Intraoperative Positioning in Maxillofacial Trauma Patients with Cervical Spine Injury—Is It Safe? Radiological Simulation in a Healthy Volunteer
Abstract
:Introduction
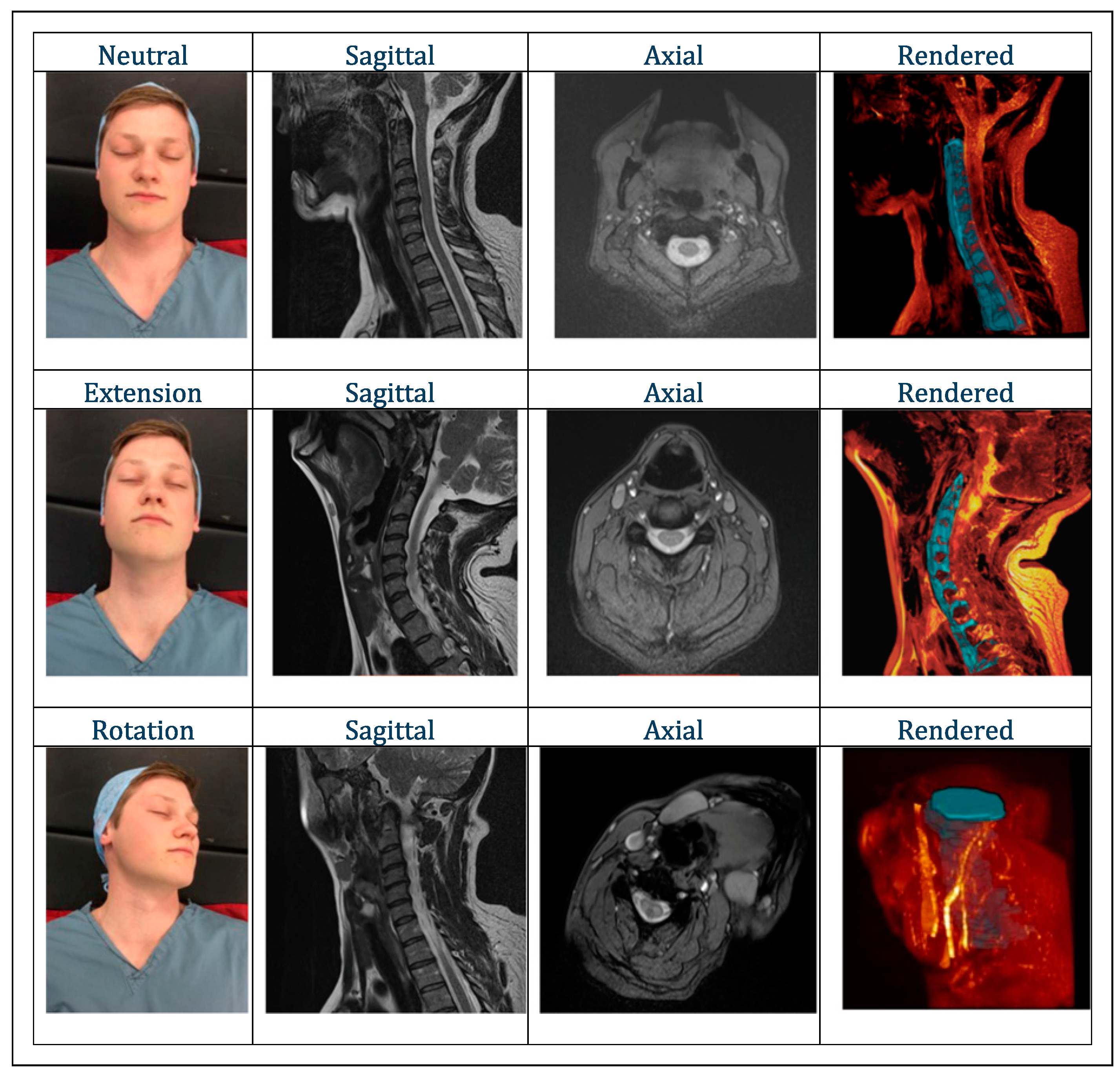
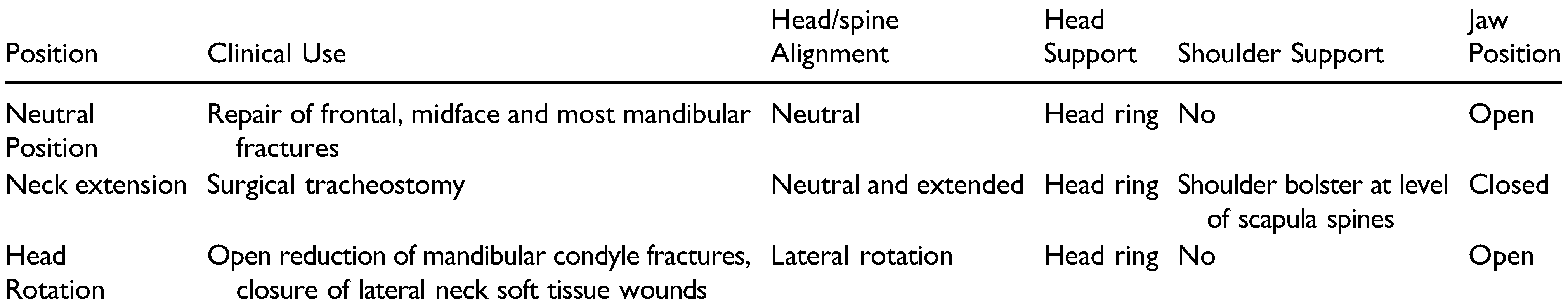
Methods
Results
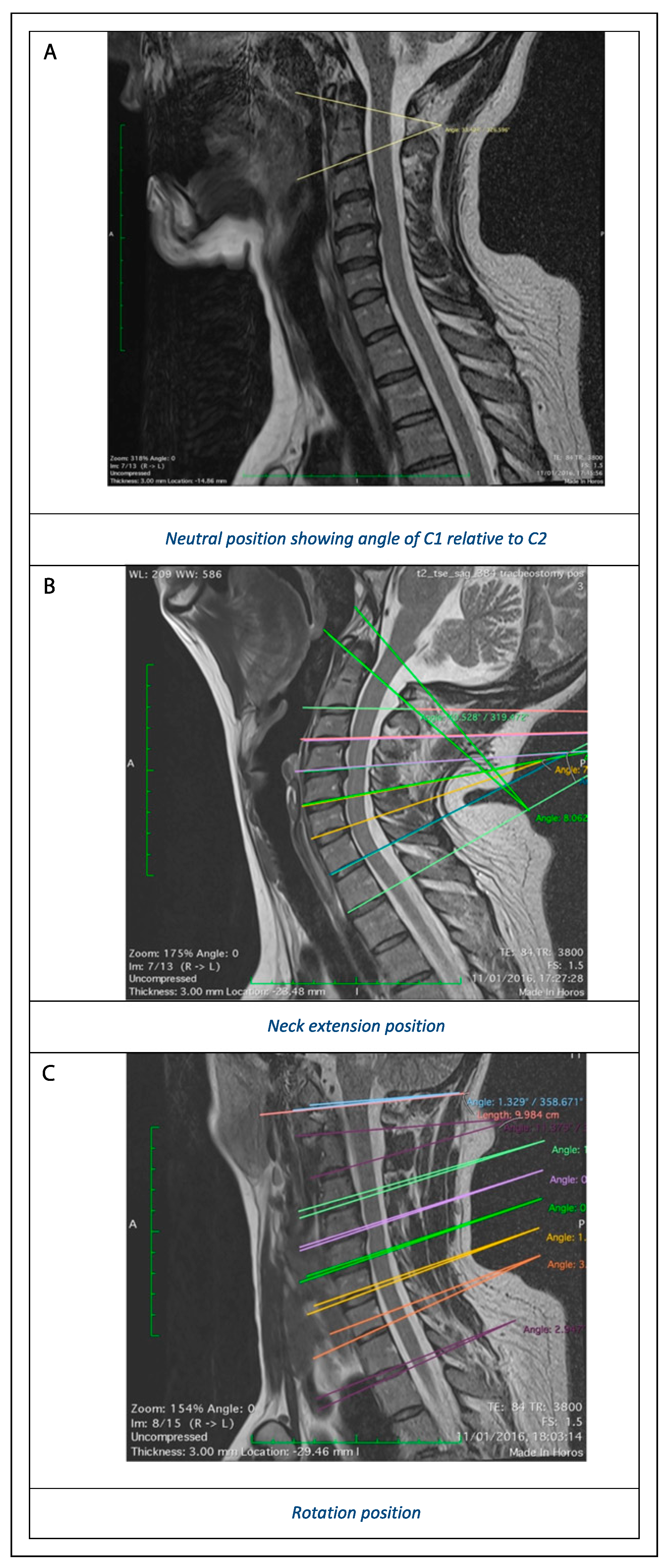
Effect of positioning on cervical spine alignment:
Effect of Extension
Effect of Rotation
Discussion
Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Elahi, M.M.; Brar, M.S.; Ahmed, N.; Howley, D.B.; Nishtar, S.; Mahoney, J.L. Cervical spine injury in association with craniomaxillofacial fractures. Plast Reconstr Surg. 2008, 121, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Mithani, S.K.; Mithani, S.K.; St-Hilaire, H.; et al. Predictable patterns of intracranial and cervical spine injury in craniomaxillofacial trauma: analysis of 4786 patients. Plast Reconstr Surg. 2009, 123, 1293–1301. [Google Scholar] [CrossRef] [PubMed]
- Chu, M.W.; Soleimani, T.; Evans, T.A.; et al. C-spine injury and mandibular fractures: lifesaver broken in two spots. J Surg Res. 2016, 206, 386–390. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S.; Abhinav, K.; Revington, P.J. A review of cervical spine injury associated with maxillofacial trauma at a UK tertiary referral centre. Ann R Coll Surg Engl; 2015, 91, 66–72 101308/003588414X14055925059633. [Google Scholar]
- Roccia, F.; Cassarino, E.; Boccaletti, R.; Stura, G. Cervical spine fractures associated with maxillofacial trauma: An 11-year review. J Craniofac Surg. 2007, 18, 1259–1263. [Google Scholar] [CrossRef] [PubMed]
- Jamal, B.T.; Diecidue, R.; Qutub, A.; Cohen, M. The Pattern of Combined Maxillofacial and Cervical Spine Fractures. J Oral and Maxillofacial Surg. 2009, 67, 559–562. [Google Scholar] [CrossRef]
- Mulligan, R.P.; Mahabir, R.C. The prevalence of cervical spine injury, head injury, or both with isolated and multiple craniomaxillofacial fractures. Plast Reconstr Surg. 2010, 125, 1647–1651. [Google Scholar] [CrossRef] [PubMed]
- Mourouzis C, Schoinohoriti O, Krasadakis C, Rallis G, Cervical spine fractures associated with maxillofacial trauma: a 3-year-long study in the Greek population. J cranio-maxillofacial surg. 2018, 46, 1712–1718. [CrossRef] [PubMed]
- Beirne, J.C.; Butler, P.E.; Brady, F.A. Cervical spine injuries in patients with facial fractures: a 1-year prospective study. International journal of oral and maxillofacial surgery. 1995, 24, 26–29. [Google Scholar] [CrossRef] [PubMed]
- Lalani, Z.; Bonanthaya, K.M. Cervical spine injury in maxillofacial trauma. Br J Oral and Maxillofac Surg. 1997, 35, 243–245. [Google Scholar] [CrossRef]
- Schilling, C. Audit of Time from Admission to Open Reduction and Internal Fixation of Mandibular Fractures. Internal audit; 2016 (unpublished).
- Stone, N.; Corneman, A.; Sandre, A.R.; Farrokhyar, F.; Thoma, A.; Cooper, M.J. Treatment delay impact on open reduction internal fixation of mandibular fractures: a systematic review. Plasti reconstr surgery. Glob open. 2018, 6, e1829. [Google Scholar] [CrossRef] [PubMed]
- Holmes, J.F.; Akkinepalli, R. Computed tomography versus plain radiography to screen for cervical spine injury: a metaanalysis. J trauma. 2005, 58, 902–905. [Google Scholar]
- National Institute for Health and Care Excellence. Spinal Injury: Assessment and Initial Management. NICE Guideline NG41; National Clinical Guideline Centre: London, UK, 2016. [Google Scholar]
- Reich, W.; Surov, A.; Eckert, A.W. Maxillofacial trauma – Underestimation of cervical spine injury. J Cranio-Maxillofacial Surg. 2016, 44, 1469–1478. [Google Scholar] [CrossRef] [PubMed]
- Hackl, W.; Hausberger, K.; Sailer, R.; Ulmer, H.; Gassner, R. Prevalence of cervical spine injuries in patients with facial trauma. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, and Endod. 2001, 92, 370–376. [Google Scholar] [CrossRef]
- Davidson, J.S.; Birdsell, D.C. Cervical spine injury in patients with facial skeletal trauma. The Journal of trauma. 1989, 29, 1276–1278. [Google Scholar] [PubMed]
- Dvorak, J.; Froehlich, D.; Penning, L.; Baumgartner, H.; Panjabi, M.M. Functional radiographic diagnosis of the cervical spine: flexion/extension. Spine. 1988, 13, 748–755. [Google Scholar] [PubMed]
- Penning, L.; Wilmink, J.T. Rotation of the cervical spine. A CT study in normal subjects. Spine. 1987, 12, 732–738. [Google Scholar] [PubMed]
- Bogduk, N.; Mercer, S. Biomechanics of the cervical spine. I: normal kinematics. Clinical biomechanics (Bristol, Avon). 2000, 15, 633–648. [Google Scholar] [PubMed]
- Dankmeijer, J.; Rethmeier, B.J. The lateral movement in the atlanto-axial joints and its clinical significance. Acta Radiologica. 1943, 24, 55–66. [Google Scholar]
- Mimura, M.; Moriya, H.; Watanabe, T.; Takahashi, K.; Yamagata, M.; Tamaki, T. Three-dimensional motion analysis of the cervical spine with special reference to the axial rotation. Spine. 1989, 14, 1135–1139. [Google Scholar] [PubMed]
 |
| (a) Anterior Mandible Position (‘Neutral’) | ||||
| AP Flexion (Sagittal Plane) | Change in Extension Angle Relative to Neutral | Rotation (Trans plane) | Change in Rotation Angle Relative to Neutral | |
| SB – C1 | —1 | - | 0 | - |
| C1–C2 | 33 | - | 0 | - |
| C2–C3 | 1 | - | 0 | - |
| C3–C4 | —8 | - | 0 | - |
| C4–C5 | —1 | - | 0 | - |
| C5–C6 | 5 | - | 0 | - |
| C6–C7 | 6 | - | 0 | - |
| C7–T1 | —4 | - | 0 | - |
| (b) Tracheostomy position (extension) | ||||
| AP flexion (Sagittal plane) | Change in extension angle relative to neutral | Rotation (Trans plane) | Change in rotation angle relative to neutral | |
| SB – C1 | 8 | 9 | 0 | 0 |
| C1–C2 | 41 | 8 | 0 | 0 |
| C2–C3 | 2 | 1 | 0 | 0 |
| C3–C4 | 2 | 10 | 0 | 0 |
| C4–C5 | 6 | 7 | 1 | 1 |
| C5–C6 | 8 | 3 | 1 | 1 |
| C6–C7 | 9 | 3 | —1 | —1 |
| C7–T1 | 3 | 7 | 0 | 0 |
| (c) Mandibular Condyle Position (Lateral rotation) | ||||
| AP flexion (Sagittal plane) | Change in extension angle relative to neutral | Rotation (Trans plane) | Change in rotation angle relative to neutral | |
| SB – C1 | —1 | 0 | 7 | 7 |
| C1–C2 | 11 | —22 | 32 | 32 |
| C2–C3 | 2 | 1 | 3 | 3 |
| C3–C4 | 1 | 9 | 2 | 2 |
| C4–C5 | 1 | 2 | 6 | 6 |
| C5–C6 | 1 | —4 | 1 | 1 |
| C6–C7 | 4 | —2 | 0 | 0 |
| C7–T1 | —3 | 1 | 1 | 1 |
© 2022 by the author. The Author(s) 2022.
Share and Cite
Pepper, T.; Spiers, H.; Weller, A.; Schilling, C. Intraoperative Positioning in Maxillofacial Trauma Patients with Cervical Spine Injury—Is It Safe? Radiological Simulation in a Healthy Volunteer. Craniomaxillofac. Trauma Reconstr. 2022, 15, 312-317. https://doi.org/10.1177/19433875211053091
Pepper T, Spiers H, Weller A, Schilling C. Intraoperative Positioning in Maxillofacial Trauma Patients with Cervical Spine Injury—Is It Safe? Radiological Simulation in a Healthy Volunteer. Craniomaxillofacial Trauma & Reconstruction. 2022; 15(4):312-317. https://doi.org/10.1177/19433875211053091
Chicago/Turabian StylePepper, Thomas, Harry Spiers, Alex Weller, and Clare Schilling. 2022. "Intraoperative Positioning in Maxillofacial Trauma Patients with Cervical Spine Injury—Is It Safe? Radiological Simulation in a Healthy Volunteer" Craniomaxillofacial Trauma & Reconstruction 15, no. 4: 312-317. https://doi.org/10.1177/19433875211053091
APA StylePepper, T., Spiers, H., Weller, A., & Schilling, C. (2022). Intraoperative Positioning in Maxillofacial Trauma Patients with Cervical Spine Injury—Is It Safe? Radiological Simulation in a Healthy Volunteer. Craniomaxillofacial Trauma & Reconstruction, 15(4), 312-317. https://doi.org/10.1177/19433875211053091




