A Prospective Study on Autotransplantation of Mandibular Third Molars With Complete Root Formation
Abstract
:Introduction
Material & Method
Inclusion Criteria
- Patients with ASA grade I and II (American Society of Anesthesiologists), between the age group of 21-66 years having fully developed mandibular third molars were selected.
- The transplant should have a suitable shape and dimension for the recipient site.
Exclusion Criteria
- Divergent root morphology of the transplant tooth than the recipient site.
- Patients having bad periodontal health.
- Medically compromised patients.
- Pregnant women.
- Third molars which require sectioning for their removal.
- Periapical or Periodontal pathology with respect to donor or recipient site.
Method
- Detailed case history of all cases which requires extraction of first or second molar were recorded. All patients underwent clinical examination, routine blood investigation, and Intaoral Periapical Radiograph (IOPA), OPG if required.
- The transplant was chosen with reference to the best morphological conformity possible. Thus, the third molar of the same quadrant of the jaw was the first choice.
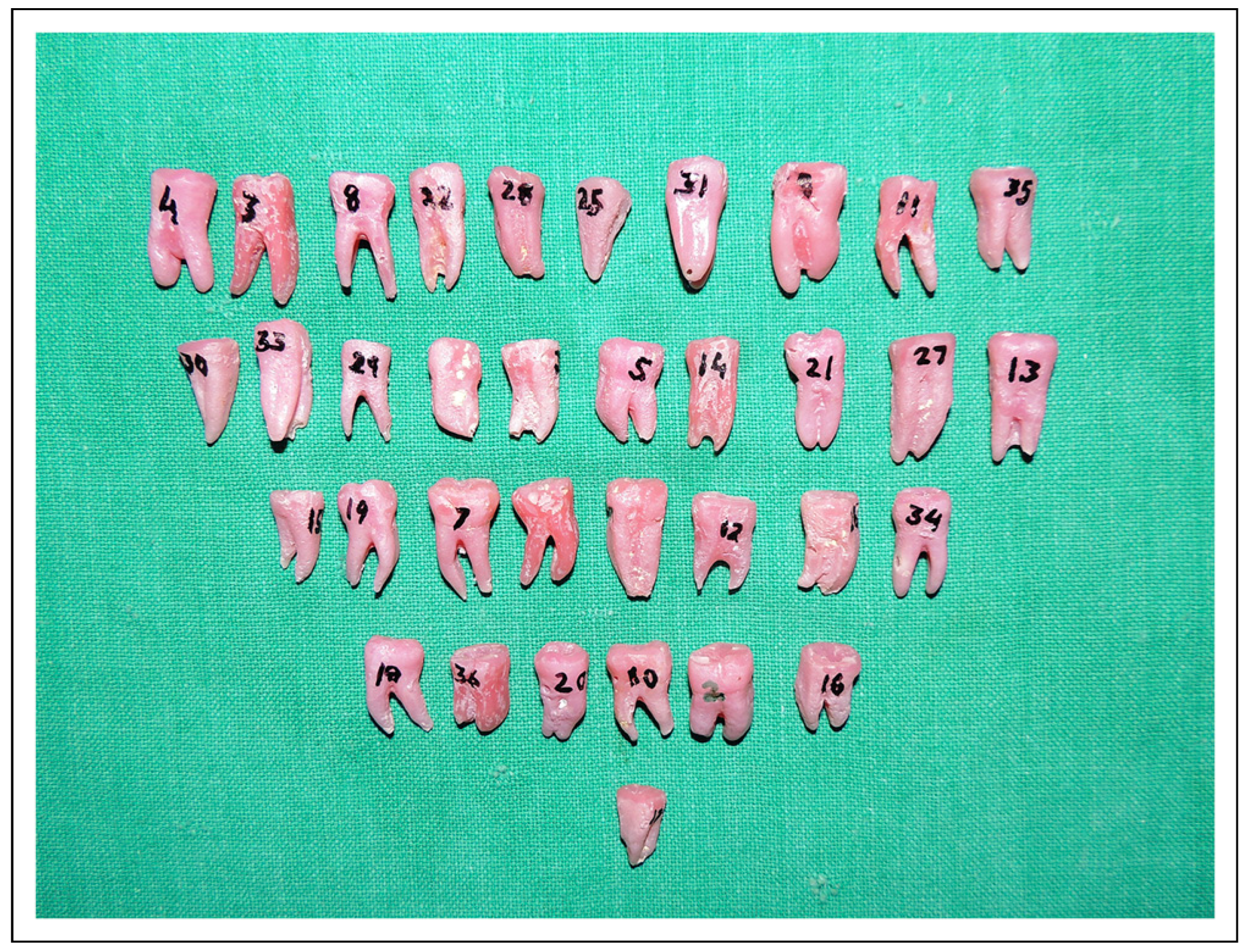
- On the basis of radiographical examination, the best suitable replica of third molar to be autotransplanted was chosen from the collection of suitable acrylic replicas (Figure 1).
- Every surgery was performed after obtaining local anesthesia.
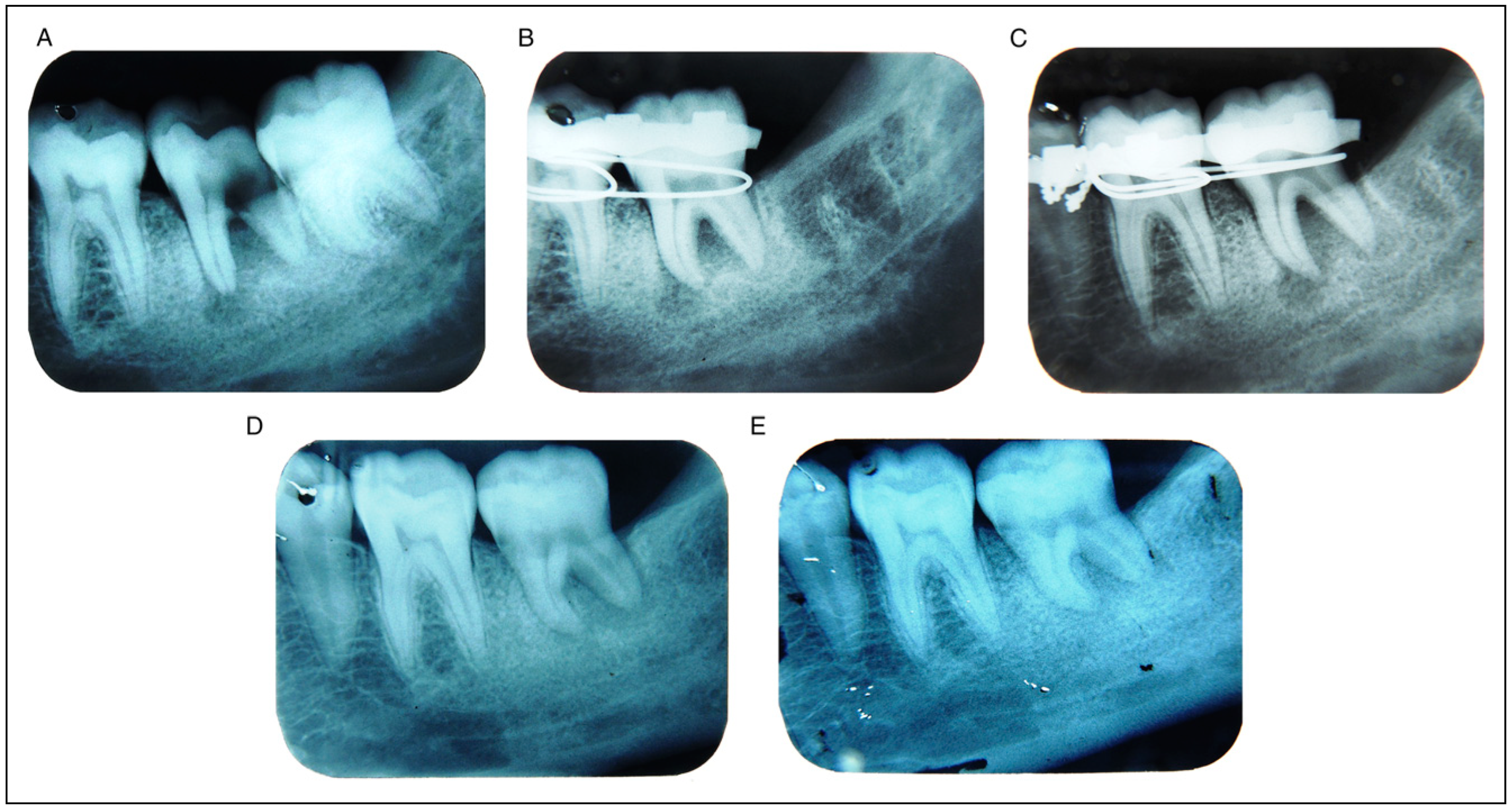
- First/second molar extraction was performed in an atraumatic manner, preserving sufficient buccal and lingual cortical plate heights (Figure 2).
- The recipient site was prepared first with the help of bone-cutting burs, chisel, rongeur, filer (Figure 3), and according to the best morphologically similar and chosen replica. The replica was gently tapped into the socket to ensure that the replica appropriately fit the recipient site (Figure 4).
- Mandibular third molar was extracted atraumatically, taking care to avoid damage to periodontal ligament in order to preserve its vitality which is essential for successful outcome of treatment (Figure 5). Simultaneously, precaution was taken not to injure the root surface, and the molar was transplanted into the prepared site with minimum possible lapse of time and less number of attempts to achieve satisfactory fit (Figure 6).
- The transplant was placed preferably with slight approximate contacts to the adjacent teeth, without interference with the opposing teeth.
- Care was taken to avoid occlusal contact from the opposing tooth.
- The transplanted tooth was appropriately splinted with adjacent teeth, and it was left for minimum of 4 weeks (Figure 7).
- Postoperative instructions and medication (5 to 7 days) were given:
- Tab. cefixime 200 mg BD 1 tab./Cap. amoxycilline 500 mg 1 cap TDS.
- Tab. Aceclofenac/Tab. diclofenac 1 tab. TDS.
- Cap. multivitamin 1 cap OD.
- Tab. ranitidine 150 mg 1 tab BD/Tab. pantoprazole-domperidone 1 tab. BD.
- Regular post-extraction instructions were given with special instructions to take semisolid/soft diet for 3 to 4 weeks and avoid pressure on the operated site. Sutures were removed after 7 days.
- Regular clinical and radiographical examinations were performed on prescribed time for follow-up.
- Medical/psychosocial support was provided, if needed, to all the patients during the surgery and in the whole course of assessment.
Criteria Parameter
Data Analysis
Results
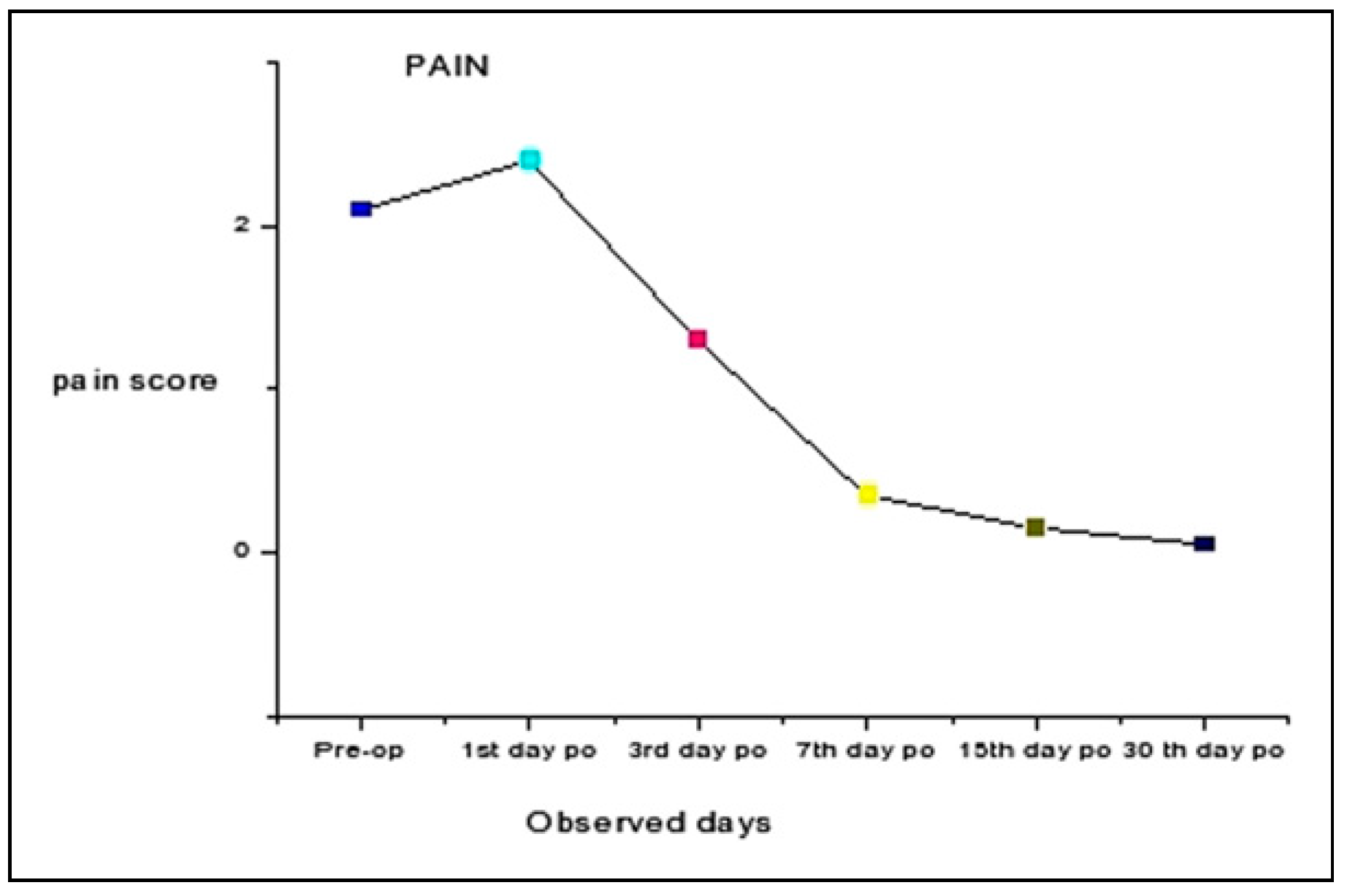
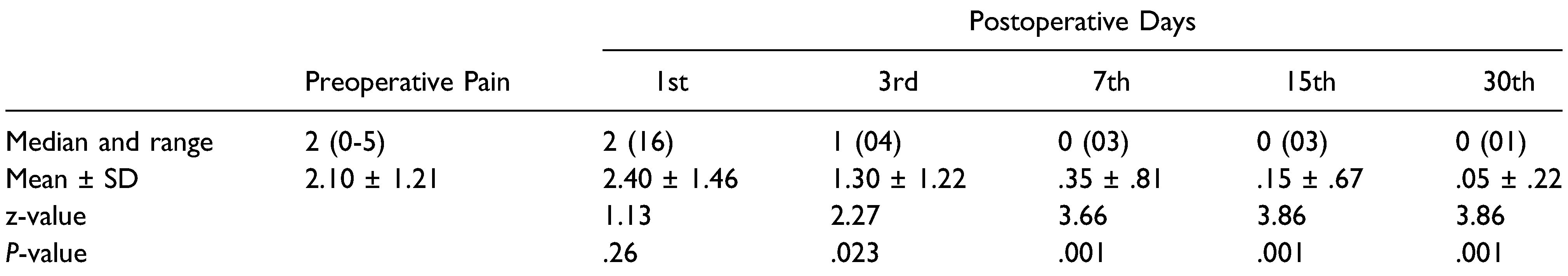
Pain [8]
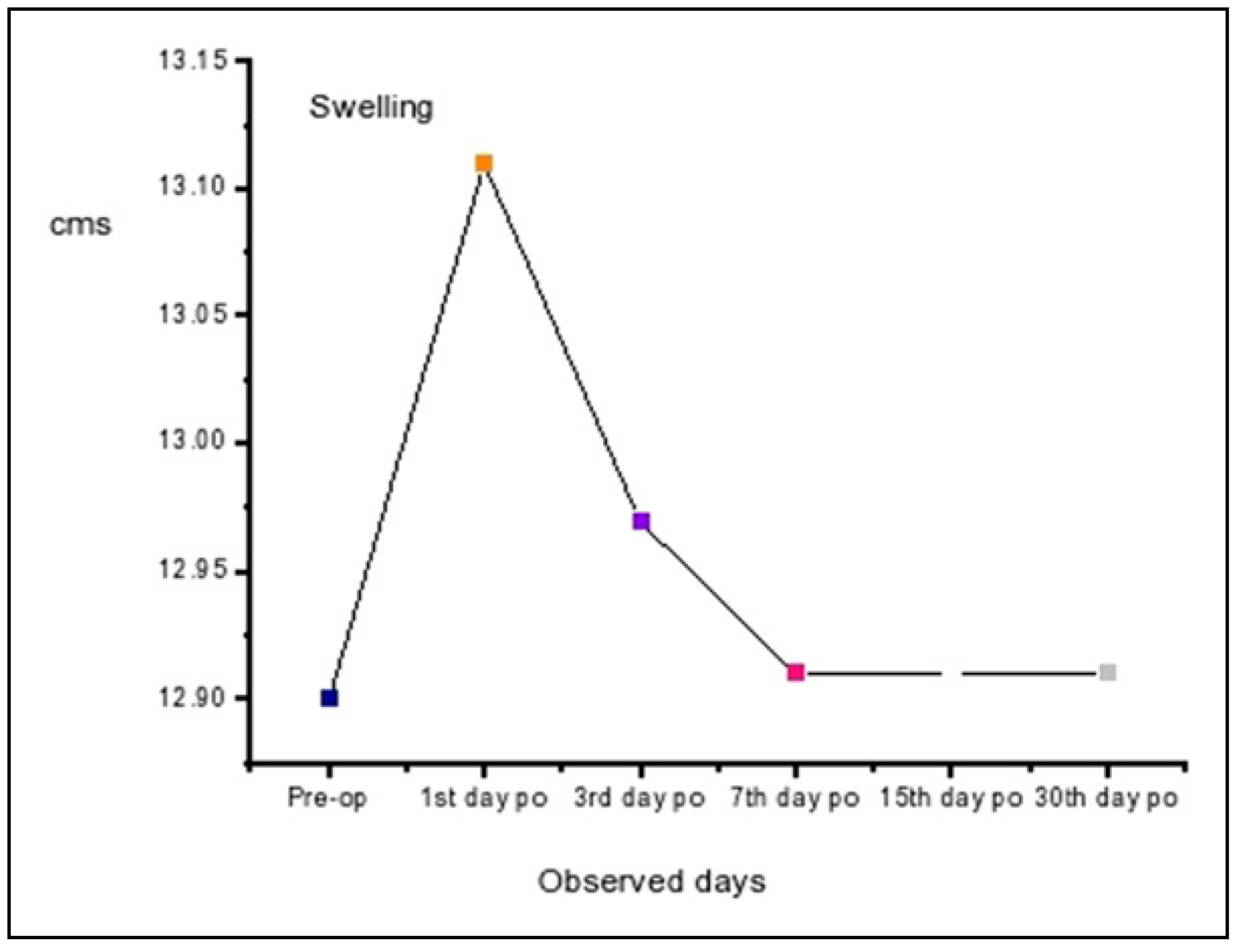
Swelling [9] (Extraoral)
Postoperative Infection
Dry Socket
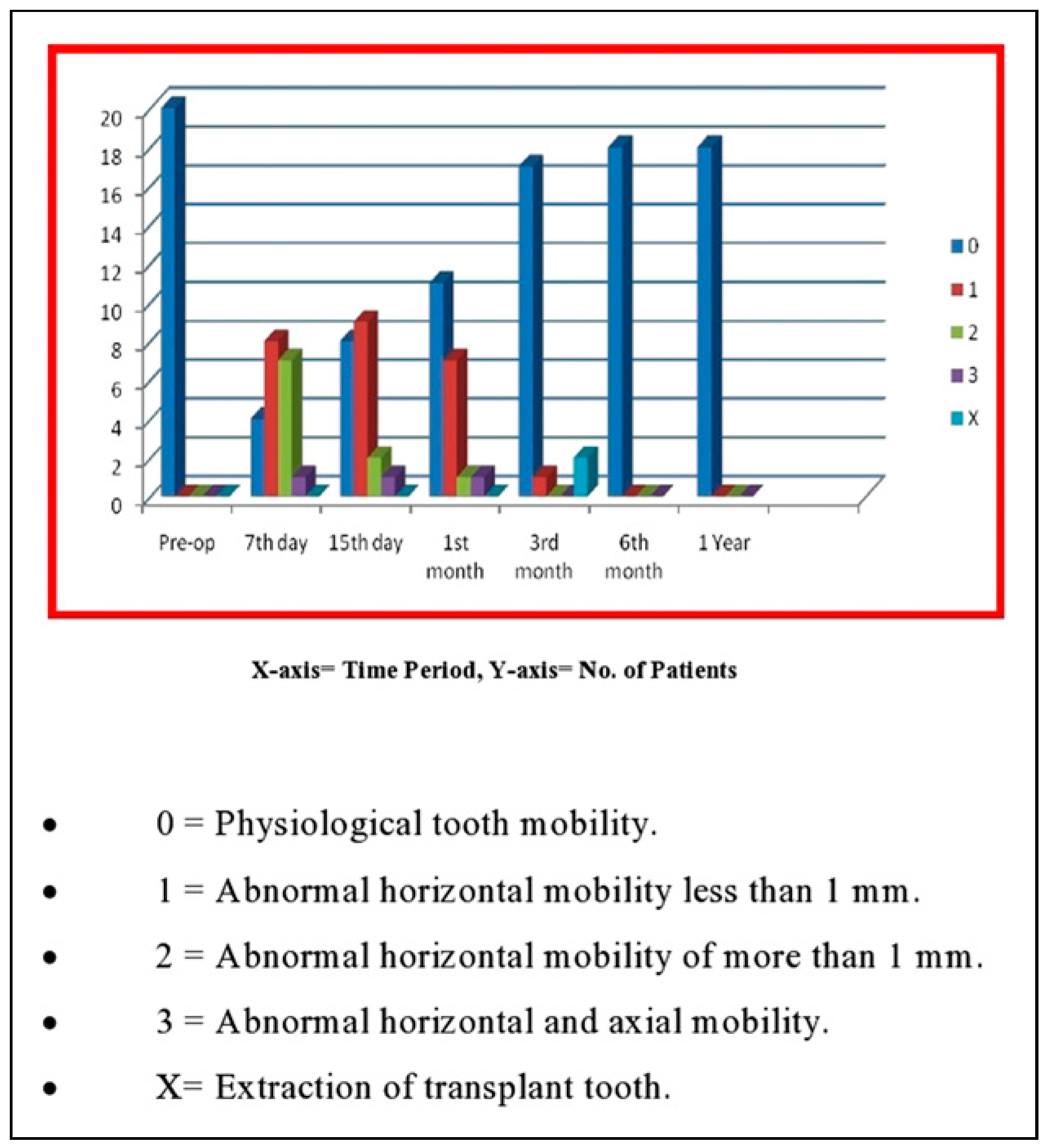
Transplant Mobility [10]
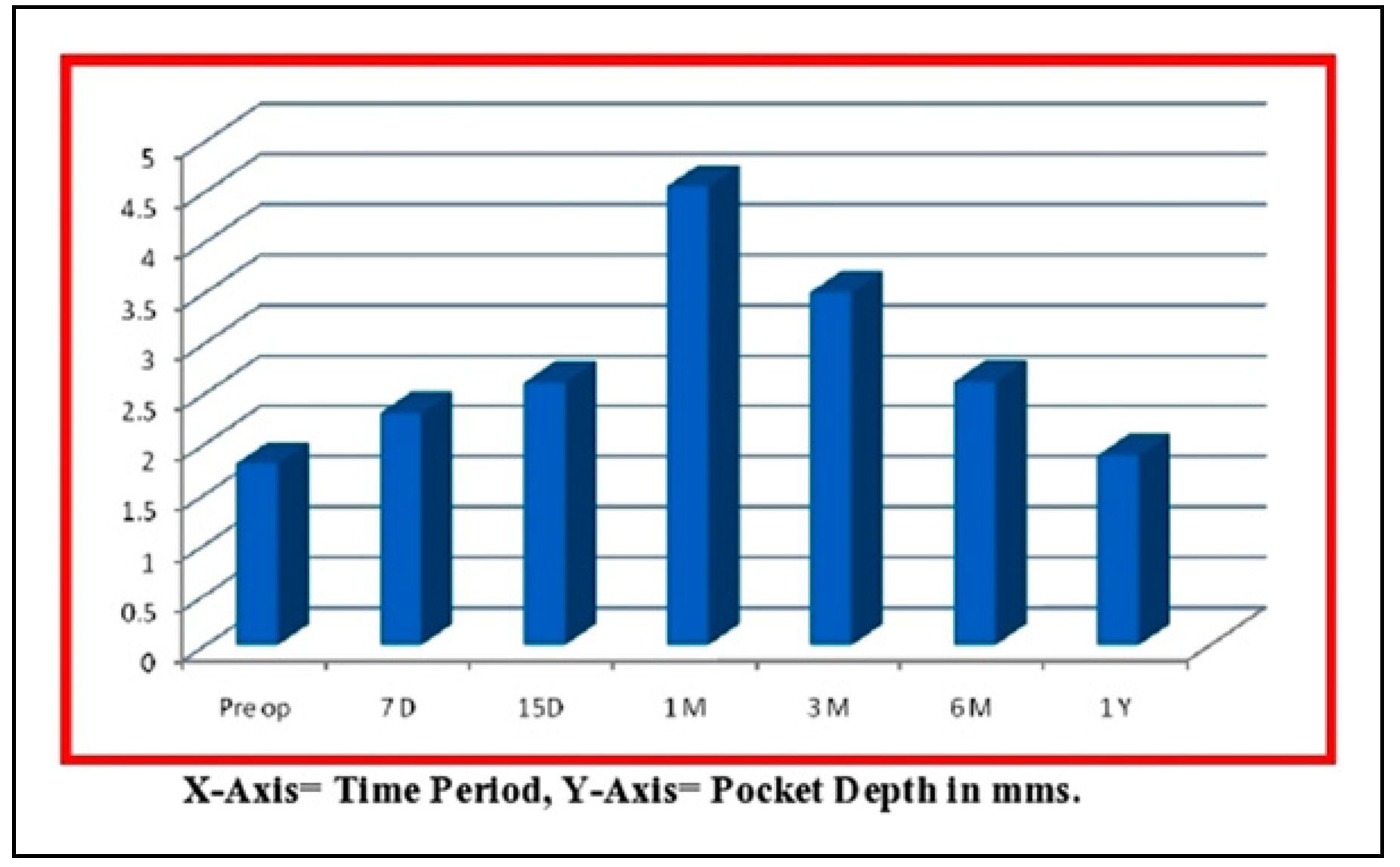
Pocket Depth [10](In Millimeters)
Radiographic Assessment
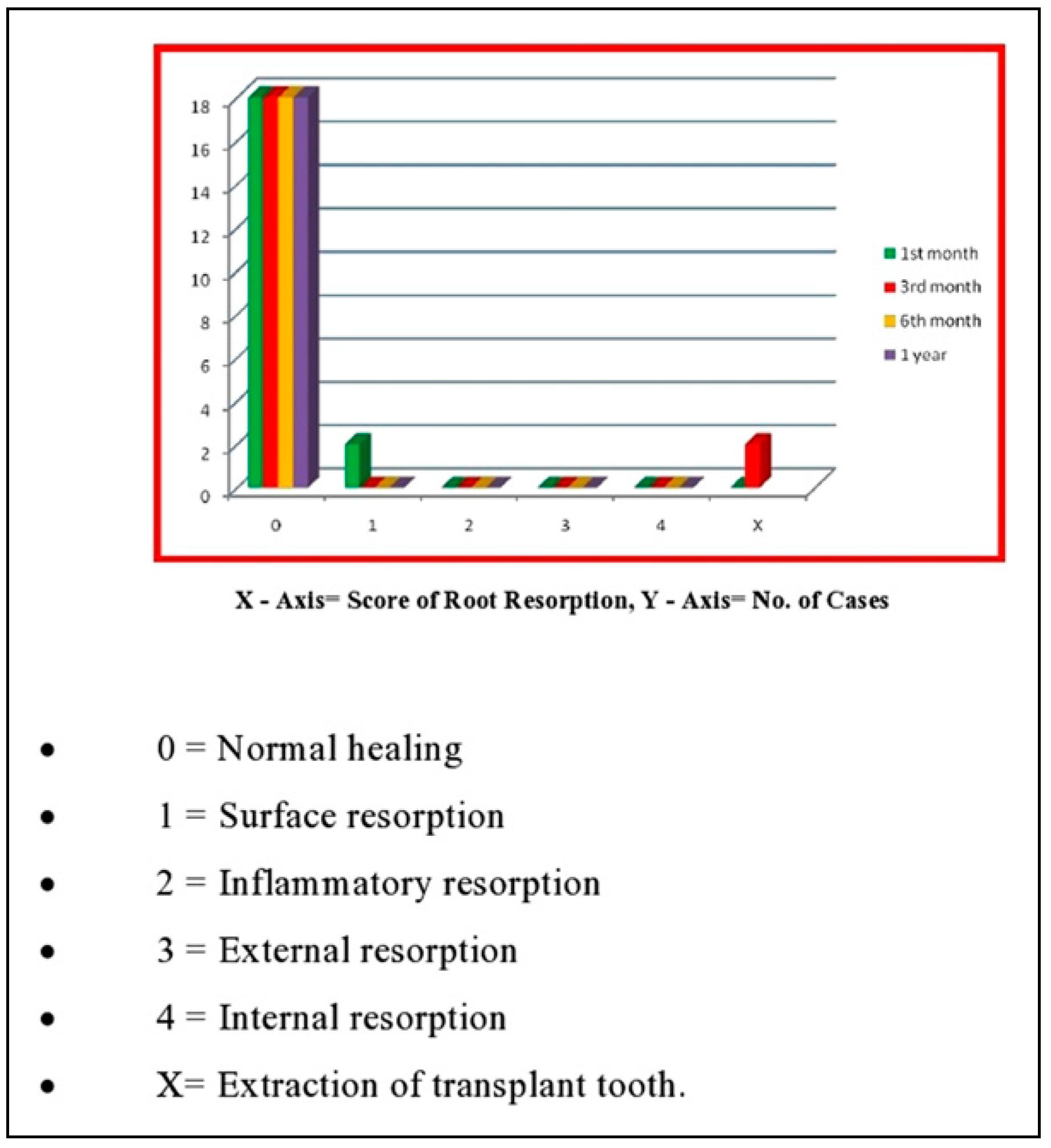
Root Resorption [11,12]
Buccal Bone [11,12]
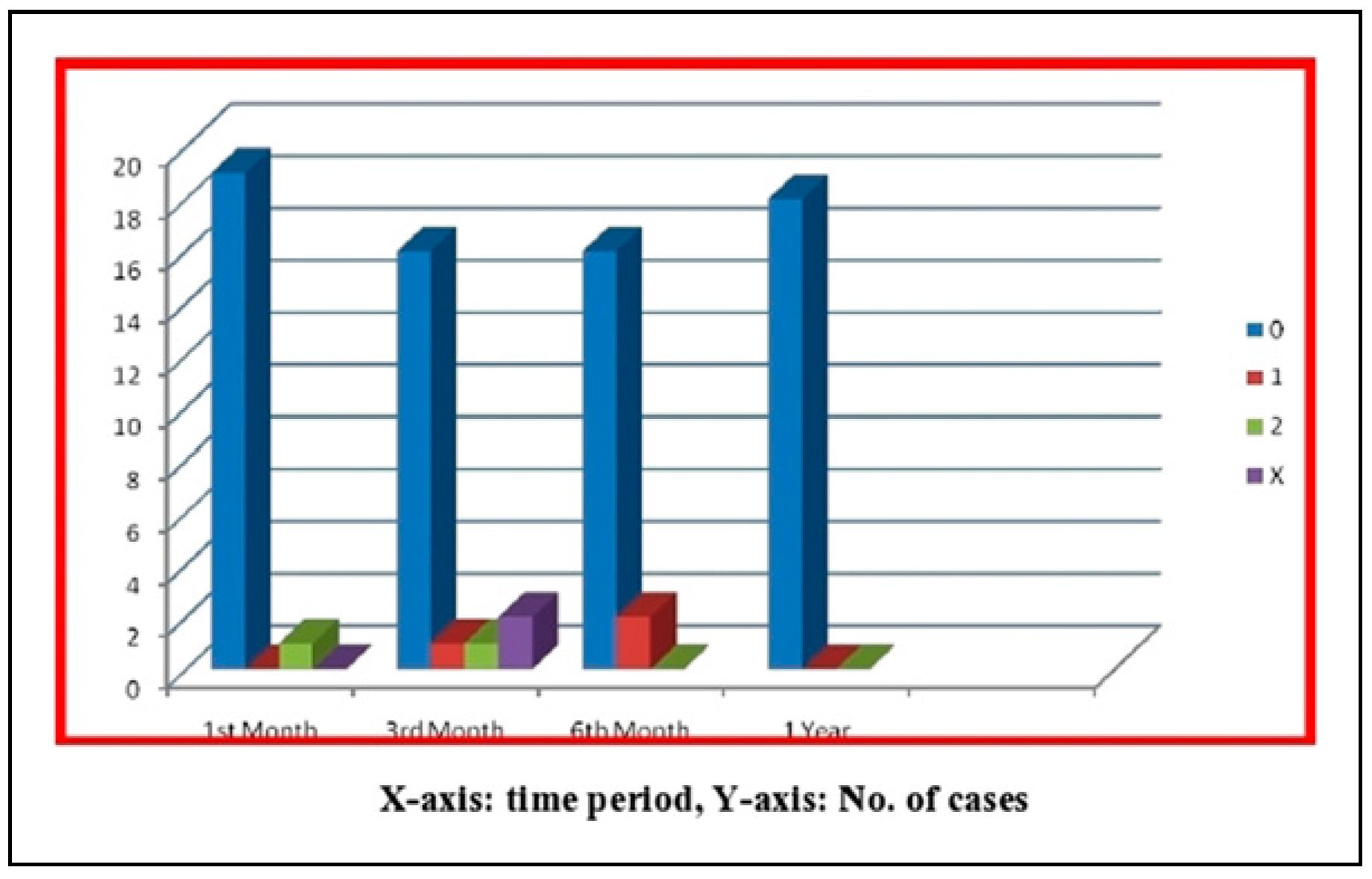
Ankylosis [4,12]
Discussion
- The tooth should be fixed in its socket without residual inflammation.
- Masticatory function should be satisfactory and without discomfort.
- The tooth should not be mobile.
- Any pathologic condition should not be apparent on the radiograph, and
- The depth of the sulcus, gingival contour, and gingival color should be normal.
Conclusion
Supplementary Materials
Funding
Conflicts of Interest
References
- Reich, P.P. Autogenous transplantation of maxillary and mandibular molars. J Oral Maxillofac Surg. 2008, 66, 2314–2317. [Google Scholar] [CrossRef] [PubMed]
- Galanter, D.R.; Minami, R.T. The periodontal status of autografted teeth: A pilot study of thirty-one cases. Oral Surg Oral Med Oral Pathol. 1968, 26, 145–159. [Google Scholar] [CrossRef] [PubMed]
- Tsukiboshi, M. Autotransplantation of teeth: Requirements for predictable success. Dent Traumatol. 2002, 18, 157–180. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Jung, J.Y.; Cha, I.H.; Kum, K.Y.; Lee, S.J. Evaluation of the prognosis and causes of failure in 182 cases of autogenous tooth transplantation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005, 100, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Yoshino, K.; Kariya, N.; Namura, D.; et al. Risk factors affecting third molar autotransplantation in males: a retrospective survey in dental clinics. J Oral Rehabil. 2012, 39, 821–829. [Google Scholar] [CrossRef] [PubMed]
- Meja`re, B.; Wannfors, K.; Jansson, L. A prospective study on transplantation of third molars with complete root formation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004, 97, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Waikakul, A.; Punwutikorn, J.; Kasetsuwan, J.; Korsuwannawong, S. Alveolar bone changes in autogenous tooth transplantation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011, 111, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Myles, P.S.; Troedel, S.; Boquest, M.; Reeves, M. The pain visual analog scale: Is it linear or nonlinear? Anesth Analg. 1999, 89, 1517–1520. [Google Scholar] [CrossRef] [PubMed]
- Pöllmann, L. Long term followup of postoperative swelling. Int J Oral Maxillofac Surg. 1983, 12, 90–94. [Google Scholar]
- Bauss, O.; Schilke, R.; Fenske, C.; Engelke, W.; Kiliardis, S. Autotransplantation of immature third molars: Influence of different splinting methods and fixation periods. Dent Traumatol. 2002, 18, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Waikakul, A.; Kasetsuwan, J.; Punwutikorn, J. Response of autotransplanted teeth to electric pulp testing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002, 94, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Nethander, G. Oral restoration with fixed partial dentures on transplanted abutment teeth. Int J Prosthodont. 1995, 8, 517–526. [Google Scholar] [PubMed]
- Honda, M.; Uehara, H.; Uehara, T.; et al. Use of replica graft tooth for evaluation before autotransplantation of a tooth. A CAD/ CAM model produced using dental-cone-beam computed tomography. Int J Oral Maxillofac Surg. 2010, 39, 1016–1019. [Google Scholar] [CrossRef] [PubMed]
- Lundberg, T.; Isaksson, S. A clinical follow-up study of 278 autotransplanted teeth. Br J Oral Maxillofac Surg. 1996, 34, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Akkocaoglu, M.; Kasaboglu, O. Success rate of autotransplanted teeth without stabilisation by splints: A long term clinical and radiological follow-up. Br J Oral Maxillofac Surg. 2005, 43, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Czochrowska, E.M.; Stenvik, A.; Bjercke, B.; Zachrisson, B.U. Outcome of tooth transplantation: Survival and success rates 17-41 years post-treatment. Am J Orthod Dentofacial Orthop. 2002, 121, 110–119. [Google Scholar] [CrossRef] [PubMed]
- Gonnisen, H.; et al. Success of autogenous transplantation: A retrospective and prospective approach. IFMBE. 2009, 25, 17–20. [Google Scholar]
- Czochrowska, E.M.; Stenvik, A.; Album, B.; Zachrisson, B.U. Autotransplantation of premolars to replace maxillary incisors: A comparison with natural incisors. Am J Orthod Dentofacial Orthop. 2000, 118, 592–600. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, S.; Yoshizawa, M.; Niimi, K.; Sugai, T.; Kitamura, N.; Saito, C. Prognostic factors for autotransplantation of teeth with complete root formation. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012, 114, S216–S228. [Google Scholar] [CrossRef] [PubMed]






 |
© 2022 by the author. The Author(s) 2022.
Share and Cite
Dhar, S.; Singh, G.; Mishra, M.; Gaur, A. A Prospective Study on Autotransplantation of Mandibular Third Molars With Complete Root Formation. Craniomaxillofac. Trauma Reconstr. 2022, 15, 340-349. https://doi.org/10.1177/19433875211055600
Dhar S, Singh G, Mishra M, Gaur A. A Prospective Study on Autotransplantation of Mandibular Third Molars With Complete Root Formation. Craniomaxillofacial Trauma & Reconstruction. 2022; 15(4):340-349. https://doi.org/10.1177/19433875211055600
Chicago/Turabian StyleDhar, Shishir, Gaurav Singh, Madan Mishra, and Amit Gaur. 2022. "A Prospective Study on Autotransplantation of Mandibular Third Molars With Complete Root Formation" Craniomaxillofacial Trauma & Reconstruction 15, no. 4: 340-349. https://doi.org/10.1177/19433875211055600
APA StyleDhar, S., Singh, G., Mishra, M., & Gaur, A. (2022). A Prospective Study on Autotransplantation of Mandibular Third Molars With Complete Root Formation. Craniomaxillofacial Trauma & Reconstruction, 15(4), 340-349. https://doi.org/10.1177/19433875211055600




