Background
Tumor resection and trauma are common causes of mandibular defects requiring oral and maxillofacial surgery and often resulting in significant aesthetic and functional deficits. With the development and application of digital surgical techniques, preformed surgical plates, and vascularized autogenous bone grafts have been widely applied as primary treatments for mandibular defect reconstruction in clinical practice.[
1,
2,
3,
4] However, considerable time and effort are required to prepare the mandibular models and manually prebend the conventional surgical plates to match the mandible and bone graft anatomical contours pre-surgically. Furthermore, the surgical plates usually require some adjustments during surgery, increasing the operation time and possibly influencing the outcome accuracy. The repetitive bending of the surgical plates contributes to stress fatigue and could lead to eventual plate fracture.[
5]
In recent years, three-dimensional (3D) printing has been used to develop patient-specific surgical plates for mandibular defect reconstruction.[
6,
7] The 3D-printed surgical plates are advantageous for mandibular reconstruction because they possess high geometrical accuracy, simplify surgical procedures, and shorten the recovery time.[
8] Our previous study demonstrated that 3D-printed surgical plates exhibited better mechanical properties than conventional ones.[
9]
This study aimed to evaluate the clinical effects and accuracy of 3D-printed personalized surgical plates used for mandibular defect reconstruction in clinical applications by comparing them to conventional surgical plates.
Design and Printing of 3D Surgical Plates
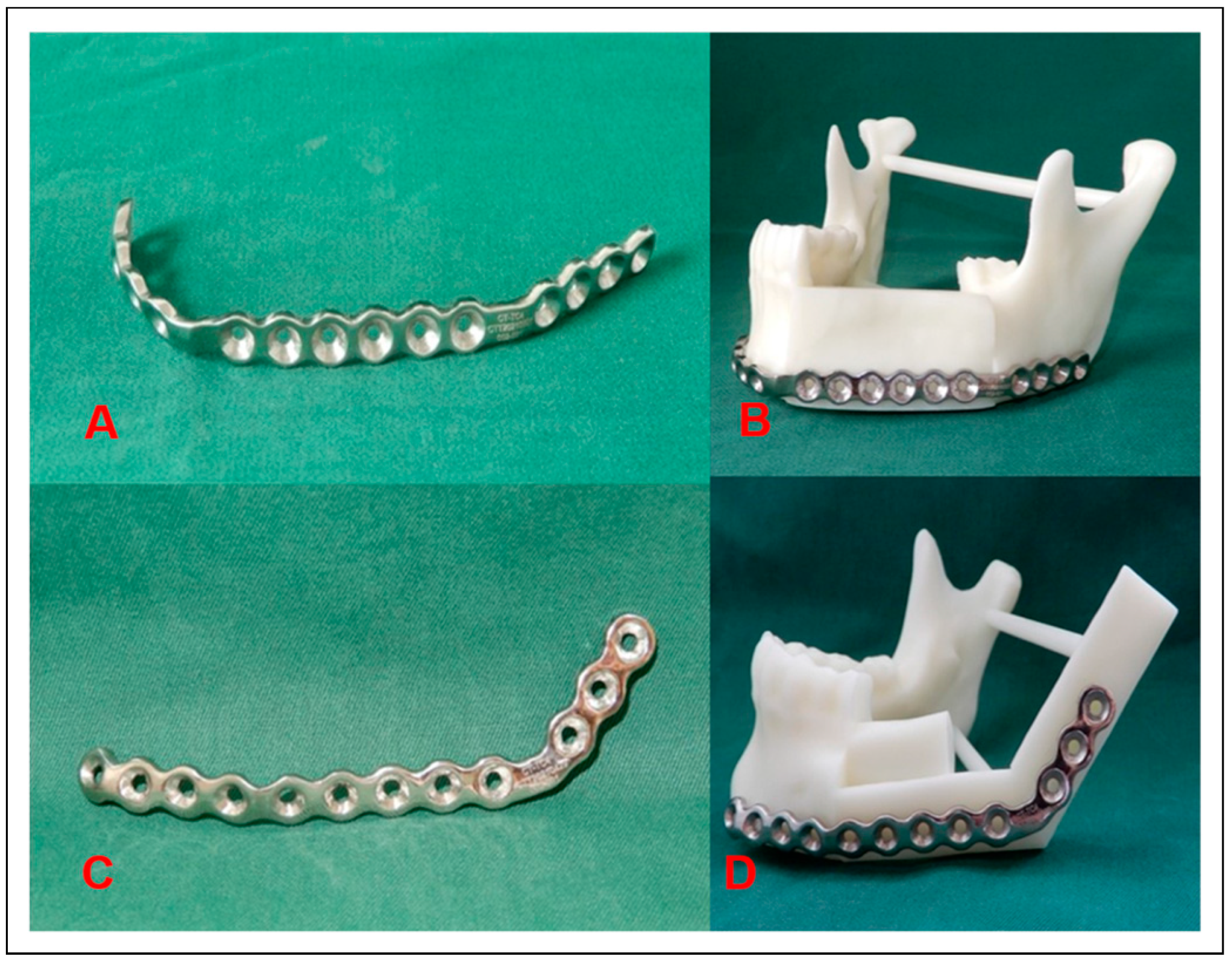
First, we designed a standardized prototype in Solid Works (Dassault Systèmes SE, Vélizy-Villacoublay, France) based on the contour parameters of a conventional surgical plate. The design data and the virtual surgical plan were imported into Magics 24.0 (Materialise). Then the standardized surgical plate was customized specifically based on the outer surface anatomy of the reconstructed mandible. Finally, the customized surgical plate data were sent to the engineers who printed the surgical plate using the selective laser melting technology in a Concept Laser M2 printer (Concept Laser, Lichtenfels, Germany) with titanium alloy (Ti-6Al-4V) as the raw material (
Figure 1).
Preparation of Conventional Surgical Plates
The stereolithographic models of the reconstructed mandibles were printed based on the virtual surgical plans. The 2.5-mm thick conventional surgical plates (MatrixMANDIBLE, DePuy Synthes, Raynham, MA, USA) were prebent manually following the models.
Design and Printing of Surgical Templates
Several templates were designed and used to realize the virtual surgical plan and improve the precision and efficiency of the surgery. The cutting templates guided the surgeons to conduct the mandibulectomy accurately, the harvest templates helped obtain the donor bone graft precisely, and the modeling templates were used to shape the bone graft into an ideal contour to match the mandibular defect.[
11] The templates were designed in Geomagic (Geomagic, Cary, NC, USA) and printed using the fused deposition modeling technology.
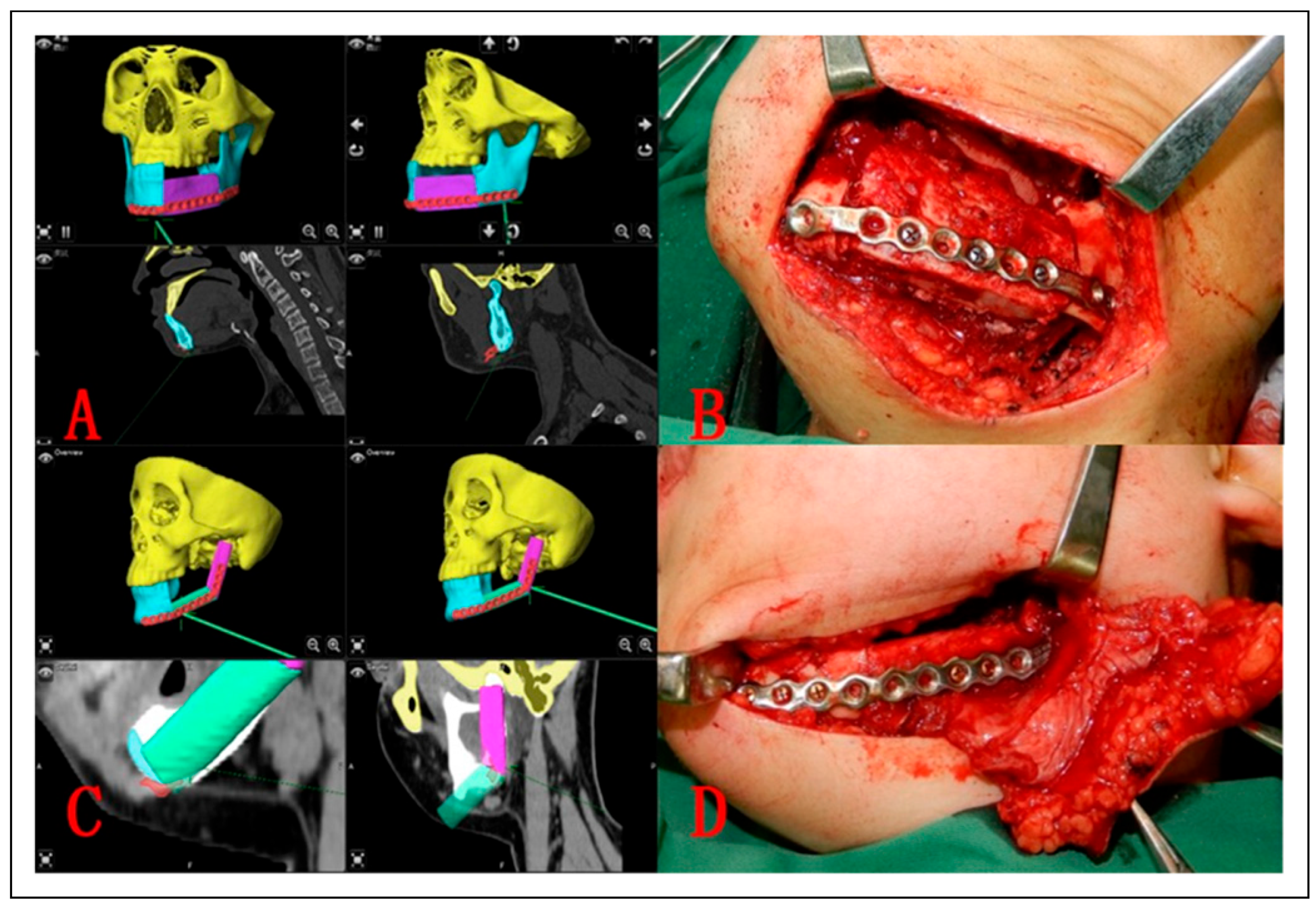
Navigation-Guided Surgical Procedures
The virtual surgical plan and the surgical plate data were imported into iPlan CMF 3.0 (Brainlab, Feldkirchen, Germany) and a navigation protocol was generated for presentation during surgery. The surgical procedures in both groups were performed fully guided by the navigation system. The tumor resection and mandibulectomy were guided by the cutting template. The deep circumflex iliac artery or free fibula flap was prepared with the assistance of the harvest and modeling templates, transferred to the recipient site, and fixed to the remaining mandible using titanium screws. The three-dimensional positions of the bone graft and surgical plate were confirmed to match the positions in the virtual surgical plan using the navigation system (
Figure 2).
A 3D-printed surgical plate and a conventional surgical plate prebent manually before surgery were used to fix the remaining mandible and bone graft in the experimental group and control group, respectively.
Outcome Evaluation
Evaluation of Clinical Application Effects. The primary endpoint was the flap survival rate in mandibular reconstruction applying the 3D-printed and conventional surgical plates. This endpoint was evaluated by the chief surgeon immediately after surgery mainly based on the survival condition of flap whether the flap was transplanted successfully, followed by whether the surgical plate fit perfectly to the bone surface with no apparent gaps or spaces between them,[
7] and whether surgical plate adjustments were made during surgery. The flap survival rate was evaluated again by the chief surgeon 2 weeks after surgery. The surgical plates and bone surface contacting conditions were also evaluated with the aid of the 1-week postoperative maxillofacial CT scan.
The secondary endpoints were the incidence of postoperative complications and patient self-evaluation of facial appearance. The surgical plate-related postoperative complications, including breakage, loosening, and exposure, were evaluated and recorded 2 weeks and six months after surgery. Other postoperative complications related to the operation areas and donor sites were also recorded. The patients evaluated and scored their facial appearance using the Visual Analogue Scale six months after surgery. The scores were categorized into fully satisfied (8-10), basically satisfied (6-7), unsatisfied (4-5), and poor (0-3).
Evaluation of Clinical Application Accuracy. The primary accuracy endpoints were position deviations of the whole mandible, transplanted bone graft, lower mandibular border on the reconstructed side, mandibular condyle and mandibular angle.
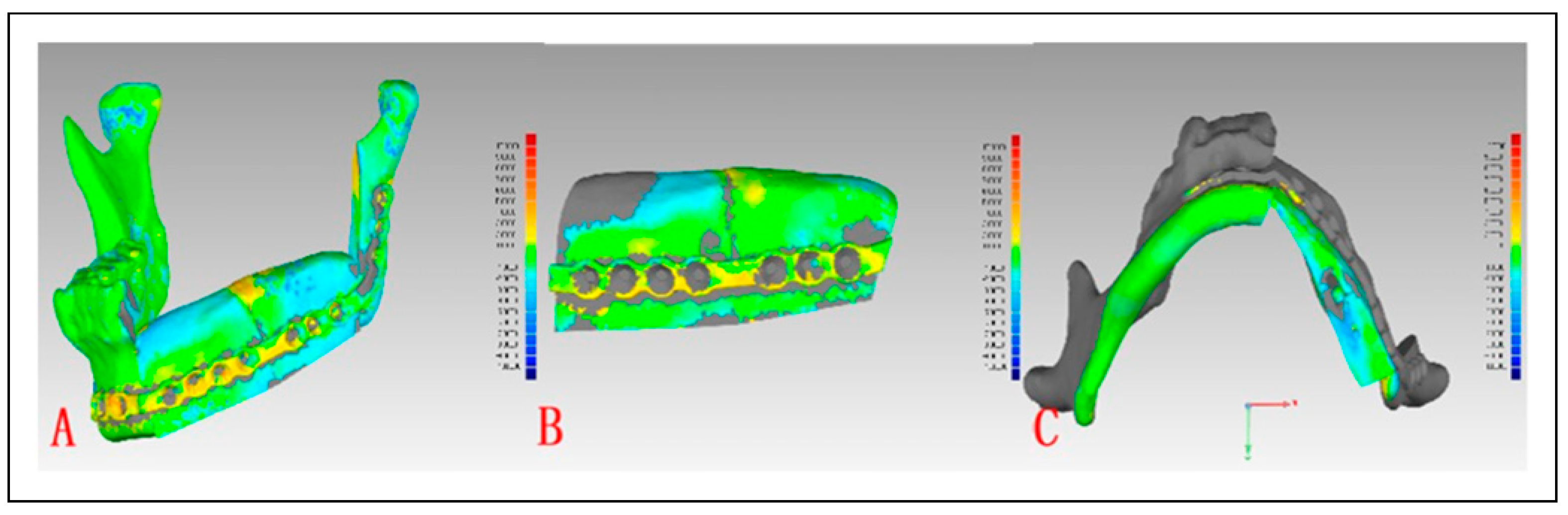
A 1-month postoperative maxillofacial CT scan was performed. The CT data and preoperative virtual surgical plan were imported into Geomagic Control X 2022 (Geomagic) for comparison. The position deviations of the whole mandible, transplanted bone graft, lower mandibular border on the reconstructed side were analyzed and calculated automatically using chromatographic analysis by the software (
Figure 3).
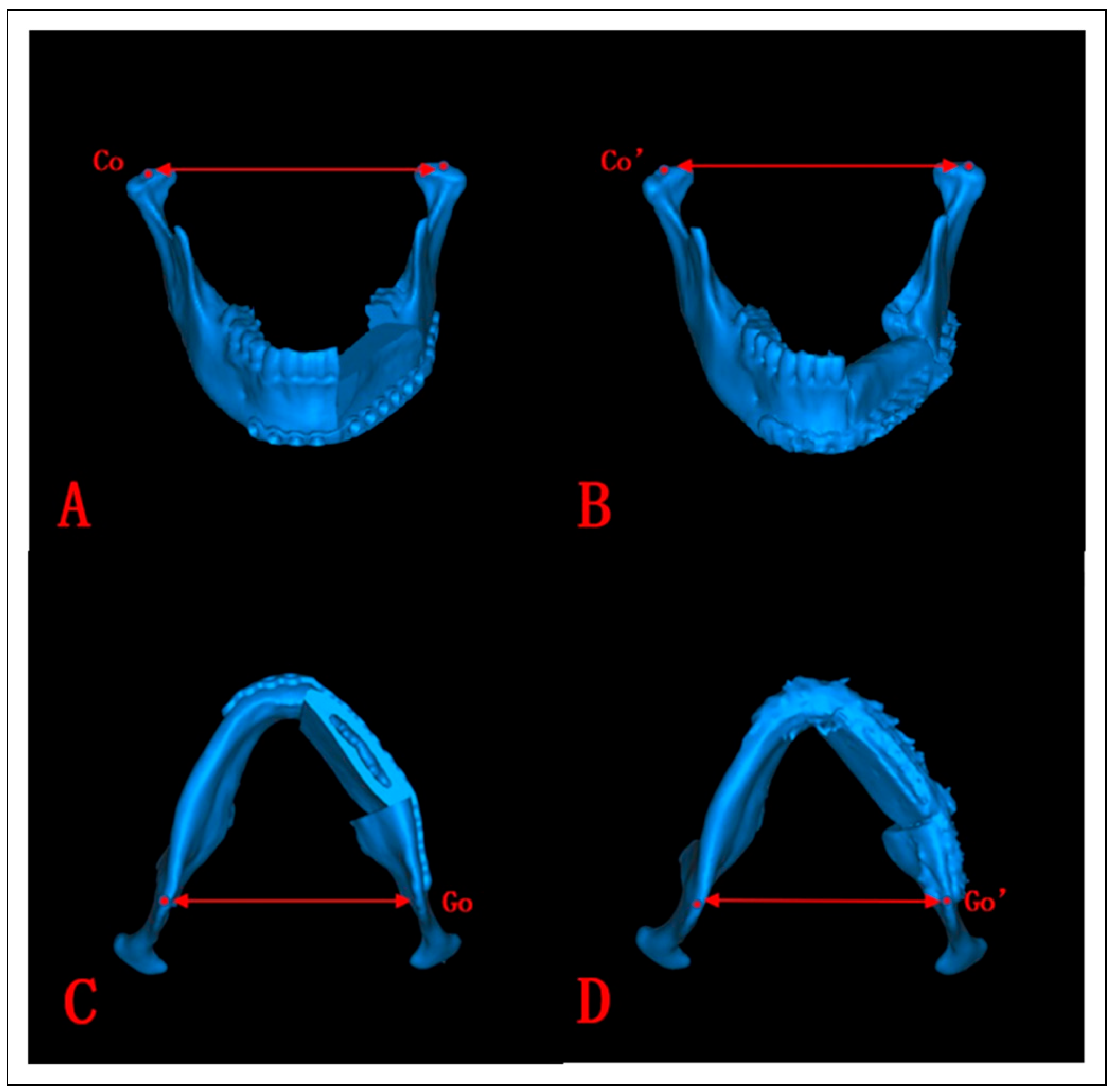
The CT data and virtual surgical plan were imported into ProPlan CMF 3.0 to assess the position deviation of the mandibular condyle and mandibular angle. The bilateral preoperative and postoperative condylions or gonions were marked by the 3D Cephalometry module. The position deviation of the mandibular condyle or mandibular angle was evaluated by comparing the preoperative and postoperative distances between the condylions (
Figure 4A,B) or the gonions (
Figure 4C,D).
Statistical Analysis
SPSS 22.0 (IBM Corp., Armonk, NY, USA) was used for the statistical analysis. Discontinuous variables are summarized as medians and interquartile ranges (IQRs) and were compared by the Mann-Whitney U test. Continuous variables are expressed as means ± standard deviations and were compared by the independent-samples t test. Categorical variables were compared by the Chi-squared test. P < 0.05 was considered statistically significant.
Results
Patient Demographics and Characteristics
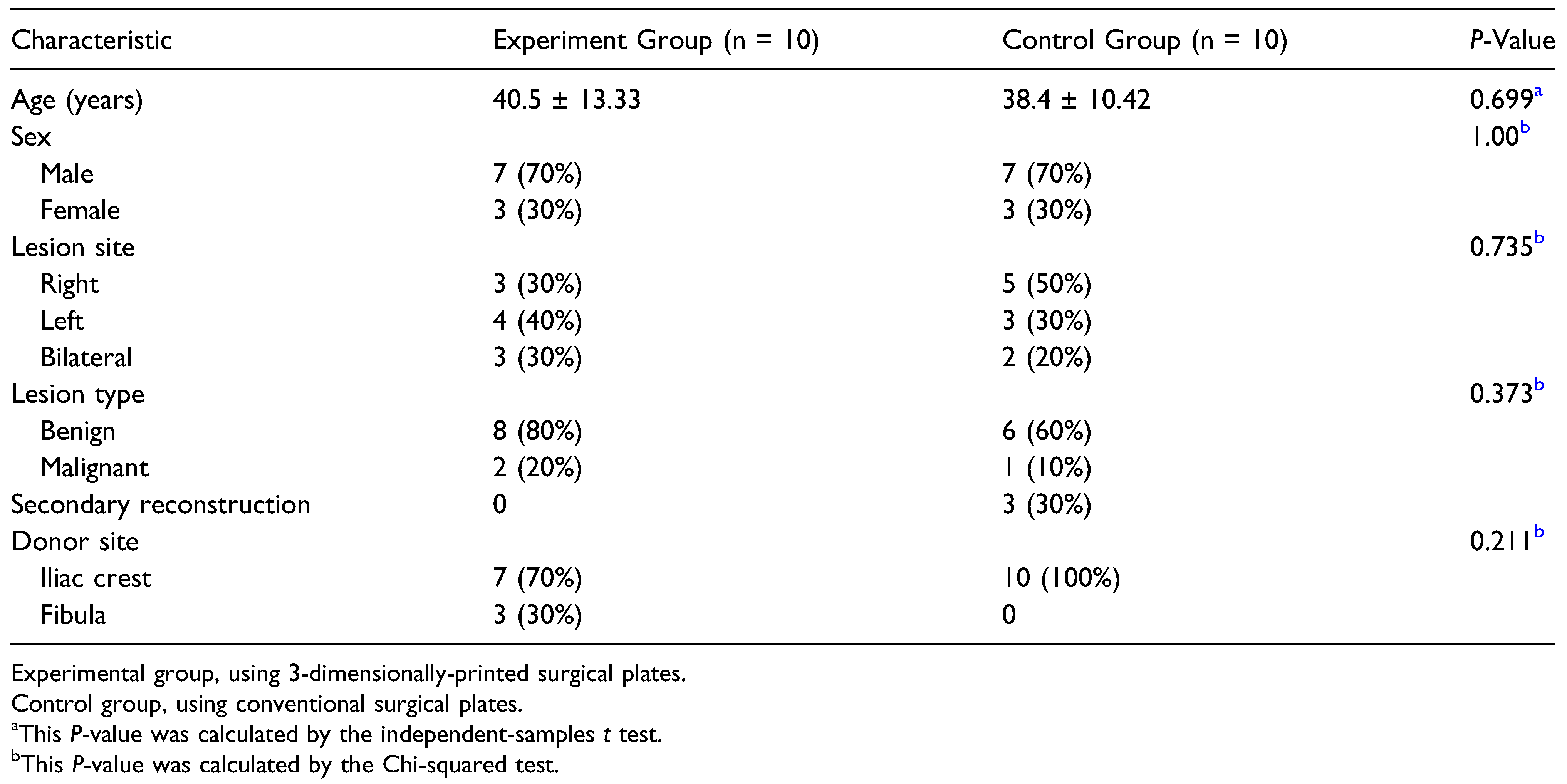
Twenty patients (14 males and six females) were included in this study, with a mean age of 39.45 ± 11.69 (range, 23-58) years and a mean follow-up of 16 ± 22.05 (range, 6-99) months (
Table 1).
The experimental group comprised ten patients who underwent simultaneous mandibular reconstruction after tumor resection, including eight with benign tumors (ameloblastoma in four, ossifying fibroma in three, and odontogenic keratocyst in one) and 2 with malignant tumors (squamous cell carcinoma in one and mucoepidermoid carcinoma in one). The control group consisted of ten patients, seven who underwent simultaneous mandibular reconstruction after tumor resection, including six with benign tumors (ameloblastoma in four and ossifying fibroma in 2) and one with a malignant tumor (chondrosarcoma), and three who underwent secondary mandibular reconstruction. The groups were similar in age, sex, lesion site, lesion type, and donor site (all P > 0.05).
Evaluation of Clinical Application Effects
The overall free flap survival rate was 100%. All free flaps were transplanted and together with applying surgical plates in the mandibular defects reconstruction with success. All surgical procedures were guided by the navigation system and successfully completed according to the preoperative virtual surgical plan. The surgical plates fixed the remaining mandibles and bone grafts stably and effectively in all patients. The 1-week postoperative maxillofacial CT and the 3D model generated clearly showed that the 3D-printed surgical plate perfectly fit the bone surface with no apparent gaps or spaces between them (
Figure 5), and no further adjustments were required during surgery. The conventional surgical plates of five patients with extensive mandibular defects involving the chin or the opposite mandible were adjusted intraoperatively.
We observed no surgical plate-related complications at the 6-month follow-up. One patient in the experimental group presented with lower extremity deep vein thrombosis one month after surgery, which was cured following thrombolytic therapy. One patient in the control group developed a wound infection in the submandibular region, which was cured with wound irrigation, drainage, and antibiotic therapy. Another patient in this group developed skin hypoesthesia in the donor site, which was gradually cured with drug and physical therapy.
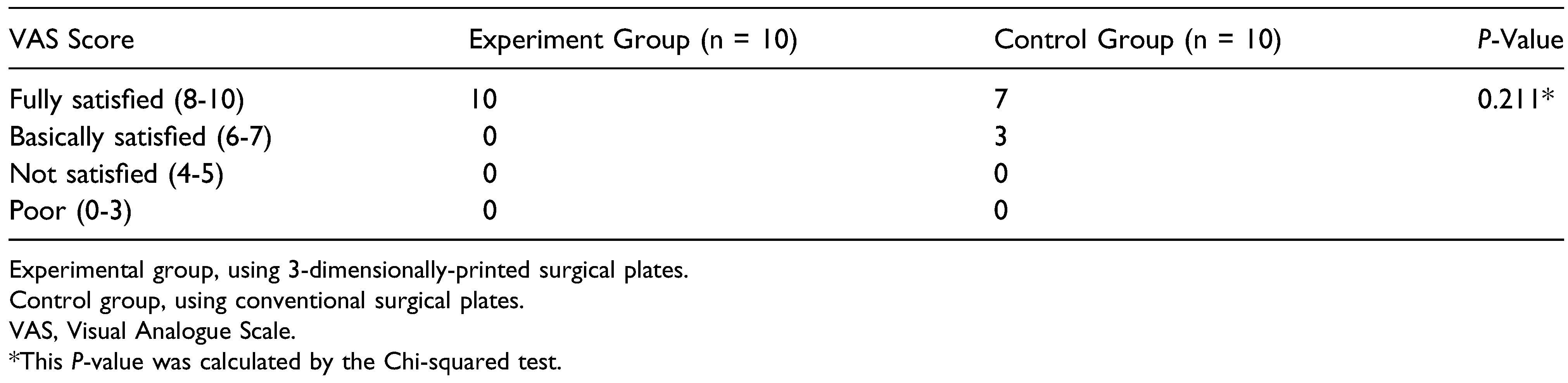
All patients in the experimental group were fully satisfied with the postoperative facial appearance, similar to patients in the control group who were satisfied (fully or basically satisfied;
P = 0.211;
Table 2).
Evaluation of Clinical Application Accuracy
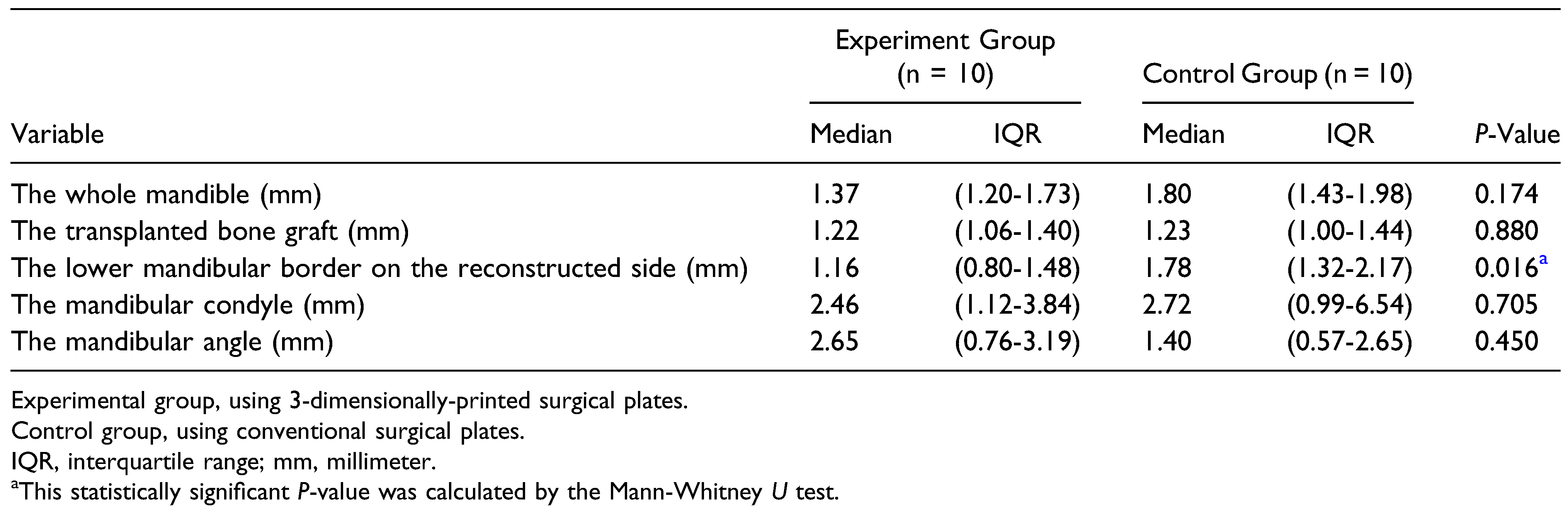
The position deviation outcomes were summarized in
Table 3.
The experimental and control groups showed similar position deviation of the whole mandible [median, 1.37 (IQR, 1.20-1.73) mm vs median, 1.80 (IQR, 1.43-1.98) mm; P = 0.174] and transplanted bone graft [median, 1.22 (IQR, 1.06-1.40) mm vs median, 1.23 (IQR, 1.00-1.44) mm; P = 0.880], indicating that 2 surgical plate types could well maintain the overall position of the mandible and transplanted bone graft.
The position deviation of the lower mandibular border on the reconstructed side in the experimental group was smaller than in the control group [median, 1.16 (IQR, 0.80-1.48) mm vs median, 1.78 (IQR, 1.32-2.17) mm; P = 0.016), showing that patients presented with a higher position accuracy and a better contour of the lower mandibular border on the reconstructed side when the 3D-printed surgical plates were used.
The experimental and control groups showed similar position deviation of the mandibular condyle [median, 2.46 (IQR, 1.12-3.84) mm vs median, 2.72 (IQR, 0.99-6.54) mm; P = 0.705], and the mandibular angle [median, 2.65 (IQR, 0.76-3.19) mm vs median, 1.40 (IQR, 0.57-2.65) mm; P = 0.450].
Discussion
Mandibular defect reconstruction is a common and challenging oral and maxillofacial surgery, with the development of 3D printing technology, especially its application in oral and maxillofacial surgery,[
12,
13] 3D-printed surgical plates and the current digital and surgical techniques have contributed to improving and advancing personalized mandibular reconstructions.[
5,
6,
7,
14]
Jules et al[
15] completed the first total mandibular defect reconstruction with a titanium jaw implant manufactured by 3D printing in 2011. Smith et al[
14] studied 16 cases of mandibular reconstruction with 3D-printed surgical plates. Yang et al[
7] conducted a prospective clinical trial to assess the feasibility, safety and accuracy of applying 3D-printed surgical plates in mandibular reconstruction. However, these previous studies had some shortcomings, such as limiting their outcome evaluation to a few aspects or conducting the research on a small sample. Furthermore, a common and critical problem was that they did not compare to the conventional surgical plates. The present study designed, 3D-printed, and applied personalized surgical plates for mandibular reconstruction. Various evaluation indexes were used, and the conventional surgical plates were set as a control to further explore, evaluate, and compare the effects and accuracy of clinically applying 3D-printed surgical plates. To our knowledge, this was the first clinical study to systematically compare 3D-printed and conventional surgical plates in China.
All mandibular reconstruction procedures in both groups were completed successfully. No complications related to the surgical plates that might adversely affect the recovery and outcomes were noted during the follow-up period. All patients were satisfied with the clinical effects and facial appearance after surgery. Therefore, the results above demonstrated that the clinical application of 3D-printed surgical plates was effective.
The high accuracy provided by the 3D-printed surgical plates is particularly important for mandibular reconstruction. We used a series of indexes to comprehensively analyze and evaluate this aspect. Our results showed that the position deviations of the whole mandible, transplanted bone graft, mandibular condyle, and mandibular angle were similar in both groups, proving that both surgical plate types could well maintain the overall position of the reconstructed mandible and normal occlusal relationship after surgery. Specifically, the position deviations of the whole mandible, transplanted bone graft, and mandibular condyle in the experimental group were lower than in the control group, indicating a more stable position after surgery. We used virtual surgical plans and performed digital surgical techniques before surgery, and the surgical procedures were operated accurately, in line with the virtual surgical plans, assisted by corresponding templates, and guided by an intraoperative navigation system in both groups. The above measures ensured the accuracy of the final surgical outcomes. The accuracy of the relevant digital techniques has been verified in previous studies.[
2,
3] Yang et al[
16] reported that the position deviations of the whole mandible, transplanted bone graft, and mandibular condyle were 1.5 ± 0.5, 3.1 ± 1.4, and 2.6 ± 3.0 mm, respectively, for 3D-printed patient-specific surgical plates, and 2.1 ± 0.7, 8.7 ± 4.2, and 5.2 ± 4.2 mm, respectively, for conventional surgical plates, comparable or slightly higher than the values in our study. Moreover, Yang et al[
7] reported in another study that the mandibular angle position deviation was 2.4 ± 3.4 mm, similar to the result in our experimental group.
The primary difference between the 2 surgical plate types is in lower mandibular border restoration. The position deviation of the lower mandibular border on the reconstructed side was significantly smaller in patients treated with 3D-printed surgical plates than in those in whom conventional surgical plates were used (P = 0.016). Unlike the conventional ones, the 3D-printed surgical plates were designed completely based on the virtual surgical plans and manufactured into physical objects directly, avoiding the regular preoperative preparations and intraoperative adjustments. Furthermore, with the help of the various templates, the surgical plates could fully fit the remaining mandible and bone graft. This was particularly evident in cases with complex or extensive mandibular defects in which the 3D-printed surgical plates were advantageous at the mandible-bone graft or bone graft-angle connection sites due to their personalized characteristics. In such cases, the 3D-printed surgical plates achieved close fitting and effective fixation, with no gaps between the plates and bone tissue that might lead to unstable fixation or displacement after surgery. The 3D-printed surgical plates could also serve as a positioning template for the bone grafts during surgery and properly verify the final positioning effects. Therefore, the 3D-printed surgical plates could restore the lower mandibular border continuity and mandible symmetry more precisely than the conventional ones, achieving higher position accuracy and better lower mandibular border contour on the reconstructed side.
Another advantage of applying the 3D-printed surgical plates is that they help simplify the preoperative preparations and intraoperative procedures. The virtual surgical plans, surgical plate prototypes, and surgical templates in this study were all designed and completed by the same surgeon with abundant clinical experience. Therefore, the standards of the design and application were highly consistent. Optimization and 3D printing were conducted by the engineers. Unlike the traditional practice in which the plans are proposed by the surgeons and processed by the engineers, our workflow could obtain a more appropriate plan and greatly improve efficiency. Moreover, learning and grasping the surgical plate and template designs were relatively easy. Consequently, it was possible to avoid printing the stereolithographic models or processing the surgical plates provided all other preoperative preparations were the same. In some complicated cases, the stereolithographic models could be used to examine and verify the fitting and accuracy of the 3D-printed surgical plates during a presurgical model surgery in vitro. Besides, the practical surgical procedures in the experimental group showed that direct and accurate positioning and fixation of the 3D printed surgical plates were achieved during surgery without any adjustments or modifications.
This study was limited by the lack of long-term clinical follow-up and long-dated evaluation of the outcomes and accuracy of clinically using the 3D-printed surgical plates in the experimental group. Although 3D-printed patient-specific surgical plates have been used for some years in several countries, the technology is relatively new and has not been widely applied in China, especially in oral and maxillofacial surgery. This is because the policies related to applying 3D-printing technology in medicine are still improving. Another limitation of the study that the number of patients involved was relatively small. While, the results showed that 3D-printed surgical plates exhibited satisfactory performance in clinical application. Therefore, a multicenter, prospective clinical study is ongoing, and more patients are being recruited continuously. Such a study could provide reliable evidence for the clinical effects and accuracy of using 3D-printed patient-specific surgical plates for mandibular reconstruction.