Abstract
Study Design: Systematic Review and Meta-analysis. Objective: This systematic review and meta-analysis aimed to compare the efficacy of 2 miniplates vs a three-dimensional plate in the management of mandibular condylar fractures. The primary objective was to assess key parameters, including intraoperative time, maximum mouth opening, complications, and functional outcomes, to determine potential differences between the 2 fixation methods. Methods: A comprehensive literature search was conducted to identify relevant studies. Inclusion criteria were applied, and the selected studies underwent systematic review. The key parameters were extracted and subjected to meta-analysis to quantify and compare the outcomes associated with the use of 2 miniplates and three-dimensional plates. The methodologies of the included studies were critically evaluated to address potential biases and confounding factors. Results: The meta-analysis results indicated that there were no statistically significant differences between the 2 fixation methods in terms of intraoperative time, maximum mouth opening, complications, and functional outcomes. However, concerns were raised regarding the high risk of bias, confounding factors, and considerable heterogeneity observed across the reviewed studies. Conclusions: The findings suggest that both 2 miniplates and three-dimensional plates are viable options for the management of mandibular condylar fractures. Despite the lack of statistical significance in the observed differences, the study highlights the need for further prospective research with enhanced methodologies, standardized protocols, larger sample sizes, and reduced bias to refine our understanding and potentially influence clinical management protocols.
Introduction
Mandibular condylar fractures, comprising 18% to 45% of all mandibular fractures [1,2], offer a captivating historical narrative intertwined with their unique functional mechanisms. The journey of understanding and managing these fractures dates back to the era of Hippocrates, who introduced innovative methods involving circumdental wires and external bandaging to re-approximate fractured segments. Traditionally, many surgeons have favoured a conservative approach as the primary treatment strategy for condylar fractures. Their rationale lies in the belief that as long as proximal and distal bone fragments maintain contact, a successful union can occur, resulting in an acceptable functional outcome [3,4,5]. However, recent advances in the field challenge this convention.
A recent systematic review and meta-analysis have brought forth compelling evidence that surgical intervention for subcondylar fractures offers superior clinical outcomes when compared to non-surgical approaches [6]. The surgical treatment of subcondylar fractures in the mandible presents a formidable challenge due to limited accessibility and the critical proximity to vital anatomical structures [7]. Over time, the landscape of subcondylar fracture treatment has evolved, with surgical intervention emerging as the standard option. This transformation can be attributed to technological advancements, the development of specialized osteosynthesis devices, and the refinement of surgical techniques, all of which have been made possible by an improved understanding of the surgical anatomy [8].
The primary objective of open reduction and internal fixation (ORIF) for subcondylar fractures is the restoration of normal anatomical structures and functions. This entails achieving fixation robust enough to withstand the physiological forces of compression and tension. Titanium plates and screws have become the widely adopted materials for this purpose, owing to their effectiveness and compatibility with the specific demands of subcondylar fracture management [9]. In the annals of surgical history, a plethora of techniques and fixation methods have been chronicled. These have encompassed the utilization of Kirchner wires, mini-plates, resorbable pins, and the relatively recent advent of 3-dimensional (3-D) plates [10]. Presently, the most prevalent approach in osteosynthesis is the deployment of a dual mini-plate fixation secured by screws. The utilization of 2 mini-plates (Figure 1) has demonstrated its capacity to furnish adequate rigidity for mandibular functionality, as well as to restore anatomical alignment with a relatively modest incidence of complications [11].
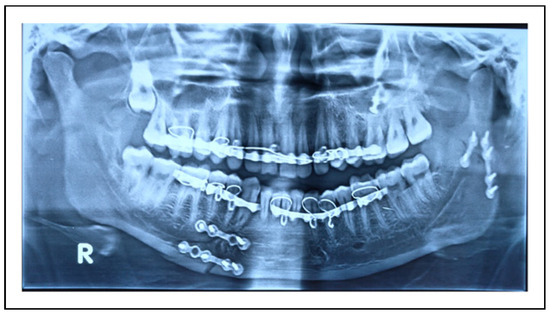
Figure 1.
Orthopantamogram showing fixation of subcondylar fracture with 2 mini-plates.
The inception of 3-D plates, (Figure 2) as eloquently described by Farmand [10] in the late 1990s for the management of mandibular fractures, introduced a frame-like, anatomically tailored approach that exhibited superior stability in contrast to conventional two-plate techniques [12]. Further merits of 3D miniplates, when juxtaposed with their conventional counterparts, encompass facile applicability, uncomplicated affixation to bone without introducing deformations or perturbations to the fracture site, concurrent reinforcement of both the superior and inferior mandibular boundaries, diminished surgical duration, and the augmentation of biomechanical steadiness [10]. Notable investigations have harnessed computed tomography (CT)-based finite element modelling to evaluate the utility of 3-D anatomical plates for mandibular subcondylar fracture repair [13]. Regrettably, scant attention has been devoted to assessing the practical efficacy of 3-D plates in real clinical scenarios.
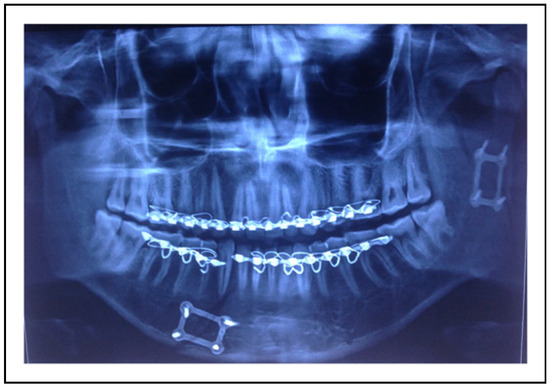
Figure 2.
Orthopantamogram showing fixation of subcondylar fracture with 3 dimensional plate.
Hence, the central objective of this systematic review and meta-analysis herein presented is to undertake a comparative scrutiny of the clinical effectiveness of the traditional two-miniplate approach vis-á-vis the utilization of 3-D anatomical plates in the surgical management of open mandibular subcondylar fractures.
Methodology
The current systematic review and meta-analysis was executed in strict adherence to the tenets delineated within the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA), coupled with the systematic structuring guided by PICO criteria, which encapsulates Population, Intervention, Control, and Outcome parameters (Table 1). It is noteworthy that this specific review has been duly recorded in PROSPERO, the globally recognized prospective repository for systematic reviews, bearing the distinguished registration number CRD42023443923. As the present study does not involve any interventions on animals or humans, this study was waived from Institutional Review Board.

Table 1.
PICO Strategy for Evaluating the Scientific Evidence.
The central query driving the present meta-analysis may be encapsulated as follows: Does the utilization of three-dimensional plates (the Intervention) surpass the conventional two-miniplate approach (the Control) in terms of bestowing enhanced stability, curtailing surgical time, expanding the range of postoperative mandibular movements, and mitigating post-surgical complications (the Outcomes), specifically in the context of treating mandibular subcondylar fractures in individuals possessing sound overall health (the Population)?”
Search Strategy
In August of the year 2023, a thorough and meticulous exploration of the scholarly domain was conducted through a comprehensive perusal of electronic databases, including PubMed, Medline, Google Scholar, and the esteemed Cochrane Library. Notably, this search was devoid of temporal constraints. The pursuit of knowledge entailed the deployment of 1 or a conjunction of search terms such as ‘3-dimensional plates,’ ‘2 miniplates,’ ‘Mandibular subcondylar fracture,’ ‘mandibular condylar fracture,’ ‘geometric plates,’ and ‘3D plates.’ The art of Boolean Operators, both ‘AND’ and ‘OR,’ was deftly employed to refine the search. In addition, a manual expedition of all periodicals pertaining to the realm of oral and maxillofacial surgery was diligently conducted.
The inquisitive nature of this endeavour did not cease with the electronic realm. It extended to the hallowed pages of identified studies and relevant reviews, with their reference lists carefully scrutinized for possible inclusion. Furthermore, the vast expanse of online databases was combed through, unveiling any ongoing clinical trials. Notwithstanding, the ‘grey literature’ was scoured for any ongoing investigations bearing relevance to the subject matter, with a view to their potential assimilation into the annals of this review.
For the purpose of PubMed/Medline, the chosen search strategy was articulated as follows:
(“condylar” [All Fields] OR “condylars” [All Fields]) AND (“fractur” [All Fields] OR “fractural” [All Fields] OR “fracture s” [All Fields] OR “fractures, bone” [MeSH Terms] OR (“fractures” [All Fields] AND “bone” [All Fields]) OR “bone fractures” [All Fields] OR “fracture” [All Fields] OR “fractured” [All Fields] OR “fractures” [All Fields] OR “fracturing” [All Fields]) AND “3” [All Fields] AND (“dimensional” [All Fields] OR “dimensionalities” [All Fields] OR “dimensionality” [All Fields] OR “dimensionalized” [All Fields] OR “dimensionally” [All Fields]) AND (“bone plates” [MeSH Terms] OR (“bone” [All Fields] AND “plates” [All Fields]) OR “bone plates” [All Fields] OR “plate” [All Fields] OR “plate s” [All Fields] OR “plated” [All Fields] OR “plates” [All Fields] OR “plating” [All Fields] OR “platings” [All Fields])
Translations
Condylar. “condylar” [All Fields] OR “condylars” [All Fields]
Fracture. “fractur” [All Fields] OR “fractural” [All Fields] OR “fracture’s” [All Fields] OR “fractures, bone” [MeSH Terms] OR (“fractures” [All Fields] AND “bone” [All Fields]) OR “bone fractures” [All Fields] OR “fracture” [All Fields] OR “fractured” [All Fields] OR “fractures” [All Fields] OR “fracturing” [All Fields]
Dimensional. “dimensional” [All Fields] OR “dimensionalities” [All Fields] OR “dimensionality” [All Fields] OR “dimensionalized” [All Fields] OR “dimensionally” [All Fields]
Plate. “bone plates” [MeSH Terms] OR (“bone” [All Fields] AND “plates” [All Fields]) OR “bone plates” [All Fields] OR “plate” [All Fields] OR “plate’s” [All Fields] OR “plated” [All Fields] OR “plates” [All Fields] OR “plating” [All Fields] OR “platings” [All Fields]
This rigorous and comprehensive search methodology forms the foundation upon which the current study rests, ensuring the breadth and depth of the literature surveyed.
Study Selection
Two diligent examiners (SKK and AJ) embarked upon an independent evaluation of all studies that held the potential to meet the eligibility criteria. This discerning scrutiny encompassed the perusal of titles, keywords, abstracts, and the entire corpus of the texts in question. In the event that disparities regarding the inclusion of particular studies arose, these discrepancies were judiciously adjudicated through erudite deliberations involving a third reviewer (VK).
Inclusion and Exclusion Criteria
Inclusion Criteria. This investigation focused on including randomized controlled trials, controlled clinical trials, and retrospective studies which compared the efficacy of 2 miniplates vs 3-dimensional plates in the treatment of mandibular subcondylar fractures.
Exclusion Criteria. To maintain methodological rigor, case reports, literary reviews, in vitro inquiries, technical annotations, and non-randomized trials with incomplete or insufficient data were excluded. Additionally, studies exploring alternative approaches to managing mandibular subcondylar fractures were not within the scope of this investigation. For consistency and coherence in analysis, only studies articulated in the English language were considered for inclusion. Studies published in other languages were excluded from this comprehensive examination.
Data Extraction
Both the reviewers exercised great care in scrutinizing the amassed studies, and they meticulously gleaned all pertinent data from the studies that found their way into our comprehensive analysis. This painstaking process entailed the extraction of a gamut of critical details, encompassing the identities of the authors, the architectural design of the respective studies, the year of their publication, the average age of the subjects, the gender distribution, the cohort size, the temporal span of post-operative follow-up, the methodology employed for fixation, the steadfastness of the fixation achieved, the typical duration of the surgical procedures, the post-surgical occlusal relationships, and any concomitant complications encountered.
The chief focal point of our inquiry revolved around the stability of the fixation as well as the average duration of time required for the placement of these plates, serving as our primary outcomes of interest. Beyond these primary parameters, secondary outcomes encompassed the postsurgical occlusal harmony and the incidence of complications, including the fracture of the plates, the formation of sialocele, facial nerve paresis, and instances of fracture nonunion.
The meticulously extracted data underwent rigorous scrutiny through a meta-analytical process, but this analysis was only conducted on studies that exhibited homogeneity in their comparative measures and the outcomes reported.
Data Synthesis and Meta-Analysis
For binary outcomes, like complications the odds ratio (OR) with a 95% confidence interval (CI) was calculated using a random-effects model. Standard mean differences with 95% CI were employed for continuous data pertaining to the time required for fixation and maximum mouth opening. Forest plots were generated to visually represent the study data. The analysis was conducted using Review Manager, version 5.3 (The Nordic Cochrane Centre, Cochrane Collaboration).
Heterogeneity Assessment
Discrepancies in the estimates of treatment effects across trials were evaluated using the Cochrane test for heterogeneity and the I2 statistic. The I2 statistic represents the percentage of variation in study outcomes attributed to heterogeneity rather than chance. According to the Cochrane handbook, heterogeneity levels can be categorized as follows: 0% - 40% (not important), 30% - 60% (moderate), 50% - 90% (substantial), and 75% - 100% (considerable). In case of considerable heterogeneity a subgroup analysis was done.
Risk of Bias Assessment
The assessment of methodological quality was executed through the diligent application of the Cochrane Collaboration’s instruments designed for the evaluation of the potential for bias in randomized controlled trials. This classification process revolved around the appraisal of 7 critical domains, each contributing to the overall risk assessment. These domains included the random sequence generation, allocation concealment, the blinding of both participants and personnel, the blinding of those responsible for outcome assessment, the handling of incomplete outcome data, selective reporting, and the potential for any other biases.
For each of these domains, responses were judiciously assigned 1 of 3 categories: ‘low,’ ‘unclear,’ or ‘high.’ It is noteworthy that the designation of ‘low’ in all domains signalled a commendable state of low risk of bias for that particular study under examination. In contrast, the presence of even a single domain receiving an ‘unclear’ or ‘high’ response conveyed a corresponding level of uncertainty or heightened risk of bias, respectively, for the study in question.
Results
Search Results
The literature search yielded 348 results, and following the elimination of duplicates, 277 distinct studies were identified. Subsequent to a preliminary screening, only 9 articles were deemed suitable for comprehensive full-text review. Upon closer examination of the full texts, a total of 7 studies met the predetermined eligibility criteria for inclusion. The study flow process is illustrated in Figure 3.
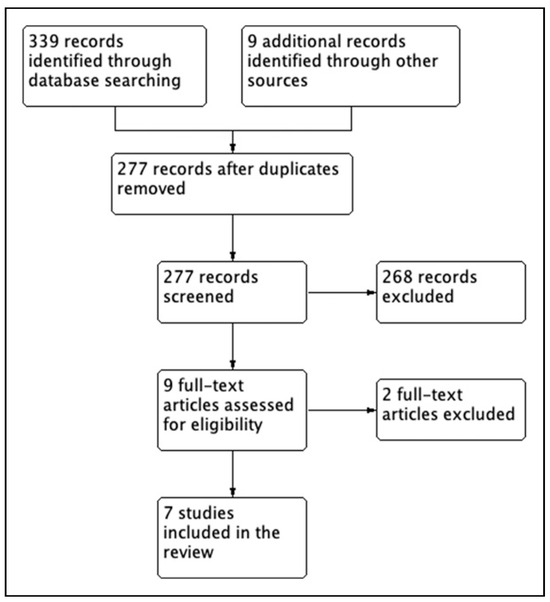
Figure 3.
Flow diagram of study selection process.
Characteristics of Included Studies
Seven studies were selected for the systematic review, comprising a total of 250 patients aged between 16 and 60 years. The participant distribution consisted of 206 males and 44 females. Among these studies, 2 each employed delta plates, rectangular plates, and trapezoidal plates, while 1 study utilized the MatrixMANDIBLE Subcondylar Plate as a three-dimensional plate. The investigations assessed a range of parameters, including intra-operative time taken for fixation, ease of plate adaptation, postoperative occlusion status, maximum mouth opening, jaw movements, and various complications. A comprehensive overview of the characteristics of the included studies is presented in Table 2.

Table 2.
Characteristics of Included Studies.
Results Pertaining to Various Parameters Assessed
Table 3 and Table 4 showcase the results related to various assessed parameters and reported complications across all included studies.

Table 3.
Different Parameters Assessed in the Included Studies.

Table 4.
Various Complications Reported in Included Studies.
Concerning the intraoperative time taken for fixation, only 3 out of the 7 studies provided data on this parameter [14,16,18]. All 3 studies indicated a statistically significant reduction in fixation time when employing a 3D plate compared to the use of 2 miniplates. Adhikari et al [14] reported superior ease of adaptation with the 3D plate in comparison to 2 miniplates, while Ahuja et al [15] noted a faster adaptation process with the 3D plate compared to 2 miniplates.
Five out of the 7 included studies [14,15,17,18,19] addressed post-operative occlusion in both groups. All studies concluded that the occlusion for all patients in both groups was satisfactory, with no statistically significant differences observed. Mouth opening was assessed by 4 studies [14,15,16,18], of which 2 found no statistically significant difference in mouth opening between the 2 groups [14,15], while 2 studies concluded that mouth opening was superior with the use of a 3D plate [16,18]. However, regarding jaw movements, 3 studies [14,15,18] that reported this parameter found no statistically significant difference between the groups.
Ganguly et al [16] investigated biting efficiency and determined that it was enhanced in patients treated with a 3D plate. On the other hand, Sukegawa et al [20] reported no statistically significant differences between the groups in terms of vertical height difference, condylar angle, and mandibular angle.
Meta-Analysis Results
The continuous data outcomes assessed in this study include the intraoperative time required for fixation and maximum mouth opening (MMO) at the 3-month follow-up. Metaanalysis for these parameters employed Mean Differences with a 95% Confidence Interval (CI). Among the 7 studies, only 2 [16,18] reported intraoperative time and MMO with mean and standard deviation. Regarding, Intraoperative Time for Fixation, Pooled estimates and outcome data analysis using the Random Effects model indicated that the fixation of a 3D plate required comparatively less time than the use of 2 miniplates (MD = —15.65, 95% CI: —31.41 to .12, P = .05, I2 = 96%) (Figure 4).
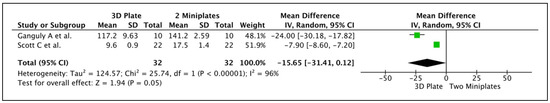
Figure 4.
Forest plot depicting the analysis of Intraoperative time taken for fixation in both the groups.
However, for Maximum Mouth Opening at 3 months, it was observed that patients treated with 2 miniplates exhibited better mouth opening than those with a 3D plate (MD = 3.76, 95% CI: —1.83 to 9.34, P = .19, I2 = 97%) (Figure 5). Both results, however, were not statistically significant and demonstrated considerable heterogeneity.
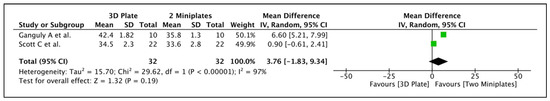
Figure 5.
Forest plot depicting the analysis of maximum mouth opening at 3 months post-operative in both the groups.
Out of the 7 studies, 6 reported complications. Given the heterogeneity in reporting various complications, a subgroup analysis was conducted. However, the analysis of dichotomous data revealed no significant difference between the 2 groups (OR = 1.31, 95% CI: .63 to 2.72, P = .66, I2 = 0%) (Figure 6). Figure 7 displays the funnel plot of the included studies concerning various reported complications.
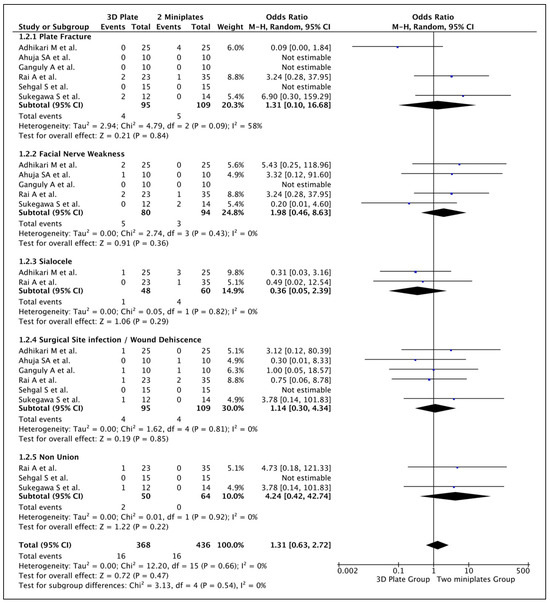
Figure 6.
Forest plot depicting the analysis of complications reported in both the groups.
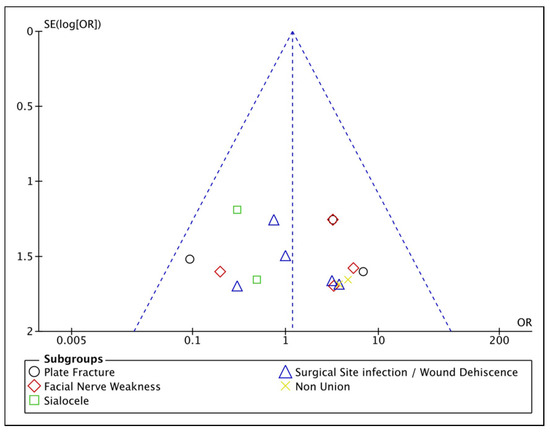
Figure 7.
Funnel plot of the included studies concerning various reported complications.
Risk of Bias Assessment
Concerning the assessment of risk of bias, 6 out of the 7 studies demonstrated a high risk of bias, introducing a potential influence on the outcomes of this meta-analysis. The risk of bias summary among the included studies is illustrated in Figure 8, while Figure 9 provides a graphical representation of the risk of bias percentages across various domains.
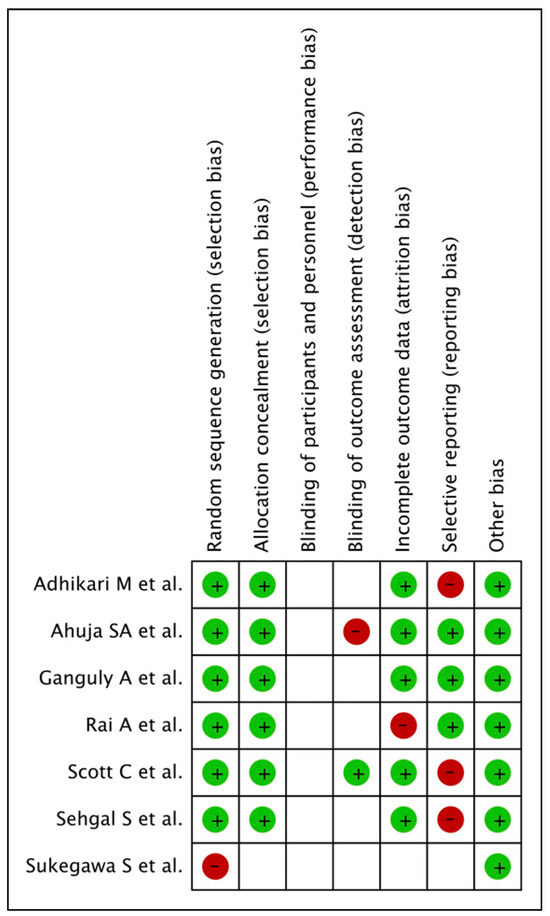
Figure 8.
Risk of bias summary of the included studies.
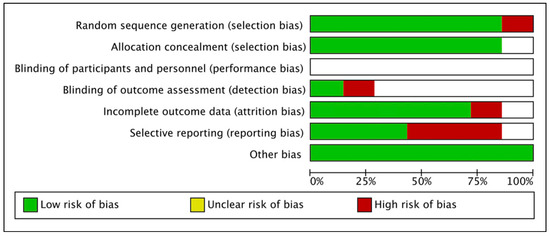
Figure 9.
Graphical representation of the risk of bias percentages across various domains.
Discussion
Fractures of the mandibular condyle constitute 10% of all facial fractures [21]. Treatment options vary based on factors such as age, mouth opening, occlusion, dentition, level of condylar fracture, degree of displacement, ramus height, concomitant fractures, patient preference, and associated injuries. Both open and closed approaches are considered, however, recent literature suggests that open reduction and internal fixation (ORIF) of subcondylar fractures yield superior outcomes in both functional and aesthetic aspects [22,23,24].
Traditionally, ORIF was carried out using a single 4 or 6 hole straight miniplate vertically positioned over the posterior border of the mandibular condylar neck being a widely employed technique [25,26,27]. However, this method exhibits a notable failure rate as it does not align with the osteosynthesis principles outlined by Meyer et al in 2002 [28], which are recommended for miniplate osteosynthesis in the mandibular region. To address these limitations, many surgeons have shifted to utilizing 2 miniplates. The first miniplate is typically placed in the axis of the condylar neck, while the second is positioned obliquely under the mandibular notch.
Despite its advantages, the placement of 2 plates and 4 screws in the small proximal condylar fragment can be challenging, and this technique is nearly impractical for cases involving high mandibular condylar fractures. As an alternative to the two-miniplate approach, specially designed 3D plates meet most requirements for achieving rigid fixation in subcondylar fractures. Some studies in the literature argue that 3D plates exhibit superiority over the conventional two-miniplate method [29].
This study aims to conduct a systematic review and meta-analysis to comprehensively compare the outcomes of mandibular condylar fracture fixation using either 2 miniplates or a 3D plate. The results reveal no statistically significant differences between the 2 approaches in terms of fixation time, maximum mouth opening, and the occurrence of complications. Additional parameters, including occlusal stability and jaw movements, exhibit similar profiles in both groups across various studies. Notably, the 3D plate demonstrates greater and faster adaptability compared to 2 miniplates [14,15].
While the time required for three-dimensional plate fixation was indeed less than that for 2 miniplates, this difference did not reach statistical significance. The reduced time can be attributed to the lower quantity of plates and screws needed for 3D plate fixation, as well as the inherent ease of adaptation. Placing 2 miniplates and screws in the proximal condylar segment is challenging, contributing to prolonged surgical durations. The advantage of a shorter fixation time lies in minimizing the duration of soft tissue retraction, potentially reducing the incidence of facial nerve paresis. Additionally, a shorter procedure duration may result in less postoperative oedema.
This systematic review revealed that mandibular movements, including opening, lateral movements, and protrusive movements, exhibited similarities in both groups across the studies analysed. This observation may stem from the fact that these movements are primarily governed by muscle attachment, and the utilized hardware is not a determining factor influencing jaw movements. Ellis et al [30] proposed that fractures involving the condylar process could impede the functional aspects of the masticatory system, potentially impacting mandibular mobility and leading to asymmetrical motion. Specifically, a condylar process fracture might disrupt the normal action of the lateral pterygoid muscle, causing a deviation toward the site of the fracture during mouth opening. Therefore, restoring the integrity of the temporomandibular joint (TMJ) ligaments and ensuring proper functioning of the lateral pterygoid muscles becomes crucial for addressing potential limitations in mandibular mobility and preventing asymmetrical movements.
Complications, such as plate fracture, facial nerve weakness, sialocele, and surgical infection, analysed in the present study do not appear to exhibit significant differences between the 2 groups. This observation is attributed to the fact that these complications are more closely associated with the surgical technique employed rather than the specific hardware used for fracture fixation. When performing (ORIF) for mandibular condylar fractures, careful consideration of plate design is crucial. An inadequately rigid plate may not withstand the physiological masticatory forces applied to the subcondylar region, potentially resulting in plate fracture, loosening of screws, or both. While adequate rigidity is essential, improper reduction may still lead to plate fracture or bending and screw loosening. Plate fracture or bending and screw loosening are indicative of either insufficient fracture stabilization or incorrect fracture reduction. Delicate soft tissue retraction is imperative to avoid injury to the facial nerve, subsequently preventing postoperative facial nerve weakness. Similarly, improper watertight closure may contribute to the formation of sialocele. Thus, meticulous attention to both the surgical technique and hardware characteristics is essential to minimize the risk of complications associated with mandibular condylar fracture fixation.
The obtained results may be subject to confounding factors, with heterogeneity emerging as a primary concern, especially in the context of the duration of fixation and maximum mouth opening. This heterogeneity, stemming from divergent methodologies employed across studies, poses a substantial challenge to result interpretation. Furthermore, some studies exhibited limited statistical power due to small sample sizes, potentially leading to false-negative conclusions. The variation in methods used to assess specific outcomes introduces an additional layer of complexity. Identified reporting bias further complicates the interpretation of results, as not all studies evaluated every outcome. A more comprehensive evaluation of all outcomes across all studies, followed by subsequent analysis, could have enhanced result accuracy. Additionally, a noteworthy concern is the uniformly high risk of bias observed across most studies, undoubtedly influencing the study outcomes. Addressing these methodological challenges and biases is crucial for refining the reliability and validity of the study results.
Considering the results of the present meta-analysis, which indicate a high risk of bias, the presence of confounding factors, and considerable heterogeneity, we assert that there is insufficient evidence to definitively conclude that 3D plates are superior to 2 miniplates for the fixation of mandibular condylar fractures. Further prospective studies with improved methodologies, standardized protocols, larger sample sizes, low risk of bias, and high-quality evidence are recommended to refine our understanding and potentially influence the management protocols for mandibular condylar fractures.
Conclusion
In light of the current meta-analysis findings, it was observed that the utilization of 3D miniplates presents a feasible option for routinely fixing mandibular fractures. Notably, 3D titanium miniplates yielded comparable results when compared to standard titanium miniplates. The quadrangle geometry inherent to the 3D plate ensures three-dimensional stability at fracture sites, offering robust resistance against torque forces. However, the results obtained in this study did not demonstrate statistical significance between the groups across all evaluated parameters. Consequently, it can be inferred that both plating systems are effective for the management of mandibular condylar fractures.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Stacey, D.H.; Doyle, J.F.; Mount, D.L.; Snyder, M.C.; Gutowski, K.A. Management of mandible fractures. Plast Reconstr Surg. 2006, 117, 48e–60e. [Google Scholar] [CrossRef]
- Morris, C.; Bebeau, N.P.; Brockhoff, H.; Tandon, R.; Tiwana, P. Mandibular fractures: an analysis of the epidemiology and patterns of injury in 4,143 fractures. J Oral Maxillofac Surg. 2015, 73, 951.e1–951.e12. [Google Scholar] [CrossRef]
- MacLennan, W.D. Fractures of the mandibular condylar process. Br J Oral Surg. 1969, 7, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Smets, M.H.; van Damme, P.A.; Stoelinga, P.J.W. Non-surgical treatment of condylar fractures in adults: a retrospective analysis. J Cranio-Maxillo-Fac Surg. 2003, 31, 162–167. [Google Scholar] [CrossRef]
- Villareal, P.M.; Monje, F.; Junquera, L.M.; Mateo, J.; Morillo, A.J.; Gonzalez, C. Mandibular condyle fractures: determinants of treatment and outcome. J Oral Maxillofac Surg. 2004, 62, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Al-Moraissi, E.A.; Ellis, E. Surgical treatment of adult mandibular condylar fractures provides better outcomes than closed treatment: a systematic review and meta-analysis. J Oral Maxillofac Surg. 2015, 73, 482–493. [Google Scholar] [CrossRef]
- Wagner, A.; Krach, W.; Schicho, K.; Undt, G.; Ploder, O.; Ewers, R. A 3-dimensional finite- element analysis investigating the bio- mechanical behavior of the mandible and plate osteosynthesis in cases of fractures of the condylar process. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002, 94, 678–686. [Google Scholar] [CrossRef]
- Kanno, T.; Sukegawa, S.; Tatsumi, H.; et al. The retromandibular transparotid approach for reduction and rigid internal fixation using two locking miniplates in mandibular condylar neck fractures. Int J Oral Maxillofac Surg. 2014, 43, 177–184. [Google Scholar] [CrossRef]
- Kisnisci, R. Management of fractures of the condyle, condylar neck, and coronoid process. Oral Maxillofac Surg Clin North Am. 2013, 25, 573–590. [Google Scholar] [CrossRef]
- Farmand, M. Experiences with the 3-D miniplate osteosynthesis in mandibular fractures. Fortschr Kiefer Gesichtschir. 1996, 41, 85. [Google Scholar]
- Hammer, B.; Schier, P.; Prein, J. Osteosynthesis of condylar neck fractures: a review of 30 patients. Br J Oral Maxillofac Surg. 1997, 35, 288–291. [Google Scholar] [CrossRef]
- Cortelazzi, R.; Altacera, M.; Turco, M.; Antonicelli, V.; De Benedittis, M. Development and clinical evaluation of MatrixMANDIBLE subcondylar plates system (synthes). Craniomaxillofacial Trauma Reconstr. 2015, 8, 94–99. [Google Scholar] [CrossRef]
- Murakami, K.; Yamamoto, K.; Sugiura, T.; Horita, S.; Matsusue, Y.; Kirita, T. Computed tomography-based 3-dimensional finite element analyses of various types of plates placed for a virtually reduced unilateral condylar fracture of the mandible of a patient. J Oral Maxillofac Surg. 2017, 75, 1239.e1–1239.e11. [Google Scholar] [CrossRef]
- Adhikari, M.; Bhatt, K.; Yadav, R.; Mandal, J.; Bhutia, O.; Roychoudhury, A. Fixation of subcondylar fractures of the mandible: a randomized clinical trial comparing one trapezoidal plate with two miniplates. Int J Oral Maxillofac Surg. 2021, 50, 756–762. [Google Scholar] [CrossRef] [PubMed]
- Ahuja, S.A.; Galinde, J.; Asnani, U.; Mistry, Y.A. Comparative evaluation of clinical outcomes using delta plates and conventional miniplates for internal fixation of mandibular condylar fractures in adults. J Oral Maxillofac Surg. 2018, 76, 1255–1266. [Google Scholar] [CrossRef] [PubMed]
- Ganguly, A.; Mittal, G.; Garg, R. Comparison between 3D delta plate and conventional miniplate in treatment of condylar fracture: a randomised clinical trial. J Cranio-Maxillo-Fac Surg. 2021, 49, 1026–1034. [Google Scholar] [CrossRef]
- Rai, A.; Jain, A.; Thukral, R. Two miniplates versus 3- dimensional plate in the management of mandibular subcondylar fractures: a retrospective analysis. Oral Maxillofac Surg. 2021, 25, 457–461. [Google Scholar] [CrossRef]
- Scott, C.; Ramakrishnan, K.; Vivek, N.; Saravanan, C.; Prashanthi, G. Does three-dimensional plate offer better outcome and reduce the surgical time following open reduction and internal fixation of adult mandibular unilateral subcondylar fractures. A randomized clinical study. J Oral Maxillofac Surg. 2021, 79, 1330.e1–1330.e12. [Google Scholar] [CrossRef]
- Sehgal, S.; Ramanujam, L.; Prasad, K.; Krishnappa, R. Three- dimensional v/s standard titanium miniplate fixation in the management of mandibular fractures--a randomized clinical study. J Cranio-Maxillo-Fac Surg. 2014, 42, 1292–1299. [Google Scholar] [CrossRef]
- Sukegawa, S.; Kanno, T.; Masui, M.; et al. Which fixation methods are better between three-dimensional anatomical plate and two miniplates for the mandibular subcondylar fracture open treatment? J Cranio-Maxillo-Fac Surg. 2019, 47, 771–777. [Google Scholar] [CrossRef]
- Gassner, R.; Tuli, T.; H€achl, O.; et al. Cranio-maxillofacial trauma: a 10 year review of 9543 cases with 21067 injuries. J Cranio-Maxillo-Fac Surg. 2003, 31, 51. [Google Scholar] [CrossRef] [PubMed]
- Eckelt, U.; Schneider, M.; Erasmus, F.; et al. Open versus closed treatment of fractures of the mandibular condylar process – a prospective randomized multi-centre study. J Cranio-Maxillo-Fac Surg. 2006, 34, 306–314. [Google Scholar] [CrossRef]
- Worsaae, N.; Thorn, J.J. Surgical versus non- surgical treatment of unilateral dislocated low subcondylar frac- tures: a clinical study of 52 cases. J Oral Maxillofac Surg. 1994, 52, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E.; Simon, P.; Throckmorton, G.S. Occlusal results after open or closed treatment of fractures of the mandibular condylar process. J Oral Maxillofac Surg. 2000, 58, 260–268. [Google Scholar] [CrossRef]
- Ellis, E.; Throckmorton, G.S.; Palmieri, C. Open treatment of condylar process fractures: assessment of adequacy of repositioning and maintenance of stability. J Oral Maxillofac Surg. 2000, 58, 27. [Google Scholar] [CrossRef]
- Haug, R.H.; Assael, L.A. Outcomes of open versus closed treatment of mandibular subcondylar fractures. J Oral Maxillofac Surg. 2001, 59, 370. [Google Scholar] [CrossRef]
- Hyde, N.; Manisali, M.; Aghabeigi, B.; et al. The role of open reduction and internal fixation in unilateral fractures of the mandibular condyle: a prospective study. Br J Oral Maxillofac Surg. 2002, 40, 19. [Google Scholar] [CrossRef]
- Meyer, C.; Kahn, J.L.; Boutemi, P.; Wilk, A. Photoelastic analysis of bone deformation in the region of the mandibular condyle during mastication. J Cranio-Maxillo-Fac Surg. 2002, 30, 160. [Google Scholar] [CrossRef]
- Darwich, M.A.; Albogha, M.H.; Abdelmajeed, A.; Darwich, K. Assessment of the biomechanical performance of 5 plating techniques in fixation of mandibular subcondylar fracture using finite element analysis. J Oral Maxillofac Surg. 2016, 74, 794.e1–794.e8. [Google Scholar] [CrossRef]
- Ellis, E.; Throckmorton, G.S.; Palmieri, C. Treatment of mandibular condylar process fractures: biological consideration. J Oral Maxillofac Surg. 2005, 63, 115–134. [Google Scholar] [CrossRef]
© 2024 by the authors. The Author(s) 2024.