Introduction
Frontal sinus fractures account for 5–15% of maxillofacial fractures [
1,
2,
3]. Often the result of high-energy trauma, frontal sinus fractures constitute damage to the anterior table, posterior table, frontal sinus outflow tract (FSOT), or a combination of these 3 structures. The anterior table of the frontal sinus forms part of the forehead, brow, and glabella, while the posterior table forms part of the anterior cranial fossa. The floor of the frontal sinus forms the medial orbital roof and contains the ostia, which drains into the nasofrontal recess [
1]. In the past, the majority of frontal sinus fractures were attributed to motor vehicle accidents [
4,
5,
6], though the advent of airbag technology has reduced this incidence and falls now account for 36–40% of all frontal sinus fractures [
7,
8]. Males in their 20s to 40s are the most common demographic presenting with this fracture type [
9]. It is relatively uncommon in children as the frontal sinus does not fully develop until adolescence [
4,
5,
7,
8,
10].
Approximately one-third of frontal sinus fractures are accompanied by injury to the FSOT. Drainage of the frontal sinus begins in the ostia and continues caudally through the FSOT and to the frontoethmoidal recess. The gold standard for evaluating frontal sinus injuries is computed tomography (CT) in axial and coronal views. Fractures in the medial portion of the frontal sinus, anterior ethmoidal complex, and floor of the frontal sinus suggest FSOT injury [
11]. Involvement of FSOT in the fracture increases the chance of obstruction of sinus drainage and associated complications.
The primary goal in managing frontal sinus fractures is to establish a “safe” sinus, meaning the reconstructed sinus carries no increased risk of obstruction or infection than that of the sinus pre-trauma [
3]. Maintaining a barrier between the sinus and intracranial contents, restoring frontal sinus outflow, and preserving the cosmetic appearance of the forehead are all components of successful treatment [
12,
13]. The AO outlines 4 options for frontal sinus fracture repair: observation, open reduction internal fixation (ORIF), obliteration, and cranialization. More recently, the use of endoscopes has introduced options for minimally invasive approaches to reduction. Treatment decisions can bemade by assessing the presence of anterior table fractures, posterior table fractures, naso-orbital-ethmoid (NOE) complex fractures, dural tears or cerebrospinal fluid (CSF) leaks, and degree of fracture comminution [
14].
Repair of anterior table fractures is mainly centered around cosmesis. This can either be addressed with immediate repair or conservatively with observation. When observed, minimally displaced fractures can have bony remodeling and scarring over the depression, which over time may lead to camouflaging the depression. Minimally displaced anterior table fractures without injury to the nasofrontal recess have minimal risk of long-term complications and can be observed. Those with greater displacement (>2 mm) or comminution can be treated with ORIF via numerous approaches. The coronal flap offers the widest exposure but can lead to associated morbidities like scar, alopecia, and paresthesia [
13]. Trephination, suprabrow, or endoscopic brow lift incisions can be used in combination with an endoscope and can offer a minimally invasive approach with smaller scars [
15]. A purely endoscopic approach using an expanded endoscopic frontal sinusotomy, specifically a Draf IIb or Draf III, can allow exposure to the sinus, and the anterior segment can be manually reduced with angled instruments under visualization with an endoscope [
16]. This precludes the need for an external scar but requires expertise in endoscopic sinus surgery.
Posterior table fractures are more likely to need repair and are rarely observed. Posterior table involvement can lead to intracranial complications including CSF leak, meningitis, and brain abscess. Minimally displaced (<2 mm) posterior table fractures without FSOT injury can be observed but should be carefully and closely monitored and assessed for CSF leak. Persistent CSF leaks beyond approximately 1 week should be treated with cranialization or obliteration. Cranialization or obliteration is also indicated in cases of greater displacement (>2 mm) of the posterior wall [
14]. Again, endoscopic surgery using Draf IIb and III procedures can allow for exposure of the posterior fracture, allowing for endoscopic repair [
16]. Fractures of the lateral sinus wall may need trephination or open external approach to improve visualization.
Frontal sinus outflow tract involvement was historically aggressively treated with cranialization or obliteration. However, there has been growing evidence for spontaneous ventilation on follow-up scans even after significant FSOT injury [
17,
18,
19]. These patients need to be very closely followed given the risk of mucocele formation without treatment. Repair of the FSOT involves a wide frontal sinusotomy and stenting of the opening.
Treatment of frontal sinus fractures endoscopically remains limited by the disconnect between trauma surgeons and rhinologists. These fractures are managed by a wide variety of surgeons with training in otolaryngology, plastic surgery, and oral-maxillofacial surgery. Each of these disciplines has a unique training background. The ability to offer an endoscopic repair may be limited by prior exposure to endoscopic techniques, referral patterns, and availability of rhinology and sinus surgeons and proper instrumentation at an institution. Further, endoscopic repair has limited utility in patients with other maxillofacial factures requiring repair or in patients requiring craniotomy, as open repair or cranialization can be performed simultaneously. Endoscopic frontal sinusotomy is best suited for acute frontal sinus fractures that are less than 10 days old to facilitate fracture segment repositioning and/or skull base repair [
16].
There is limited research on the evaluation and management of frontal sinus fractures due to a lack of large patient cohorts and poor attrition rates during follow-up in trauma populations. This retrospective study will review the current demographics, evaluation, and management techniques of frontal sinus fractures at a level 1 trauma center.
Methods
We conducted a retrospective review of patients who presented to a single level I trauma center, the R Adams Cowley Shock Trauma Center at the University of Maryland, from January 1, 2019 to December 31, 2019. A database of all patients who underwent CT face and sinus with or without contrast was queried. Records of patients with non-traumarelated indications were excluded. Radiology reports previously documented by University of Maryland Medical Center board-certified radiologists were reviewed for fracture types, fracture characteristics, and associated injuries. Patients with 1 or more fractures involving the frontal sinus were included. A separate database was then created from this information. Inpatient and outpatient records (Epic Hyperspace, Epic Systems Corporation, Verona, WI) including emergency department, trauma center, inpatient, and outpatient office visits were reviewed. Patient demographics, past medical history, social history, medications, mechanism of injury, fracture characteristics, associated fractures and injuries, surgical service involved, management plans, operative details, and follow-up complaints were collected from each patient’s electronic health record.
Statistical Analysis
Descriptive statistics were performed using an encrypted Microsoft Excel spreadsheet (Microsoft Corporation, Redmond, WA). Statistical analysis was performed using R (version 4.2.0 “Vigorous Calisthenics,” R Foundation for Statistical Computing, Vienna, Austria). The Chi-square test of independence was performed with alpha of .05 using the Yates’ continuity correction. When a Chi-square expected value was less than 5, the Fisher’s exact test was performed with alpha of .05. Odds ratios were calculated for significant associations using the Haldane-Anscombe correction as necessary. This study received approval from the Institutional Review Board at the University of Maryland (HP- 00094851).
Results
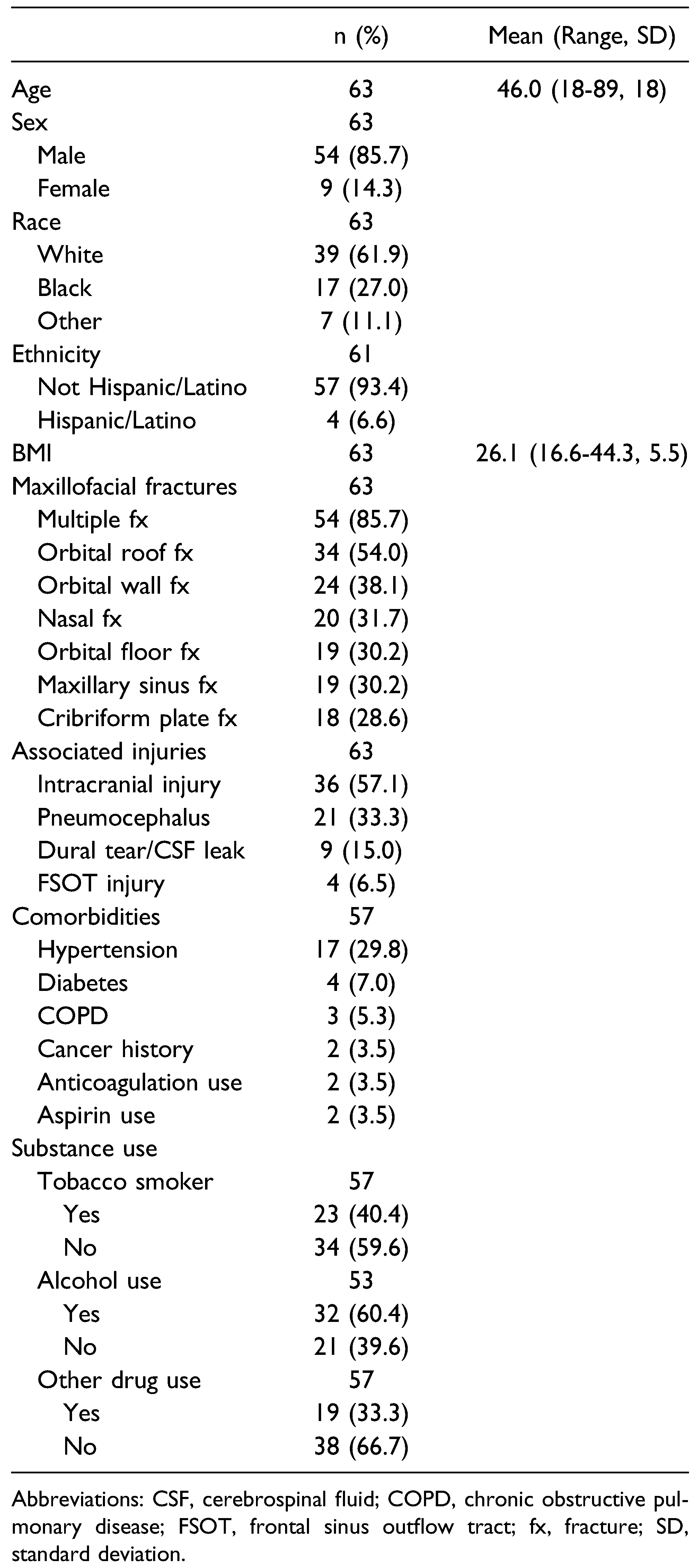
In 2019, 3554 patients presented to Shock Trauma Center and underwent a maxillofacial CT. After excluding patients being evaluated for non-trauma-related indications and removing duplicate scans within the same hospital stay, 2081 patients remained. Of these patients, 858 (41.2%) patients sustained at least 1 maxillofacial fracture. Sixtythree (7.3% of those with a maxillofacial fracture) patients had at least 1 fracture involving the frontal sinus. The mean age of patients with frontal sinus fractures was 46.0 years, and 54 (85.7%) patients were male (
Table 1). Of those patients, thirty-nine (61.9%) patients identified as White and seventeen (27.0%) identified as Black, which is representative of Maryland’s population in 2019 (58% White and 29% Black) [
20]. The most common medical comorbidity in this sample was hypertension (n = 17, 29.8%). According to the social history on admission, alcohol use was reported in 32 (60.4%) patients, smoking tobacco was reported in 23 (40.4%) patients, and other drug use was reported in 19 (33.3%) patients.
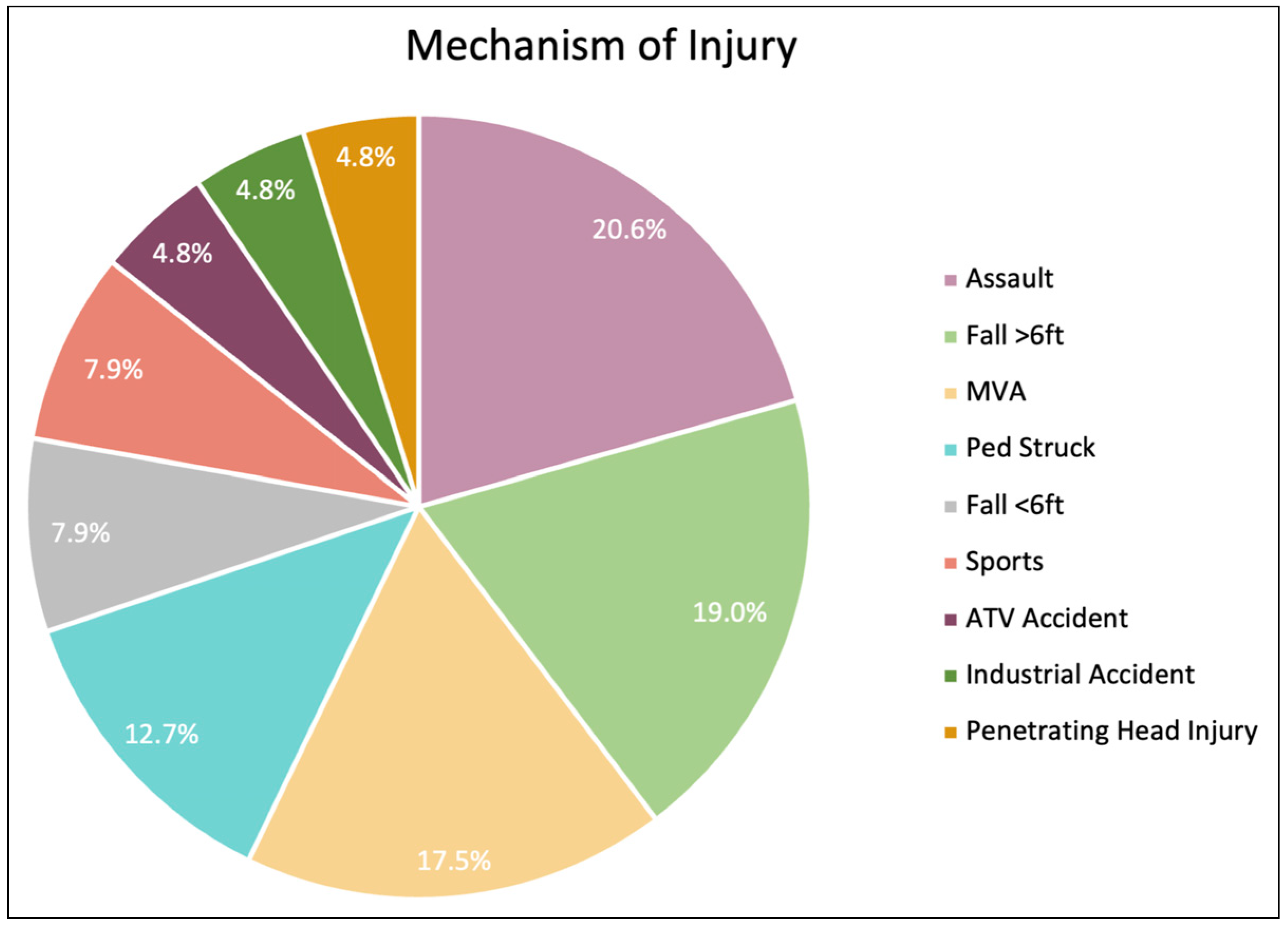
The most common mechanism of injury leading to frontal sinus fracture was falls (n = 17, 27.0%), followed by assaults (n = 13, 20.6%) and then motor vehicle accidents (MVA) (n = 11, 17.5%) (
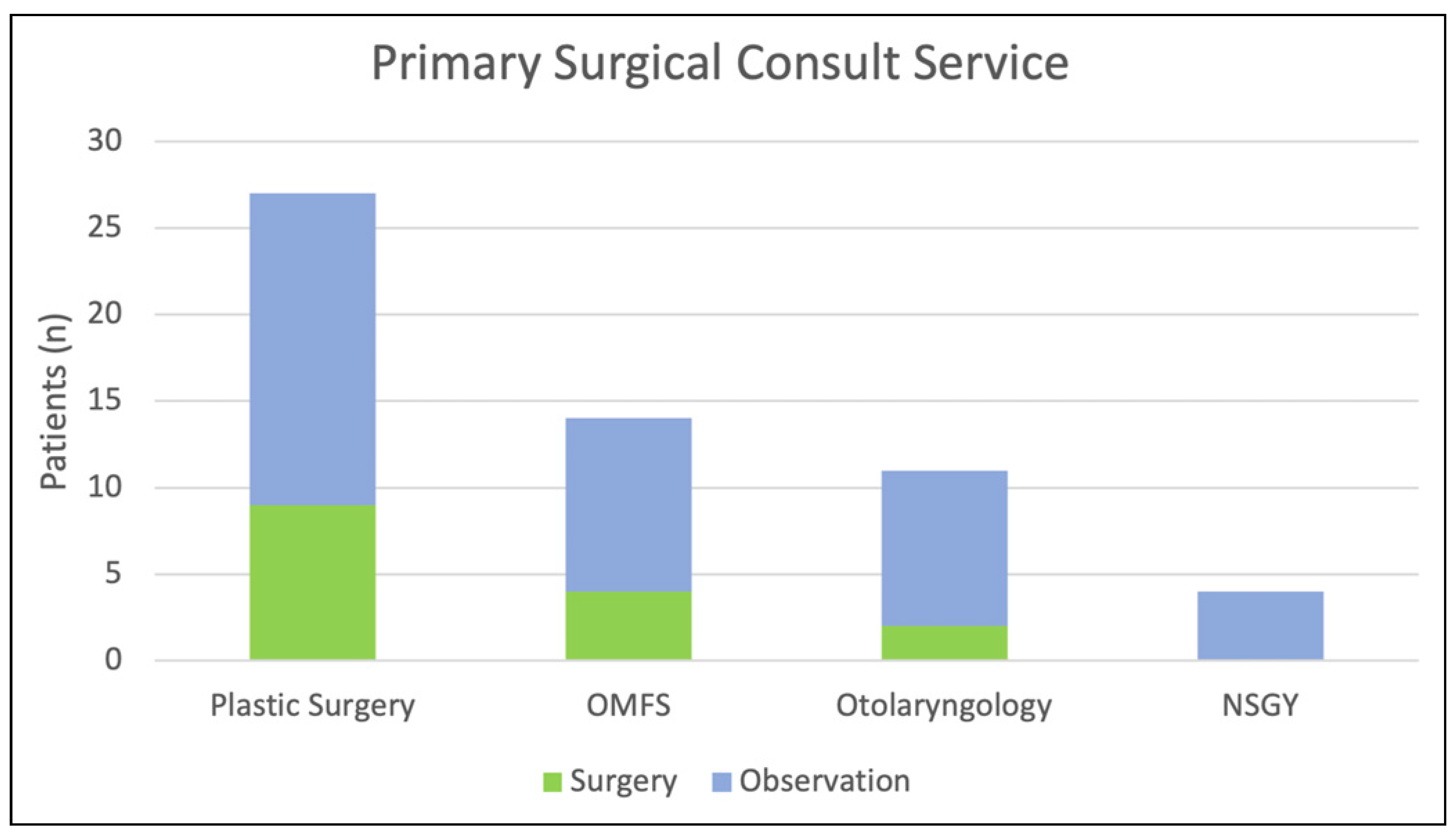
Figure 1). The average hospital length of stay was 8.2 days (range 0 to 62 days), and patients had a mean Glasgow Coma Score of 12.3 on primary evaluation in the trauma resuscitation unit (TRU). Three services split the maxillofacial trauma call calendar: Plastic Surgery, Oral and Maxillofacial Surgery (OMFS), and Otolaryngology (ENT). In this cohort, Plastic Surgery was the most frequently involved surgical consult service (n = 27, 45.8%), followed by OMFS (n = 14, 23.7%) and Otolaryngology (n = 14, 23.7%), then Neurosurgery (n = 4, 6.8%) (
Figure 2). Of the 63 patients, 4 patients were deceased before the maxillofacial trauma services were consulted but after fractures were identified on CT scan, and 3 patients consulted by Otolaryngology died prior to definitive management. No statistically significant association was found between consult service and management strategy (surgery vs observation) (
P = .58).
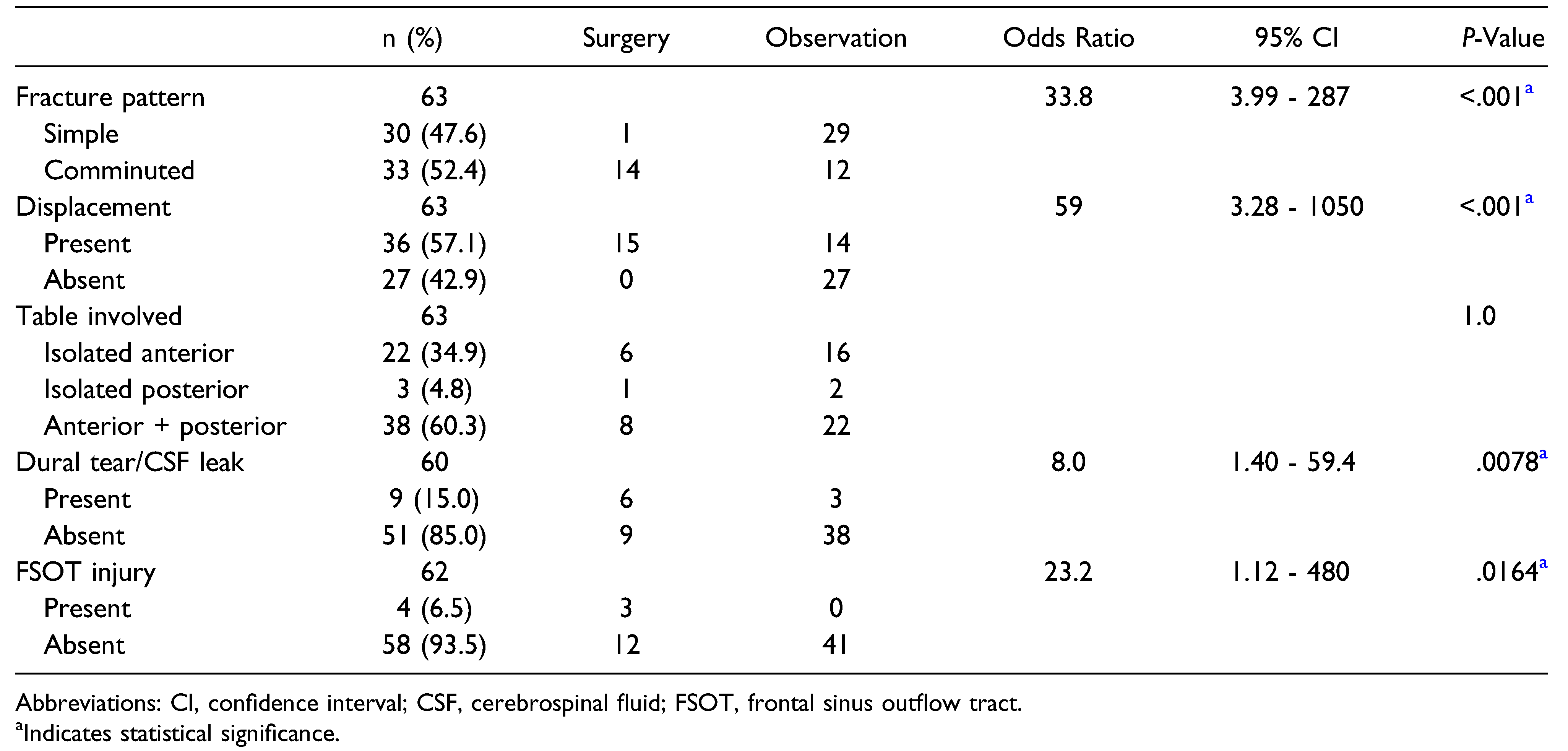
When categorized by fracture pattern, 22 of 63 patients (34.9%) had isolated anterior table fractures, 3 patients (4.8%) had isolated posterior table fractures, and 38 patients (60.3%) had fractures involving both anterior and posterior tables (
Table 2). A total of 33 (52.4%) frontal sinus fractures were comminuted, and 36 (57.1%) were displaced. Both fracture displacement and comminution were significantly associated with surgical intervention (odds ratio [OR] = 59,
P < .0001 and OR = 33.8,
P < .0001, respectively). Anterior or posterior table involvement was not found to be associated with surgical repair vs observation (
P = 1.0). Posterior table involvement compared to isolated anterior table fractures was associated with an 80.5% vs 13.6% risk of intracranial injury (relative risk 5.9,
P < .0001), 46.3% vs 9.1% risk of pneumocephalus (relative risk 5.1,
P < .01), and 18.4% vs 4.5% risk of dural tear/CSF leak (relative risk 4.1,
P = .238).
Fifty-four (85.7%) patients had multiple maxillofacial fractures (
Table 1). Orbital fractures were commonly associated with frontal sinus fractures, affecting 48 (76.2%) of patients. Of these, orbital roof fractures (n = 34, 54.0%) were most common, followed by orbital wall fractures (n = 24, 38.1%). Thirty-six (57.1%) patients sustained other intracranial injuries, and pneumocephalus was present in twenty one (33.3%) patients with frontal sinus fractures. Nine (15.0%) patients were diagnosed with a dural tear or CSF leak.
The presence of a dural tear/CSF leak or FSOT injury was associated with surgical intervention (OR = 8.0,
P = .0078 and OR = 23.2,
P = .016, respectively) (
Table 2). Eight out of nine (88.9%) patients with a dural tear/CSF leak had a posterior table frontal sinus fracture; however, not all dural tears were directly associated with the posterior table fracture according to operative notes. Seven out of nine (87.5%) patients with a dural tear/CSF leak were noted to have pneumocephalus on their CT face. The 2 clinical CSF leaks were managed with external ventricular drainage or observation—the latter resolved spontaneously after repair of facial fractures. The 7 dural defects diagnosed intraoperatively were surgically repaired by neurosurgery. Fractures affecting the FSOT occurred in 4 patients (6.5%), and one of these patients died prior to definitive management. Of the remaining patients, 1 underwent cranialization, 1 underwent ORIF of their anterior table fracture, and 1 underwent ORIF of their anterior table fracture and endoscopic frontal sinusotomy.
There were 7 (11.1%) deaths prior to definitive management of the frontal sinus fracture (
Table 3), 6 of which were due to traumatic brain injury. All 7 patients who died prior to definitive management had frontal sinus fractures that were comminuted, displaced, and involving both anterior and posterior tables. Fifteen (26.8%) of the remaining fifty six frontal sinus fractures were surgically repaired with a mean time to fixation of 6 days (range 1 to 51 days, SD ± 13 days) after diagnosis. Removing the outlier of 1 fracture that was managed as an outpatient 51 days after diagnosis, the mean time to fixation was 2.9 days (range 1 to 11 days, SD ± 2.9 days). The open bicoronal flap approach was used most often (n = 11, 73.3%), followed by existing forehead lacerations in the other 4 (26.7%) patients. Eight (53.3%) patients underwent open reduction internal fixation of their frontal sinus fracture(s); 5 (33.3%) patients underwent cranialization; 1 (6.7%) patient underwent obliteration; and 1 (6.7%) patient underwent open reduction only. Of the 41 (73.2%) of patients who were expectantly managed, none underwent delayed fixation of their frontal sinus fracture to our knowledge. Involvement of the anterior table, posterior table, or both tables was not associated with management strategy, operative approach, or operation type (
P = 1.0,
P = .32, and
P = .091, respectively) (
Table 2 and
Table 3).
When reviewing all patients with frontal sinus fractures, the overall complication rate was 12.5% for those patients on whom we had adequate follow-up data. Thirty-two (57.1%) patients had follow-up longer than 1 week after their frontal sinus fracture diagnosis (mean 4.7 months, range 8 days to 25.5 months). Of these patients, 2 (6.3%) had nerve injuries postoperatively (1 developed temporal branch of the facial nerve paresis and 1 developed frontal nerve hyperesthesia), 1 (3.1%) developed an infection (sinusitis treated with antibiotics), and 1 (3.1%) had a forehead contour deformity. An additional 7 patients (21.9%) complained of headaches, 6 of whom had sustained a concurrent intracranial injury; however, this was not included in our overall complication rate. No patients were reported to have mucocele or hematoma. The patient with a cosmetic deformity had initially declined surgery for their displaced anterior table fracture and was later amenable to undergo delayed outpatient repair of their fracture by otolaryngology; however, the patient did not follow-up to schedule surgery. Only one patient returned to the operating room for loose hardware and underwent hardware removal and scar revision 2 years after the initial operation. Of the 32 patients with follow-up data, 3 of 14 (27.3%) patients that underwent operative fixation of their frontal sinus fracture had one of the abovementioned complications, while only 1 of 18 (5.9%) patients who were observed had a complication. However, this difference was not significant (OR = 4.64, P = .30).
Discussion and Literature Review
In our study sample of an urban population at a level I trauma center, 7.3% of patients presenting with maxillofacial fractures sustained frontal sinus fractures, consistent with the current literature. Two recent reviews of urban trauma centers noted frontal sinus fracture rates of 7.9% and 8.3% [
7,
8]. The most common mechanism of injury in the current study was falls (27.0%), followed by assaults (20.6%) and motor vehicle accidents (17.5%). In comparison, our sample had lower rates of falls (27.0% vs 40.6% and 36%) and MVA (17.5% vs 26.3% and 38%) [
7,
8]. The rate of frontal sinus fractures resulting from MVA has been consistently decreasing in the last 50 years. Strong, Pahlavan, and Saito noted a decline in MVA-associated frontal sinus trauma from 71% to 52% in data collected from 1974 to 1986 compared to 1987 to 2002 [
4]. A more recent meta-analysis by Lopez et al. found a further decline from 54% in 1996–2000 to 33% in 2016–2020 [
21]. Improved motor vehicle safety and traffic laws is likely the reasoning behind this trend, given the decline in fatalities per 100 million vehicle-miles from the 1970s to 2010s and decline in injuries per 100 million vehicle-miles from the 1990s to 2010s [
22]. Compared to Obayemi et al.’s sample [
7], our sample had higher rates of assaults (20.6% vs 13.1%), pedestrians struck (12.7% vs 0%), ATV accidents (4.8% vs 0%), and industrial accidents (4.8% vs 0%). Our results highlight the variety of mechanisms that can cause frontal sinus fractures.
At our institution, facial trauma consults are split among Otolaryngology, Plastic Surgery, and OMFS. Frontal sinus fractures were most often evaluated by Plastic Surgery in this study, likely due to random clustering of cases by trauma call week. Otolaryngology was more likely than Plastic Surgery and OMFS to recommend conservative management; however, this observation was not statistically significant (P = .58). In addition to 4 primary consults managed with observation, Neurosurgery assisted Plastic Surgery with 6 operations highlighting the interdisciplinary nature of this fracture type.
Over 85% of patients in the study sustained multiple maxillofacial fractures, with orbital fractures associated in 76.2% of cases. Sixty percent of fractures were severe enough to traverse both anterior and posterior tables, and fifty-seven percent of patients also suffered from intracranial injuries. As expected and noted in prior reviews, posterior table fractures pose a higher risk for pneumocephalus and dural tear/CSF leak. Our data support this finding with pneumocephalus in 46.3% of posterior table fractures compared to 9.1% of isolated anterior table fractures and dural tear/CSF leak in 21.1% of posterior table fractures compared to 4.5% of isolated anterior table fractures. Overall, patients with identified frontal sinus fractures had an eleven percent mortality rate, 3% higher than a previous study at the same institution over a decade prior [
23]. In such patients, management of traumatic brain injuries and other life-threatening injuries takes precedence over addressing frontal sinus trauma.
The operative repair rate of frontal sinus fractures in this study (26.8%) was consistent with recent published reports of frontal sinus fracture management, with surgical intervention ranging from 25 to 29% [
7,
8]. However, worldwide management of frontal sinus fractures appears to vary. A 2021 review of 338 cases in Israel reported an operative rate of 22.8% [
24], while a similar-sized review published in the same year in Egypt reported an operative rate of 46.1% [
25]. In congruence with proposed frontal sinus management algorithms and other recent studies [
7,
10,
14,
15,
21,
26], both fracture displacement and comminution were significantly associated with surgical intervention in our sample. Fractures were more likely to be operative with associated dural tears/CSF leaks and FSOT involvement. While FSOT injuries with obstruction or displacement are typically operatively managed, many algorithms recommend observation for acute CSF leaks associated with non-displaced posterior table fractures [
10,
14,
15,
23]. Persistent CSF leaks should be repaired endoscopically using a Draf IIb or III to gain access, or open approach if wider visualization is required. Table involvement alone was not associated with management strategy, surgical approach, or operation; however, these results may have been limited by our small sample size.
Our institution’s observation-based approach to nondisplaced frontal sinus fractures is consistent with current opinions in the literature [
10,
12,
15,
26,
27]. All patients in this sample who had non-displaced frontal sinus fractures were managed with observation, and none of these patients required delayed repair to our knowledge. While not statistically significant, the observation group had a lower complication rate than the surgical group. To our knowledge, only 2 prior studies have compared complication rates across observed and surgical groups, both finding lower rates for the observed group [
5,
23]. Observation with long-term follow-up can be a safe and effective management strategy for frontal sinus fractures; however, this may be challenging in the trauma population given poor follow-up rates. In our sample, the overall average follow-up was 118 days including 17 patients treated conservatively with no followup, limiting our evaluation of long-term complications. Given poor follow-up in the trauma population, this may also influence the surgeon’s decision to observe these fractures. Reported rates of complications resulting from frontal sinus fractures are quite variable in the literature. Here, we report a 12.5% overall complication rate. This is higher than Lopez et al.’s recent meta-analysis reporting a 9.3% complication rate [
21] but lower than Viezel-Mathieu et al.’s recent study reporting 26% [
8].
The endoscopic endonasal approach, as well as the combined endoscopic brow lift approach, allows for access to both anterior and posterior tables without the morbidity of traditional open approaches. The endoscopic endonasal approach can be used to address FSOT injuries as well as to allow for frontal sinusotomy with stenting [
13,
16]. Only 1 otolaryngologist utilized an endoscopic approach to an FSOT injury in this sample. In this case, an open approach was still utilized to reduce the anterior table fracture after failure of the endoscopic approach to reduce the fracture. This was thought to be related to a delay in repair greater than 10 days since injury. The limited use of these minimally invasive approaches is likely due to the complexity of maxillofacial trauma patients, with a majority of patients sustaining multiple craniofacial fractures often requiring concurrent repair. The additional training requirement to master these approaches and limited exposure to endoscopy during Plastic Surgery and OMFS residencies may also contribute. Further, there may be limited access or referral patterns to rhinologists and sinus surgeons who may help address these fractures using an endoscopic approach. Endoscopic approaches to the frontal sinus provide excellent functional and aesthetic outcomes [
16,
28,
29]. Additionally, the FSOT can be widened to facilitate frontal drainage via the Draf IIb or III endoscopic procedure, minimizing the risk of sinusitis or mucocele [
16,
26,
30]. While they limit swelling and scarring, reduction of fracture components can be more challenging with endoscopy and thus careful patient selection is key [
31]. Despite the safety and efficacy of endoscopic management of frontal sinus fractures [
16], this approach remains infrequently utilized due to provider training and experience based on our sample and others [
7,
8]. This points to an excellent opportunity for collaboration between maxillofacial trauma surgeons and rhinologists with expertise in endoscopic techniques.
The frequency of FSOT injuries in our sample was less than that currently reported in the literature (6.5% vs 25–50%) [
11]. A prior study found the rate of FSOT injury evident on CT imaging was 96% after retrospective review of the imaging compared to 3% on initial radiology reports [
32]. Our study was based on CT scan reports read by radiologists; therefore, our rate is likely under representative of the true incidence. Two patients in this study with FSOT injuries had surgery to address the fracture—1 via cranialization and 1 via endoscopic frontal sinusotomy. The patient who did not undergo operative intervention for their FSOT was noted to be at a high risk for nasofrontal duct obstruction on post-operative imaging. While this patient did not develop complications in the 11 days post-operatively from ORIF of their anterior table fracture, no long-term follow-up was established, and it is unknown if the patient developed sinus obstruction or other complications. It is recommended that patients with a patent but fractured FSOT undergo observation with repeat imaging in 2 to 6 months and at 12 months to assess aeration of the frontal sinuses [
15,
23,
26,
33]. There is mounting evidence that FSOT injury increases the risk of complications, highlighting the importance of assessing patency of the FSOT in patients with frontal sinus trauma [
21,
23]. However, this close long-term follow-up and opting for observation may be difficult in the trauma population given the lack of reliable long-term follow-up.
Limitations
This review has several limitations. First, frontal sinus fractures identified on imaging other than maxillofacial CT are not captured in our sample. However, given the indication for maxillofacial CT in trauma patients with known or suspected facial fractures, we believe that our methods likely captured most frontal sinus fractures. Second, fracture characteristics were reviewed based on radiology reports, consult notes, and operative notes. Any findings not documented in the electronic medical record were not captured. Third, there is inherent variability in treatment plans across surgeons and institutions, especially for a fracture type without a clear consensus on management algorithms. The various surgical services involved in evaluating frontal sinus fractures have different training backgrounds and techniques for addressing these fractures. For example, otolaryngology is more likely to incorporate endoscopic approaches in managing frontal sinus fractures given that endoscopic sinus surgery training is a part of most otolaryngology training programs [
33]. However, we recognize that surgeons at our institution have limited training and experience in endoscopic management of frontal sinus trauma, which leads to bias toward open approaches in this study. This also highlights a deficit and opportunity for collaboration between maxillofacial trauma surgeons and rhinologists with expertise in endoscopic access to the frontal sinus. Fourth, our evaluation of complications is limited by a poor follow-up rate in this trauma population. Almost half of patients studied did not have follow-up beyond 1 week, including 1 patient who underwent operative fixation of their frontal sinus fracture. If patients presented to an outside hospital with complications related to their frontal sinus fracture, these complications were not captured in our analysis. Finally, the results are limited by our sample size, especially for subgroup analyses. Association analyses should be interpreted with caution.