Introduction
Edentulous mandible fractures present a unique set of challenges within the broader landscape of mandibular trauma. Despite their relatively low incidence, accounting for less than 5% of all mandibular fractures, the dearth of high-quality evidence regarding their optimal management underscores the complexity of these cases [
1]. A seminal Cochrane review in 2013 emphasized the inadequacy of evidence to unequivocally support a standardized treatment approach, advocating instead for individualized strategies informed by clinician expertise and patient-specific factors [
2]. Further complicating matters, the classification system proposed by Luhr in 1996, based on remaining mandibular height (class I = 16–20 mm; class II = 11–15 mm; and class III = <10 mm), underscores the heterogeneity of edentulous mandible fractures [
3].
Conventionally, open reduction and internal fixation (ORIF) has been the cornerstone of treatment for these fractures, aimed at restoring mandibular continuity and function promptly. However, despite improved outcomes, there are several challenges associated with open treatment, many of which stem from the resorbed bony architecture. Deficient anatomical landmarks, limited options for secure fixation, and the heightened risk of injury to the inferior alveolar nerve (IAN) during screw placement are among the primary obstacles encountered. Additionally, considerations regarding the size and positioning of reconstruction plates to facilitate future prosthetic rehabilitation, along with the absence of an occlusal reference and difficulties in achieving proper condylar seating, further complicate treatment decisions. Moreover, the compromised osteogenic potential in elderly patients, coupled with altered blood flow dynamics in the edentulous mandible, elevate the risk of complications such as nonunion and infection.
In light of these multifaceted challenges, the potential benefits of leveraging virtual surgical planning (VSP) and patient-specific implants (PSI) are increasingly recognized. While the existing literature on VSP for edentulous mandible fractures is scant, emerging studies typically showcase the utilization of an anatomically reduced 3D printed skull model for preoperative bending of a reconstruction plate [
4,
5,
6]. One of the studies used post-operative analysis to show the accuracy of the final reduction to the planned outcome with good results [
6].
This case series is unique as it is the first to analyze the use of PSIs in patients with fractures of Luhr class III mandibles. By elucidating the advantages and demonstrating a systematic workflow for this technique, we aim to provide valuable insights into enhancing the management of these challenging cases.
Materials and Methods
Patient Selection
This case series included 5 patients with Luhr class III mandibles who sustained fractures and underwent ORIF between October 2020 and February 2023. Patients A-D were treated at Massachusetts General Hospital by 1 provider and Patient E was treated at Detroit Receiving Hospital by a second provider.
Inclusion criteria required: sustained a fracture/s of an edentulous mandible; pre-operative computed tomography (CT) scan; mandibular body height <11 mm as measured on the coronal cuts of the preoperative CT scan at the area of shortest distance; underwent VSP with fabrication of custom cutting/drilling guides and implant; post-operative imaging; at least 1 post-operative follow-up.
Virtual Planning Workflow and Basic Design Considerations
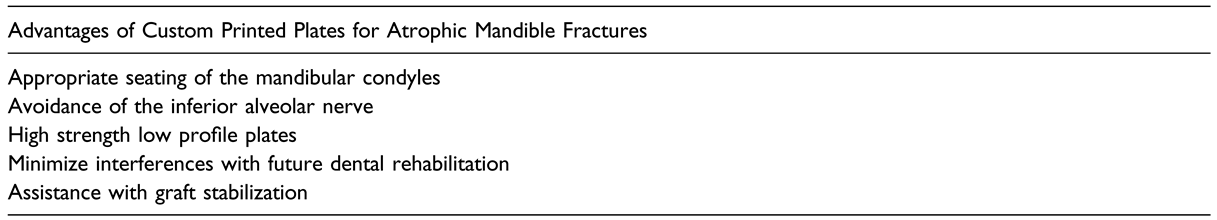
The diagnostic CT scan obtained at the time of initial presentation was converted to a Digital Imaging and Communications in Medicine (DICOM) file and uploaded to the VSP software (Materialise, Belgium) to generate a three-dimensional model of the patient’s skull and mandible. With the aid of an engineer, the mandible was segmented to isolate the fracture fragments, which were then virtually reduced into the correct anatomic positions, ensuring appropriate seating of the condyles bilaterally (
Figure 1).
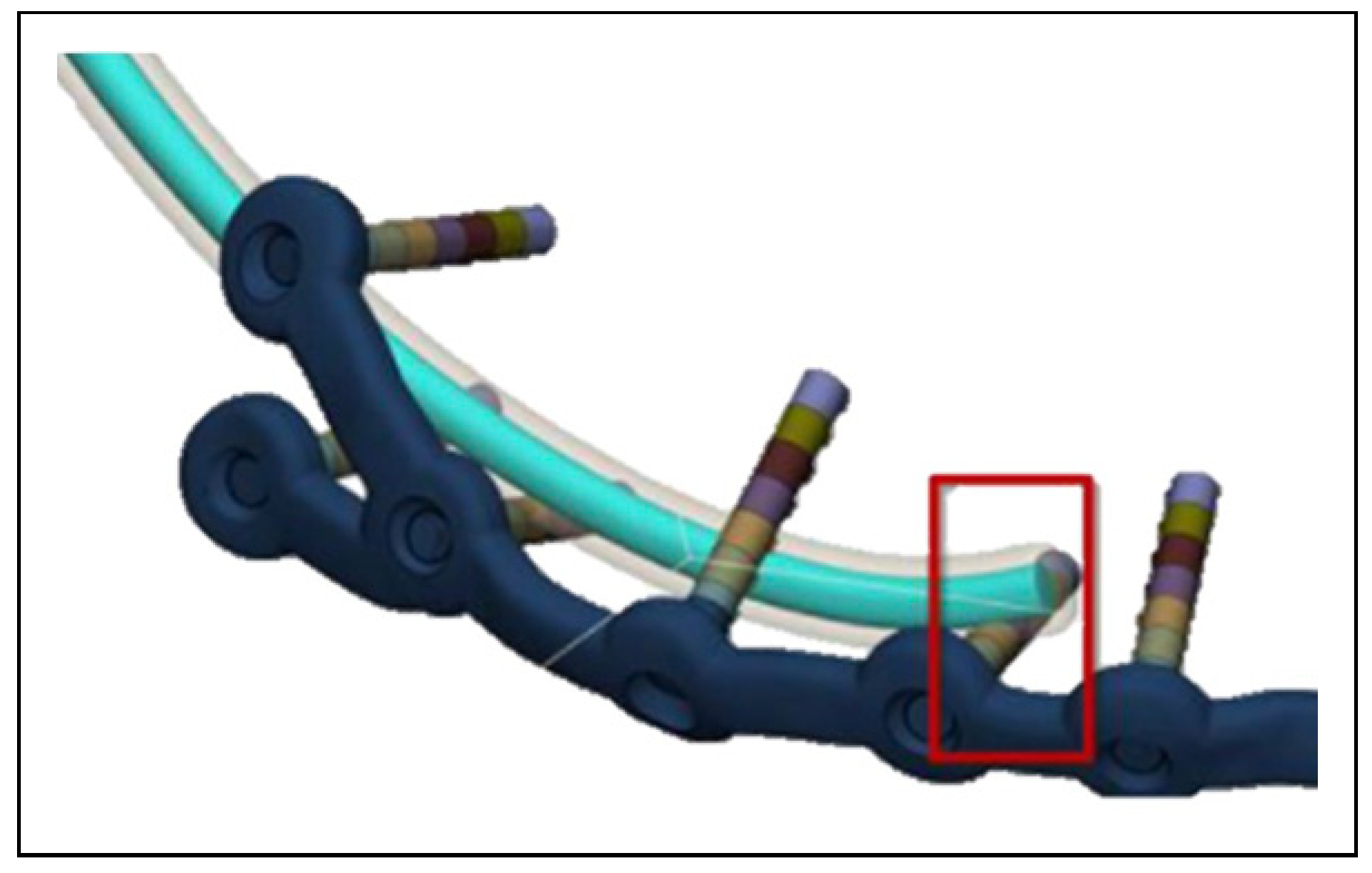
Once satisfactory virtual reduction was obtained, an implant was designed to conform to the patient’s unique mandibular anatomy and fracture pattern while limiting interference in the areas that a future dental prosthesis would seat. The drilling guides and PSI were designed to avoid the IAN and allow for screw fixation in the areas of the best remaining bone stock (
Figure 1 and
Table 1).
Several factors must be considered to enhance the intraoperative adaptation of guides and implants to the mandible. Discrepancies may arise between the patient’s anatomy at the time of surgery and when the preoperative imaging was taken. To capture the true anatomy, it is essential to obtain high-resolution CT scans with a slice thickness of less than 1 mm. Additionally, the surgery should be scheduled within a reasonable timeframe to avoid further physiological changes and degradation of the fractured mandible.
The design of drilling guides is a critical aspect of custom mandibular surgery, ensuring the virtual surgical plan is precisely replicated in the operating room. If the guides are incorrectly seated, the final implant will be inappropriately positioned. Therefore, guides should be designed to closely fit unique anatomical features to aid in positioning, despite slight variations that may be encountered. Guides can include registration tabs that wrap around the mandibular borders or align with stable anatomic landmarks such as the mandibular angle, ramus, or coronoid notch. This design ensures the guide is positionally unambiguous and eliminates any unwanted rotational movements that could result in incorrect seating.
Guides can be manufactured from either titanium or polyamide. The titanium variant is typically lower profile and more resistant to deforming forces, whereas polyamide guides offer the flexibility to be trimmed or adjusted intraoperatively to ensure proper alignment.
Another crucial element for ensuring accurate placement of guides and implants is the use of a 3D printed model. This enables the surgeon to thoroughly visualize and assess the fit of the guide or implant on the model, confirming correct seating in vivo.
Patients D and E presented with infected fractures and paresthesia within the IAN distribution at the time of initial consultation. In cases that require more extensive debridement with resultant continuity defects, resection margins can be virtually planned and incorporated into the drilling/cutting guide. The PSIs for both patients were also designed with a crib to span the area of discontinuity and aid in supporting a bone graft (
Table 1). Plate thickness ranged from 2.0–2.4 mm for all patients in accordance with the principles of load-bearing osteosynthesis.
Surgical Technique
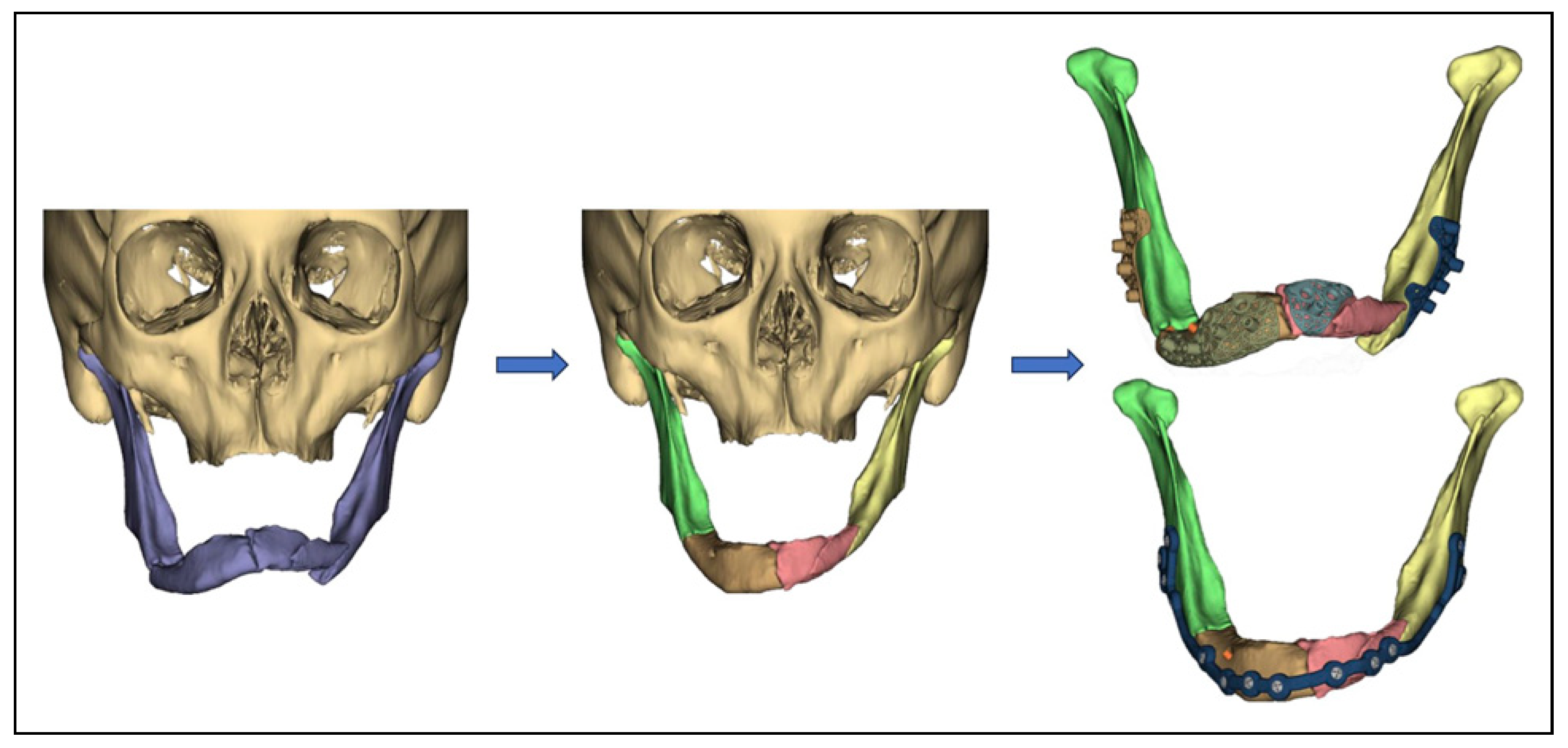
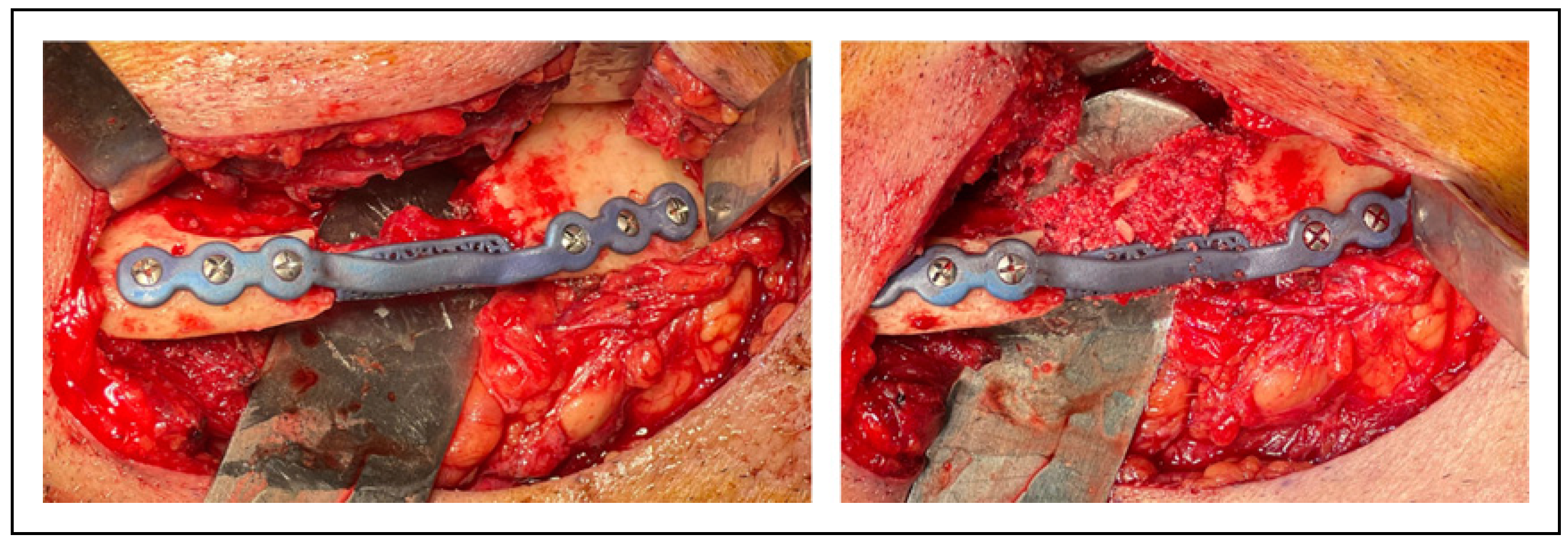
All patients were treated via an extraoral approach. The fracture segments were mobilized and debridement was performed as needed to remove intervening fibrous tissues to allow for appropriate reduction. The prefabricated guides were positioned onto the mandibular fracture segments and the predictive screw holes were drilled (
Figure 2).
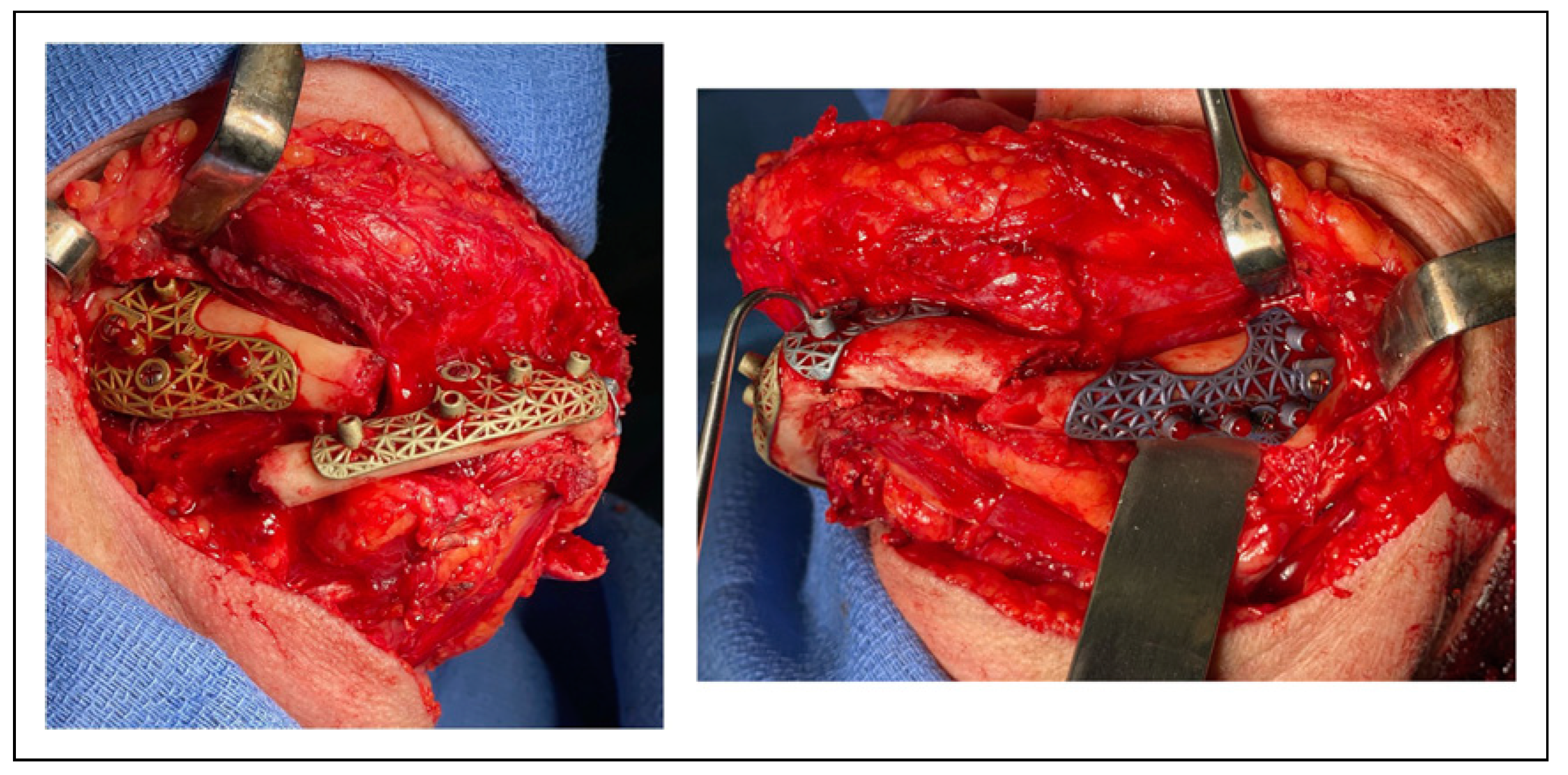
In the cases of patients D and E, the guides were placed and resection of the bony margins was performed. The guides were removed and the implants were placed with appropriate alignment of the predictive screw holes. The PSIs were subsequently fixated with bicortical screws. Bone grafting was performed in a similar fashion for patients A-D, utilizing bone marrow aspirate concentrate (BMAC) harvested from the right hip, combined with bone morphogenetic protein on an acellular sponge and allograft (
Figure 3). Patient E received a combination of Vivigen (LifeNet Health, Virginia) and platelet rich fibrin (PRF) at the site of fracture.
Postoperative Analysis
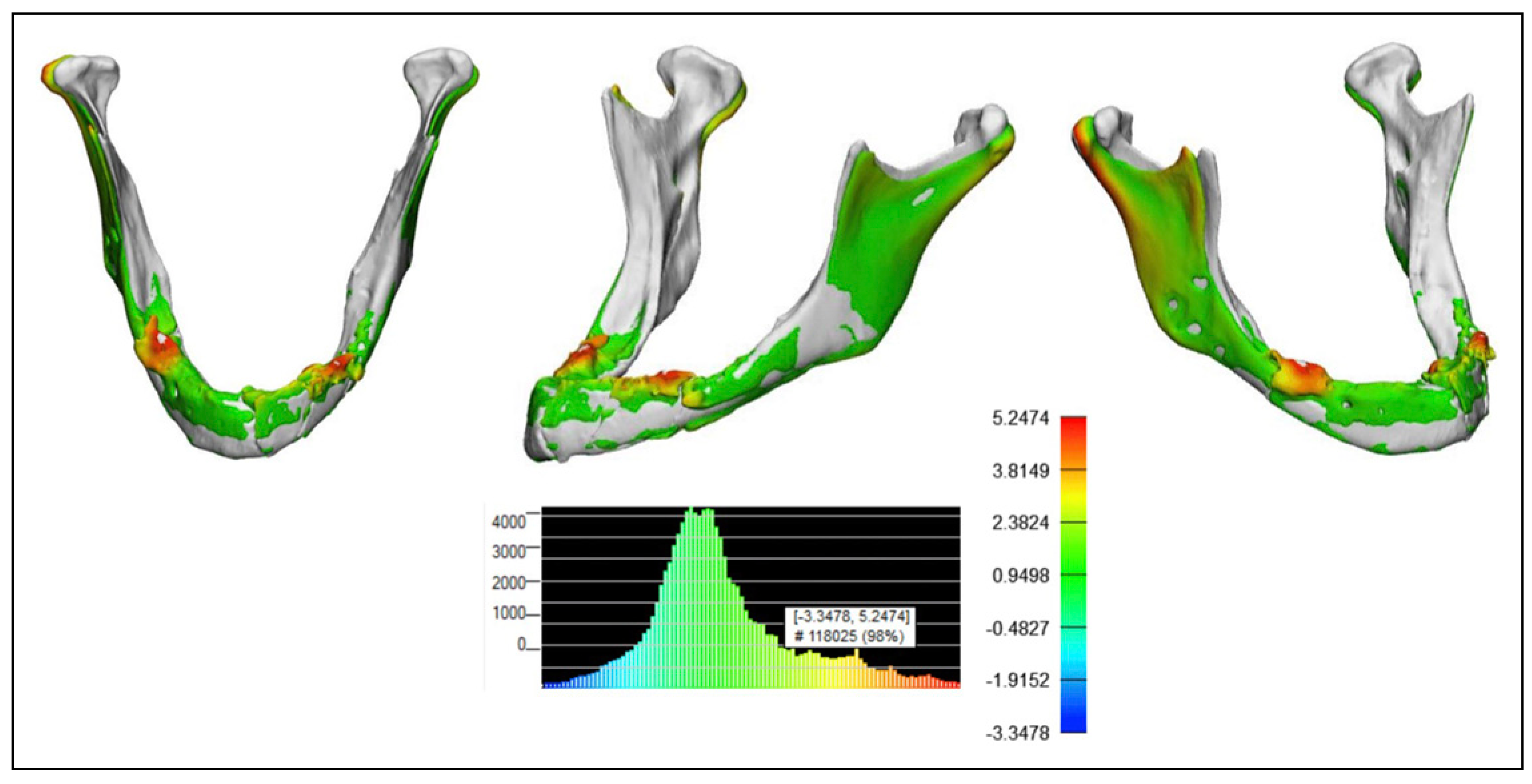
The post-operative CT scan is converted into a DICOM file and subsequently uploaded to a clinical software engineer (Materialise, Belgium) in order to assess the accuracy of the operative reduction. The images undergo a segmentation process and are rendered into a three-dimensional representation. These images are then integrated into the Materialise 3-matic
® design optimization software, which is equipped with advanced features. This software enables the overlay of postoperative images with the pre-planned positions, facilitating a detailed analysis of any deviations between the 2. Heat mapping analysis was then used to assess the accuracy within 2.0 mm of the planned position. An overlay of the plate position and the mandibular position can give a visualization of the accuracy as well (
Figure 4).
Discussion
Edentulous mandible fractures are a unique entity with treatment decisions that are highly patient dependent and warrant careful consideration. A nuanced approach is essential to ensuring optimal patient outcomes. The purpose of this case series is to highlight the numerous advantages of VSP and PSIs compared to other treatment modalities (
Box 1).
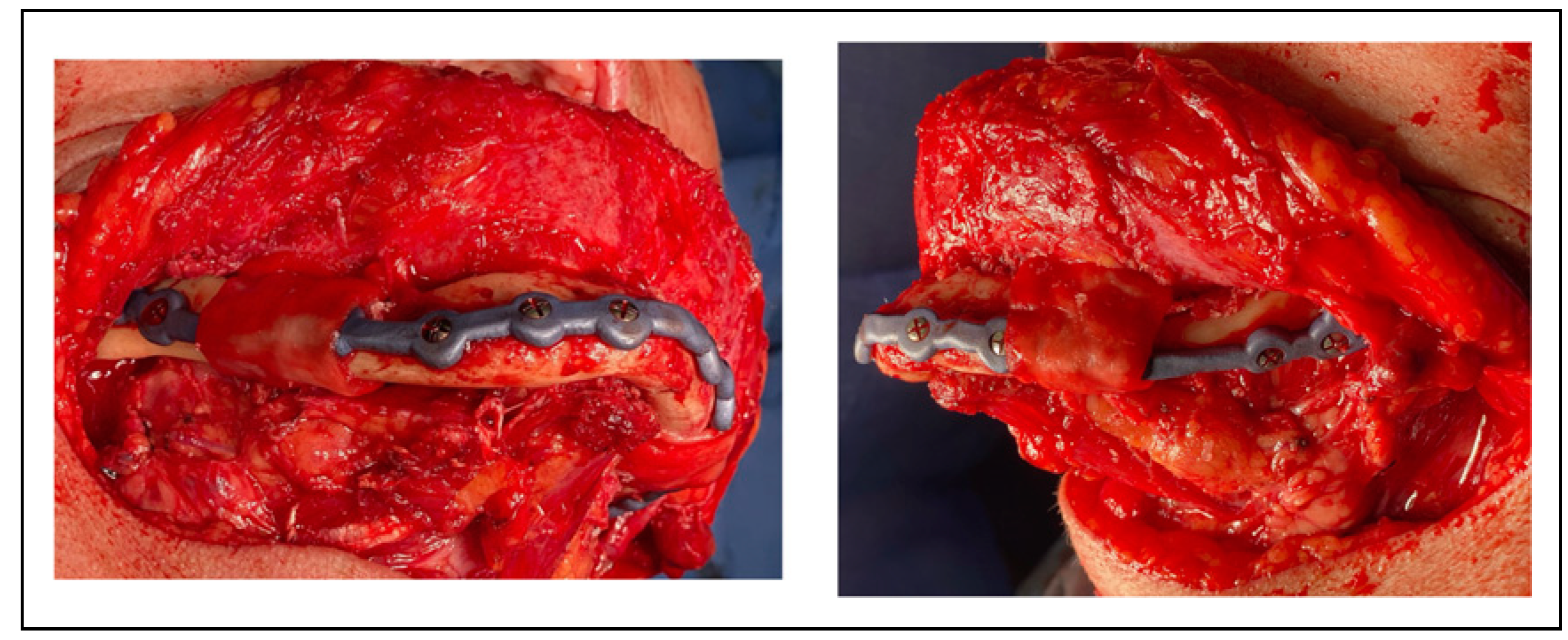
Box 1. Advantages of custom printed plates for atrophic mandible fractures.
The patient cohort under review mirrors the demographic profile observed in previous studies, typified by an advanced age averaging 66.4 years, a high prevalence of multiple comorbidities, and a predominant etiology of falls [
1]. Duration of hospitalization ranged from 1–3 days; patient C required inpatient rehabilitation and was awaiting an available bed at the accepting facility, delaying her discharge.
One of the considerations when deciding to use PSIs is the length of time to treatment as there is a period needed for design and fabrication. The turn-around time varies, but generally 7–10 days are needed to obtain a PSI. For 3 of the 5 patients the length of time from consultation to treatment was 6 weeks or less. Hospitalization was not required for any of the patients after the initial consultation. Pain medication was prescribed as needed prior to surgery and a blenderized “non-chew” diet was recommended. Patients A and B, both experiencing homelessness and significant social and financial challenges, faced considerable barriers in accessing care. They were both lost to follow-up several times, before ultimately returning to continue treatment.
The follow-up period in this series is varied and ongoing. The average follow-up thus far has been 5.4 months with a range of 2–8 months. There were no complications reported at the time of surgery nor at the last follow up visit. There were no wound dehiscences, infections, hardware failures, or facial nerve injuries. Patients D and E remained paresthetic in the left IAN distribution, with slight improvement from the preoperative examinations.
Post-operative analysis was completed for all patients. There was no violation of the nerve canal by any of the screws. Again, one of the benefits of VSP is determining the various angulations for bicortical screw placement to avoid the nerve canal (
Figure 5).
The condylar position can also be assessed on the postoperative analysis. A large benefit of VSP is the ability to appropriately seat the condyles while aligning the fracture segments and mitigating improper torquing. The percentage of mandibular overlay within 2 mm between the planned and postoperative states ranged from 63% to 98%. Four of the cases had greater than 87% of overlay. In the case of Patient D, the degree of overlay was expected to be lower as the patient previously underwent ORIF at an outside institution and experienced a plate fracture. The presence of hardware on the preoperative CT obscured the underlying bony anatomy introducing a level of inaccuracy. The fracture was also infected and required resection of both the proximal and distal margins with a resulting continuity defect.
There are several options to treat edentulous mandible fractures in an open fashion. Certain practitioners advocate for the use of mini-plates as it allows for an intra-oral approach and less periosteal dissection [
7]. The downsides of this technique is that it is semi-rigid fixation and often leads to displacement/fracture of the small plates during function. The minimal dissection may also lead to malalignment of the fracture segments due to decreased visualization.
The current AO guidelines recommend load-bearing osteosynthesis with bicortical screw fixation given the lack of bony buttressing. Reconstruction plates can be cumbersome and are difficult to perform nuanced bends in, making positioning challenging. This is made even more demanding when accounting for the position of the IAN and future prosthetic rehabilitation. The use of VSP and PSIs can help to overcome many of these obstacles, while minimizing the risk of surgical complications and decreasing the time under anesthesia in this vulnerable patient population.
Conventional open surgical approaches can be employed in custom mandibular surgery. To accommodate the specific design and orientation of the drilling guides and custom hardware, surgeons may need broader exposure than what traditional non-custom methods dictate. This alteration may be necessary to adequately visualize key anatomic landmarks that are critical in positioning the guides accurately and securing the plates properly. One of the benefits of VSP, is that the guides can be tailored to account for access issues and in certain cases can diminish the need for extensive dissection due to a more targeted and precise approach.
Four of the patients had printed PSIs and 1 patient had a milled PSI. Milled plates are stronger than their printed counterparts and can also accept locking screws. However, design options are limited for milled plates and generally require a linear design. Printed PSIs have significantly greater design options, which is a huge asset when accounting for appropriate fracture reduction, eluding the IAN, and avoiding future prosthetic interferences.
There are a few studies that have described the utilization of VSP coupled with in-house 3D printing of an anatomically reduced mandibular model, allowing for the pre-bending of a reconstruction plate prior to surgery [
8,
9]. As the 3D printing is completed in house and a stock plate is utilized, there is minimal turnaround time and thus decreased delay in getting the patient to surgery. Theoretically, intraoperative time should also be decreased, as plate bending is completed preoperatively.
However, it’s important to consider the mechanical implication of bending a stock plate, as the strength and stability of metals decrease with the degree and frequency of bending. Printing a model of the mandible and pre-bending a stock reconstruction plate still carries the risk of overbending and weakening the plate. This technique also does not account for the angulation and placement of the fixation screws so as to avoid injury to the IAN. By using a printed or milled PSI, the strength of the plate remains uncompromised resulting in a decreased risk of plate fracture and IAN injury. As previously discussed, one of the challenges of severely atrophic mandible fractures is the lack of anatomical landmarks. Without drilling guides that are uniquely designed to adapt to the mandible, the provider may still have difficulty correctly reducing the fracture segments into the correct orientation despite having a pre-bent plate.
Dental rehabilitation is of the utmost importance following these fractures, hinging on plate positioning and achieving bony union. VSP allows for the implant to be designed to adapt to the lateral surface or inferior border of the mandible at different locations to avoid interfering with a future removable prosthetic. An additional benefit is the ability to incorporate a crib into the design of the implant, spanning any continuity defects, and helping to stabilize a bone graft (
Figure 6).
There are limitations to this technique with one of the largest concerns involving the cost. While the authors agree that cost should be considered and should not be a barrier to treatment, severely atrophic edentulous mandible fractures are rare. Many of the challenging nuances involved in these cases can be overcome with utilization of VSP/PSI, making the increased cost worth it in the most difficult cases. There is also a delay in treatment due to the turnaround time for fabrication of the PSI. There is rarely an indication to emergently treat these fractures and an additional week of delay is usually not clinically relevant.
This is the first case series describing the workflow for management of atrophic mandible fractures utilizing PSIs with post-operative analysis. There are numerous benefits to this technique and given the relative infrequency of these fractures, the authors feel that the increased cost in these specific cases is worth consideration.