Abstract
Study Design: A retrospective study. Objective: The Markowitz-Manson classification system categorizes nasoorbitoethmoid (NOE) fractures by severity of injury and remaining integrity of the medial canthal tendon. However, this system does not account for direction of bony displacement (in-fracture vs out-fracture), which can greatly affect symptomatology and management. We hypothesize that NOE fractures will present differently based upon their severity: Type I injuries are likely to present with medial nasal bone displacement (in-fracture), whereas Type III fractures will be more prone to lateral displacement (out-fracture). Methods: A retrospective review was performed for all patients with NOE fractures who were evaluated by the plastic surgery department at a level 1 trauma center over a 6-year period. Computed tomography data were evaluated to assess for directionality of fracture segment displacement. Frequencies of medial, lateral, and non-displacement across NOE types were compared by Chi-Squared Goodness of Fit and Fisher’s Exact Tests. Results: 111 patients met inclusion criteria. The patient population was 73.9% male and averaged 51.2 years old. When bilateral fractures were counted independently, there were 141 cases in total: 115 Type I, 20 Type II, and 6 Type III. Type I fractures were most commonly in-fractured (48.7%), while Type III injuries were consistently out-fractured (100%) (p < .001). Conclusions: While Type II and III NOE fractures have dominated clinical focus, this study highlights the prevalence of impaction within Type I fractures. These findings advocate for a more comprehensive approach to the evaluation of Type I NOE fractures and their potential risks, including traumatic hypotelorism and nasal airway obstruction.
Introduction
The nasoorbitoethmoid (NOE) complex includes the delicate confluence of nasal bones, ethmoid bone, frontal processes of the maxilla, and medial orbital walls at the central midface.[1] Fractures to this area represent one of the most complex challenges in maxillofacial trauma due to the intricate anatomy and function of the structures involved. Such injuries can result in notable nasal and orbital deformities, which may lead to impairments such as telecanthus, enophthalmos, nasal airway obstruction, diplopia, epiphora, and even vision loss.[2,3] Additionally, the NOE complex’s proximity to the cranial base increases the risk for complications such as cerebrospinal fluid (CSF) leak and intracranial involvement.[4]
Injuries to this area are often caused by high-impact, blunt force trauma. Common mechanisms include physical assault following direct blows to the face, falls, and sports injuries.[5,6,7] In the past, motor vehicle accidents were one of the leading causes, particularly in cases where individuals were unbelted and the bridge of their nose was smashed by the steering wheel.[8] Today, while still common, the frequency of NOE fractures due to road collisions has progressively declined given the widespread implementation of seatbelts and airbags.[9]
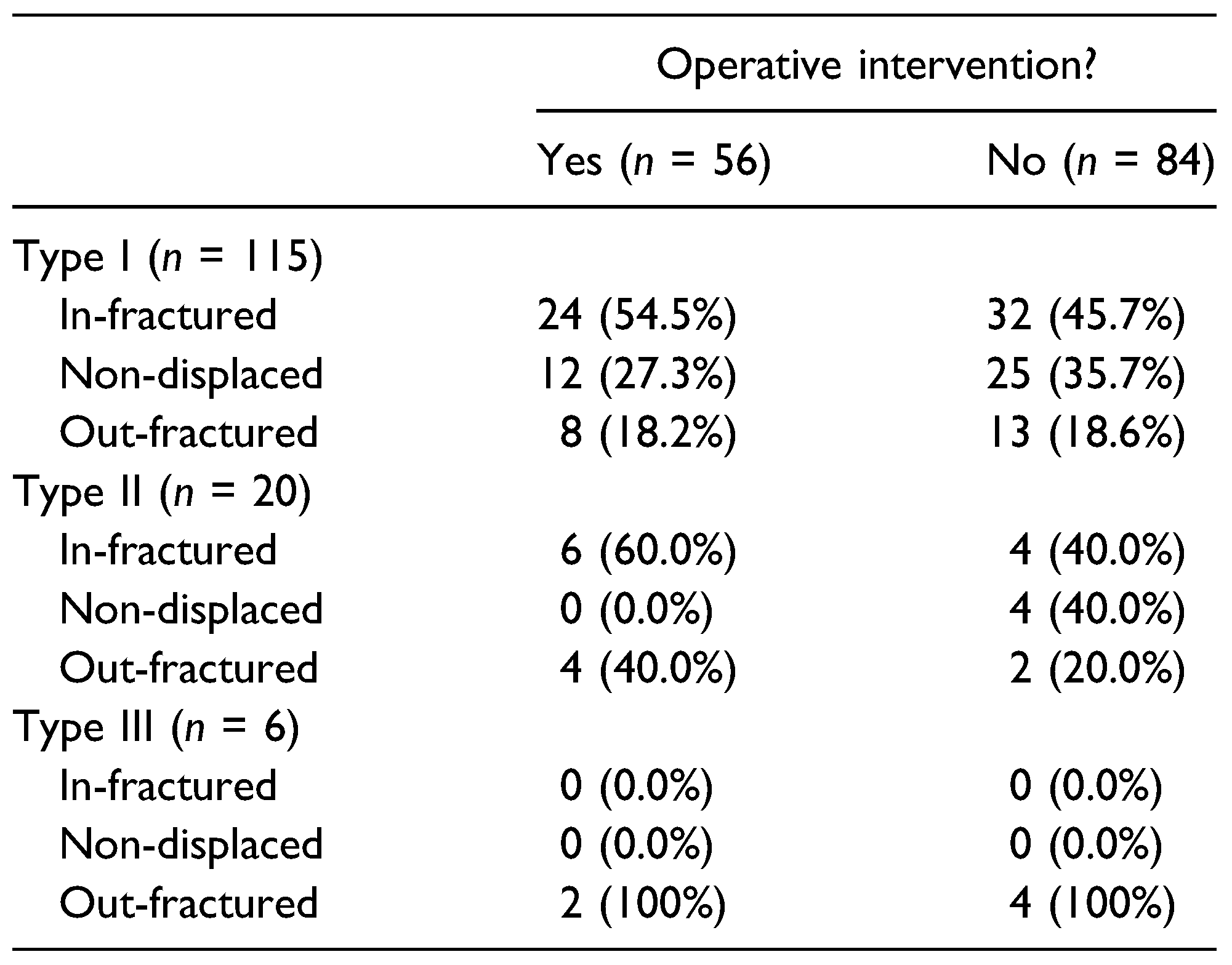
The Markowitz-Manson classification system is commonly used for categorizing traumatic injuries to the NOE complex. This schema divides NOE fractures into three subtypes depending on the integrity of the medial canthal tendon (MCT), which is a strong, fibrous band of tissue that connects the medial portion of the eyelid to the bones of the medial orbit.[5] Type I fractures are characterized by an intact MCT that remains attached to a single large bone fragment.[10] Type II fractures present with canthal attachment to a smaller comminuted bone segment, while Type III fractures are defined by comminution that extends to the MCT insertion site, causing avulsion of the tendon itself.[10] The three fracture subtypes are depicted in Figure 1. Categorically, bilateral fractures are classified according to the more severe side.[1]
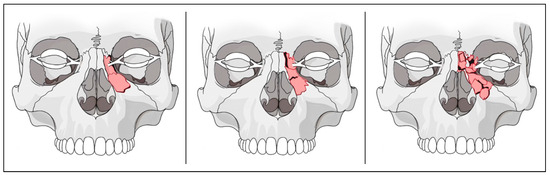
Figure 1.
These illustrations demonstrate the Markowitz-Manson classification scheme. (Left) A Type 1 fracture, where the medial canthal tendon (MCT) remains attached to a large central bone fragment; (middle) a Type II fracture, where the bone fragments are comminuted but the MCT remains intact; and (right) a Type III fracture, where the bony fragments are comminuted and the MCT is avulsed.
The Markowitz-Manson system is useful for describing the extent of comminution of bone. However, the schema does not account for direction of bony displacement, which can greatly affect symptomatology. Lateral displacement of nasal bone fragments (out-fracture) can result in traumatic telecanthus, requiring surgical correction with the placement of a transnasal wire.[11] Less commonly discussed, though more commonly presenting, are the consequences of medial displacement of bone (in-fracture). Such impaction injuries may cause an entirely different set of symptoms, most notably nasal airway obstruction. This study aims to systematically assess directional patterns of bony displacement in NOE fractures and correlate these findings with the Markowitz-Manson criteria to better understand the impact of displacement direction on clinical outcomes.
Methods
A retrospective review of a prospectively maintained Research Electronic Data Capture (REDCap) database was performed for all patients with NOE fractures who were evaluated by the plastic surgery department at a level 1 trauma center over a 6-year period. Approximately 80% of the institution’s facial trauma call is handled by the plastic surgery service, making the database a robust sampling of the facial injuries seen at this institution.[12] Data collection consisted of electronic medical record (EMR) review and computed tomography (CT) analysis. The study adhered to all pertinent institutional research policies and was carried out after Institutional Review Board approval.
Electronic Medical Record Review
All patients with diagnosed NOE fractures were evaluated for this study regardless of mechanism of injury or age. Patients less than 18 years of age were excluded given notable differences in pediatric facial trauma epidemiology, management, and treatment.[13,14,15,16,17] Patient demographic data, such as date of birth, date of presentation, sex, mechanism of injury, and decision for operative management, were documented from the medical record. Inclusion criteria required the presence of the words, “naso-”, “orbito-”, “ethmoid-”, “NOE”, or any combination thereof in relevant radiological, operative, or plastic surgery consult notes. NOE fractures reported as part of a larger set of panfacial injuries were included. Exclusion criteria included any prior history of facial trauma or facial fracture fixation due to risk of prior interventions affecting central fragment displacement.
Computed Tomography Analysis
Inclusion criteria required that patients had high resolution CT imaging of the facial skeleton with axial, sagittal, and/or coronal slices measuring less than 1 mm. Exclusion criteria included extensive motion artifact or imaging volumes that did not capture the facial skeleton in its entirety. Relevant axial, coronal, and three-dimensional reconstructions were reviewed by a senior surgeon and trained plastic surgery resident for each patient. All fractures were classified according to the Markowitz-Manson criteria. For comminuted fractures, radiography was correlated with the EMR to differentiate Type II and Type III injuries. Following classification of fracture type, all injuries were categorically subclassified by the directional displacement of the central fragment relative to the nasofrontal junction. Possible vectors included nondisplaced, in-fractured (also referred to as “medially displaced” or “impacted”), or out-fractured (also called “laterally displaced” or “blown out”). All bilateral facial fractures were treated as two distinct, unilateral fractures.
Outcome Measures and Statistical Analysis
Cohort demographics and patient characteristics were summarized using descriptive statistics. Primary outcomes included NOE fracture subtype and direction of central fragment displacement, while secondary outcomes included whether operative intervention was pursued. Given that all collected Type III NOE fractures were out-fractured, the Chi-Squared Goodness of Fit test was used to compare the significance of out-fracture frequency among all three subtypes. Fisher’s Exact Test was then separately used to assess the association of central fragment directionality (infracture, non-displaced, and out-fracture) among NOE subtypes I and II. All data were analyzed using R (R Core Team, 2020, The R Foundation for Statistical Computing, Vienna, Austria) and RStudio (RStudio Team, 2020). Results were considered significant at a P-value <.05.
Results
We identified a total of 158 NOE patients managed by the plastic surgery service over a 6-year period. Overall, 111 eligible patients were included; 47 were excluded due to missing data, insufficient high-resolution CT imaging, or history of prior facial trauma. The patient population had an average age of 51.2 ± 21.8 years. The youngest patient was 21 years old and the oldest was 98 years old. The population was 26.1% female and 73.9% male. Cohort demographics are recorded in Table 1. Among the 111 patients, 29 (26.2%) had unilateral right NOE fractures, 52 (46.8%) had unilateral left NOE fractures, and 30 (27.0%) had bilateral fractures. When bilateral fracture cases were treated independently, there were 59 (41.8%) right NOE fractures and 82 (58.2%) left NOE fractures in total. In total, this study included 141 fractures present among the 111 included patients. For all subsequent analyses, bilateral NOE fractures were treated as two distinct unilateral entities.

Table 1.
Patient Demographics and Clinical Data. When Bilateral Fracture Cases Were Treated as Two Distinct Unilateral Fractures, There Were 59 (41.8%) Right NOE Fractures and 82 (58.2%) Left NOE Fractures in Total.
Despite recent declines, motor vehicle accidents remained the most common cause of NOE injury overall (34.8%), followed by falls (26.2%), assault (21.3%), other blunt-force trauma (16.3%), and ballistic injuries (1.4%). Type I fractures comprised the vast majority of all cases (81.6%), followed by Type II (14.2%), then Type III (4.2%) (Table 2). Fracture subgroups (Type I, II, or III) were then broken down by direction of central fragment displacement. Type I fractures were predominantly in-fractured (48.7%), followed by non-displaced (33.0%), and out-fractured (18.3%). Type II fractures were similarly predominantly in-fractured (50%). The remaining 50% of Type II injuries were split between non-displaced (20%) and out-fractured (30%). Three-dimensional reconstructions showing an infractured Type I NOE injury and an out-fractured Type III injury are shown in Figure 2. Although Type I fractures were predominantly in-fractured, there was no significant association between central fragment directionality and fracture subtype due to limited sample size (p = .386). Type III injuries were entirely out-fractured (100%) (p < .001) (Figure 3 and Figure 4).

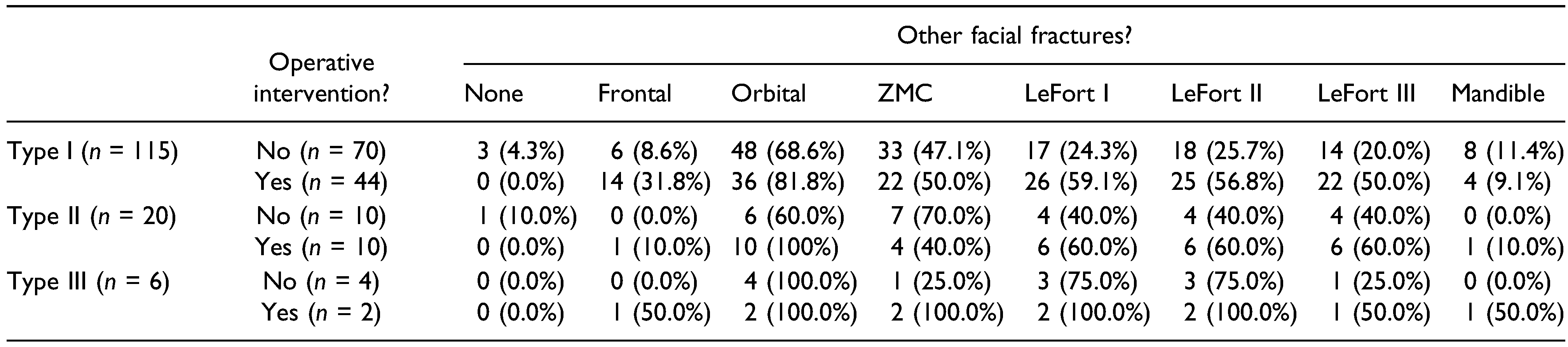
Table 2.
Distribution of NOE Fracture Subtype by Central Fragment Vector Displacement, Mechanism of Injury, and Operative Intervention. All Bilateral NOE Fractures Were Treated as Two Distinct Unilateral Fractures, Giving 141 Total Observations. One Operative Intervention for Type 1 was Not Recorded in the EMR. Distribution of NOE Fracture Subtype by Central Fragment Vector Displacement, Excluding All Nondisplaced Fractures.

Figure 2.
3D reconstructions with red arrow showing (A) an in-fractured central fragment in a Type I NOE injury (left side) vs (B) an outfractured central fragment in a Type III NOE injury (right side).

Figure 3.
Graph showing breakdown of central fragment directionality by Markowitz-Manson NOE subtype.

Figure 4.
Graph showing breakdown of Markowitz-Manson NOE subtype by central fragment directionality.
In total, fifty-six fractures (39.7%) were operatively managed (Table 3). Among these, 30 were in-fractured (53.6%), 12 were non-displaced (21.4%), and 14 were out-fractured (25.0%). All operative cases, across all three subtypes, had at least one other facial fracture, frequently influencing the decision to operate (Table 4).

Table 3.
Operative Intervention by Central Fragment Directionality. One Operative Intervention for Type I was Not Recorded in the EMR and Thus Excluded From Analysis.

Table 4.
Breakdown of Operative Intervention by Association With Other Facial Fractures. Note That Many Patients had Pan-Facial Fractures and Thus Percentages Across Rows are Often Greater Than 100%.
Type I Fractures
Type 1 fractures were predominantly in-fractured (48.7%), followed by nondisplaced (33.0%), and out-fractured (18.3%). When only displaced fractures were considered, 72.7% of injuries were in-fractured and 27.3% out-fractured. These large segment NOE fractures were most commonly caused by motor vehicle accidents (32.2%) and falls (29.5%), followed closely by assault (21.7%) and other forms of blunt trauma (15.7%). The majority of Type I fractures (60.9%) were managed non-operatively (Table 2). Among the 44 operative cases, 24 (54.5%) were in-fractured, 12 (27.3%) were non-displaced, and 8 (18.2%) were out-fractured (Table 3). Each of the non-displaced cases had concomitant facial injuries that served as indications for intervention. Operative management for one non-displaced Type I case was not recorded and thus excluded from analysis. Among these operative cases, 36 (81.8%) had a concurrent orbital fracture, 26 (59.1%) had a LeFort I fracture, 25 (56.8%) had a LeFort II fracture, 22 (50.0%) had a LeFort III fracture, 14 (31.8%) had a frontal bone fracture, and 4 (9.1%) had a mandible fracture (Table 4).
Type II Fractures
Type II fractures were predominantly in-fractured (50.0%) as well, followed by out-fractured (30.0%), and nondisplaced (20.0%). When only displaced fractures were considered, 62.5% of injuries were in-fractured and 37.5% were out-fractured. Type II fractures were most commonly caused by motor vehicle accidents (50.0%), assault (25.0%), and other forms of blunt trauma (20.0%). Only one Type II fracture was due to a fall. When compared to the Type I subgroup, exactly half of all Type II injuries were managed operatively (50.0%) (Table 2). Among operative cases, six (60.0%) were in-fractured, none (0.0%) were nondisplaced, and four (40.0%) were out-fractured (Table 3). Among these operative cases, 10 (100%) had concurrent orbital fractures, 6 (60.0%) had LeFort I fractures, 6 (60.0%) had LeFort II fractures, 6 (60.0%) had LeFort III fractures, and 1 (10.0%) had a mandibular fracture (Table 4). The injury patterns noted above were not mutually exclusive.
Type III Fractures
Type III fractures were the least common subtype (4.2%). All cases were out-fractured with significant lateral displacement (100%). These patients were largely injured by motor vehicle accidents (33%) and falls (33%). Interestingly, only two of the six fractures (33.3%) were managed operatively: two of the remaining fractures were attributed to patients who refused surgery in favor of conservative management. The final two fractures were attributed to a single patient who did not undergo surgery due to the severity of his associated brain injuries and who expired shortly thereafter. Of the operatively managed cases, all had concurrent orbital, ZMC, and LeFort fractures (Table 4).
Discussion
The original classification scheme for NOE injuries by Markowitz and Manson places an emphasis on identifying fracture cases where the central fragment is completely displaced or obliterated.[10,18] In the most extreme cases, disrupted structural support for the medial canthal tendon leads to lateral displacement of the fractured medial orbit.[1,5] This may result in a rounded eye shape where the orbits appear too far apart, referred to as traumatic telecanthus. Such cases need to be addressed in a timely fashion and require complex surgical intervention,[1,2,5] which has led to an overwhelming emphasis in the literature on the identification and management of Type II and III NOE fractures. Given the historic focus on the more severe type of NOE trauma, it is easy to forget that Type I injuries are the most common.[12,16,19] This subtype typically results from lower-energy impacts compared to Types II and III, which are rarer due to the greater force required to cause such extensive damage: Type II NOE fractures are thought to comprise less than 30% of all NOE cases, while Type III fractures are the rarest, making up less than 5%.[1,3,20,21,22,23] Yet even with this overwhelming frequency, less focus has been directed towards the management of Type I fractures due to their (typically) lower degree of clinical severity. Since Type I fractures are non-comminuted, management may include closed reduction to manipulate the affected bone segments back into proper alignment.[1,6] However, the predominance of impaction injury within this subtype points us towards an underrecognized and nuanced medial displacement of the central fragment and MCT into the nasal airway, with the potential risk of hypotelorism, facial numbness secondary to compression of the infraorbital nerve, and restricted nasal airflow.[24] This frequency of medial displacement stands in contrast to the presumed lateral displacement more traditionally associated with NOE fractures: in-fractures in this study made up 46.8% of displaced fractures overall, whereas out-fractures only comprised 23.4%. Indeed, this is even more significant in the less severe Type I injuries, with nearly 3/4s (72.7%) of displaced fractures determined to be in-fractured in nature.
Furthermore, the interaction between these fracture patterns and other associated facial injuries adds of a layer of complexity to the management of NOE fractures. In this study, all recorded fractures were associated with at least one other fracture of the mandible, midface, or frontal bones. In scenarios where other midfacial trauma is present, the structural integrity of the facial skeleton may be compromised, which can predispose to the development of certain fracture lines over others. For example, the presence of additional midface injuries could potentially favor the occurrence of out-fractures due to reduced structural support against impacting forces, leading to a higher likelihood of lateral displacement. This relationship highlights the importance of a comprehensive assessment of all facial injuries in patient with NOE fractures, as understanding the full extent of trauma can significantly influence treatment approach. This interplay also suggests that fracture pattern might not only be a direct consequence of initial impact, but also a result of the interplay with other facial injuries.
The findings described above serve to highlight the fact that NOE injuries are more nuanced than the typical didactics describing unstable fracture patterns presenting with characteristic traumatic telecanthus and lateral structural displacement. Instead, it is worthy of note that thirty percent of NOE fractures were nondisplaced. Among the others, however, two thirds of displaced fractures presented in an in-fractured pattern, with a different set of clinical findings from those of traditional teaching. Nasal airway obstruction is the most common complaint following such injuries, also frequently presenting with infraorbital nerve compression and mild hypotelorism. This presentation is also more common among Type I injuries (nearly 75%), whereas all Type III cases presented in the classic out-fractured pattern. In-fracture vs out-fracture also appeared to be significantly associated with the presence of concomitant injuries, which were present in all patients within the study. It stands to reason that an isolated Type I injury would most likely be infractured, whereas one coupled with a laterally displaced zygomatic complex might instead become out-fractured due to the loss of a stabilizing buttress.
It is important to note the limitations of the present study. First, approximately 20% of all potential patients were excluded from this study due to being managed by other services within the trauma center, resulting in a dataset that may not fully represent the entire spectrum of NOE fracture evaluation and management at our institution. Moreover, an additional 30% of patients within this subset were then excluded due to inadequate CT scans, incomplete records data, or prior facial trauma. This further narrows the available cohort and may introduce selection bias, as the included patients again may not be representative of the broader population. Both of these limitations are compounded by a relatively small sample size, which notably affects the statistical power of the study. As a result, some of the included findings were not statistically significant, limiting the confidence with which these results can be applied to clinical practice.
More broadly, the study’s retrospective nature and reliance on a single institution’s database limits the generalizability of these findings, especially since different institutions may serve different demographic populations. For example, most patients in this study suffered blunt trauma to the face, with only a small percentage experiencing ballistic injuries. Additionally, while the classification systems employed are useful for describing fracture severity and direction of bony displacement, they do not fully account for the multifaceted context of these injuries. As shown above, many NOE fractures occur as part of panfacial fractures in a larger trauma setting. Finally, this study was also limited in regard to the diversity of bony displacement direction within each fracture subtype. Further research should aim to include a broader, multi-center data pool and correlate findings with specific clinical outcome measures to provide a more holistic understanding of NOE fractures and their management.
Conclusion
This study offers a comprehensive analysis of NOE fractures, emphasizing the range of clinical presentations based on the Markowitz-Manson system and direction of central fragment displacement. Type III NOE fractures often dominate the literature due to their association with traumatic telecanthus and need for complex surgical intervention. Indeed, this study confirms an overwhelming predominance of lateral displacement within this subtype. However, it is crucial to recognize that the majority of NOE cases fall within the simpler Type I pattern. Our findings indicate a more common incidence of medial bone displacement within Type I injuries, with a different presentation characterized by nasal airway obstruction and traumatic hypotelorism. These observations suggest that the clinical significance of in-fractured NOE injuries may be underrecognized, warranting closer attention to their assessment and management.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Nguyen, M.; Koshy, J.C.; Hollier, L.H. Pearls of Nasoorbitoethmoid Trauma Management. Semin. Plast. Surg. 2010, 24, 383–388. [Google Scholar] [CrossRef]
- Han, P.S.; Kim, Y.; Herford, A.S.; Inman, J.C. Complications and Treatment of Delayed or Inadequately Treated Nasoorbitoethmoid Fractures. Semin. Plast. Surg. 2019, 33, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Becelli, R.; Renzi, G.; Mannino, G.; Cerulli, G.; Iannetti, G. Posttraumatic Obstruction of Lacrimal Pathways: A Retrospective Analysis of 58 Consecutive Naso-Orbitoethmoid Fractures. J. Craniofacial Surg. 2004, 15, 29–33. [Google Scholar] [CrossRef]
- Balaraman, K. Frontal and naso-orbito-ethmoid complex fractures. In Oral and Maxillofacial Surgery for the Clinician; Bonanthaya, K., Panneerselvam, E., Manuel, S., Kumar, V.V., Rai, A., Eds.; Springer Nature: Berlin, Germany, 2021; pp. 1251–1266. [Google Scholar] [CrossRef]
- Goodmaker, C.; Hohman, M.H.; De Jesus, O. Naso-orbito-ethmoid fractures. In StatPearls; StatPearls Publishing: St. Petersburg, FL, USA, 2023; Available online: https://www.ncbi.nlm.nih.gov/books/NBK557468/ (accessed on 14 August 2023).
- Baril, S.E.; Yoon, M.K. Naso-orbito-ethmoidal (NOE) fractures: a review. Int Ophthalmol Clin. 2013, 53, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Rosenberger, E.; Kriet, J.D.; Humphrey, C. Management of nasoethmoid fractures. Curr. Opin. Otolaryngol. Head Neck Surg. 2013, 21, 410–416. [Google Scholar] [CrossRef]
- Roden, K.S.; Tong, W.; Surrusco, M.; Shockley, W.W.; Van Aalst, J.A.; Hultman, C.S. Changing Characteristics of Facial Fractures Treated at a Regional, Level 1 Trauma Center, From 2005 to 2010: an assessment of patient demographics, referral patterns, etiology of injury, anatomic location, and clinical outcomes. Ann. Plast. Surg. 2012, 68, 461–466. [Google Scholar] [CrossRef]
- Murphy, R.X.; Birmingham, K.L.; Okunski, W.J.; Wasser, T. The Influence of Airbag and Restraining Devices on the Patterns of Facial Trauma in Motor Vehicle Collisions. Plast. Reconstr. Surg. 2000, 105, 516–520. [Google Scholar] [CrossRef]
- Markowitz, B.L.; Manson, P.N.; Sargent, L.; Kolk, C.A.V.; Yaremchuk, M.; Glassman, D.; Crawley, W.A. Management of the Medial Canthal Tendon in Nasoethmoid Orbital Fractures: The Importance of the Central Fragment in Classification and Treatment. Plast. Reconstr. Surg. 1991, 87, 843–853. [Google Scholar] [CrossRef]
- Shore, J.W.; Rubin, P.A.; Bilyk, J.R. Repair of Telecanthus by Anterior Fixation of Cantilevered Miniplates. Ophthalmology 1992, 99, 1133–1138. [Google Scholar] [CrossRef]
- Nissen, N.J.B.; Okhah, Z.I.; Basta, M.N.; Hsieh, S.; Crozier, J.W.M.; Jehle, C.C.; Rao, V.; Woo, A.S. Underdiagnosis of Nasoorbitoethmoid Fractures in Patients with Zygoma Injury. Plast. Reconstr. Surg. 2020, 145, 1001–1008. [Google Scholar] [CrossRef]
- Margulies, S.S.; Thibault, K.L. Infant Skull and Suture Properties: Measurements and Implications for Mechanisms of Pediatric Brain Injury. J. Biomech. Eng. 2000, 122, 364–371. [Google Scholar] [CrossRef] [PubMed]
- Coats, B.; Margulies, S.S. Material Properties of Human Infant Skull and Suture at High Rates. J. Neurotrauma 2006, 23, 1222–1232. [Google Scholar] [CrossRef] [PubMed]
- Boyd, D.C.; Cheek, K.G.; Boyd, C.C. Fatal non-accidental pediatric cranial fracture risk and three-layered cranial architecture development. J. Forensic Sci. 2023, 68, 46–58. [Google Scholar] [CrossRef]
- Glenney, A.E.; Irgebay, Z.; Cheng, L.G.; et al. Paediatric nasoorbitoethmoid fractures: a single institution’s 15-year experience. J Craniofac Surg. 2023, 34, 1717–1721. [Google Scholar] [CrossRef]
- Xue, A.S.; Maricevich, R.S.; Braun, T.L. Differences in the Management of Pediatric Facial Trauma. Semin. Plast. Surg. 2017, 31, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Markowitz, B.L.; Manson, P.N. Panfacial fractures: organization of treatment. Clin Plast Surg. 1989, 16, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Remmler, D.; Denny, A.; Gosain, A.; Subichin, S. Role of three-dimensional computed tomography in the assessment of nasoorbi-toethmoidal fractures. Ann Plast Surg. 2000, 44, 553–562. [Google Scholar] [CrossRef]
- Markowitz, B.L.; Manson, P.N.; Sargent, L.; Kolk, C.A.V.; Yaremchuk, M.; Glassman, D.; Crawley, W.A. Management of the Medial Canthal Tendon in Nasoethmoid Orbital Fractures: The Importance of the Central Fragment in Classification and Treatment. Plast. Reconstr. Surg. 1991, 87, 843–853. [Google Scholar] [CrossRef]
- Ellis, E. Sequencing treatment for naso-orbito-ethmoid fractures. J Oral Maxillofac Surg. 1993, 51, 543–558. [Google Scholar] [CrossRef]
- Paskert, J.P.; Manson, P.N. The Bimanual Examination for Assessing Instability in Naso-Orbitoethmoidal Injuries. Plast. Reconstr. Surg. 1989, 83, 165–167. [Google Scholar] [CrossRef]
- Pati, D.; Mishra, N.; Kar, I.; Meher, B.; Samal, D.; Rath, K.C. Nasoorbitoethmoid fractures in a tertiary care hospital of eastern India: a prospective study. Natl. J. Maxillofac. Surg. 2021, 12, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, E.P.; Hopper, R.A.; Suver, D.W.; Hayes, A.G.; Gruss, J.S.; Birgfeld, C.B. Zygomaticomaxillary complex fractures and their association with naso-orbito-ethmoid fractures: a 5-year review. Plast Reconstr Surg. 2012, 130, 1296–1304. [Google Scholar] [CrossRef] [PubMed]
© 2024 by the author. The Author(s) 2024.