Quantifying Aerosol Generation in Maxillofacial Trauma Repair Techniques
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Operative Techniques
2.3. Data Collection
2.4. Statistical Analyses
3. Results
3.1. Distance from Source
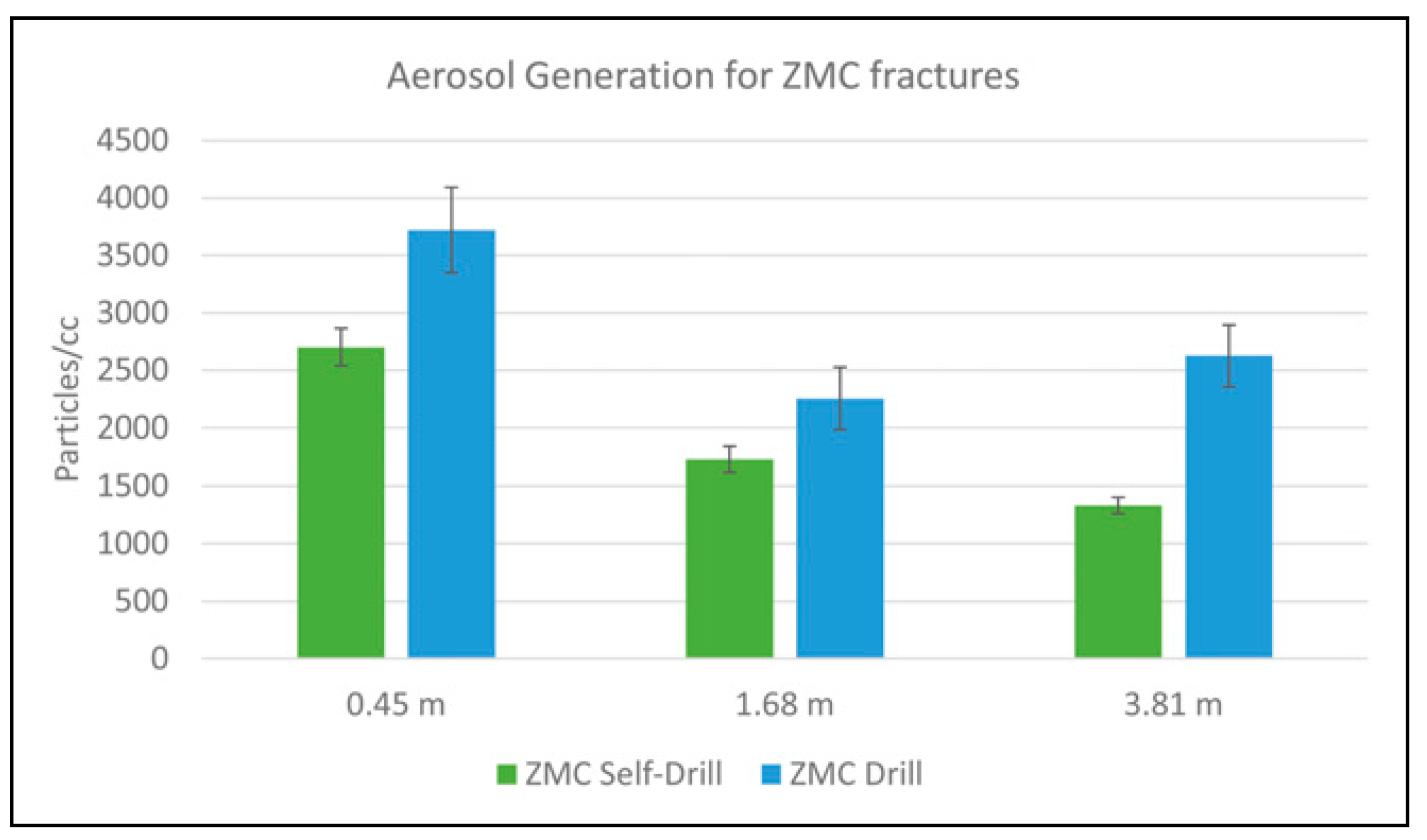
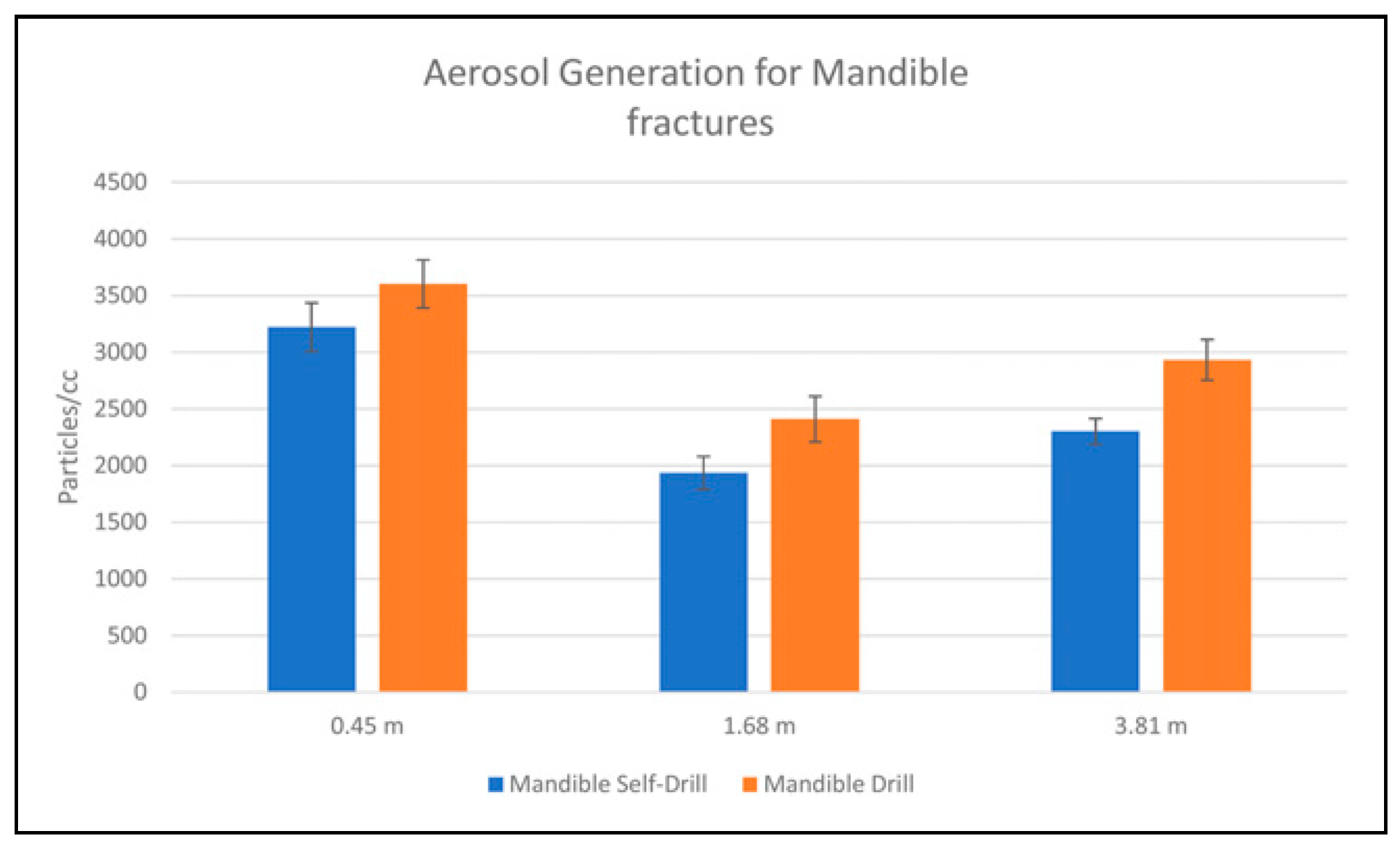
3.2. Self-Drilling vs. Power Drilling
4. Discussion
5. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Oran, D.P.; Topol, E.J. Prevalence of asymptomatic SARS-CoV2 infection. Ann. Intern. Med. 2020, 173, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Ochoa, S.A.; Franco, O.H.; Rojas, L.Z.; Raguindin, P.F.; Roa-Díaz, Z.M.; Wyssmann, B.M.; Guevara, S.L.R.; Echeverría, L.E.; Glisic, M.; Muka, T. COVID-19 in health-care workers: A living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am. J. Epidemiol. 2021, 190, 161–175. [Google Scholar] [CrossRef]
- Burrer, S.L.; de Perio, M.A.; Hughes, M.M.; Kuhar, D.T.; Luckhaupt, S.E.; McDaniel, C.J.; Porter, R.M.; Silk, B.; Stuckey, M.J.; Walters, M. Characteristics of health care personnel with COVID-19—United States, February 12-April 9, 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 477–481. [Google Scholar] [CrossRef]
- Olliaro, P.; Torreele, E.; Vaillant, M. COVID-19 vaccine efficacy and effectiveness-the elephant (not) in the room. Lancet Microbe 2021, 2, e279–e280. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, E.; Ritchie, H.; Ortiz-Ospina, E.; Roser, M.; Hasell, J.; Appel, C.; Giattino, C.; Rodés-Guirao, L. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 2021, 5, 947–953. [Google Scholar] [CrossRef]
- Ysrafil, Y.; Mus, R.; Gama, N.I.; Rahmaisyah, D.; Nur’amalia, R. Emerging mutation in SARS-CoV-2 spike: Widening distribution over time in different geographic areas. Biomed. J. 2021, S2319-4170(21)00090-1, Online ahead of print. [Google Scholar] [CrossRef]
- Zeyaullah, M.; AlShahrani, A.M.; Muzammil, K.; Ahmad, I.; Alam, S.; Khan, W.H.; Ahmad, R. COVID19 and SARS-CoV-2 variants: Current challenges and health concern. Front. Genet. 2021, 12. [Google Scholar] [CrossRef]
- Pan, Y.; Zhang, D.; Yang, P.; Poon, L.L.M.; Wang, Q. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect. Dis. 2020, 20, 411–412. [Google Scholar] [CrossRef]
- Zou, L.; Ruan, F.; Huang, M.; Liang, L.; Huang, H.; Hong, Z.; Yu, J.; Kang, M.; Song, Y.; Xia, J.; et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N. Engl. J. Med. 2020, 382, 1177–1179. [Google Scholar] [CrossRef]
- Buonanno, G.; Stabile, L.; Morawska, L. Estimation of airborne viral emission: Quanta emission rate of SARS-CoV-2 for infection risk assessment. Environ. Int. 2020, 141, 105794. [Google Scholar] [CrossRef]
- CDC. Scientific Brief: SARS-CoV-2 Transmission. In CDC; 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html (accessed on 27 June 2021).
- Tang, S.; Mao, Y.; Jones, R.M.; Tan, Q.; Ji, J.S.; Li, N.; Shen, J.; Lv, Y.; Pan, L.; Ding, P.; et al. Aerosol transmission of SARS-CoV-2? Evidence, prevention and control. Environ. Int. 2020, 144, 106039. [Google Scholar] [CrossRef] [PubMed]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, T.Y.; Dedhia, R.D.; Chiao, W.; Dresner, H.; Barta, R.J.; Lyford-Pike, S.; Hamlar, D.; Stephan, S.J.; Schubert, W.; Hilger, P.A. A guide to facial trauma triage and precautions in the COVID-19 pandemic. Facial Plast. Surg. Aesthet. Med. 2020, 22, 164–169. [Google Scholar] [CrossRef]
- Ye, M.J.; Sharma, D.; Campiti, V.J.; Rubel, K.E.; Burgin, S.J.; Illing, E.A.; Ting, J.Y.; Park, J.H.; Johnson, J.D.; Vernon, D.J.; et al. Aerosol and droplet generation from mandible and midface fixation: Surgical risk in the pandemic era. Am. J. Otolaryngol. 2021, 42, 102829. [Google Scholar] [CrossRef]
- Gadkaree, S.K.; Derakhshan, A.; Workman, A.D.; Feng, A.L.; Quesnel, A.M.; Shaye, D.A. Quantifying aerosolization of facial plastic surgery procedures in the COVID-19 era: Safety and particle generation in craniomaxillofacial trauma and rhinoplasty. Facial Plast. Surg. Aesthet. Med. 2020, 22, 321–326. [Google Scholar] [CrossRef]
- Grant, J.; Shafi, A.; Halsnad, M. Aerosol prevention in osteosynthesis for maxillofacial trauma—A technical note. Br. J. Oral. Maxillofac. Surg. 2020, 58, 721–722. [Google Scholar] [CrossRef] [PubMed]
- Ghai, S. Facial trauma management during the COVID-19 era: A primer for surgeons. Curr. Med. Res. Pract. 2020, 10, 169. [Google Scholar] [CrossRef]
- Shokri, T.; Saadi, R.A.; Liaw, J.; Bann, D.V.; Patel, V.A.; Goyal, N.; Lighthall, J.G. Facial Plastic and Reconstructive Surgery During the COVID-19 Pandemic. Ann. Plast. Surg. 2020, 85 (2S), S166–S170. [Google Scholar] [CrossRef]
- Edwards, S.P.; Kasten, S.; Nelson, C.; Elner, V.; McKean, E. Maxillofacial trauma management during COVID-19: Multidisciplinary recommendations. Facial Plast. Surg. Aesthet. Med. 2020, 22, 157–159. [Google Scholar] [CrossRef]
- Leung, N.H.L. Transmissibility and transmission of respiratory viruses. Nat. Rev. Microbiol. 2021, 19, 528–545. [Google Scholar] [CrossRef]
- Gilardino, M.S.; Chen, E.; Bartlett, S.P. Choice of internal rigid fixation materials in the treatment of facial fractures. Craniomaxillofacial Trauma. Reconstr. 2009, 2, 49–60. [Google Scholar] [CrossRef] [PubMed]
- Grant, M.; Buchbinder, D.; Dodson, T.B.; Fusetti, S.; Leung, M.Y.Y.; Aniceto, G.S.; Schramm, A.; Strong, E.B.; Wolvius, E. AO CMF international task force recommendations on best practices for maxillofacial procedures during COVID-19 pandemic executive summary. Craniomaxillofacial Trauma. Reconstr. 2020. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
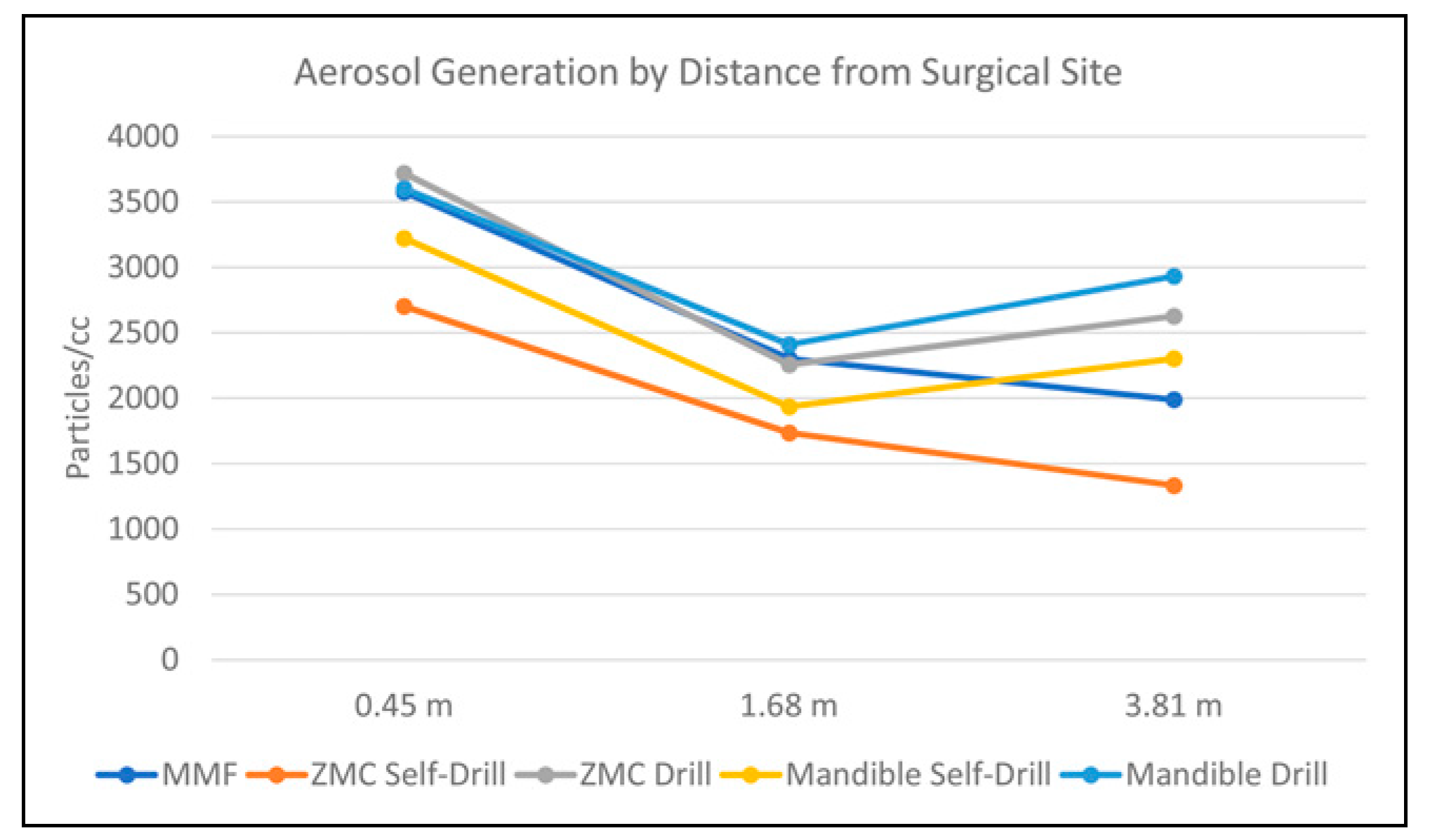
| Procedure | Distance (meters) | Mean Aerosol Count (Particles/cc) | Standard Deviation (Particles/cc) | p Value |
|---|---|---|---|---|
| MMF | 0.45 | 3575.075 | 202.065 | <0.001 |
| 1.68 | 2302.5 | 176.27 | ||
| 3.81 | 1990.455 | 215.963 | ||
| ORIF ZMC drill | 0.45 | 3719.952 | 371.931 | <0.001 |
| 1.68 | 2255.86 | 272.841 | ||
| 3.81 | 2626.2 | 268.311 | 1.000 | |
| ORIF ZMC hand-screw | 0.45 | 2702.548 | 162.882 | <0.001 |
| 1.68 | 1734.274 | 114.848 | ||
| 3.81 | 1332.867 | 71.763 | ||
| ORIF mandible drill | 0.45 | 3604.142 | 210.801 | <0.001 |
| 1.68 | 2410.542 | 201.522 | ||
| 3.81 | 2932.417 | 179.453 | 1.000 | |
| ORIF mandible hand-screw | 0.45 | 3221.617 | 214.076 | <0.001 |
| 1.68 | 1935.522 | 145.839 | ||
| 3.81 | 2301.813 | 113.796 | 1.000 |
| Procedure | Distance (meters) | Mean Aerosol Count (Particles/cc) | Standard Deviation (Particles/cc) | p Value |
|---|---|---|---|---|
| Mandible hand-screw | 0.45 | 3221.617 | 214.076 | <0.01 |
| Mandible drill | 3604.142 | 210.801 | ||
| Mandible hand-screw | 1.68 | 1935.522 | 145.839 | <0.01 |
| Mandible drill | 2410.542 | 201.522 | ||
| Mandible hand-screw | 3.81 | 2301.813 | 113.796 | <0.01 |
| Mandible drill | 2932.417 | 179.453 | ||
| ZMC hand-screw | 0.45 | 2702.548 | 162.882 | <0.01 |
| ZMC drill | 3719.952 | 371.931 | ||
| ZMC hand-screw | 1.68 | 1734.274 | 114.848 | <0.01 |
| ZMC drill | 2255.86 | 272.841 | ||
| ZMC hand-screw | 3.81 | 1332.867 | 71.763 | <0.01 |
| ZMC drill | 2626.2 | 268.311 |
© 2021 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McCann, A.; Singerman, K.; Coxe, J.; Singletary, J.; Wang, J.; Collar, R.; Hsieh, T.-y. Quantifying Aerosol Generation in Maxillofacial Trauma Repair Techniques. Craniomaxillofac. Trauma Reconstr. 2022, 15, 362-368. https://doi.org/10.1177/19433875211059314
McCann A, Singerman K, Coxe J, Singletary J, Wang J, Collar R, Hsieh T-y. Quantifying Aerosol Generation in Maxillofacial Trauma Repair Techniques. Craniomaxillofacial Trauma & Reconstruction. 2022; 15(4):362-368. https://doi.org/10.1177/19433875211059314
Chicago/Turabian StyleMcCann, Adam, Kyle Singerman, James Coxe, John Singletary, Jun Wang, Ryan Collar, and Tsung-yen Hsieh. 2022. "Quantifying Aerosol Generation in Maxillofacial Trauma Repair Techniques" Craniomaxillofacial Trauma & Reconstruction 15, no. 4: 362-368. https://doi.org/10.1177/19433875211059314
APA StyleMcCann, A., Singerman, K., Coxe, J., Singletary, J., Wang, J., Collar, R., & Hsieh, T.-y. (2022). Quantifying Aerosol Generation in Maxillofacial Trauma Repair Techniques. Craniomaxillofacial Trauma & Reconstruction, 15(4), 362-368. https://doi.org/10.1177/19433875211059314




