Introduction
Trauma injuries comprise ten percent of worldwide deaths per year, surpassing global mortality due to HIV/AIDS, tuberculosis, and malaria combined [
1]. A majority of trauma burden includes the head and neck region [
1,
2]. Within the craniomaxillofacial (CMF) skeleton, fractures of the man- dible are common and comprise between 20 and 50% of CMF fractures managed at large trauma centers [
3]. While mandible fracture treatment is fairly well established in high resource settings, the majority of fractures occur in low and middle-income countries (LMICs), which have substantial limitations on resources and equipment [
4,
5].
Unlike other bones of the CMF skeleton, the mandible is under significant masticatory force. As such, suboptimal treatment of mandibular fractures can result in life-altering complications such as malunion, non-union, and infection [
6]. The primary goal in the treatment of mandible fractures is to ensure anatomic healing across fracture segments and a return to premorbid occlusion. For some mandibular frac- tures this is achieved by surgical exposure, reduction, and fixation of the bone fragments. Untreated, mandible frac- tures can result in malocclusion, trismus, infection, airway compromise, and even death.
The gold standard for fixation of mandible fractures is the use of plates and screws to facilitate rigid osteosynthesis [
7]. These materials are often not available in LMICs given their high cost. Prior to the widespread adoption of plates and screws, interosseous wiring was used to achieve semi-rigid fixation and wire osteosynthesis [
8,
9]. Plating alternatives such as interosseous wiring or maxillomandibular fixation (MMF) are relied upon in many LMICs, as these techniques can be performed inexpensively and the materials remain widely available.
Interosseous wiring was first described in 1847 and continues to be widely employed today [
8,
9], yet force analysis studies of the technique do not exist. In this study, we use cadaveric mandibles to compare formations of interosseous wiring to each other and to rigid internal fixation with plates and screws. We aim to provide objective evidence regarding the most stable interosseous wiring formations to CMF surgeons practicing in resource-limited settings, when plates and screws are not available.
Methods
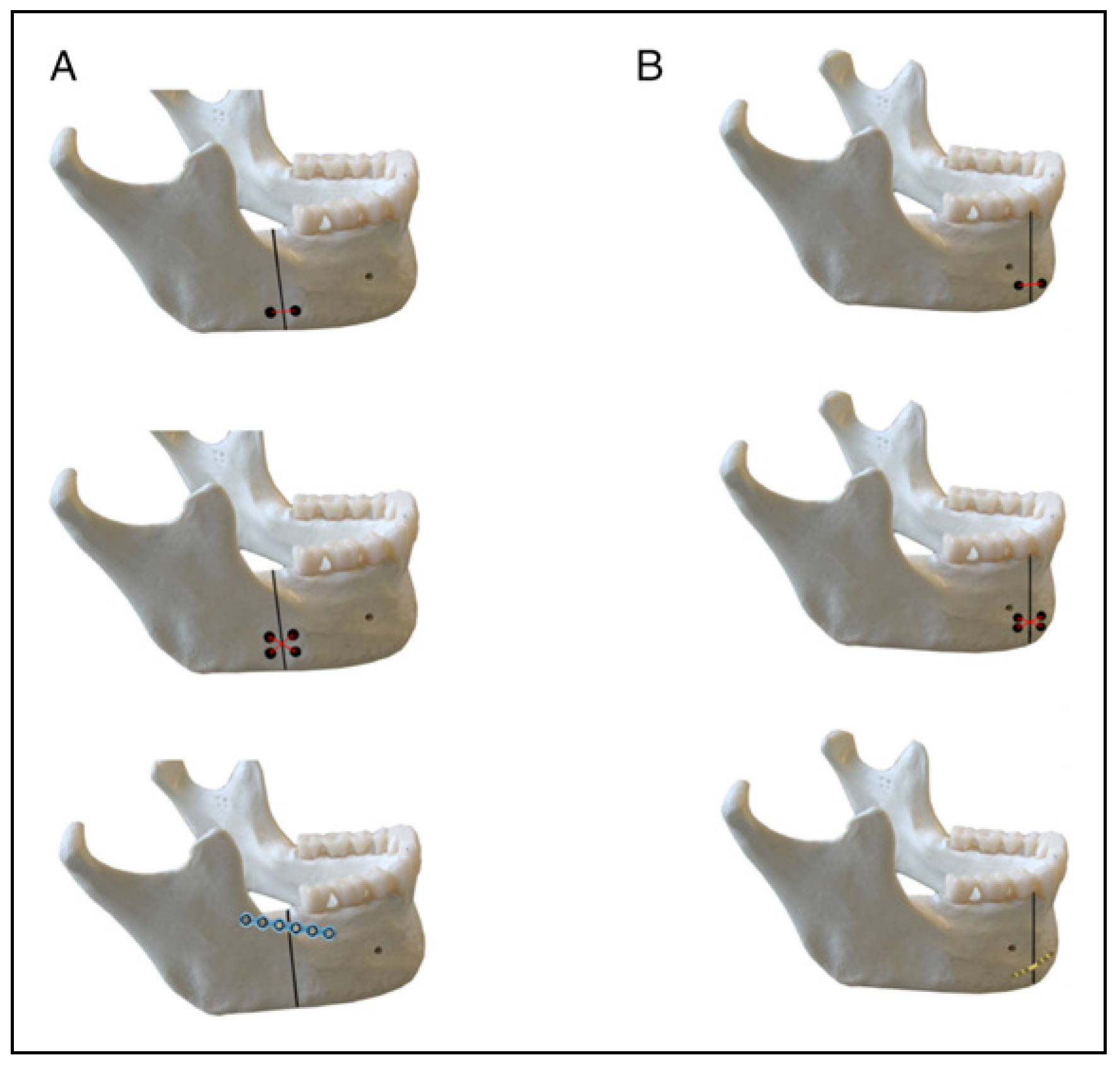
All studies were conducted at the Massachusetts Eye and Ear Infirmary (MEE) or Massachusetts Institute of Tech- nology (MIT) between July 2018 and July 2020. Human cadaveric tissue was obtained from the Anatomy Gifts Registry (Hanover, MD, USA) and transported to a des- ignated research surgical suite. All cadavers were screened for infectious diseases including HIV, HTLV, Hepatitis B and C, and CMV. All operative photographs taken for research purposes were de-identified. As solely a cadaver study that did not involve live subjects, this study was exempt from requiring Institutional Review Board approval. Fractures of the mandibular angle and parasymphysis were created using a non-powered bone saw. Five trials were performed for each fixation method at both fracture sites. Bicortical holes were created with a DePuy Synthes (Raynham, MA, USA) 1.5 mm drill bit in a standard fashion. Osseous holes intended for interosseous wiring were uniformly placed 2 mm from the fracture line, 2 mm from the border of the mandible, and 2 mm from any ad- ditional drill hole. Interosseous wire formations that were tested included (1) a two-hole interosseous wire loop and (2) a four-hole figure-of-eight interosseous wire formation. Twenty-four gauge stainless steel wire was passed through the drilled holes and twisted down to achieve fixation. For parasymphyseal fractures, plating was achieved by fixation of a 2 mm locking 6 hole titanium plate with 12 mm bi- cortical screws. For mandibular angle fractures, plating was achieved by a 2 mm locking 6 hole titanium plate along the oblique ridge (i.e., “Champy technique”), using 8 mm monocortical screws. The tested wire and plating formations are demonstrated graphically in
Figure 1. An FM-204-100K Digital Force Gauge (M&A Instruments Inc, Arcadia, CA, USA) was used to measure forces, in Newtons (N), directed along the direction of the masseter muscle. Outcomes were the force at which fracture diastasis was first observed, and the force to induce failure of fixation technique. Full failure was defined as the two portions of the mandible detaching from one another.
All cadavers used in the study were males between 60 and 70 years old. Status of dentition was recorded to account for variability in bone stock. Statistical analysis was per- formed using STATA 16.0 (StataCorp, College Station, TX, USA). A one-sample student t-test was used to determine significant differences in failure forces with a P-value of .05 used as the threshold for significance.
Results
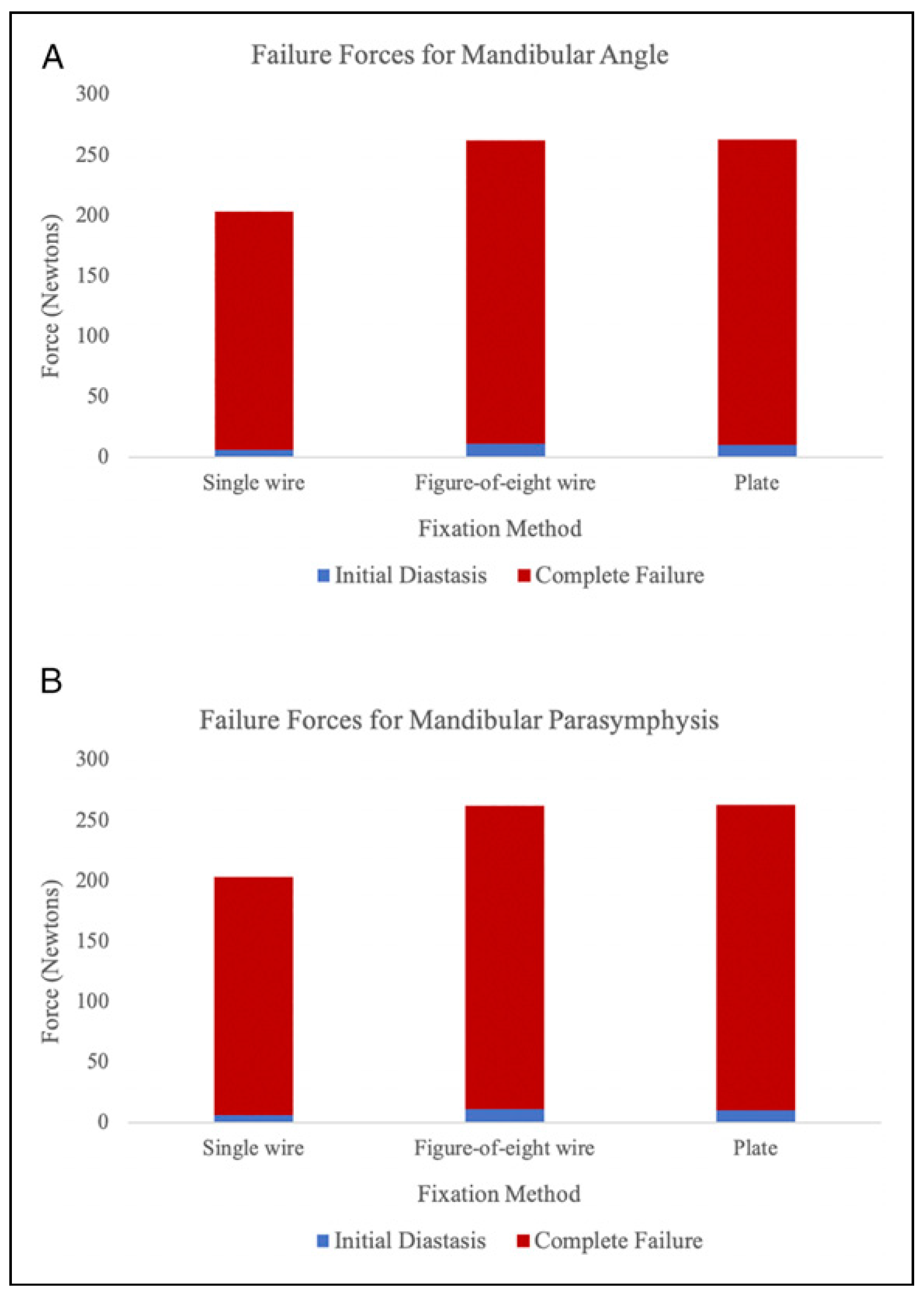
Overall results for both mandibular and parasymphyseal fractures are demonstrated graphically in
Figure 2. As expected, the diastasis force was significantly lower than the failure force. Failure forces were not significantly different between the figure-of-eight wiring and plating, which approached the maximal testable forces with the described testing setup and surpassed physiologic forces.
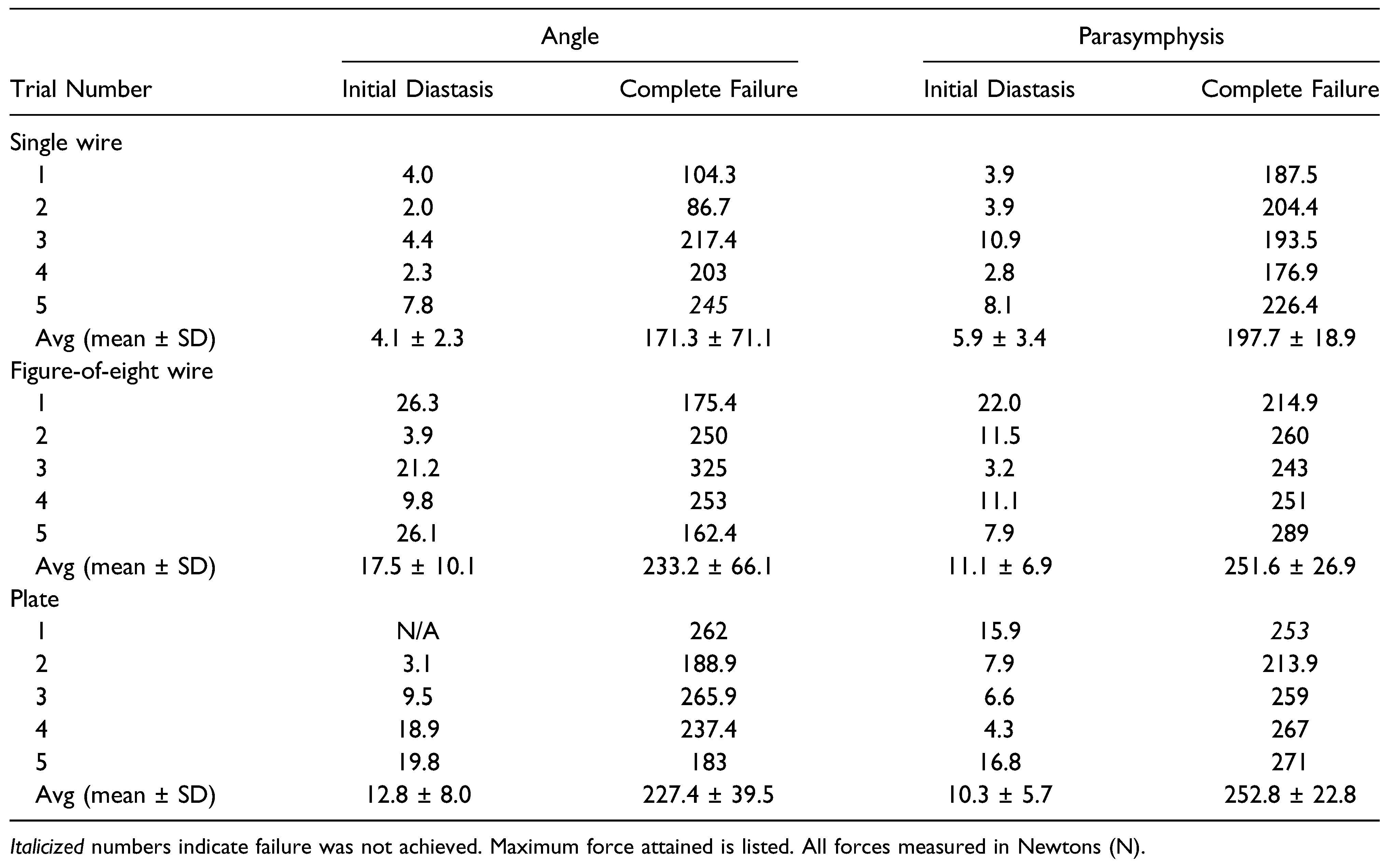
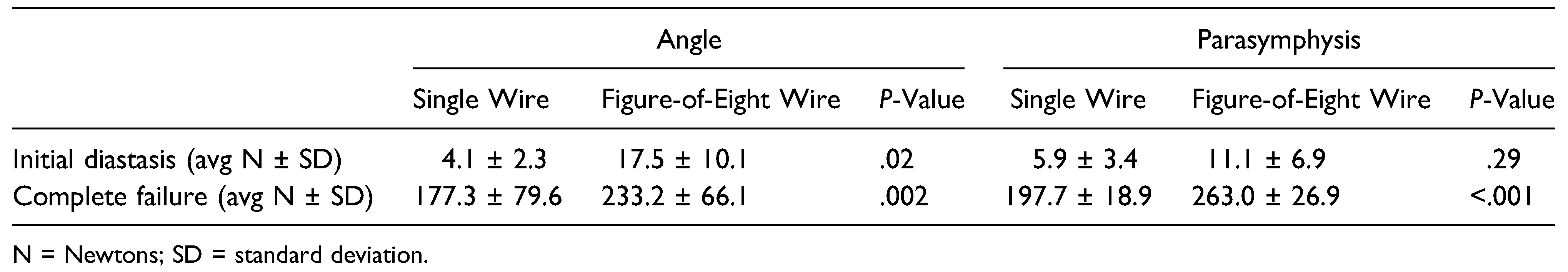
For mandibular angle fractures, the mean force required to achieve diastasis, or separation from bony contact of two segments, was 4.1 N (SD 2.3), 17.5 N (SD 10.1), and 12.8 N (SD 8.0) for single wire, figure-of-eight wiring, and plating, respectively (
P < .001). The mean force required to achieve complete failure was 171.3 N (SD 71.1) for single wire, 233.2 N (SD 66.1) for figure-of-eight wiring, and 227.4 N (SD 39.5) for plating (
P < .001) (
Table 1).
Similarly, for parasymphyseal fractures, the average force required to achieve initial diastasis was 5.9 N (SD 3.4), 11.1 N (SD 6.9), and 10.3 N (SD 5.7) for single wire, figure- of-eight wire, and plating, respectively. The difference in mean force required to achieve initial diastasis was not statistically significant (
P = .29). The mean force required to achieve complete failure was 197.7 N (SD 18.9) for single wiring, 251.6 N (SD 26.9) for figure-of-eight wiring, and 252.8 (SD 22.8) for plating. The difference for complete failure between single wiring and figure-of-eight wiring was statistically significant (
P = .002) (
Table 2). Notably, complete failure was not reached in a majority of the figure- of-eight wiring and plating cadavers. For these trials, maximum force achieved was used for the purposes of statistical analysis.
Discussion
Plates and screws are the gold standard to provide rigid internal fixation (RIF) of most mandibular fractures [
5,
7]. However, these materials are costly and frequently un- available to many patients in LMICs. Until RIF materials become readily available throughout the world, investigations of interosseous wire formations yield important data. This study shows that interosseous wiring can provide significant stability to a mandibular fracture, with a figure-of-eight wire formation providing significantly more stability than a simple wire loop. The force required for diastasis was low in this study, and in physiologic conditions would likely be higher due to the significant soft tissue attachments that would provide stability to the mandible. However, the absolute failure force shows significantly higher stability with a figure-of-eight wire formation. Notably, the distance that the holes for the interosseous wiring were placed from the fracture line may have significant clinical implications in providing stability.
Biomechanical force analysis studies have provided useful information for clinicians, particularly in the field of orthopedic surgery. Load-to-failure testing has been used to examine different plating types for femur fractures, radius fractures, and spinal fixation, providing valuable insight into the feasibility and outcomes of using new materials and plating alternatives [
10,
11,
12]. These studies have not been as well described for mandible fractures, particularly for in- terosseous wiring [
13]. Champy et al. identified that strains within the mandible do not exceed 550 N/mm
2, though generally the mandible is subjected to significantly smaller strain [
14]. Forces examining jaw mechanics show that under normal conditions, the mandible is subjected to a series of deformations, stresses, and strains during chewing, biting, and speaking [
15]. Forces in the range of 44.6–74.4 kg/m
2 can cause a mandibular fracture in healthy bone [
16]. Repairs of mandibular fractures must be able to withstand physio- logical forces to ensure proper healing and prevent infec- tion. This study shows that to withstand physiologic forces across the cadaveric mandible, interosseous wiring provides adequate, but not superior, support compared to plate and screw fixation.
Due to the paucity of data on the repair of mandible fractures with interosseous wiring, we compared our results with internal fixation in other anatomical subsites described in the literature. Force analysis studies examining the failure force of interosseous wiring in fifth metatarsal fractures in comparison with tension bands shows that interosseous wiring can withstand forces of up to 113.7 ± 46.6 N [18]. These fixations involve smaller bones, however, and may not be accurately translated to the forces that a mandible fixation could withstand. Comparatively, our study showed that figure-of-eight interosseous wiring provides stability at a force of greater than 250 N. This compared favorably to the stability achieved by the gold standard for mandibular fixation, the use of plates and screws. Additionally, the existing limited studies examining outcomes for interosseous wires show that they can be an effective tool in achieving bony union (100%) and occlusion (100%) with a 5–12% infection rate [
8,
9]. This is particularly pertinent as approximately 90% of global trauma occurs in LMICs, where interosseous wiring may be one form of internal fixation [
5,
17,19,20].
The results of this study must be viewed within the context of the study design. The primary outcome measure in this project was the linear pulling force across the mandibular fracture zone; in vivo, however, complex, multi- vector muscular forces act in concert on the mandible. The variation in bone strength between mandibles results in each specimen having different biomechanical force properties; specifically, each mandible will vary in bone density, which could cause some variability in the failure force of plating alternatives. We attempted to control for this by using only cadavers between 60 and 70 years old. Notably, there is also significantly less variation in mandibular bone density as compared to weight bearing bones affected by osteoporosis [21]. We were limited to testing the force achieving first diastasis and the maximal failure force in mandible spec- imens; however, in physiologic conditions the mandible endures forces in a number of vectors and magnitudes.
Despite these limitations, this study is one of the first to examine interosseous wiring in direct comparison to tita- nium plating for the fixation of mandible fractures. In LMICs where interosseous wiring is sometimes used, identifying the most stable methods of fracture fixation offers significant utility. The biomechanical data from testing the failure forces show that interosseous wiring still holds significant clinical utility, and informs clinicians that figure-of-eight wiring may be a viable alternative when traditional plating options are not available.