Introduction
Injury scoring systems like Injury Severity Score (ISS) and New Injury Severity Score (NISS) are commonly used to predict the outcome of general trauma associated with mortality, morbidity and outcomes as well as the length of hospital stay and cost of treatment.[
1] Several maxillofacial trauma scores have been proposed for scoring maxillofacial trauma and some of them have shown a strong association with length of hospital stay and cost of treatment.[
1] Although multiple maxillofacial trauma scores have been developed, proposed and used over the years, they are limited by either their complexity or incompleteness, require paperwork and physical recording and need further steps to integrate them with the electronic health record systems. ZS maxillofacial trauma score is a recent scoring system that incorporates the strength of previous scoring systems and improves on them to make it one of the most complete systems of scoring maxillofacial trauma.[
2] This app was based on the work of two authors, Simon Holmes (Consultant Oral and Maxillofacial Surgeon, Barts Health NHS Trust) and Zeeshan Ahmad (Junior Doctor, NHS Greater Glasgow and Clyde) who published their original paper in the British Journal of Oral and Maxillofacial Surgery in September 2012. This system is user friendly, app-based visual system for coding facial trauma and is free to use, at the same time, it can be easily integrated into the electronic health record system for sharing among the different disciplines involved in patient care and be stored indefinitely with less carbon footprint compared to paper-based recording systems. There are very few studies that define the association between a patient’s maxillofacial trauma score with perioperative outcomes like operative time, ICU requirement and hospital stay, which are the indirect indicators of cost of treatment. Prediction of the consumption of medical resources and the length of hospital stay is one of the functions of a trauma scoring system. The final results of such scores can offer better judgement of the condition of the injury, treatment assessment and the prognosis, to determine the treatment planning and therapeutic medical resource consumption.[
3] Ability to predict the hospital stay and ICU requirement based on a simple scoring system can be an essential communication instrument for attending maxillofacial surgeons.
Our research question was to ascertain whether the ZS maxillofacial trauma score could predict the operative time, need for ICU and length of stay in maxillofacial trauma patients. Our specific aims were to find the association between ZS score and operative time, need for ICU and length of stay and if a strong association is evident, then prepare a statistical model for prediction of the outcomes based on the ZS score.
Patients and methods
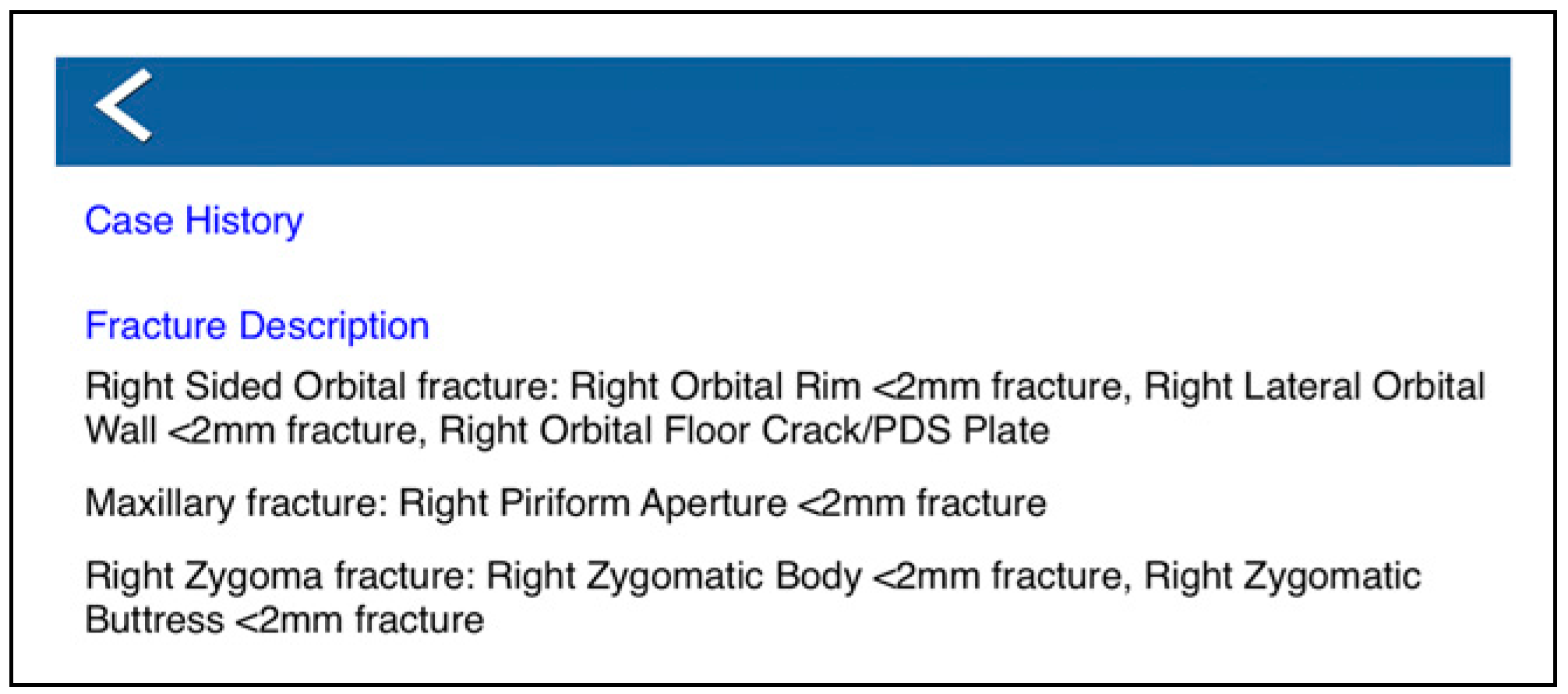
A retrospective chart review of patients was designed and conducted in our unit from October 2018 to October 2019. The study was reviewed and approved by the ethical committee of the institutional review board at the College of Medical Sciences (IRB number: 2020-0063). Inclusion criteria were patients of all age, admitted and operated for isolated maxillofacial bony fractures including all combination of facial fractures, during a period from October 2018 to October 2019, confirmed with a 3D reformatted CT scan (Toshiba 160 Aquilon Prime, Canon Medical systems corporation, Japan) under the Maxillofacial unit and not meeting any of the exclusion criteria. Patients with chronic disease, neurocerebral injuries, orthopaedic or other organ injuries, pregnant patients, patients with isolated dentoalveolar trauma and extensive soft tissue injuries that would require individual management were excluded. Smaller (<1 cm) Soft tissue injuries that did not require a separate repair and would not affect the surgical approach to the fractures were included. Data were retrieved from the electronic medical record system and patients were identified by their hospital identification number. ZS maxillofacial trauma scoring app allows us to select individual bones of the facial skeleton and select a fracture pattern based on what they may find on clinical examination and X-Ray/CT image interpretation. The result is the production of the ZS Score which is a numerical summation of the individual weights assigned to the different fracture patterns selected across the craniofacial skeleton. The final ZS Score can then be used as a means to rapidly calculate trauma severity, triage patients and plan for complex surgical cases. Within the app, users can also annotate their findings by adding a free text note detailing crucial information such as the mechanism of trauma and GCS. This can then be published as a full PDF report through the app and emailed to other clinicians or printed using AirPrint technology. The app also can add free-text notes, automated text summaries of all the fractures selected, production of PDF summary reports displaying the ZS facial skeleton, numerical score values, automated text descriptions and the added ability to email and print summary reports directly within the app.
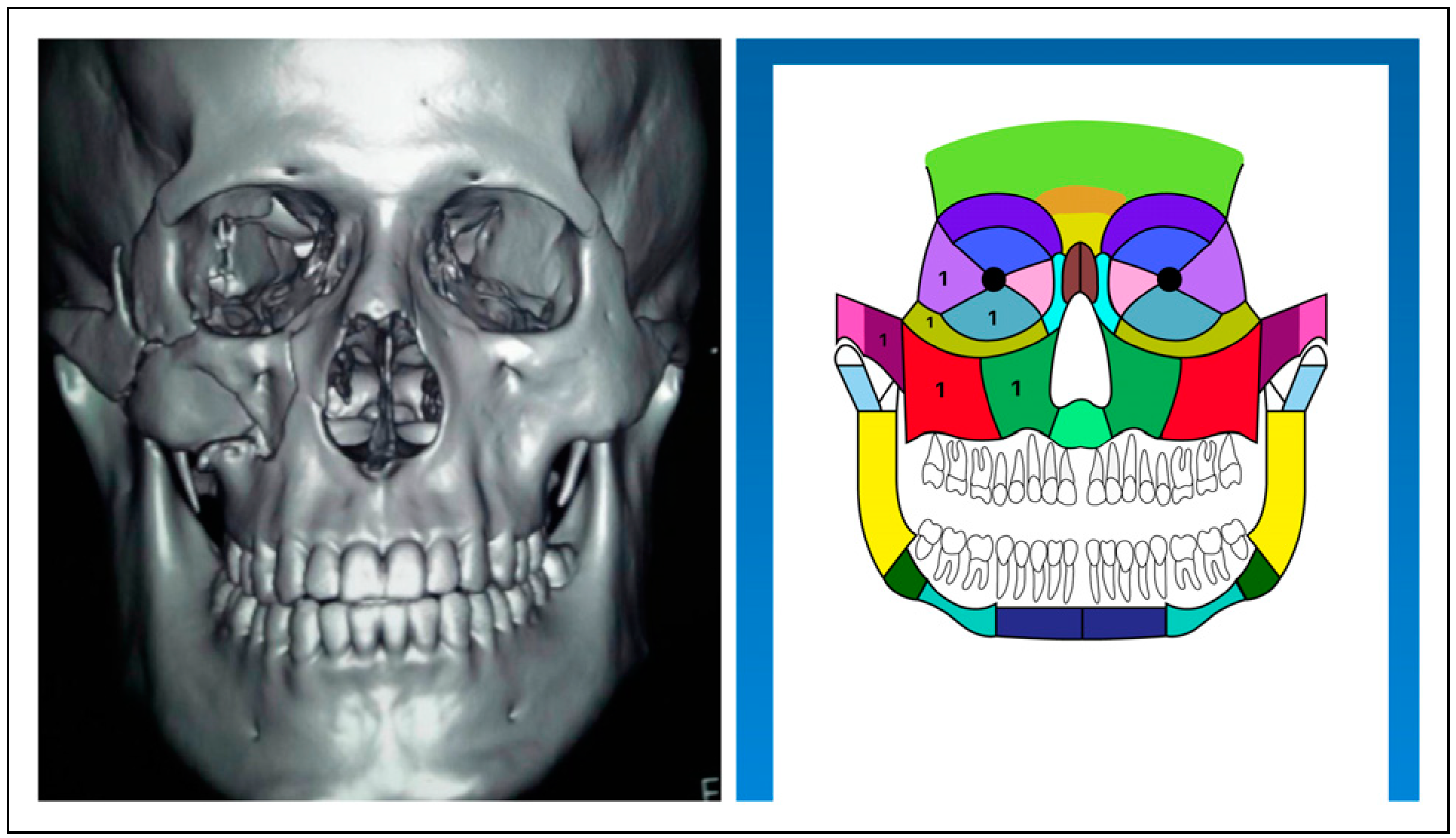
ZS maxillofacial trauma score was calculated manually from the pre-operative 3D reformatted image viewed on Vitrea advanced visualization platform (Vital images, USA) by 1 investigator and scored on ZS maxillofacial scoring system iOS app on an Apple iPad as described by the authors of the ZS maxillofacial trauma score (
Figure 1).[
4] The scoring does not require expertise in maxillofacial trauma as it is colour coded, intuitive and generates a report based on the CT scan for efficient communication and can be shared among users in the unit (
Figure 2). Permission was taken from the developers of the ZS maxillofacial trauma score to use the scoring system as an academic and research tool. Age and gender were considered covariates. All the patients were operated within 24 hours of admission under general anaesthesia and the principal investigator was the primary surgeon involved in all the operations to ensure there was no difference in outcomes because of different surgeons. The exposure, approach and fixation were based strictly on standard international guidelines.[
5] The primary outcome of interest was the operative time which was recorded in minutes. Our secondary outcome was the length of stay, which was recorded as the number of days from the day of admission to the day of discharge and ICU admission which was recorded as a dichotomous outcome. The decision to admit to ICU was based on the airway evaluation performed by the anaesthesiologist. The sample size was calculated based on our primary continuous outcome of interest (operative time), with the literature reported standard deviation of 20 minutes and a margin of error of 5 units. The calculated sample size was 62 at a 95% power of the study. We included a total of 100 samples to reduce confounder bias and increase the power of the study. Non-parametric Correlation analysis was performed for interval variables and crosstabulation for categorical outcomes. Multiple linear regression was performed to analyse the effect of predictors over continuous outcomes of operative time and length of stay. Outlier analysis was performed to check the fitness of outliers in the regression model. Logistic regression was performed for the need for ICU outcome.
Results
There were 95 males and 5 female patients included in the study. The age ranged from 3 to 84 years with a mean of 30.76 (SD = 14.04). The ZS trauma score ranged from 1 to 65 with a mean of 8.86 (SD = 9.65). The average operative time was 74.42 (SD = 82.88) minutes. The average length of stay was 6.45 days (SD = 7.14 days) and ranged from 1 day to 37 days. Out of 100, 27 patients required ICU care.
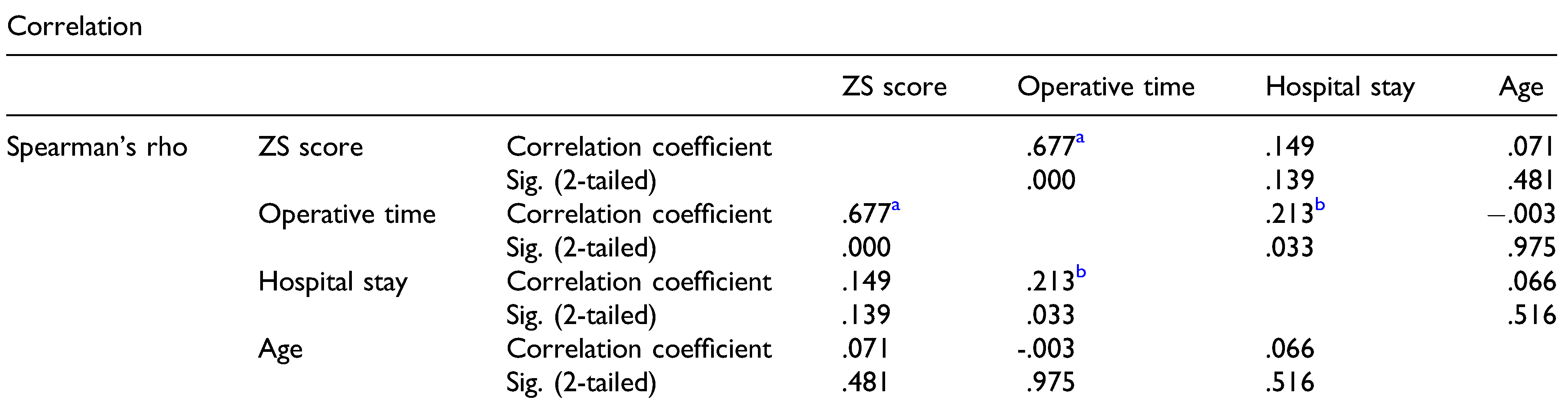
There was a statistically strong and significant association between ZS score and operative time (
r = 0.67,
P < .001). There was no statistically significant association between age and gender with any of the outcomes (
Table 1). Length of hospital stay had no association with any predictors. Interestingly, it showed a statistically significant but weak association with operative time (
r = 0.213,
P = .017).
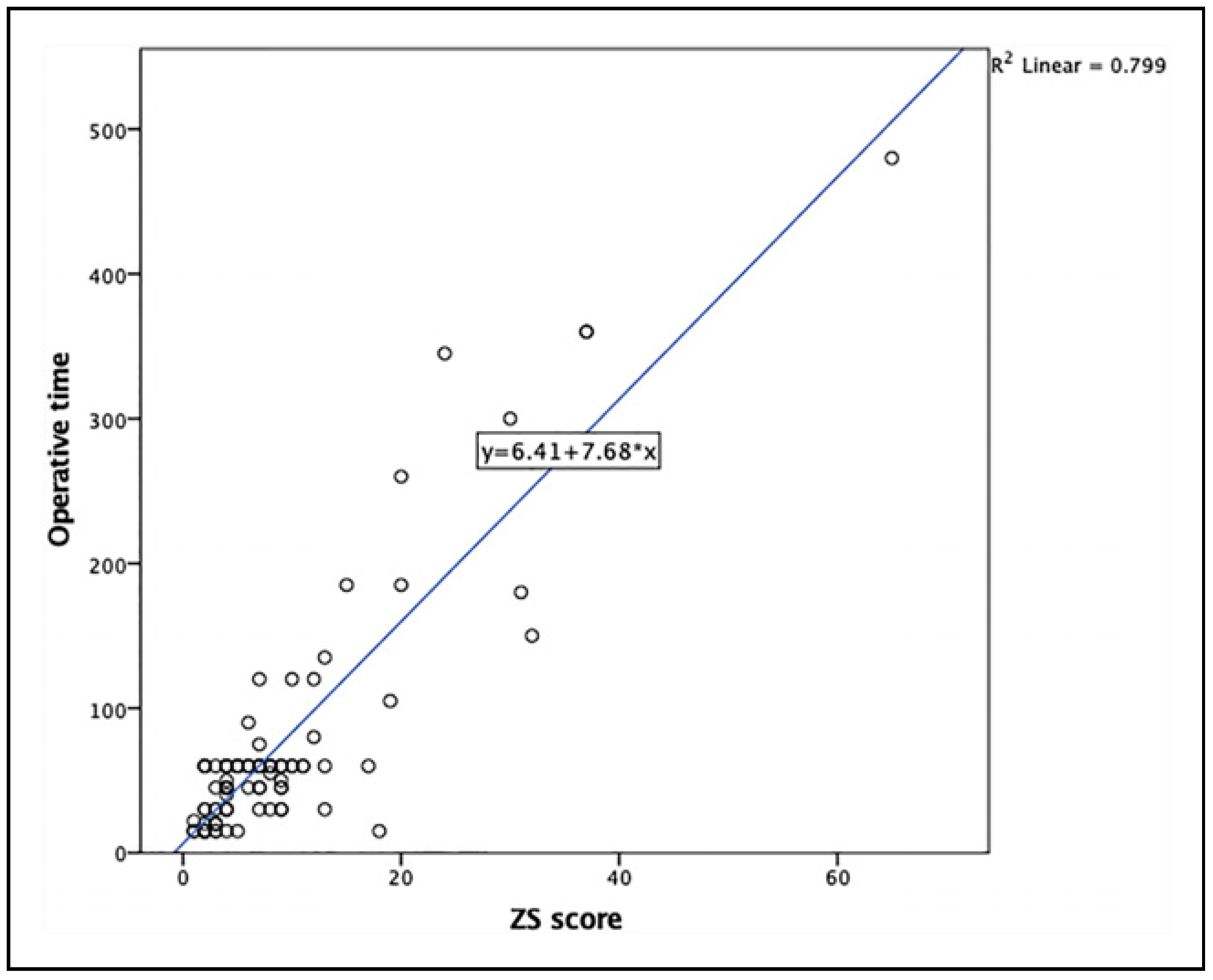
Multiple linear regression was performed with ZS score as predictor and age and gender as covariates. The results of the regression indicated that the model explained 79.7% of the variance with operative time and the model was significant, F (1,98) = 390.12, P < .001. Multicollinearity diagnostics excluded the covariates, age and gender, as their Correlation coefficient was very low with ZS score and the Variance Inflation Factor (VIF) was below 5 (.998 for age and .996 for gender).
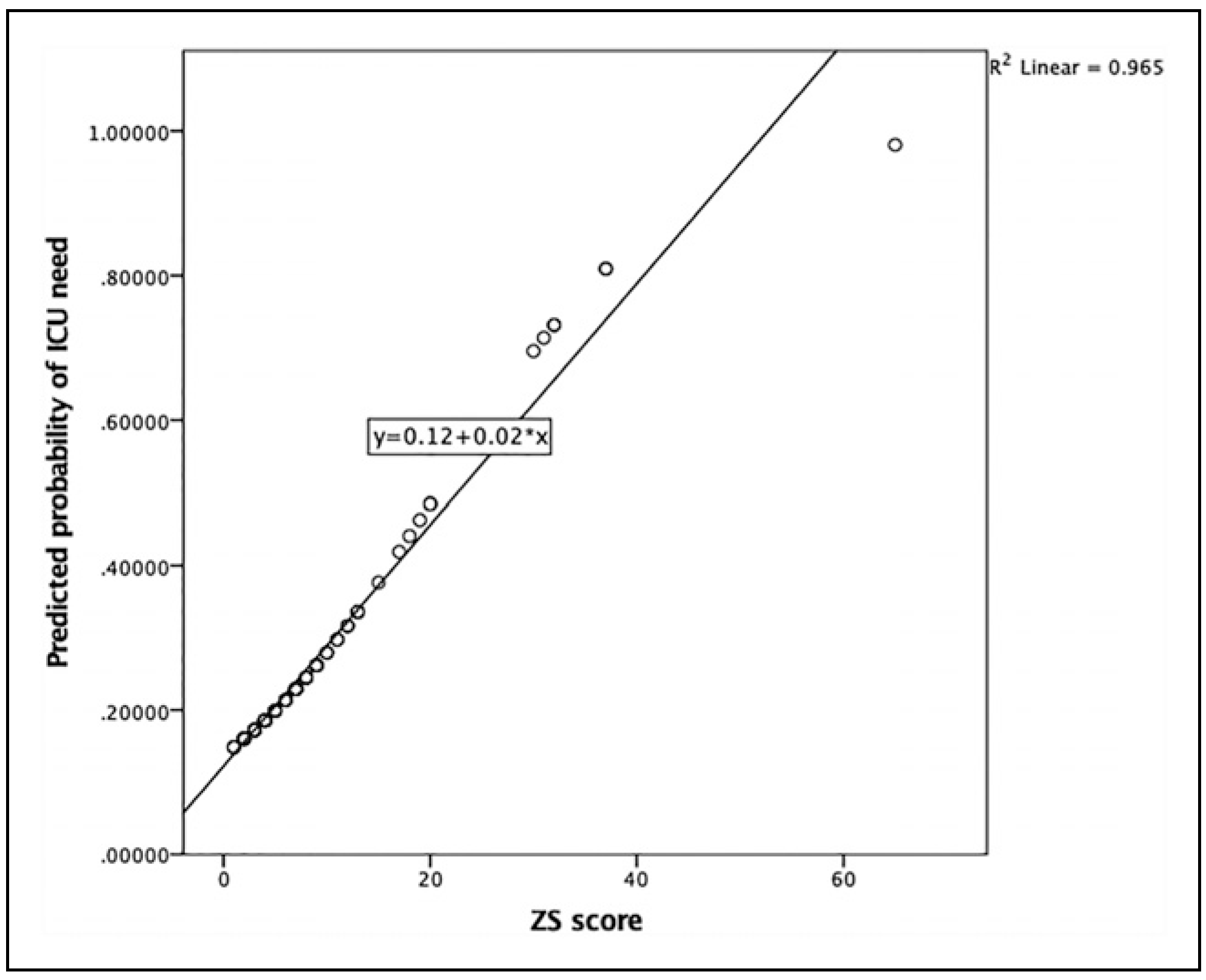
The predicted probability plot (
Figure 3) confirms the fit of the regression model but the linear regression scatter plot (
Figure 4) had few outliers and aggregation of low ZS scores; therefore, outlier analysis was performed. The resulting standardized residual scatter plot and case-based diagnostics shows only 2 data points as heteroscedastic, and the calculated Cook’s distances were below the value of 1, which confirms the data to be homoscedastic. The outliers were included in the analysis and the results because they were confirmed to be statistical outliers but not regression outliers and the assumption of the linear regression model was proved to be statistically true. It was found that the ZS score predicted operative time (
b1 = 7.67,
P < .001) in our study sample. The final predictive model in our study sample was: Operative time = 6.41 + (7.6*ZS score).
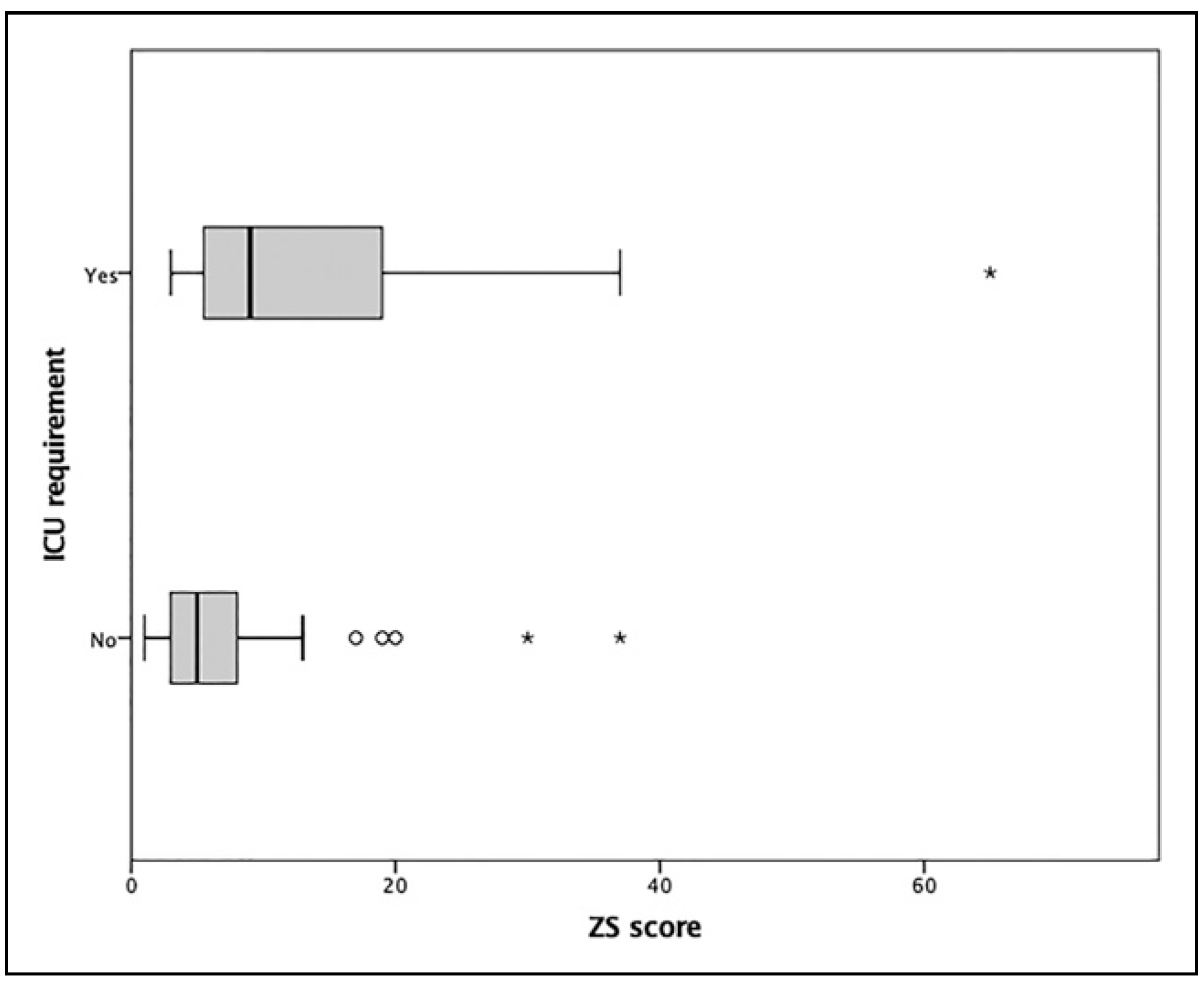
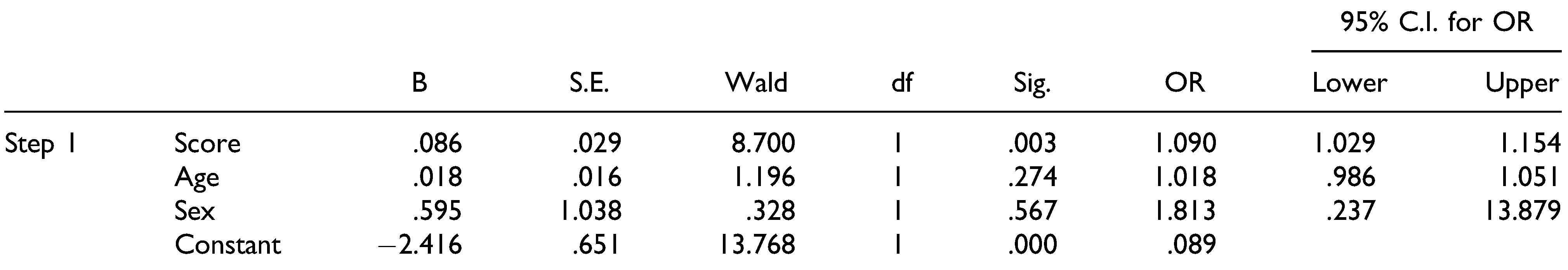
To explore the correlation between the predictor variables and the need for ICU, a binary logistic regression was performed. The overall logistic regression model was statistically significant,
X2(3) = 13.682,
P = .003 and Nagelkerke
R2 = .186. The goodness of fit of the model was confirmed with Hosmer and Lameshow test,
X2(8) = 2.157,
P = .976. The contingency table for Hosmer and Lameshow test predicts ICU requirement with significant accuracy and there were no significant outliers. Increasing ZS score was more likely to be associated with ICU admission (OR = 1.019) with each unit increase in ZS score increases the probability of ICU requirement by 9%. Only the ZS score could predict the ICU outcome with statistical significance while no statistically significant association was found between age and gender with the ICU need (
Table 2). Boxplots of ZS Scores against the outcome of ICU requirement shows higher ZS scores associated with ICU need (
Figure 5) and the predicted probability of ICU need plotted against the ZS score produces a linear regression association (
Figure 6).
Discussion
Our study was designed to seek the application of app-based ZS maxillofacial trauma score to predict the operative time, ICU need and length of stay. We aimed to find the predictive model based on an easy to use app-based maxillofacial trauma score to predict the operative time, ICU need and length of stay.
Our results show that there is a significant, strong and positive association of ZS score with operative time, and it can predict operative time based on the statistical linear regression model. A similar correlation was found between operating time and facial trauma score by Zhang et al[
4] and Catapano et al,[
3,
6] although they did not explore the predictive capability of their scores. Though operative time is directly dependent upon the surgical approach used and the type and number of fixations, ours study involved a single surgeon in all the operations to avoid this variation and a standard approach following established international guidelines for fixation was used, hence the linear regression model can be truly predictive, but needs to be verified in further prospective studies, preferably at multiple centres.
In our study, the ZS trauma score showed a statistically significant association with the ICU requirement and the statistical regression model was able to predict ICU requirement based on the increasing ZS score, independent of age and gender. These findings suggest that the ZS trauma score can be used as a prognostic tool in maxillofacial trauma management, at the same time being app-based, can be carried in the pocket on smartphones and tablets to record, rapidly interpret and share. Although, this finding is confounded, because ICU need was evaluated by the anaesthetist, not based on the ZS score. We believe a prospective study with adjusted analysis for ICU need based on ZS score, independent of airway evaluation status can explain the relationship better.
The first facial injury score was the Cooter David score,[
7] an alphanumeric score that is based upon the division of the face into major and minor regions which are assigned an alphabetical value. A numerical value is assigned to the severity of bony fractures but the scoring system is complex due to the involvement of cranial structures and does not delineate between craniofacial structures like orbit and pterygoid plates.[
7] Another classification system proposed by Donat et al[
8] is based on the skeletal support mechanism of vertical and horizontal buttresses of the midface but fails to incorporate orbital walls and nasal bone in the scoring system. This system provides so many fracture combinations that it loses its clinical use. Buitrago-Tellez et al[
9] proposed a new classification based on the AOASIF classification system of Muller et al. Although very descriptive of fracture patterns, this system does not provide final summary measures of fracture severity. Furthermore, each of these classification systems excluded the mandible and soft tissue, which is necessary for scoring facial injuries.
Maxillofacial Injury Severity Score (MFISS) was proposed by Zhang et al[
3] in 2005 which was based on AIS-90 standards of facial injury and also incorporated patientrelated outcomes like malocclusion, limited mouth opening and facial deformity. This system significantly correlated with the cost and length of hospital stay but it failed to account for orbital and frontal bone involvement, both of which significantly impact the management and outcome of facial trauma patients. The facial injury severity scale (FISS) was proposed by Bagheri et al[
10] in 2006 which was devised as a communicative tool between trauma management teams but has less predictive value for perioperative outcomes. A novel facial fracture severity scale was developed by Catapano et al[
6] in 2010 where anatomic fracture regions were colour coded but they did not account for soft tissue injuries and severity of the fracture. Their model of scoring is comprehensive and predictive; however, not incorporating fracture severity undermines its strength.
ZS maxillofacial trauma score developed by Ahmad et al[
4,12] in 2012 utilized the strength of all scoring systems and improved them. It is a weighted assessment of fracture patterns and utilizes comminution and segmentation as a regional multiplier in the determination of the final score.[
11] It takes into account the number of fractures in various anatomic regions, the severity of fractures, the complexity of condylar fractures and the involvement of dentition. It can be scored easily by minimally trained emergency personnel with the help of a visually developed app (iOS) and can be stored and shared electronically. The app eliminates the steps of calculation and procurement of a colour coded chart, simultaneously displaying results along with a case summary for the patient.
Studies have shown that maxillofacial trauma scores have a good predictive value of the patient outcomes as well as perioperative outcomes like the hospital stay, operative time and cost of treatment.[
12,
13] A similar study by Ramalingam et al[
14] has shown an association between maxillofacial trauma score and economic burden on the patient’s family. This can be used as a counselling tool to routinely predict the patient’s clinical outcomes as well as perioperative outcomes and obtain informed consent from the patient’s family. Our results show that a significant number of patients required ICU care. This could be due to the difference in the level of isolated maxillofacial injuries presenting to our centre alongside a lack of monitoring facilities in the general ward. Patients in the upper limit of trauma score with comminuted midfacial fractures or extensive orofacial lacerations require airway monitoring and support, which is only available in ICU at our centre. Our unit’s protocol requires overnight ICU care for panfacial fractures and prolonged operations that require a blood transfusion, tracheostomy or respiratory monitoring. A study by Holmgren et al[
15] compared various perioperative outcomes of the maxillofacial trauma patients managed with or without tracheostomy at a level I trauma centre. They reported an average of 1.33 days of ICU stay and 6.82 days of hospital stay in patients managed without tracheostomy. Our cohort of patients is similar to the non-tracheostomy group in the above study and our results are similar in length of stay (6 days) and average ICU requirement (1.33 days). Our study could not find any correlation between the ZS score and length of hospital stay. This result is similar to the authors of the ZS trauma score who found a significant correlation of the ZS score with the number of implants used, which is an indirect indicator of treatment cost but could not find any significant correlation between the score and hospital stay of patients.[
2] In a survey of trauma patients by Al Hassani et al,[
16] 1 out of 5 patients underwent surgery with a median length of stay in ICU for 5 days and in hospital for 7 days which is similar to our finding. Length of hospital stay is influenced by many factors like age of the patient, existing comorbidities, experience and skill of the operating surgeon, type and duration of anaesthesia and discharge criteria of the hospital, which might explain why we could not find any association between the ZS score and the length of hospital stay.[
17,
18] We recommend a larger prospective study, with a subgroup and cut-off analysis of ZS score which may yield significant variation with length of stay, and explain the non-significant finding in our study. A recent retrospective study by Canzi et al. introduces a new, simple, comprehensive and reproducible score for facial trauma called CFI (Comprehensive Facial injury) score, in which its severity is expressed in relation to the surgical duration necessary for definitive treatment. It demonstrated a linear regression between CFI score and surgical duration, and a high degree of accuracy in forecasting overall surgical time for each type of facial injury.[
19] Another recent publication by Aita et al reported that FISS scores greater than 5 presented with 18 times the chance of needing intervention in the OR and a greater possibility of hospitalization longer than 3 days (
P < .01). Higher FISS scores may predispose patients to a longer hospitalization time, a greater chance of undergoing surgical procedures and a greater need for follow-up by other medical specialities.[
20] Our regression model based on the ZS score found similar predictive capability for the surgical operative time which according to the authors is the parameter identified as the most significant in expressing the commitment of care required, while having the advantage of being smartphone based. Smartphones are ubiquitous and electronic health record systems are more likely to be easily integrated with smartphone based apps in the near future, thus simplifying the application and integration of facial trauma score in overall patient management.[
21] The ZS score model in its original form does not include the frontobasal unit, but a recent update has been proposed by Douglas et al,[
22] where a craniofacial disruption index was integrated with the existing ZS model, promising an updated app with the added craniofacial disruption score to complement the ZS score model.
The limitation of this study is its retrospective design which can be a source of selection bias. Though we made sure with strict inclusion criteria that patients with comorbidities and concomitant multisystem injuries are not included in the sample for homogeneity and to remove confounding bias, there are still many factors that may affect the outcomes. The ZS score does not contain a soft tissue component. Extensive soft tissue injuries could potentially affect the outcomes and findings of the study, although we excluded those cases for homogeneity in the sample, this limitation remains and needs to be addressed by the app developers in the future. The ZS facial trauma score app is available only on iOS, and we believe if the system is ported to the android platform, which has a wider user base, it will increase the user ratio. A multicenter study with a larger and standardized sample is recommended to further confirm the predictive value of the ZS score, preferably with patient oriented outcomes. It will also be interesting to compare the results from multiple units in future.
ZS maxillofacial trauma score is a simple, intuitive, user friendly and visual app-based scoring system which provides a composite score that can be utilized for documentation, communication and prognostic purpose. The ZS score can predict the operative time and increasing ZS score was associated with ICU requirement, but the need for ICU was based on airway evaluation only. Additionally, ZS score could not predict hospital length of stay in this study. As it is an app-based scoring system, it has the potential to be integrated into the electronic medical record system, which can simplify the documentation of facial trauma. It can also be used as a counselling and communication tool between caregivers and the patient’s family. Medical devices and apps are already invaluable tools for us, and as their features and uses expand, they are expected to become even more widely incorporated into nearly every aspect of clinical practice. We believe an app-based facial trauma score like the ZS score can provide meaningful, accurate and timely information and guidance to the end-user to serve the vital purpose of improving patient outcomes.