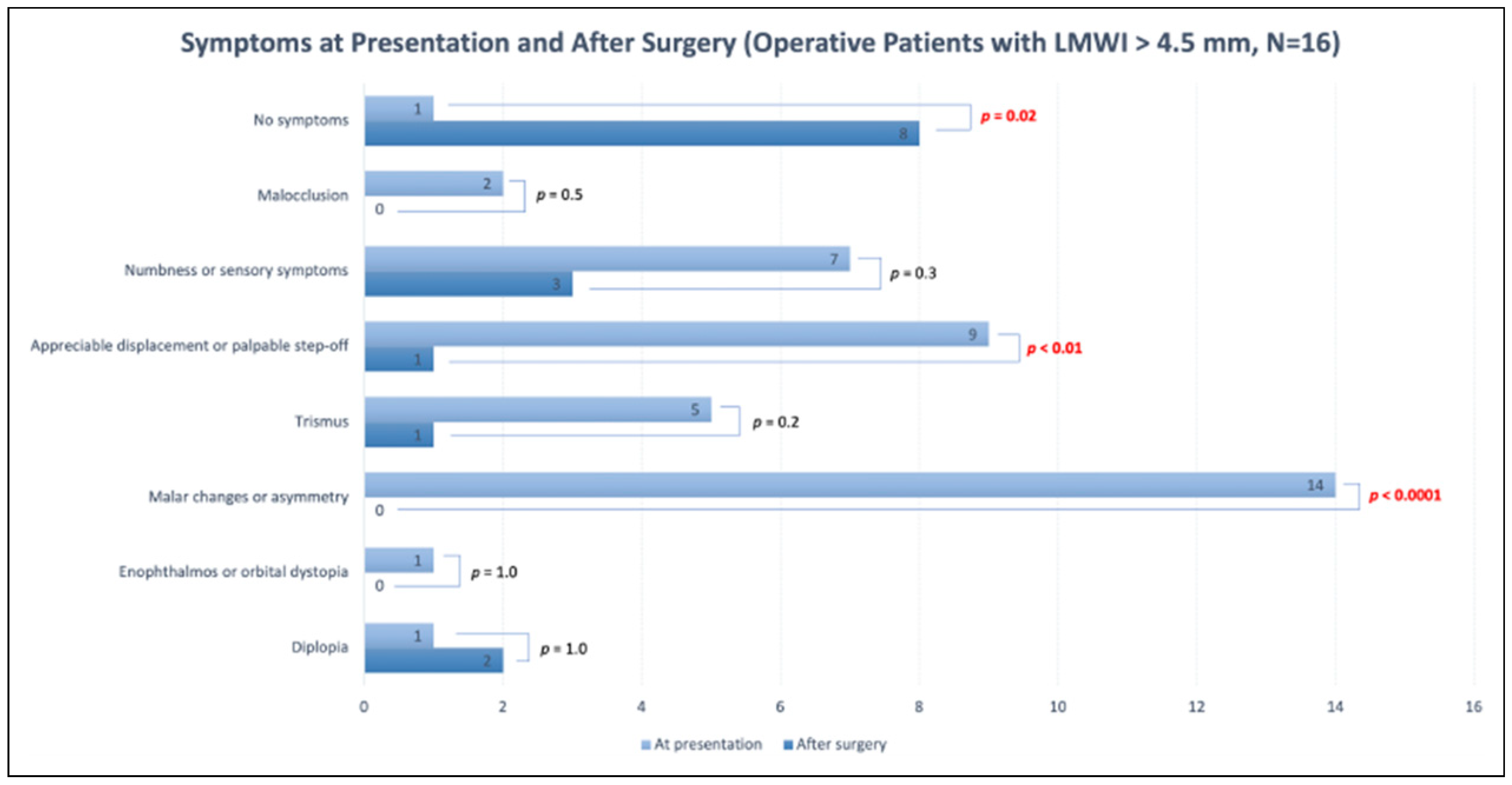
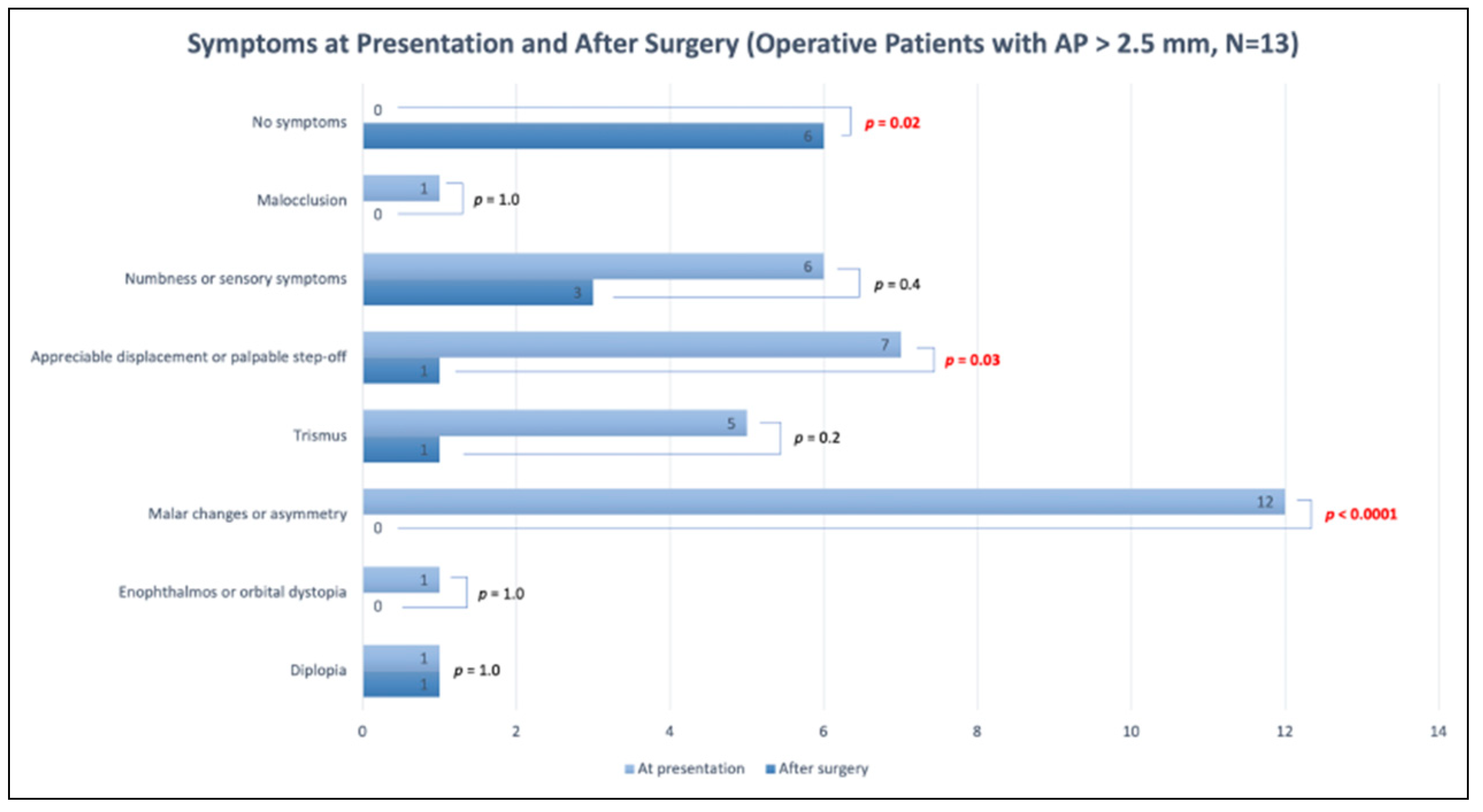
Patients who underwent surgery were seen by their surgeon for a follow-up visit an average of 16 days after surgery, at which time symptom progression was noted. The number of patients endorsing no symptoms increased from 5% at initial presentation to 57% at surgical follow-up (
P < .001). The only symptom that increased in frequency was diplopia, although this change was non-significant (
P = 1.0). The frequency of all other symptoms significantly declined, including malar changes (decreased by 76%,
P < .0001), appreciable displacement or step-off (decreased by 52%,
P < .001), and trismus (decreased by 33%,
P = .02) (
Figure 9). Outcomes assessment was also performed for the subset of surgical candidates who met the radiographic operative thresholds delineated by this study (ie, LMWI
> 4.5 mm or AP displacement
> 2.5 mm posteriorly). Among the 16 surgical candidates with LMWI
> 4.5 mm and the 13 surgical candidates with
> 2.5 mm of posterior displacement, the frequency of appreciable displacement or step-off (
P < .01 and
P = .03, respectively) and malar changes (
P < .0001 for both groups) decreased significantly following surgery. A significant proportion of both subsets of patients experienced complete resolution of symptoms following surgery (
P = .02 for both groups) (
Figure 10 and
Figure 11).
Logistic regression analysis was also conducted to assess relationships between preoperative radiographic characteristics of patients’ fractures and 2 dependent variables: symptoms at initial presentation and symptoms following surgery (
Table 8). No statistically significant relationships were identified.
Discussion
Determining the optimal management of zygomaticomaxillary complex fractures can be challenging in the absence of severe displacement or acute symptoms. In this paper, we reviewed a number of displacement vectors of ZMC fractures to determine which were associated with clinical symptoms and predicted operative intervention. For practical purposes, we chose to focus on two-dimensional vectors, as most practitioners evaluate patients using CT scans along individual planes (ie, axial, coronal, and sagittal). Although 3D rendering can be performed and may allow for a better depiction of ZMC displacement, measuring displacement vectors with this methodology can be challenging and difficult to standardize [
10]. Despite the frequency of ZMC fractures, there is no consensus on indications regarding surgical management. Most previous authors agree that persistent clinical symptoms associated with ZMC displacement are indications for surgery [
11]. In our cohort, malar flattening, trismus, and a visible or palpable infra-orbital step-off were all statistically significant predictors of operative intervention. Malar flattening was the most common presenting clinical symptom in our patients with ZMC fractures at 31% (29/95) and was also the most common symptom necessitating operative intervention at 73% (22/30).
When analyzing the various possible displacement vectors for patients with ZMC fractures, we found the critical vectors that significantly predicted clinical symptomatology were lateral maxillary wall impaction (
Figure 1), AP displacement (
Figure 3), and vertical displacement (
Figure 4). LM displacement (
Figure 5) did not demonstrate a statistically significant association with any of our collected clinical variables.
Lateral maxillary wall impaction exhibited 1.36 times increased odds for malar changes (OR = 1.36,
P < .001) and 1.23 times increased odds for visible or palpable bony step-off (OR = 1.23,
P < .01) for every millimeter of displacement. The lateral maxillary wall is the key component of the zygomaticomaxillary buttress which functions to hold the zygoma in position. The authors hypothesize that ZMC fractures associated with a significant medial displacement of the lateral maxillary wall can serve as a surrogate marker for ZMC instability, and, in particular, disruption of the ZM buttress, which leads to greater displacement of the zygoma body and thereby malar changes. The importance of the ZM buttress for clinically significant displacement in ZMC fractures has been cited before. Prabhu et al. reported displacement along the ZM buttress to be most closely related to rotational deformity along the lateral-medial axis, which translated to an increase in the rate of post-operative complications among patients with ZMC fractures [
12].
AP displacement also illustrated increased odds for malar changes in our patients with ZMC fractures (OR = 1.18,
P = .01). Specifically, patients with malar changes experienced an average of 2.4 mm of posterior displacement vs .3 mm in patients without malar changes. In a study of malar eminence (ME) asymmetry in patients with ZMC fractures, Cho et al. also found that measured ME differences in AP plane exhibited the largest degree of difference between the fractured and non-fractured sides [
6]. Like lateral maxillary wall impaction, AP displacement of the zygoma occurs with fracturing along critical facial skeletal buttresses that hold the zygoma in an anatomic position. As such, fracture displacement at the ZM and ZT sutures from a posteriorly directed force would result in AP displacement and sub-sequent malar flattening.
In contrast, vertical displacement of the zygoma did not affect malar position but did exhibit a statistically significant increased odds for subjective malocclusion (OR = 1.47,
P = .03). Among our 95 patients with ZMC fractures, complaints of malocclusion were rare, occurring in only 10 patients. Patients noting malocclusion would complain of early contact or shifting of their teeth on the affected side. Previous literature have suggested that a sense of malocclusion following ZMC fractures is a result of either infra-orbital neuropraxia or soft tissue swelling and not necessarily related to displacement degree or vector [
13,
14]. Malocclusion in ZMC fractures may also result from masseter spasm secondary to facial trauma, which may pull the mandible toward the ipsilateral side and temporarily mimic the presence of a crossbite [
15]. In our cohort, vertical displacement was the only vector statistically associated with malocclusion. There are 2 proposed mechanisms whereby vertical displacement could account for this: (1) inferior displacement of the zygoma may lead to increased compression of the infraorbital nerve as it exits the infraorbital foramen; (2) vertical shift of the zygoma may inferiorly displace the alveolus, potentially altering the position of the maxillary teeth. The findings of this study suggest that clinicians should be suspicious of skeletal malocclusion in the setting of vertical displacement in patients with ZMC fractures. In addition to describing clinically significant displacement vectors in patients with ZMC fractures, we hope to provide general guidelines when evaluating patients with ZMC fractures radiographically. In our study, we found that ZMC fractures with concomitant lateral maxillary impaction of
> 4.5 mm were 12 times more likely to require surgery compared to patients with ZMC fractures with a lesser degree of displacement in this vector (
P < .001). Additionally, patients with ZMC fractures that exhibited
> 2.5 mm of posterior displacement in the AP vector demonstrated 14.3 times increased odds for surgery (
P < .001) (
Figure 6). Taken together, these 2 displacement vectors and measurement cut-offs place patients with ZMC fractures into an increased risk category for potential operative intervention, which should influence patient counseling, shared operative decision-making, and determine need for close follow-up. Outcomes assessment of surgical follow-up data, which indicate that surgery significantly benefits patients with injuries meeting these thresholds (
Figure 10 and
Figure 11), supports these radiographic cut-offs for operative intervention. Specifically, operating on these subsets of surgical candidates can be expected to yield significant improvement in symptoms including appreciable displacement or palpable step-off and malar changes—a finding that further validates the relationships between these symptoms and the radiographic characteristics LMWI and AP displacement noted earlier in this study (
Table 4). Moreover, our findings may also guide decision-making regarding which patients do
not need surgery. Unsurprisingly, plastic surgeons can feel confident that patients without any symptomatology may be managed conservatively (
P < .001). In patients who do present with symptoms, surgeons can feel relatively confident that those without a clinical presentation of trismus, step-off of the infraorbital rim, or malar flattening may also be managed conservatively. Certain radiographic characteristics, including a maximal anterior-posterior displacement less than 3 mm or maximal vertical displacement less than 2 mm, were also consistent with a lower chance of requiring surgery (
P < .001 and
P = .02, respectively). Moreover, patients whose fractures are displaced less than 15 mm in all vectors may be counseled that their injuries are at very low risk for requiring surgical intervention (
P < .001) (
Figure 7). Together, these clinical presentations and displacement cut-offs place certain patients with ZMC fractures at lower risk for operative management and can, as a result, be used to systematically inform which patients do not require additional follow-up.
Symptom progression in nonoperative patients over at least a 2-week post-injury follow-up period was evaluated to account for symptoms that may only become apparent after resolution of edema, such as diplopia and orbital dystopia. The observed decline in the rates of all symptoms, including orbital dystopia, diplopia, and malar changes, throughout this follow-up period supports the applicability of the study’s predictive model (
Figure 8).
It is important to note that this study primarily analyzes surgical indication, as patient preferences largely determine the ultimate decision to operate. For example, when the indication for surgical intervention is a contour deformity, patient and provider preference and tolerance for asymmetry are variable. Beyond aesthetic preference, we have found in clinical practice that some patients with significantly displaced ZMC fractures may prefer conservative management due to other factors, including insurance status, medical comorbidities, or cultural values. Meanwhile, some patients with minimally displaced ZMC fractures may opt for operative management for cosmetic improvement or other personal reasons.
There are important limitations to this study to consider when evaluating our results. Although this study aims to relate 2D displacement vectors with clinical symptoms, ZMC fractures are best understood in the 3D perspective. When ZMCs occur, their displacement occurs along multiple vectors, not just along a single plane. Our study analyzed each 2D vector in isolation, which is valuable when considering that most patients are assessed using 2D CT slices. Additionally, reports of clinical symptoms and provider evaluation of patients are subject to heterogeneity, which is challenging to address due to the retrospective nature of the study. However, clinical evaluation of our patients was consistently performed by experienced craniofacial surgeons to help mitigate this limitation and, in all cases, patients’ subjective assessment of their facial asymmetries were considered. Moreover, regardless of surgeon variation in threshold for intervention, our study findings—especially those that clarify the relationships between clinical symptomatology and radiographic characteristics—may be generalized to clinical practice at other institutions, as these findings can serve to inform more objective surgical decision-making.