The Effect of Chitohem Bleeding Inhibitor Powder on Pain and Bleeding After Tonsillectomy by Suturing Method
Abstract
:Introduction
Method and Materials
Results
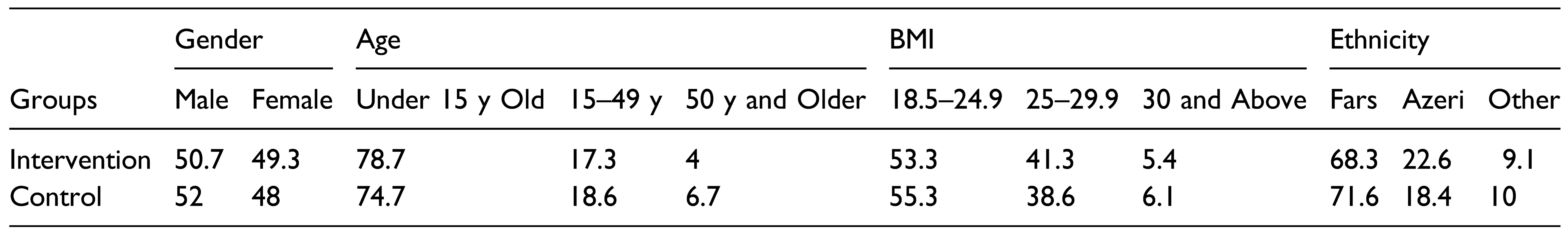
Background Factors (Gender, Age, BMI Index, and Ethnicity)
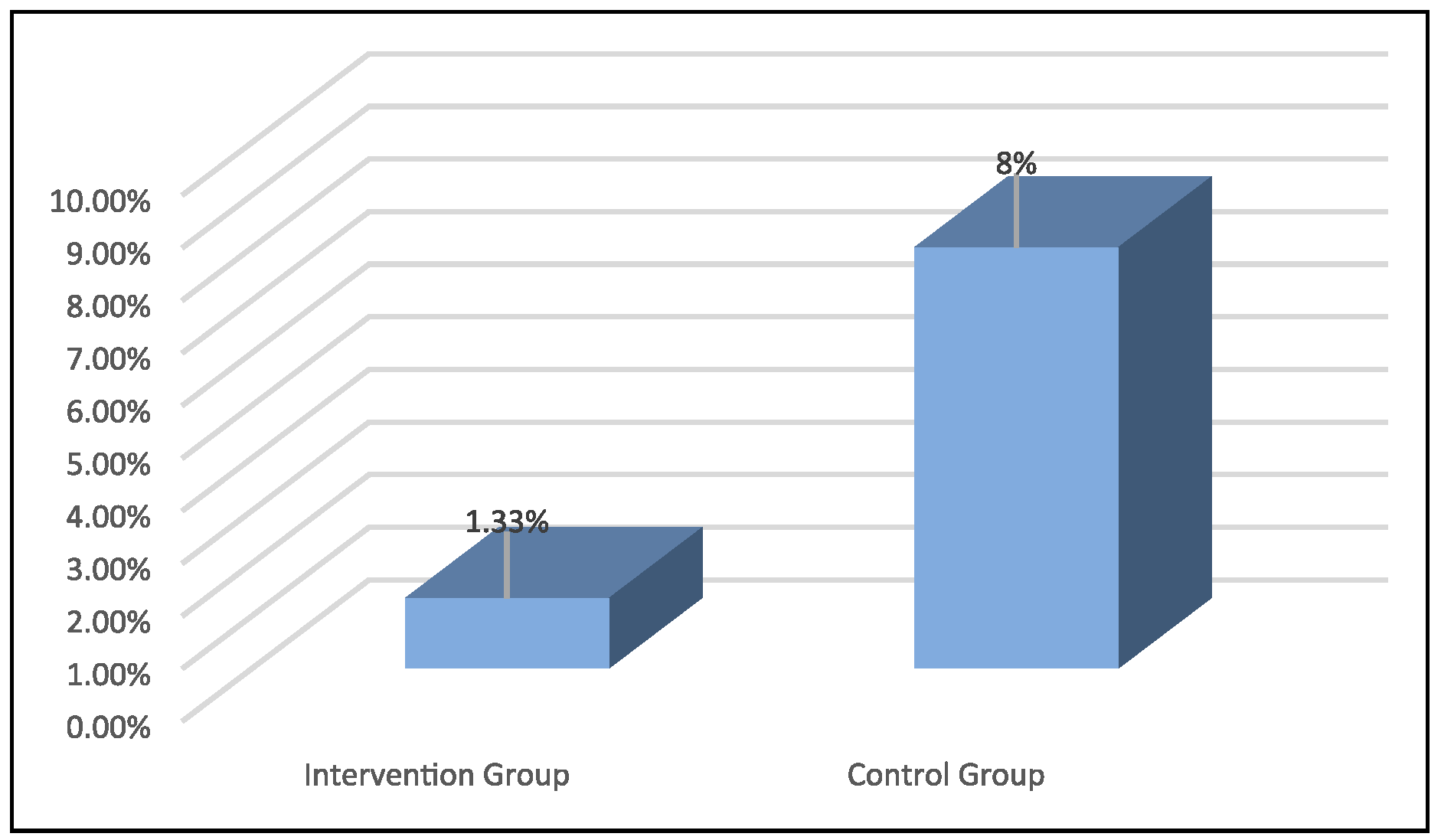
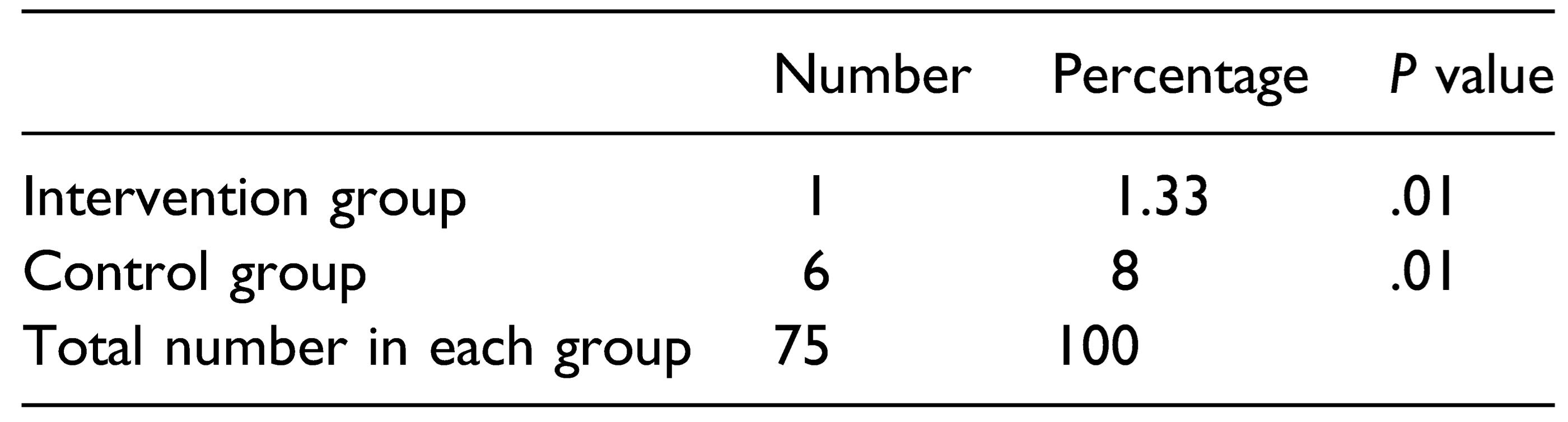
Frequency of Bleeding in the First 24 hours
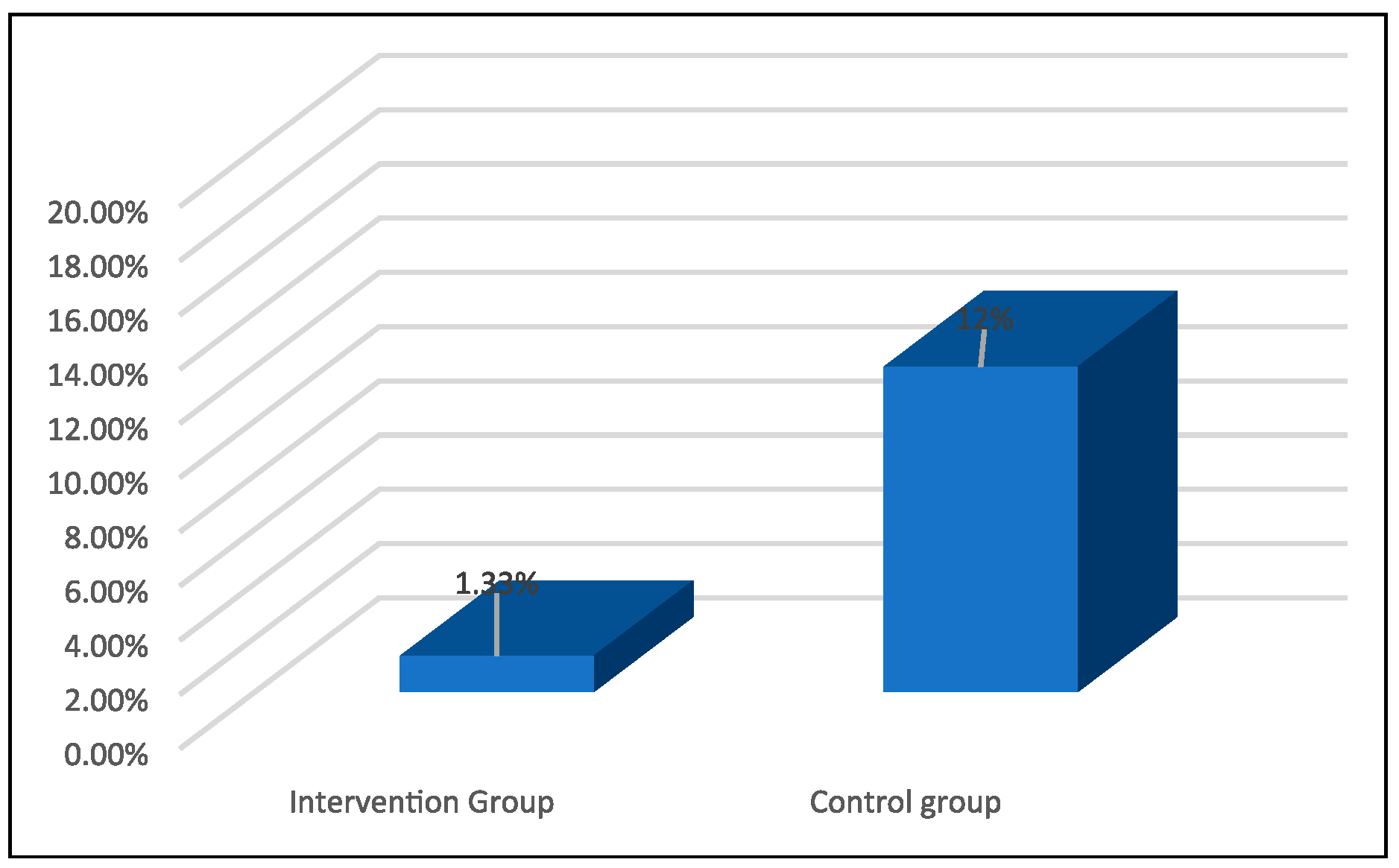
Frequency of Using Analgesics (Apotel) in the First 24 hours After Surgery
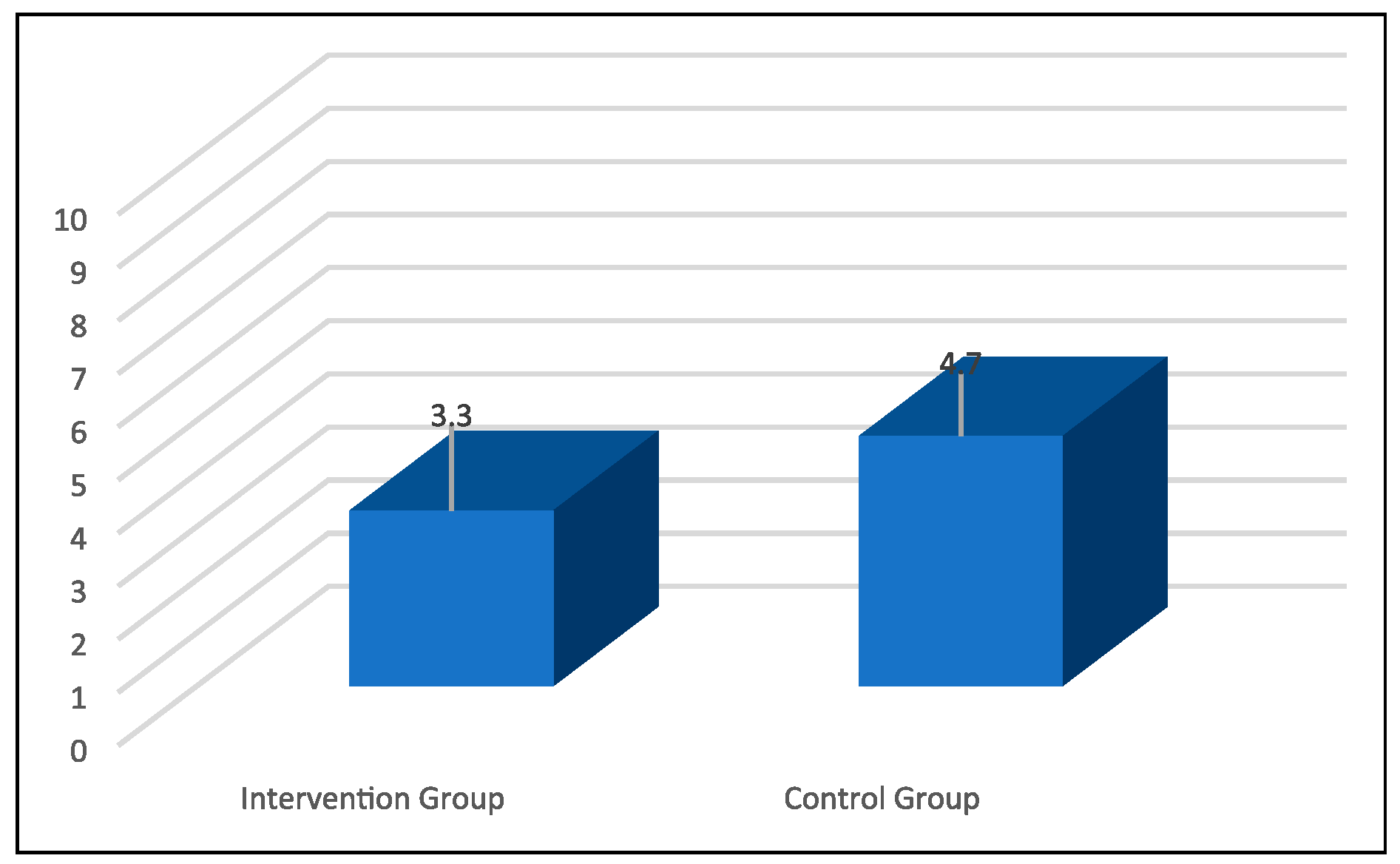
Postoperative Feeding Onset Time in Both Groups
Discussion
Conclusion
Funding
Ethical Statement
Acknowledgments
Conflicts of Interest
| 1. | A single-blind study occurs when the participants are deliberately kept ignorant of either the group to which they have been assigned or key information about the materials they are assessing, but the experimenter is in possession of this knowledge. Single-blind studies are typically conducted when the participants’ knowledge of their group membership or the identity of the materials they are assessing might bias the results [26]. |
References
- Stelter, K. Tonsillitis and Sore Throat in Children. In GMS Current Topics in Otorhinolaryngology, Head and Neck Surgery; 2014; p. 13. [Google Scholar]
- Bhattacharyya, N.; Kepnes, L.J. Economic benefit of tonsillectomy in adults with chronic tonsillitis. Ann. Otol. Rhinol. Laryngol. 2002, 111, 983–988. [Google Scholar] [CrossRef]
- Spinou, C.; Kubba, H.; Konstantinidis, I.; Johnston, A. Role of tonsillectomy in histology for adults with unilateral tonsillar enlargement. Br. J. Oral Maxillofac. Surg. 2005, 43, 144–147. [Google Scholar] [CrossRef] [PubMed]
- Sunkaraneni, V.; Jones, S.; Prasai, A.; Fish, B. Is unilateral tonsillar enlargement alone an indication for tonsillectomy? J. Laryngol. Otol. 2006, 120, 1. [Google Scholar] [CrossRef]
- Marchica, C.L.; Dahl, J.P.; Raol, N. What's New with Tubes, Tonsils, and Adenoids? Otolaryngol. Clin. 2019, 52, 779–794. [Google Scholar] [CrossRef] [PubMed]
- Morad, A.; Sathe, N.A.; Francis, D.O.; McPheeters, M.L.; Chinnadurai, S. Tonsillectomy versus watchful waiting for recurrent throat infection: a systematic review. Pediatrics 2017, 139. [Google Scholar] [CrossRef] [PubMed]
- De Luca Canto, G.; Pacheco-Pereira, C.; Aydinoz, S.; Bhattacharjee, R.; Tan, H.L.; Kheirandish-Gozal, L.; et al. Adenotonsillectomy Complications: A Meta-analysis. Pediatrics 2015, 136, 702–718. [Google Scholar] [CrossRef]
- Bhattacharyya, N.; Kepnes, L.J.; Shapiro, J. Efficacy and quality-of-life impact of adult tonsillectomy. Arch. Otolaryngol. Head. Neck Surg. 2001, 127, 1347–1350. [Google Scholar] [CrossRef]
- Baumann, I.; Kucheida, H.; Blumenstock, G.; Zalaman, I.M.; Maassen, M.M.; Plinkert, P.K. Benefit from tonsillectomy in adult patients with chronic tonsillitis. Eur. Arch. Oto-Rhino-Laryngol. 2006, 263, 556–559. [Google Scholar] [CrossRef]
- Kollar, P.; Suchy, P.; Muselik, J.; Bajerova, M.; Havelka, P.; Sopuch, T. Hemostatic effects of oxidized cellulose. Česká Slov. Farm. 2008, 57, 11–16. [Google Scholar]
- Shafaeifard, S.; Sarkarat, F.; Pahlevan, R.; Ezati, A.; Keyhanlou, F. Investigating the effect of Chitobem powder on coagulation time and the complications following tooth extraction. J. Res. Dent. Sci. 2017, 14, 138–143. [Google Scholar]
- Hajizadeh, S.; Shariati, A.; Jahani, S.; Haibar, h.; Haghighizadeh, M.H. Comparison of Chitoflem powder and sand bag for controlling bleeding after femoral angiography. Jundishapur J. Chronic Dis. Care 2018, 7. [Google Scholar]
- 13. Kordestani, S.S.; Noohi, F.; Azarnik, H.; et al. A randomized controlled trial on the hemostasis of femoral artery using topical hemostatic agent. Clin. Appl. Thromb./Hemost. 2012, 18, 501–505. [Google Scholar]
- Chamanzari, H.; Choubdar, M.; Shariffpour, F.; Ghollami, H.; Daneshvari, F. Comparison of Celox powder and conventional dressing on hemostasis of vascular access site in hemodialysis patients. Evidence-Based Care 2015, 4, 25–34. [Google Scholar]
- Hejazi, F.; Hosseinzadeh, F.; Irani Rad, L.; Bagheri, A.; Vahedian, M.; Damanpak, V. Effectiveness of Celox powder and standard dressing in control of angiography location bleeding. J. Babol Univ. Med. Sci. 2013, 15, 30–36. [Google Scholar]
- Brown, M.A.; Daya, M.R.; Worley, J.A. Experience with chitosan dressings in a civilian EMS system. JEM (J. Emerg. Med.) 2009, 37, 1–7. [Google Scholar]
- Wedmore, I.; McManus, J.G.; Pusateri, A.E.; Holcomb, J.B. A special report on the chitosan-based hemostatic dressing: experience in current combat operations. J. Trauma Acute Care Surg. 2006, 60, 655–658. [Google Scholar]
- Mortazavi, S.; Atefi, M.; Roshan, S.P.; Tanide, N.; Radpey, N.; Bagheri, Z. Characteristics of Cool Clot, the Invented Novel Hemostatic Agent. Sci. J. Iran. Blood Transfus. Organ. (KHOON) 2011, 8. [Google Scholar]
- Nouri, S.; Sharif, M.R.; Jamali, B.; Panahi, Y. Comparison the effect of calcium sulfate and ferric sulfate in controlling liver bleeding: an animal model study. Razi J. Med. Sci. 2016, 22, 27–34. [Google Scholar]
- Nouri, S.; Sharif, M.R. Hemostatic effect of aluminum chloride in liver bleeding: an animal model study. Tehran Univ. Med. J. TUMS Publ. 2014, 72, 435–442. [Google Scholar]
- Hashemi Tayer, A.; Amirizadeh, N.; Almasi-Hashiani, A.; Kamravan, M.; Mohammadi, M. A new fibrin sealant: hemostatics evaluation in the animal model. Sci. J. Iran. Blood Transfus. Organ. 2013, 10. [Google Scholar]
- Darbemanneh, G.; Hashemi, A.; Kordestani, S.S.; Karimian, F.; Najarian, S. A novel haemostatic powder delivery device applicable in minimally invasive surgery. JMET (J. Med. Eng. Technol.) 2014, 38, 32–36. [Google Scholar]
- Masova, L.; Rysava, J.; Krizova, P.; et al. Hemosvptic effect of oxidized cellulose on blood platelets. Sb. Lek. 2003, 104, 231–236. [Google Scholar] [PubMed]
- Pierce, G.F.; Mustoe, T.A.; Altrock, B.W.; Deutel, T.F.; Thomason, A. Role of platelet-derived growth factor in wound healing. J. Cell Biochem. 1991, 45, 319–326. [Google Scholar] [PubMed]
- Golebiewska, E.M.; Poole, A.W. Platelet secretion: From haemostasis to wound healing and beyond. Blood Rev. 2015, 29, 153–162. [Google Scholar]
- Salkind, N. Single-Blind Study. In Encyclopedia of Research Design; Sage: Thousand Oaks, CA, USA, 2010. [Google Scholar]
 |
 |
 |
 |
© 2022 by the authors. Multimed Inc.
Share and Cite
Seied-Mohammad Doulabi, S.-R.; Moradi, A.; Roozbahany, N.A.; Rezaei, S.; Khoshfetrat, N.; Shamsian, F.; Baghi, M. The Effect of Chitohem Bleeding Inhibitor Powder on Pain and Bleeding After Tonsillectomy by Suturing Method. Craniomaxillofac. Trauma Reconstr. 2023, 16, 205-210. https://doi.org/10.1177/19433875221092571
Seied-Mohammad Doulabi S-R, Moradi A, Roozbahany NA, Rezaei S, Khoshfetrat N, Shamsian F, Baghi M. The Effect of Chitohem Bleeding Inhibitor Powder on Pain and Bleeding After Tonsillectomy by Suturing Method. Craniomaxillofacial Trauma & Reconstruction. 2023; 16(3):205-210. https://doi.org/10.1177/19433875221092571
Chicago/Turabian StyleSeied-Mohammad Doulabi, Seied-Reza, Alireza Moradi, Navid Ahmady Roozbahany, Sohbat Rezaei, Niloufar Khoshfetrat, Fahime Shamsian, and Mehran Baghi. 2023. "The Effect of Chitohem Bleeding Inhibitor Powder on Pain and Bleeding After Tonsillectomy by Suturing Method" Craniomaxillofacial Trauma & Reconstruction 16, no. 3: 205-210. https://doi.org/10.1177/19433875221092571
APA StyleSeied-Mohammad Doulabi, S.-R., Moradi, A., Roozbahany, N. A., Rezaei, S., Khoshfetrat, N., Shamsian, F., & Baghi, M. (2023). The Effect of Chitohem Bleeding Inhibitor Powder on Pain and Bleeding After Tonsillectomy by Suturing Method. Craniomaxillofacial Trauma & Reconstruction, 16(3), 205-210. https://doi.org/10.1177/19433875221092571




