Abstract
Study Design: Retrospective cohort analysis. Objective: To examine the impact the COVID-19 pandemic and its accompanying societal measures had on the incidence, characteristics, and management of maxillofacial traumatic injuries. Methods: This cohort analysis compared facial trauma injuries presenting to the highest-volume Level I Trauma Center in New Jersey, USA from 1 January to 31 July in 2020 and 2019. Differences in demographics, mechanisms, and interventions were compared between the pandemic period (16 March–31 July 2020) and the equivalent pre-pandemic date period in 2019 using X2, Fishers Exact, and Mann–Whitney U testing. Results: In total, 616 subjects were included. The daily incidence of facial trauma consults during the 2020 pandemic (1.81 ± 1.1) decreased compared to 2019 (2.15 ± 1.3) (p = 0.042). During the outbreak, there was an increase in the proportion of subjects with positive urine drug screens (21.5% vs. 12.2%; p = 0.011) and injuries related to domestic violence (10.2% vs. 4.5%; p = 0.023). Patients were 30% less likely to be transferred from local hospitals (RR, 0.70 [0.53–0.93]; p = 0.014). Although subjects had a 25% increased risk of presenting with injuries deemed procedural (RR, 1.25 [95% CI, 1.05–1.56]; p = 0.048), a greater proportion were discharged with operative procedures scheduled as outpatients (16.0% vs. 4.9%; p = 0.005). Conclusions: The COVID-19 pandemic has impacted both the epidemiology and management of maxillofacial traumatic injuries, perhaps secondary to modifications in personal and community behaviors or the effects on healthcare systems in our region.
Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has had an immense impact on population, community, and individual behaviors and habits. Both government and personal measures were taken to limit spread of the virus and reduce healthcare burden including stay-at-home mandates, state-wide curfews, social distancing, and self-quarantine. Non-urgent and elective care was temporarily suspended in an effort to minimize viral exposure and its burden on the healthcare system. However, the impact on the prevalence and epidemiology of non-elective care, such as those precipitated by trauma, has yet to be fully elucidated. Early studies have demonstrated significant reductions in the volume and nature of both traumatic and orthopedic injuries.[1,2,3]
Historically, maxillofacial traumatic injuries demonstrate a predilection for young-adult, male patients and are most commonly caused by motor vehicle accidents.[4,5] As previously shown, seasonal trends, national holidays, and natural disasters influence the incidence of facial trauma.[6,7] Limited evidence has suggested changes in facial trauma epidemiology and injury paradigms during the COVID pandemic.[8,9,10,11,12]
Serving as the transfer center for over 30 hospitals in the area, our academic Level I Adult and Pediatric Trauma Center admits over 3,500 patients for traumatic injuries annually. As the only regional institution for maxillofacial trauma, our facility represents a model setting to examine epidemiological changes in patient, injury, and management trends. The purpose of this study was to examine how the incidence and characteristics of facial traumatic injuries were impacted by the COVID-19 pandemic. The investigators hypothesized that facial trauma volume and epidemiology would be unaffected during the outbreak. The specific aims were to compare the daily incidence, patient demographics, injury characteristics, and management paradigms between the 2020 pandemic and the same date range from the previous year.
Methods
Following approval from the Cooper University Health Care Institutional Review Board Committee (#20-480), the investigators designed a retrospective analysis of our institution’s prospectively maintained trauma registry. The study population was composed of all patients who received a consultation for facial trauma evaluation from January 1, 2019 to July 31, 2019 and January 1, 2020 to July 31, 2020. Each subject’s electronic medical records were independently reviewed and data was extracted into a secure study database.
Time (date of consultation) was the primary predictor variable used to classify subjects into two main cohorts: pandemic (March 16, 2020–July 31, 2020) and prepandemic (March 16, 2019–July 31, 2019). We used March 16th to define the start of the pandemic period as this corresponded to when regional government officials enacted a state-of-emergency and introduced a mandatory stay-at-home order which enforced a curfew, closed all in-person academic activities, and barred all non-essential businesses.
For the purpose of secondary analysis, we defined subgroups based on the following date parameters in both 2019 and 2020 cohorts: before (January 1–March 15), peak (March 16–June 8), and reopening (June 9–July 31), for a total of six subgroups. June 8th corresponded to the date when the regional stay-at-home order was lifted and phased plans for societal openings were integrated.
The primary outcome variables of interest were the incidence and characteristics of the facial trauma, defined as: patient age (continuous); gender (nominal); type of presentation (EMS trauma alert, emergency room consult/triage, or transfer from outside institution); mechanism of injury (nominal); relation to domestic violence (dichotomous); relation to self-harm (dichotomous); positive blood alcohol and/or urine drug screen testing (dichotomous); intubated at the time of consultation (dichotomous); status of COVID testing at the time the consult was seen (when applicable: negative test, positive test, pending, or never tested); the structures injured related to the trauma (mandibular, midface, orbital, frontal sinus, nasoethmoid complex, nasal bone, and/or soft tissue); treatment provided (no intervention, bedside procedure performed at the time of consult, procedure performed in the operating room within 24 h of consult, procedure performed in the operating room after 24 h of consult but within the same hospitalization, or operative intervention to be scheduled as an outpatient). Incidence was measured as total counts and number of consults per day. The proportion of subjects who either died, transferred, left against medical advice, or refused treatment was recorded.
Descriptive statistics were calculated for the cohort. Shapiro-Wilk testing was performed to assess normal distribution of the data. Differences in daily consult volume between the main study cohorts were calculated by independent samples t-test. Difference in the outcome variables were evaluated using Pearson Chi-square and Fishers Exact testing (categorical variables) and Mann–Whitney U testing (continuous variables). Relative risk (RR) with 95% confidence intervals (95% CIs) were calculated via Chi-square and Fishers Exact testing. A two-sided critical value of p < 0.05 was used to define significance. In the subgroup analysis, we compared outcome variables between the 2020 and 2019 subgroups (before 2019 vs. before 2020; peak 2019 vs. peak 2020; and reopening 2019 vs. reopening 2020). All statistical analysis was conducted using SPSS (IBM SPSS Statistics Software, Version 27.0. Armonk, NY, USA).
Results
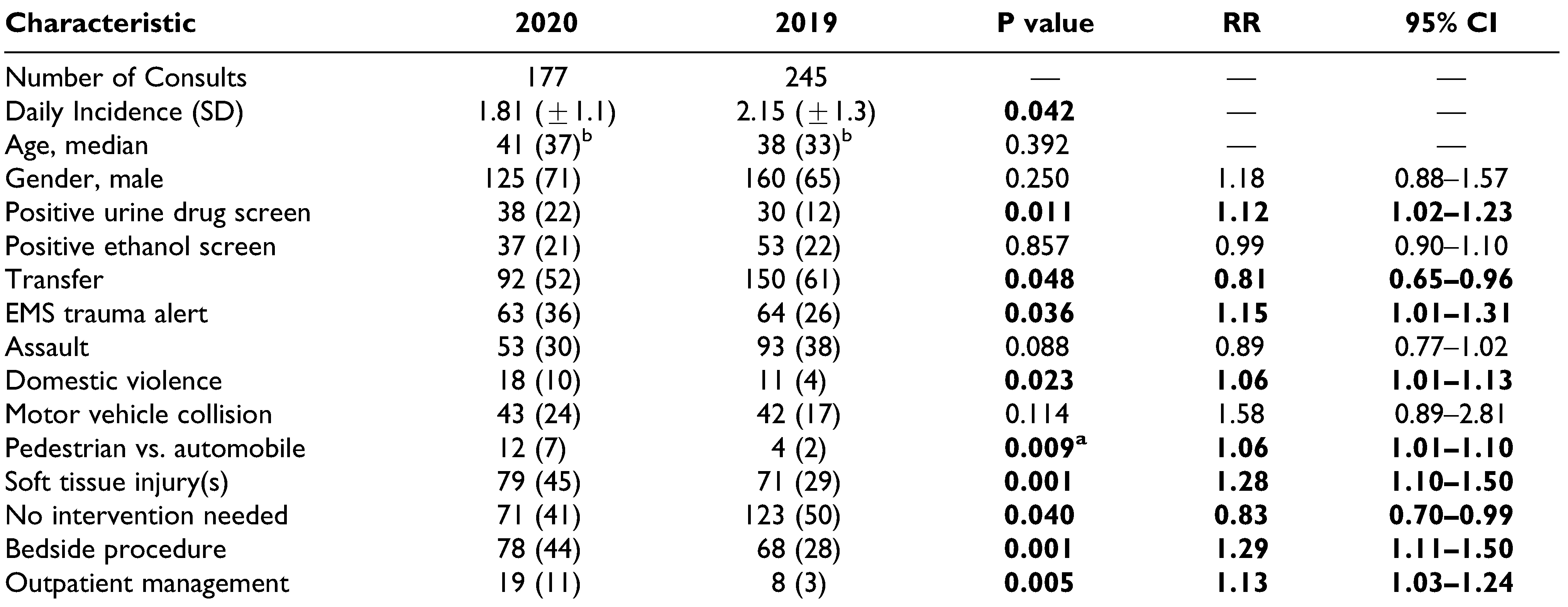
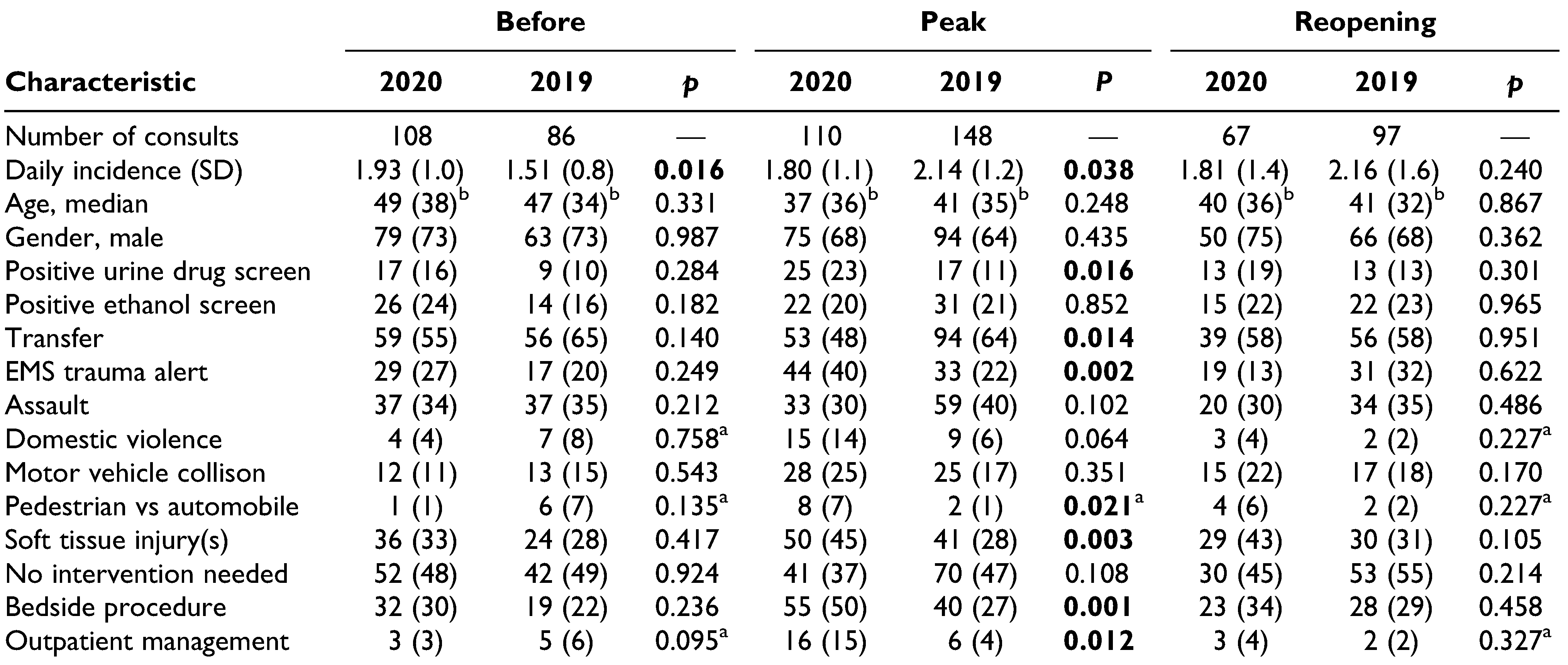
In total, 616 facial trauma cases were included in the study: 331 in 2019, 285 in 2020. During the 2020 pandemic period, there were less facial traumatic injuries (n = 177) compared to 2019 (n = 245) and there was a significant difference in the daily incidence of consults (1.81 + 1.1) compared to the year prior (2.15 + 1.3) (p = 0.042). A similar trend was observed when comparing the peak period in 2020 (1.80 + 1.1) to the equivalent dates in 2019 (2.14 + 1.2) (p = 0.038). This significant difference was specific for the peak period and not observed when comparing the reopening periods (p = 0.240). There were significantly more consults per day (1.93+1.0) during the before 2020 period (January 1–March 15, 2020) compared to the before 2019 period (January 1–March 15, 2019) (1.51 + 0.8) (p = 0.016). Figure 1 illustrates the differences in the incidence of consults over the study periods.
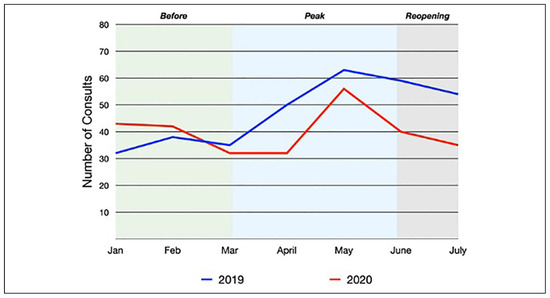
Figure 1.
Number of consults each month for 2019 and 2020. The before, peak, and reopening subgroup periods are represented by the shaded background colors.
The median age of patients seen during the pandemic was 41 years old (range: 2–95) and 38 years old in 2019 (range: 2–100) (p = 0.392). No differences were observed among the subgroups. Males represented 70% of patients in the pandemic period and 65% in the 2019 period (p = 0.25). No significant differences in gender distribution were observed amongst the subgroups.
There was a greater proportion of cases during the pandemic with positive urine drug screens (21.5%) compared to the pre-pandemic cohort (12.2%) (RR, 1.12 [95% CI, 1.02–1.23]; p = 0.011). Again, this difference was exclusive for the peak period (RR, 1.14 [95% CI, 1.02–1.29]; p = 0.016) and not seen between the reopening subcohorts (p = 0.301). There was no difference in the proportion of subjects with positive alcohol blood screens during the pandemic (21%) compared to the year prior (22%) (p = 0.857).
The proportion of transfers from outside institutions was decreased during the pandemic compared to the prior year (52.0% vs. 61.2%) (RR, 0.81 [95% CI, 0.65–0.96]; p = 0.048). Patients during the peak pandemic were 30% less likely to have been transferred compared to the year prior (RR, 0.70 [95% CI, 0.53–0.93]; p = 0.014). This trend was not observed when stratified for the before or reopening subgroups. Consults were 1.15 times as likely to present as an EMS alert during the pandemic compared to 2019 (RR, 1.15 [95% CI, 1.01–1.31]; p = 0.036). A significant difference was noted amongst the peak subgroups (RR, 1.30 [95% CI, 1.09–1.54]; p = 0.002), but not in the before or reopening subgroups. There were no significant differences in the proportions of emergency room consultations.
The most common mechanism of injury causing facial trauma during the pandemic was assault (29.9%) followed by motor vehicle collisions (24.3%). The most common mechanism during the 2019 cohort was assault (38.0%) followed by falls (31.4%). Consults seen during the pandemic had the same risk of having been assaulted compared to those from the year prior (RR, 0.89 [95% CI, 0.77–1.02]; p = 0.088). These nonsignificant relationships persisted when stratified amongst subgroups. The proportion of injuries related to domestic violence increased during the pandemic (10.2% in 2020 vs. 4.5% in 2019) (RR, 1.06 [95% CI, 1.01–1.13]; p = 0.023). Patients were more likely to have been pedestrians struck by an automobile during the pandemic (RR, 1.06 [95% CI, 1.01–1.10]; p = 0.009). There were no differences observed in the proportions of those who suffered from motor vehicle collisions, falls, power tools accidents, or sporting accidents. Eleven patients (6.21%) presented with injuries resulting from dog bites during the pandemic compared to 12 patients (4.90%) the year prior (p = 0.557). There were no significant differences in the incidence or proportion of self-harm injuries resulting in facial injury.
There was a significant increase in the proportion of consults entailing soft tissue injury during the pandemic (44.6%) compared to the year before (29.0%) (RR, 1.28 [95% CI, 1.10–1.50]; p = 0.001). Patients presenting during the peak pandemic had a 33% increased risk of having soft tissue injury requiring specialist evaluation compared to 2019 (RR, 1.33 [95% CI, 1.09–1.62]; p = 0.003). The most commonly injured osseous structures during the 2020 pandemic were the nasal bones (30.5%) and the midface (29.9%). During the corresponding period in 2019, the orbit (29.4%) and the nasal bones (29.0%) were most commonly injured. There were no significant differences in the proportion of patients who experienced mandible, midface, frontal sinus, naso-orbitoethmoid (NOE), orbital, nasal bone, and multiple osseous injuries between any of the 2020 and 2019 periods. Incidence of injury by diagnosis is graphically illustrated in Figure 2.
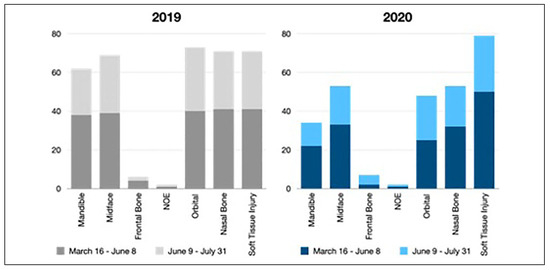
Figure 2.
Incidence of the structures injured during the 2020 pandemic and 2019. The data is further stratified into the peak periods (March 16th–June 8th) and reopening periods (June 9th–July 31st).
Patients who presented during the pandemic had a 25% increased risk of presenting with injuries deemed procedural compared to those the year prior (RR, 1.25 [95% CI, 1.05–1.56]; p = 0.048), as nearly 60% of consults were felt to require intervention (vs. 49.8% in 2019). Bedside procedures on the day of consultation were performed for 44.1%of cases compared to only 27.8%pre-pandemic (RR, 1.29 [95% CI, 1.11–1.50]; p = 0.001). Subjects had a 46% increased risk of requiring a bedside procedure when stratified for the peak period (RR, 1.46 [95% CI, 1.18–1.80]; p < 0.001). There was a significant increase in the proportion of subjects requiring intervention who were discharged and scheduled for surgery as an outpatient (16.0% vs. 4.9%) (RR, 1.13 [95% CI, 1.03–1.24]; p = 0.005). This difference was exclusive for the peak period (RR, 1.17 [95% CI, 1.03–1.34]; p = 0.012) and not observed in the before or reopening subgroups. Only 9% of subjects were admitted and had surgical procedures in the operating room during the pandemic compared to 20.8% the year prior (RR, 0.87 [95% CI, 0.80–0.94]; p = 0.001). There were no differences in the proportion of consults who were admitted (for any reason) nor those who were intubated at the time of consultation. Table 1 summarizes differences in demographic and select endpoints between the 2020 pandemic and 2019 pre-pandemic cohorts. There were no other significant differences between all other outcome variables on the subgroup analysis. Table 2 illustrates the comparison of 2020 and 2019 subgroups.

Table 1.
Comparison of Demographics and Select Outcomes Between the Pandemic Cohort (March 16–July 31, 2020) and the Corresponding Pre-Pandemic Cohort (March 16–July 31, 2019).

Table 2.
Select Demographics and Outcomes Comparing the 2020 and 2019 Subgroups: 2020 Before vs. 2019 Before (January 1–March 15); 2020 Peak vs. 2019 Peak (March 16–June 8); and 2020 Reopening vs. 2019 Reopening (June 9–July 31).
In the 2020 pandemic group, 51 (29%) patients had negative COVID tests prior to the consult being seen. Forty-one (23%) patients had pending tests at the time the consult was seen, five of which ultimately resulted as positive. Eighty-five (48%) patients were never tested for COVID-19.
Discussion
Individual, community, and populational aspects of daily living have faced noticeable adjustments in effort to curtail the COVID-19 pandemic. The purpose of this study was to analyze how the pandemic and associated changes impacted trends in maxillofacial traumatic injuries. Specifically, this investigation aimed to evaluate differences in the incidence, patient and injury characteristics, and management patterns between the 2020 pandemic and the year prior. Our analysis showed a significant reduction in the absolute number and daily volume of consults during the pandemic. Despite the reduction in volume, patients had a 25% increased risk of requiring procedural intervention compared to the year prior. Although assaults were still the most common cause of injury, a greater proportion were related to domestic violence and more patients had positive urine drug screens.
The data presented in this report provides insight into individual and societal behaviors during periods of quarantine, social distancing efforts, and government-directed shutdowns. Undesired consequences of the enacted public health measures included economic recession and massive layoffs, which likely induced stressful domestic circumstances. The increase in domestic abuse may be secondary to an increased likelihood of violent encounters precipitated during household confinement. The greater proportion of patients found to have positive urine drug screens further supports the notion of increasing rates of substance abuse during the global health crisis.[13] Finally, there was a significant increase in pedestrians struck by motor vehicles, which may represent a higher volume of pedestrians in the community or increases in reckless driving behaviors in response to decreased traffic. These findings parallel the results of other investigations to date.[8,9,10,11,12]
Perhaps more significant than the changes in epidemiology were the alterations in management paradigms and systems-based practices and brought forth by the pandemic. Not only was there a difference in the proportion of those who presented as traumas and EMS arrivals, there was a precipitous drop off in transfers from locoregional hospitals. This finding likely parallels the allotment of resources for patient testing, professional transport, and hospital bed availability during the pandemic. Further, there was an increase in bedside procedures performed. While this may be partially attributable to the increase in soft tissue injuries for which bedside procedures may be more appropriate, this trend may reflect efforts to reduce hospital admissions.
During the pandemic, there was an increase in the proportion of consults deemed operative, yet, operative injuries were more likely to be managed on an outpatient basis in comparison to 2019. Such patients were discharged home with conservative measures and short interval follow-up for surgical scheduling. This was likely done in an effort to reduce hospital admissions and healthcare burden during these unprecedented times. Inadvertently, this approach may also reduce the costs associated with inpatient hospitalization stays. In a similar CMF series, Ludwig et al. observed no difference in the proportion of patients admitted during the pandemic, but those admitted had an increased average length of stay compared to prior years.[12] Favoring outpatient management avoids the pitfalls of prolonged hospitalization in appropriately selected patients, but follow-up rates and outcomes must be strongly considered. If outcomes are non-inferior with outpatient management, this may be a positive effect brought forth by the pandemic. Our data prompts future investigations to explore potential factors predictive of outcomes balanced against associated reductions in healthcare expenditures.
Interestingly, 71% of patients had an unknown COVID status at the time the consult was seen during the pandemic. While the number, speed, and availability of testing increased in the later months, there was still a significant cohort who were never tested. Often the severity and urgency of traumatic injuries precedes pending laboratory results and providers must place themselves at an increased risk of potential exposure and personal injury. Nevertheless, it is crucial that hospitals and healthcare systems ensure the well-being of their employees is a top priority.
Although this was a moderate size sample, there are a number of limitations that should be noted. This analysis did not account for socioeconomic data or insurance status which likely influence the epidemiology and management of maxillofacial traumatic injuries. Though our institution serves as the largest state-designated Level I Trauma Center in New Jersey and services a diverse patient population transferred from neighboring counties, our results are specific to the geographical region. Similarly, weather patterns were not accounted for in our analysis. As noted by Bram et al warmer weather was observed during the pandemic year, which generally results in increased trauma incidence.[1,6] The subgroup analysis comparing prepandemic 2020 (January 1 to March 15) to the same time period in 2019 serves to demonstrate no difference in baseline in trends, which partially mitigates the influence temporal factors may hold. Multicenter studies should be conducted to further elucidate the associations explored in this report. Studies analyzing delays to care for maxillofacial injuries should be prioritized, as neglected injuries can lead to difficult to treat functional and cosmetic defects.
Conclusion
The COVID-19 pandemic has influenced all aspects of medical practice including facial trauma epidemiology and management. This study improves the current understanding of the severity, etiology, and characteristics of facial injuries during the pandemic, while providing insight into individual and community behaviors. This serves to promote future implementations aimed at optimal treatment practices and injury prevention. With a notable reduction in consult volume and locoregional transfers, maxillofacial tertiary-care centers can be better prepared to treat patients during severe resource allocation. Favoring bedside procedures and outpatient management, elicited by necessity during the current pandemic, may hold the potential to reduce hospital admission rates and associated costs. This report enlightens future investigations designed to assess treatment outcomes and economic effects related to these practices.
Author Contributions
Luke Stanisce: Conception and design, Acquisition of data, Analysis and interpretation of data, Drafting the article, Critical revision of the article, Final approval of the article, Agreement to be accountable for all aspects of the work, Overall responsibility. Alec H Fisher: Conception and design, Acquisition of data, Analysis and interpretation of data, Drafting the article, Critical revision of the article, Final approval of the article, Agreement to be accountable for all aspects of the work. Bo Young Choi: Acquisition of data, Analysis and interpretation of data, Critical revision of the article, Final approval of the article, Agreement to be accountable for all aspects of the work. Andrew Newman: Analysis and interpretation of data, Critical revision of the article, Analysis and interpretation of data, Final approval of the article, Agreement to be accountable for all aspects of the work. Ju Ling Wang: Analysis and interpretation of data, Critical revision of the article, Analysis and interpretation of data, Final approval of the article, Agreement to be accountable for all aspects of the work. Yekaterina Koshkareva: Conception and design, Analysis and interpretation, Critical revision of the article, Final approval of the article, Agreement to be accountable for all aspects of the work, Overall responsibility.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Bram, J.T.; Johnson, M.A.; Magee, L.C.; et al. Where have all the fractures gone? The epidemiology of pediatric fractures during the covid-19 pandemic. J Pediatr Orthop. 2020, 40, 373–379. [Google Scholar] [PubMed]
- Christey, G.; Amey, J.; Campbell, A.; Smith, A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for 2COVID-19 in New Zealand. N Z Med J. 2020, 133, 81–88. [Google Scholar] [PubMed]
- Placella, G.; Salvato, D.; Delmastro, E.; Bettinelli, G.; Salini, V. CoViD-19 and ortho and trauma surgery: The Italian experience. Injury. 2020, 51, 1403–1405. [Google Scholar] [PubMed]
- Wusiman, P.; Maimaitituerxun, B.; Guli null Saimaiti, A.; Moming, A. Epidemiology and pattern of oral and maxillofacial trauma. J Craniofac Surg. 2020, 31, e517–e520. [Google Scholar] [CrossRef] [PubMed]
- Gassner, R.; Tuli, T.; Hächl, O.; Rudisch, A.; Ulmer, H. Craniomaxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003, 31, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.M.; Willett, K. What is the effect of the weather on trauma workload? A systematic review of the literature. Injury. 2015, 46, 945–953. [Google Scholar] [PubMed]
- Stonko, D.P.; Dennis, B.M.; Callcut, R.A.; et al. Identifying temporal patterns in trauma admissions: Informing resource allocation. Winfield RD, ed. PLoS One. 2018, 13, e0207766. [Google Scholar]
- de Boutray, M.; Kün-Darbois, J.D.; Sigaux, N.; et al. Impact of the COVID-19 lockdown on the epidemiology of maxillofacial trauma activity: a French multicentre comparative study. Int J Oral Maxillofac Surg. 2020, 50, 750–755. [Google Scholar] [PubMed]
- Salzano, G.; Dell’Aversana Orabona, G.; Audino, G.; et al. Have there been any changes in the epidemiology and etiology of maxillofacial trauma during the covid-19 pandemic? An italian multicenter study. J Craniofac Surg. 2020. [Google Scholar]
- Saponaro, G.; Gasparini, G.; Pelo, S.; et al. Influence of Sars-Cov 2 lockdown on the incidence of facial trauma in a tertiary care hospital in Rome, Italy. Minerva Stomatol. 2020. [Google Scholar] [CrossRef]
- Vishal; Prakash, O.; Rohit; Prajapati, V.K.; Shahi, A.K.; Khaitan, T. Incidence of maxillofacial trauma amid covid-19: a comparative study. J Maxillofac Oral Surg 2020, 1–6. [Google Scholar]
- Ludwig, D.C.; Nelson, J.L.; Burke, A.B.; et al. What is the effect of COVID-19-related social distancing on oral and maxillofacial trauma? J Oral Maxillofac Surg. 2020, 79, 1091–1097. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.Q.; Kaelber, D.C.; Xu, R.; Volkow, N.D. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry. 2020, 26, 30–39. [Google Scholar] [CrossRef] [PubMed]
© 2021 by the author. The Author(s) 2021.