Facial Lacerations Related to Recreational Activities: A National 10-Year Evaluation From US Emergency Departments
Abstract
:Introduction
Methods
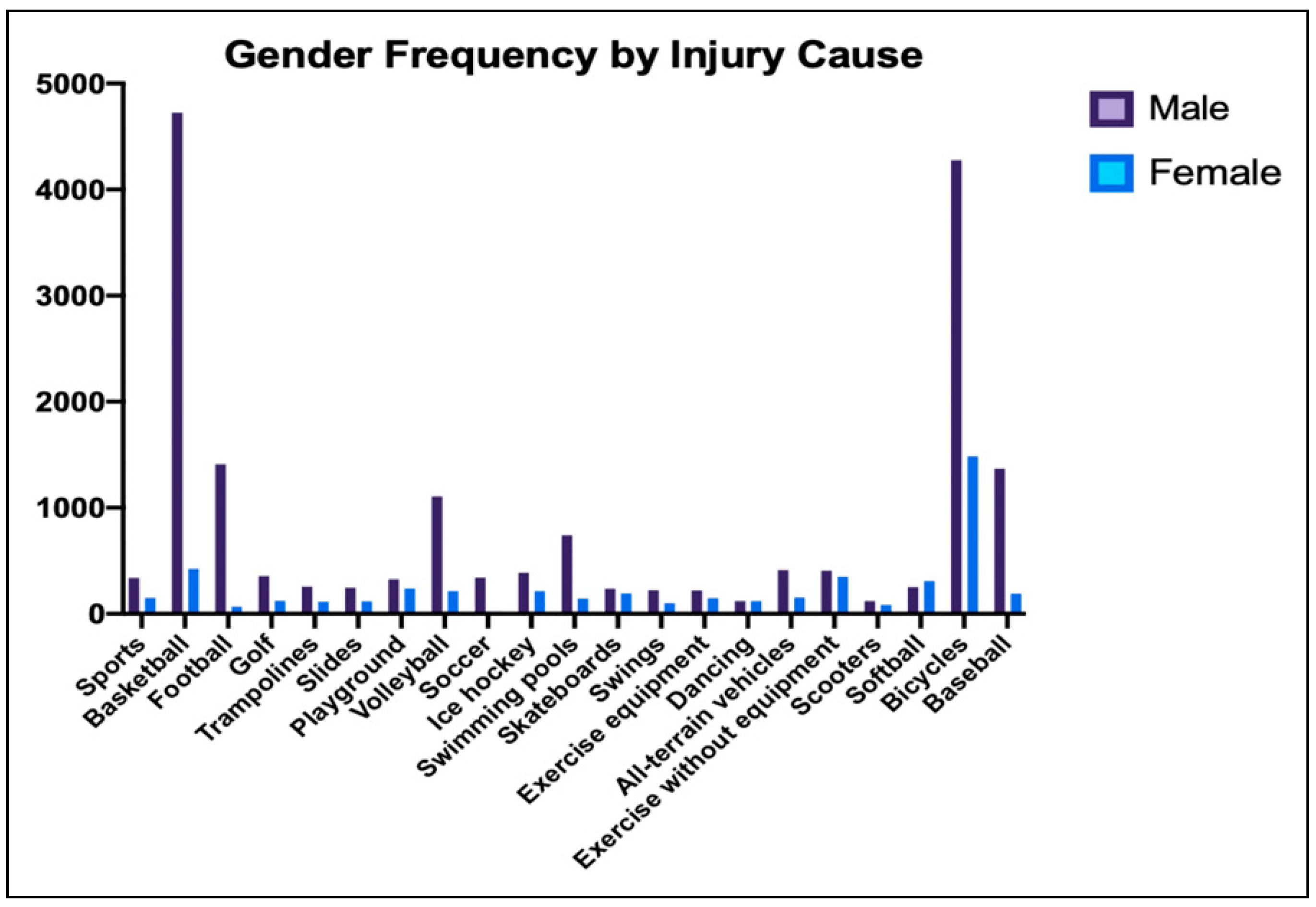
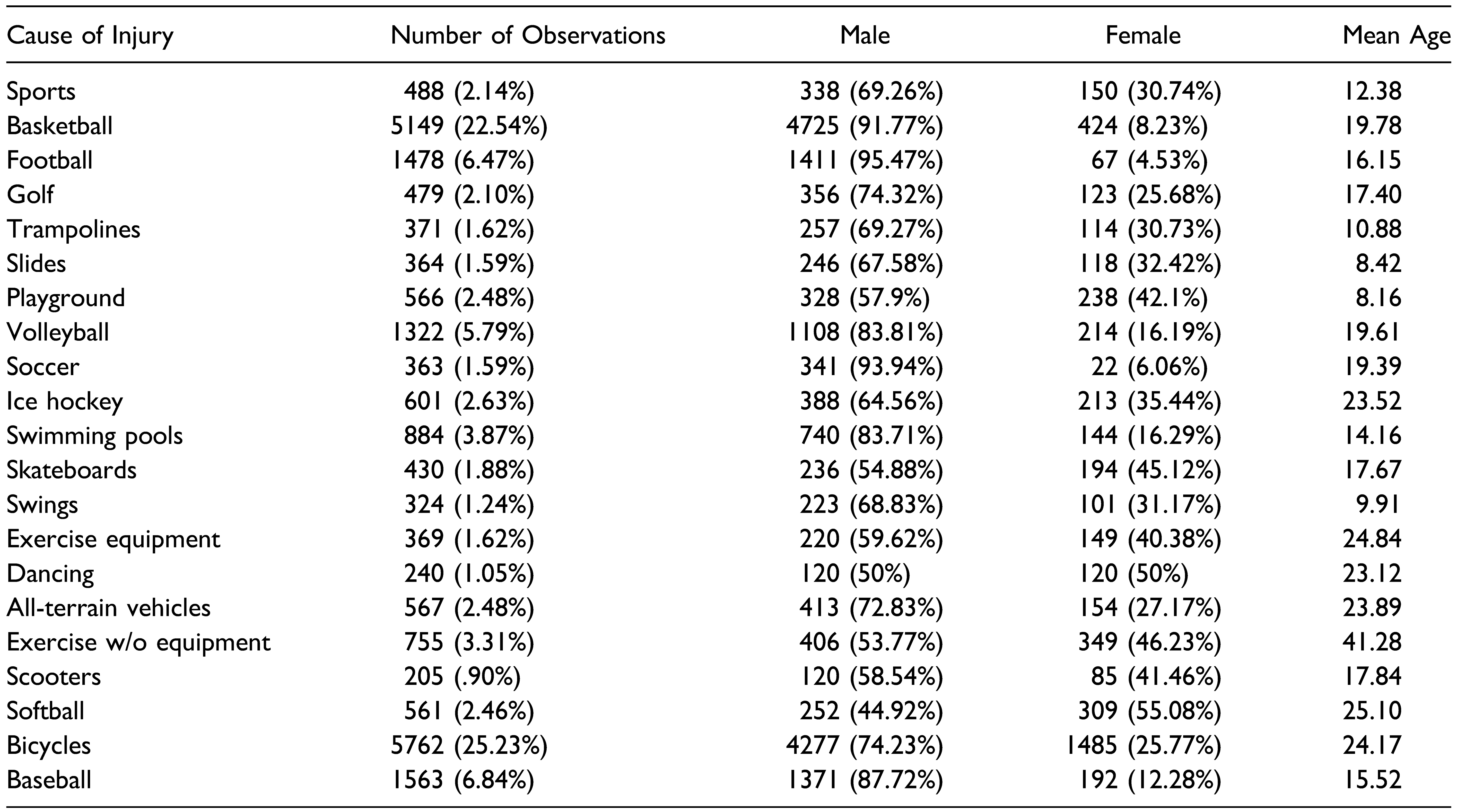
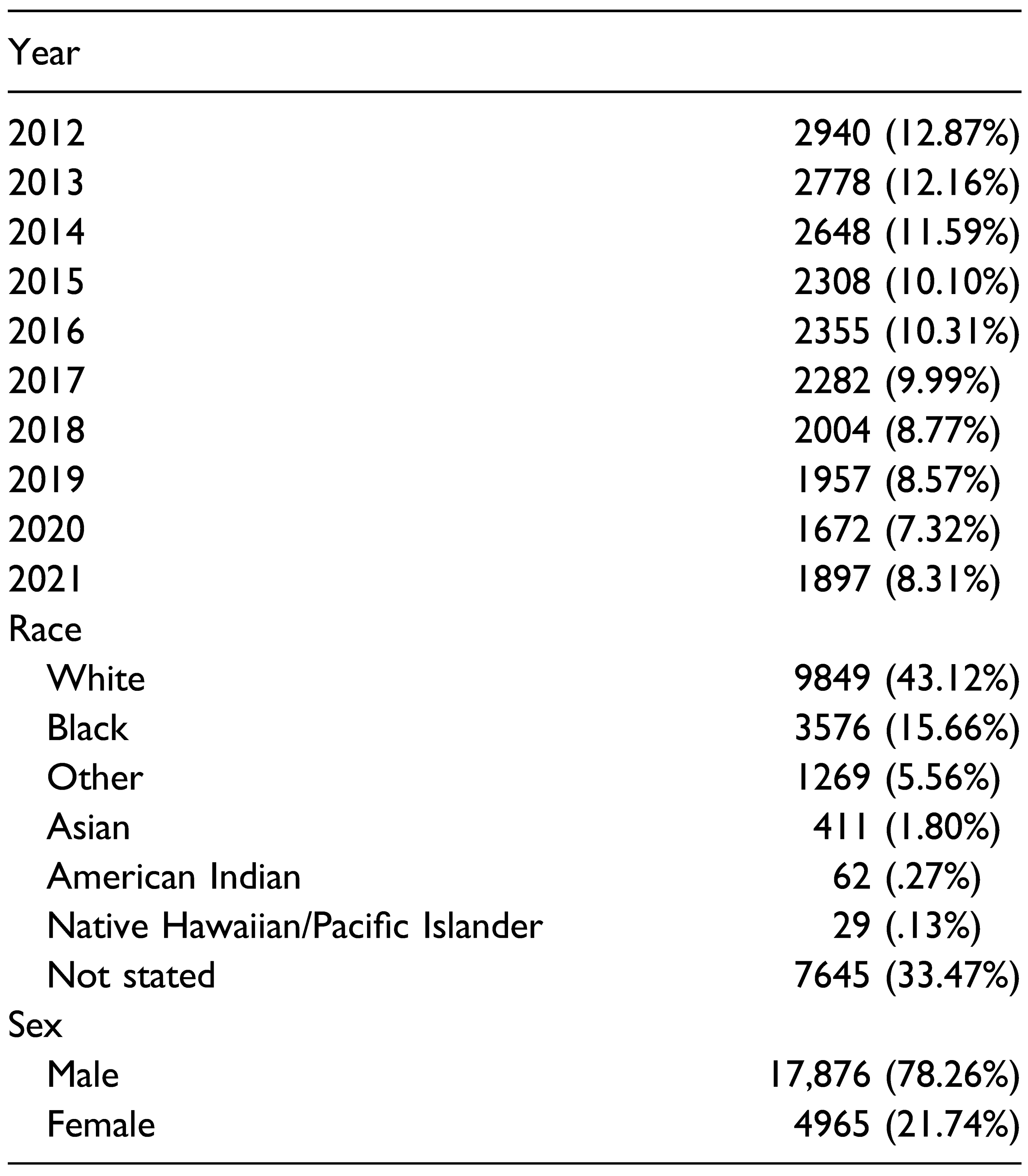
Results
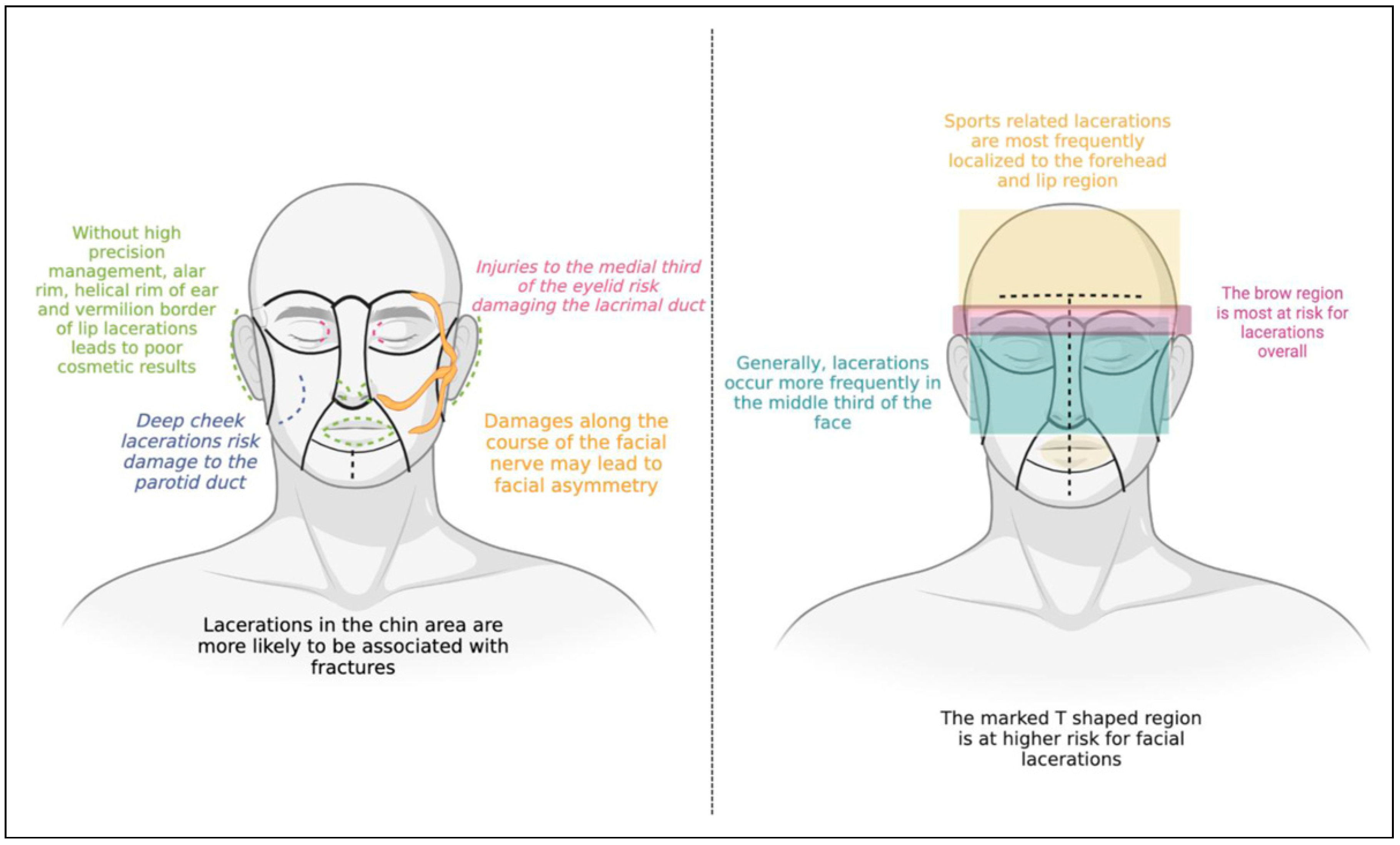
Discussion
Limitations
Conclusions
Funding
Declaration of Conflicting Interests
References
- Bolt, R.W.; Watts, P.G. The relationship between aetiology and distribution of facial lacerations. Inj Extra. 2004, 35(1), 6–11. [Google Scholar] [CrossRef]
- Romeo, S.J.; Hawley, C.J.; Romeo, M.W.; Romeo, J.P.; Honsik, K.A. Sideline management of facial injuries. Curr Sports Med Rep. 2007, 6(3), 155–161. [Google Scholar] [CrossRef] [PubMed]
- Tebble, N.J.; Thomas, D.W.; Price, P. Anxiety and selfconsciousness in patients with minor facial lacerations. J Adv Nurs. 2004, 47(4), 417–426. [Google Scholar] [CrossRef] [PubMed]
- Hoogewerf, C.J.; van Baar, M.E.; Middelkoop, E.; van Loey, N.E. Impact of facial burns: Relationship between depressive symptoms, self-esteem and scar severity. Gen Hosp Psychiatr. 2014, 36(3), 271–276. [Google Scholar] [CrossRef] [PubMed]
- Bisson, J.I.; Shepherd, J.P.; Dhutia, M.; Dhutia, M. Psychological sequelae of facial trauma. J Trauma. 1997, 43(3), 496–500. [Google Scholar] [CrossRef] [PubMed]
- Roccia, F.; Bianchi, F.A.; Zavattero, E.; Baietto, F.; Boffano, P. Etiology and patterns of facial lacerations and their possible association with underlying maxillofacial fractures. J Craniofac Surg. 2011, 22(6), e19–e23. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, T.B.O.; Cancian, L.R.L.; Marques, C.G.; Piatto, V.B.; Maniglia, J.V.; Molina, F.D. Six years of facial trauma care: An epidemiological analysis of 355 cases. Braz J Otorhinolaryngol. 2010, 76(5), 565–574. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R. Factors influencing the incidence of maxillofacial fractures. Oral Maxillofac Surg. 2012, 16(1), 3–17. [Google Scholar] [CrossRef] [PubMed]
- Shinkle, D. State safe bicycle passing laws. NCSL Legisbr. 2018, 26(32), 1–2. [Google Scholar]
- Strotmeyer, S.J.; Behr, C.; Fabio, A.; Gaines, B.A. Bike helmets prevent pediatric head injury in serious bicycle crashes with motor vehicles. Inj Epidemiol. 2020, 7(1), 24. [Google Scholar] [CrossRef] [PubMed]
- Sheu, Y.C.; Chen, L.H.; Hedegaard, H. Sportsand Recreationrelated Injury Episodes in the United States, 2011–2014. Vol. 99. Natl Health Stat Report; 2016.
- Lyons, T.W.; Miller, K.A.; Miller, A.F.; Mannix, R. Racial and ethnic differences in emergency department utilization and diagnosis for sports-related head injuries. Original research. Original research. Front Neurol. 2019. [CrossRef]
- Zhang, X.; Carabello, M.; Hill, T.; Bell, S.A.; Stephenson, R.; Mahajan, P. Trends of racial/ethnic differences in emergency department care outcomes among adults in the United States from 2005 to 2016 original research. Front Med. 2020. [CrossRef] [PubMed]
- Cone, D.C.; Richardson, L.D.; Todd, K.H.; Betancourt, J.R.; Lowe, R.A. Health care disparities in emergency medicine. Acad Emerg Med 2003, 10(11), 1176–1183. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Ramgopal, S.; Marin, J.R. Racial and ethnic differences in low-value pediatric emergency care. Acad Emerg 2022, 29, 698–709. [Google Scholar] [CrossRef] [PubMed]
- Khidir, H.; Salhi, R.; Sabbatini, A.K.; et al. A quality framework to address racial and ethnic disparities in emergency department care. Ann Emerg Med. 2023, 81(1), 47–56. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine Committee on U, Eliminating R. Ethnic disparities in health C. In Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care; Smedley, B.D., Stith, A.Y., Nelson, A.R., Eds.; National Academies Press: Washington, DC, USA.
- Dalsania, A.K.; Fastiggi, M.J.; Kahlam, A.; et al. The relationship between social determinants of health and racial disparities in COVID-19 mortality. J Racial Ethn Health Disparities. 2022, 9(1), 288–295. [Google Scholar] [CrossRef] [PubMed]
- Dickson, T.J.; Terwiel, F.A. Head injury and helmet usage trends for alpine skiers and snowboarders in western Canada during the decade 2008–9 to 2017–18. J Sci Med Sport. 2021, 24(10), 1004–1009. [Google Scholar] [CrossRef] [PubMed]
- Koch, D.A.; Hagebusch, P.; Lefering, R.; Faul, P.; Hoffmann, R.; Schweigkofler, U.; TraumaRegister, D.G.U. Changes in injury patterns, injury severity and hospital mortality in motorized vehicle accidents: A retrospective, crosssectional, multicenter study with 19,225 cases derived from the TraumaRegister DGU(®). Eur J Trauma Emerg Surg. 2023, 49, 1917–1925. [Google Scholar] [CrossRef] [PubMed]
- Ganga, A.; Kim, E.J.; Tang, O.Y.; et al. The burden of unhelmeted motorcycle injury: a nationwide scoring-based analysis of helmet safety legislation. Injury. 2023, 54(3), 848–856. [Google Scholar] [CrossRef] [PubMed]
- Akbari, M.; Lankarani, K.B.; Tabrizi, R.; et al. The effect of motorcycle safety campaign on helmet use: A systematic review and meta-analysis. IATSS Res. 2021, 45(4), 513–520. [Google Scholar] [CrossRef]
 |
 |
© 2023 by the author. The Author(s) 2023.
Share and Cite
Hauc, S.C.; Huelsboemer, L.; Lewis, K.; Hosseini, H.; Williams, M.; Rivera, J.C.; Alperovich, M. Facial Lacerations Related to Recreational Activities: A National 10-Year Evaluation From US Emergency Departments. Craniomaxillofac. Trauma Reconstr. 2024, 17, 238-243. https://doi.org/10.1177/19433875231211757
Hauc SC, Huelsboemer L, Lewis K, Hosseini H, Williams M, Rivera JC, Alperovich M. Facial Lacerations Related to Recreational Activities: A National 10-Year Evaluation From US Emergency Departments. Craniomaxillofacial Trauma & Reconstruction. 2024; 17(3):238-243. https://doi.org/10.1177/19433875231211757
Chicago/Turabian StyleHauc, Sacha C., Lioba Huelsboemer, Katelyn Lewis, Helia Hosseini, Mica Williams, Jean Carlo Rivera, and Michael Alperovich. 2024. "Facial Lacerations Related to Recreational Activities: A National 10-Year Evaluation From US Emergency Departments" Craniomaxillofacial Trauma & Reconstruction 17, no. 3: 238-243. https://doi.org/10.1177/19433875231211757
APA StyleHauc, S. C., Huelsboemer, L., Lewis, K., Hosseini, H., Williams, M., Rivera, J. C., & Alperovich, M. (2024). Facial Lacerations Related to Recreational Activities: A National 10-Year Evaluation From US Emergency Departments. Craniomaxillofacial Trauma & Reconstruction, 17(3), 238-243. https://doi.org/10.1177/19433875231211757



