Abstract
Study Design: Retrospective, observational, cross-sectional study. Objective: To determine the incidence of skiing-related facial trauma and to identify their patterns in terms of potential risk factors, mechanism of injury, anatomical location, and degree of severity. Methods: Data was collected using the National Electronic Injury Surveillance System and included snow skiing-related incidents during the years 2009 to 2018. Specifically, injuries limited to the facial region including the head, face, eye(s), mouth, neck or ear(s) were reported. Patients with fractures were further classified by the study variables. Descriptive statistics were used to classify continuous variables while chi-square analysis was used to compare categorical variables. Results: A total of 514 (n = 514) patients met the inclusion criteria within the study period. The majority of injuries were due to concussions (59%), followed by lacerations (18%), fractures (11%), contusions (11%) and dental injuries (1%). Of the fractures seen, the majority were nasal (30%) and cervical spine (30%), followed by midface (27%), mandible (9%) and skull (4%). In our population, head injuries were more common in females (80%) than in males (60%), whereas, mouth injuries were more common in males (8%) than females (1%) [χ2 = 30.2, p < 0.001]. Conclusions: Skiing-related craniofacial trauma remains a significant mechanism of injury. Our data illustrates a need to correlate these injuries to the use of personal protective equipment. Furthermore, this data calls for the strict implementation of such equipment and the development of safety protocols to further prevent deleterious injury.
Introduction
With an estimated 200 million people participating worldwide, skiing has remained the most popular winter sport.[1] Estimates place the number of leisure skiers in the United States at over 13 million, with about 57 million visits to ski areas annually.[2] These visits have contributed to an estimated 600,000 ski- and snowboarding-related injuries in North America alone.[1] Because they represent over half of the injuries experienced among adult and child recreational skiers, much of the research devoted to skiing-related injuries has focused exclusively on lower extremity soft tissue trauma and fractures.[3,4,5]
In recent years, however, concerns over concussions and traumatic brain injury have become a more frequently studied topic regarding skiing-related injuries. Consequently, the research detailing head injuries sustained in this setting has expanded and influenced the technology surrounding helmets and protective gear, as well as encouraged increased regulations regarding the implementation of such equipment.[6]-[9] However, little research has been done to determine if the benefits of helmets extend to the face, despite the fact that previous studies have cited skiing to be the most common cause of sports-related oral and maxillofacial trauma.[8,10,11] Furthermore, despite the prevalence of craniofacial trauma sustained while skiing, facial injuries have only been explored to a modest degree. By reviewing the data associated with skiing-related facial trauma, a more comprehensive understanding of the factors that surround injury can be pursued, and evidence-based recommendations for safety measures and effective treatment protocols can be made. This study aims to determine the incidence of skiing-related facial trauma and to identify patterns in the context of mechanism of injury, anatomical location, and degree of severity.
Materials and Methods
An analysis of skiing-related facial trauma was conducted using the National Electronic Injury Surveillance System (NEISS). The NEISS is a valid injury surveillance system that collects consumer product-related injuries that occur in the United States from emergency departments (ED) of approximately 100 hospitals.[12] Reported information includes gender, race, ethnicity, injury diagnosis, affected body parts, incident location, and a brief description of said incident. The NEISS database qualifies as a non-human research source of public, anonymized data. Therefore, the Philadelphia College of Osteopathic Medicine’s (Philadelphia, PA) institutional review board (IRB) policy considers this research exempt from IRB review.
The NEISS was accessed in January 2020 and our query included snow skiing-related incidents that occurred between the years 2009 and 2018. Inclusion criteria included subjects >18 years of age and older who sustained a maxillofacial injury while snow skiing. Data surrounding each event were collected including injury type (concussion, contusion/abrasion, fracture, laceration, and dental injury), injury location (head, eyeball/globe, face [eyelid, eye area and nose], neck, mouth [lips, tongue, and teeth], and ear), and disposition of the patient (treated and released, transferred, admitted, held for observation, signed out against medical advice [AMA], and death). Patients with fractures were further classified by fracture location including nasal, midface, mandible, cervical spine, or skull. Variables of interest included age, gender, race, type of injury, anatomical location of injury, and disposition. Exclusion criteria included patients under the age of 18. Additionally, patients who sustained injuries that did not conform to the aforementioned categories were excluded from analysis.
Descriptive statistics including frequency, percentages, and means, were used to categorize continuous variables. Chi-square analysis was used to compare categorical variables using IBM SPSS® Version 26 (Armonk, NY). Statistical significance was set at a p-value <0.05.
Results
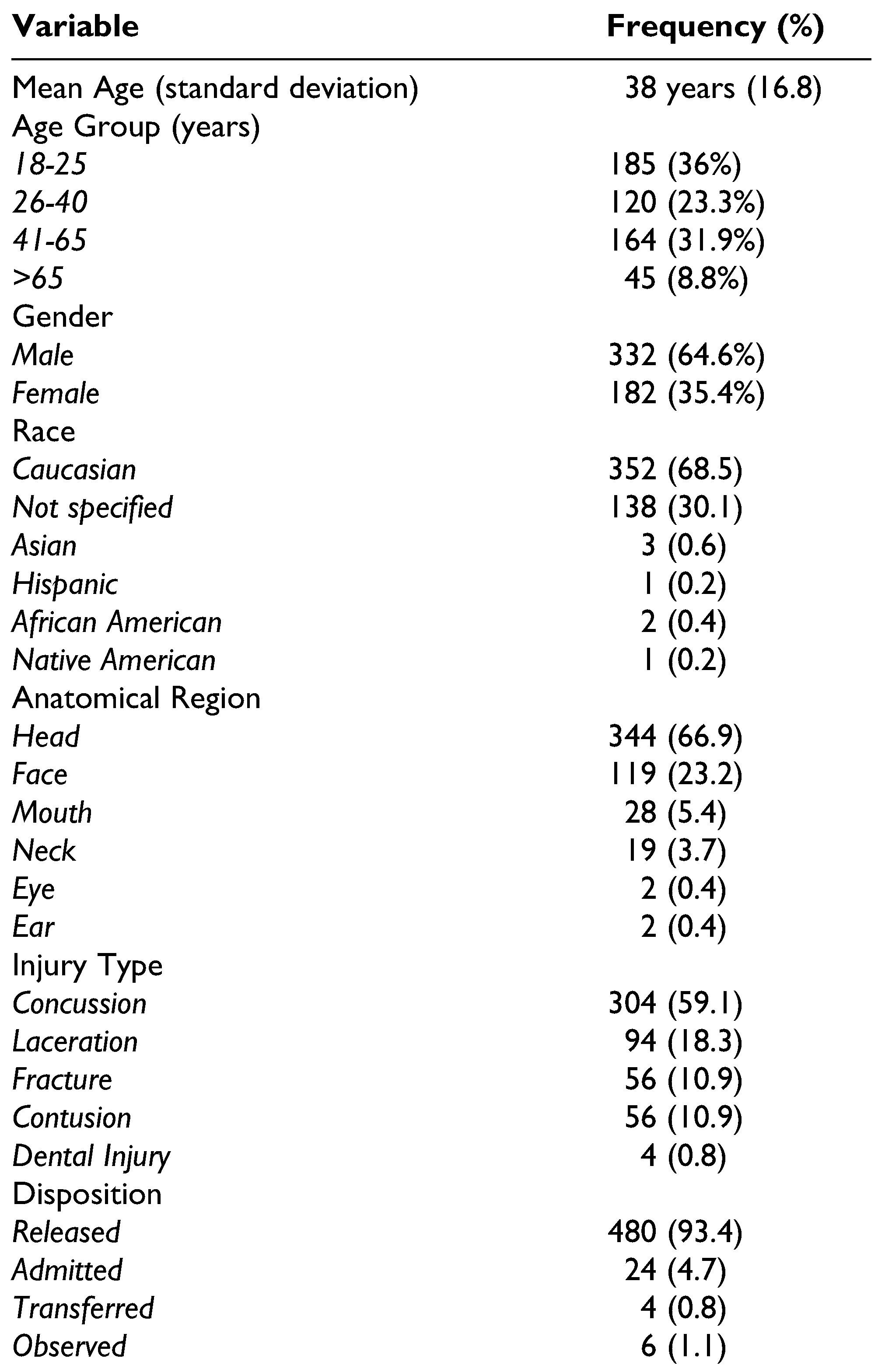
Between the years of 2009 and 2018, a total of 514 (n = 514) patients met our inclusion criteria. The mean age was 38 years with young adults (age group: 18-25) incurring 36% of the total injuries. Patients greater than 65 years of age only comprised 8.8% of the total sample. The patients were predominantly Caucasian and male. The vast majority of injuries were due to concussions, followed by lacerations, fractures, and contusions. Dental injuries were among the smallest minority representing not even 1% of the total injuries. The most common disposition for our patients was treated and released, followed by admission, transfer, and observation. With respect to location, the most common anatomical region of injury was the head (66.9%), followed by the face (23.2%), mouth (5.4%), neck (3.7%), eye (0.4%), and ear (0.4%) (Table 1).

Table 1.
Epidemiology of Emergency Department Visits (N = 514).
In our population, head injuries were more common in females (80%) as opposed to males (60%), whereas, mouth injuries were more common in males (8%) than females (1%) [χ2 = 30.2, p < 0.001]. There was no correlation between anatomical region of injury and age nor race. Concussions and contusions were more likely to occur in females (69%, 15%) than in males (54%, 9%), while lacerations were more likely to occur in males (24%) than in females (8%) [χ2 = 29.3, p < 0.001]. There were no gender disparities within fractures or dental injuries. There were no associations between type of injury and age nor race. Furthermore, there were no correlations between disposition and either age, gender nor race.
The majority of patients who sustained injuries were treated and released. This disposition was further stratified by injury type and included patients with concussions (95%), contusions (98%), lacerations (97%), and dental injuries (100%). This was in contrast to facial fractures, of which 71.4% of patients were treated and released. Patients with fractures (21%) were significantly more likely to be admitted compared to patients who suffered from concussions (3%), lacerations (2%), contusions (0%) and dental injuries (0%) [χ2 = 62.2, p < 0.001]. Patients with head (95%), face (97%), eye (100%), mouth (96%), and ear (100%) injuries were most likely to be treated and released compared to neck injuries (32%) which were most likely to be admitted (58%) or transferred (11%) [χ2 = 158.8, p < 0.001]. There were no associations between type of injury and anatomical region.
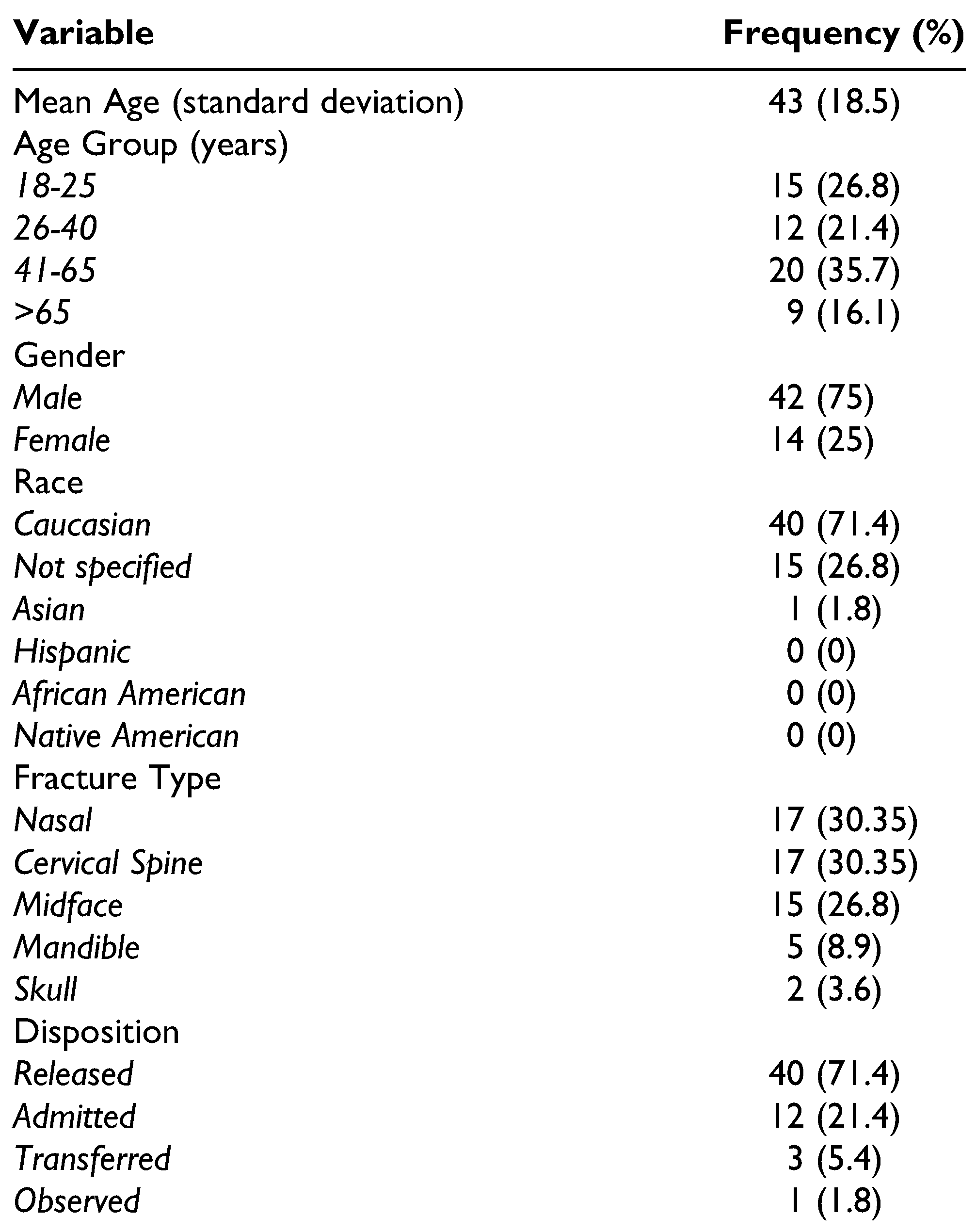
Within the subset of patients who sustained a fracture (n = 56), we found a similar demographic distribution as above. The most common type of fracture sustained while skiing was nasal (30.35%) or cervical spine (30.35%), followed by midface (26.8%), mandible (8.9%) and skull (3.6%). Patients between the ages of 41 and 65 sustained the most fractures with the mean age being 43 years. The most common disposition for patients with fractures was treated and released (71.4%), followed by admission (21.4%), transfer (5.4%), and observation (1.8%) (Table 2). There were no associations between fracture type and age, gender, nor race. Patients with nasal (100%), midface (87%) and mandible (80%) fractures were more likely to be treated and released compared to those with cervical spine (29%) or skull (50%) fractures whom were admitted [χ2 = 36.2, p < 0.001].

Table 2.
Facial Fracture Subcohort (N = 56).
Discussion
As skiing remains the most popular winter recreational activity among adults and children alike, the sport has expanded to include various subtypes including alpine, freestyle aerial and non-aerial skiing, ski mountaineering, big mountain skiing, and extreme skiing.[3] This has contributed to the rising numbers of skiers on the slopes and indirectly to the amount of facial traumas seen in this population. While many studies attribute the majority of skiing-related facial traumas to falls, collisions with other slope enthusiasts remain the second most common type of accident associated with facial injuries.[5,8,10,13] Thus, it is imperative to develop a comprehensive knowledge of these injuries in order to implement safety protocols and inform patient education. This study showed that particular patterns can be discerned from craniofacial injuries suffered while skiing.
Similarly, head injuries and traumatic brain injuries associated with recreational and professional skiing have influenced the research and legislation surrounding the use of protective head gear. Although information regarding the use of protective equipment within the NEISS database was not available, the vast majority of injuries reported were due to concussions which comprised 59% of our total sample. Furthermore, in terms of anatomical location, the head was reported as the most common site of injury representing 67% of the total injuries. This is consistent with previous studies which have shown that head injury occurs in up to 47% of skiing or snowboarding injuries and is the predominant cause of death in skiing-related accidents.[7] Fortunately, helmets have been shown to be effective in reducing linear acceleration experienced by the head and can reduce the risk of severe injuries and skull fractures as much as 60%.[7,14] It should be noted, however, that the helmet’s ability to protect skiers from traumatic brain injury (TBI), including skull fracture and concussion, has been called into question. Bailly et al, performed a case control study which demonstrated that the effect of helmet use on TBI was not significant.[15] Our study showed that skull fractures comprised the smallest minority at 4% of the total fractures reported. This could be due in part to the use of helmets which have become the norm despite the lack of universal regulations surrounding their use. With the exception of New Jersey, which requires persons under 18 years of age to wear a helmet, regulations in the North America leave this decision to the individual.[6] Despite, the lack of compulsory wear, about 57% of skiers and snowboarders wore helmets voluntarily during the 2009 to 2010 season as compared to 25% during the 2002 to 2003 season. [1] One study reviewing 17 seasons of the sport found that voluntary helmet use from 1991 to 2012 rose from 8% to 84%.[16] Furthermore, studies have found that the prevalence of injuries to the head has decreased from 8.4% to 6.8% and the prevalence of potentially serious head injuries declined from 4.2% to 3.0%.[17] It still remains unclear, however, whether or not these benefits extend to the face. One study that looked at the benefits of helmet use in reducing facial injuries found that the adjusted odds ratio estimate for facial injury among helmeted subjects compared with those who were not helmeted was 0.93 (CI = 0.79-1.09), which was not significant.[2] However, Bailly et al, found that when involved in a traumatic incident, helmet-wearing participants were at a lower risk of “other types of head injuries” which included but did not differentiate between lacerations, bruises, and face trauma.[15] By continuing to examine the patterns and mechanisms of injury specific to facial trauma, we can gain a better understanding of the protective effect of helmets, or lack thereof.
Overall, our data showed that males sustained the majority of skiing-related injuries (65%). This is consistent with previous research supporting that males have an overwhelmingly higher frequency of skiing-related trauma compared to females.[2,5,10,11,18] This trend is also true for facial bone fractures and is consistent with our findings which show that 75% of fractures occurred in males.[5,8,10] Today, there are both male and female helmets that include improved safety technology and meet the standards set by the United States Consumer Product Safety Commission, however, in the United States these standards are not mandatory. Furthermore, it is worth noting that the majority of ski helmets are unisex and those that do distinguish between male and female styles are strictly due to their color and ornamentation and not differences in the materials or overall design of the helmet. It is possible that the difference in injuries sustained while skiing between men and women is largely due to risk behavior, skill level, and the likelihood of wearing a helmet. There is persistent professional and public perception that the act of wearing a helmet could confer an increased sense of safety to the user, thus encouraging them to take greater risk and potentially negate the protective effect of a helmet.[19] According to a 2011 study by Ruˇzic et al which explored risk-taking behaviors in skiing among helmet wearers and non-helmet wearers, the population that contributes the most to the overall risk index value is male helmet wearers, signifying that male helmet wearers take more risks while skiing than others.[20] Furthermore, it has been known that male skiers generally take more risks than females on the slopes, regardless of helmet usage.[20] Ružic et al also found that occasional helmet users as compared with consistent helmet users displayed higher risk-taking behavior.[20] These findings were also echoed in a 2019 study by Willick et al, who found that male gender, younger age, snowboarding, higher perceived sport ability, and more time spent on the mountain and in the terrain park are associated with an increased risk-taking behavior among recreational skiers and snowboarders.[19] Thus, this may explain why males consistently sustain far more injuries on the slopes than females. Unfortunately, due to the limitations of the NEISS data query, we were unable to determine the degree of protective equipment, if used at all, that was present during the time of injury.
Of the fractures sustained, the highest percentages were seen in the nose and cervical spine, which each comprised 30% of the total number of fractures. The high percentage of nasal fractures is consistent with other sports. While our study focused entirely on the adult population, previous research has demonstrated that the most common site of facial fracture among pediatric patients participating in winter recreational activities is the nose.[6] This trend is consistent with the idea that younger skiers are particularly vulnerable to injury due to continued growth and underdeveloped coordination, skills, and perception.[3] Thus, further study regarding the use of facial protection, especially surrounding the nose, may be even more critical among these populations.[6] Our data also showed a high percentage (30%) of cervical spine injuries which are frequently seen in high contact sports such as football and wrestling.[19] Interestingly, of the patients who suffered cervical spine fractures, only 4 of the patients sustained concomitant injuries, none of which were facial fractures. These injuries consisted of a femur fracture, scalp laceration with elbow dislocation, bilateral pulmonary contusions, and free fluid in the pelvis. While we are not able to determine from our data which fractures, if any, correlate specifically to cervical spine injuries, this would be worth pursuing due to the life-threatening nature of these types of fractures. Spinal cord injuries are found in nearly 50% of patients with cervical vertebral injuries.[20] Spinal shock, neurogenic shock, vascular injury, soft tissue injury, and transient neurological deficits are just some of the devastating complications associated with these injuries.[20] While some studies have found that helmet use is associated with reduced risk of neck injuries, it remains unknown as to what degree of protection they provide.[14] This further emphasizes the need to correlate helmet use with reduced risk of injury to the neck and facial region and possibly the need to examine these injuries in the context of controlled studies.
Due to the limitations of NEISS reporting, information in regards to complications and detailed hospital course was unavailable. Mechanism of injury, slope conditions, slope terrain, weather conditions, and the experience level of the patients at the time of injury were not widely available. It is also important to note that this research did not reveal any significant correlations between facial trauma and concomitant pathology, however, this may be borne out in a larger sample size. Furthermore, as stated above, we were unable to determine the degree of protective equipment, if used at all, that was present during the time of the injury. The NEISS collects data in a nonstandardized manner across these various health systems, creating possible inconsistencies. As maxillofacial trauma providers, we also acknowledge the less-than-perfect reporting of facial injury regions. The database reports these injuries as involving the head, face (including the eyelid, eye area and nose), eyeball, mouth (including the lips, tongue, and teeth), neck and ear. There is significant cross-over with these structures which could potentially skew the results. Other limitations include the possibility of underreporting due to treatment at on site facilities, urgent care centers, and primary care offices. This is especially relevant for less severe soft tissue and dental injuries. Previous research has indicated that the most common type of soft tissue injury were lacerations followed by hematomas. [8] This is consistent with our findings of which 18% were lacerations followed by contusions at 11%. Although dental injury accounted for just 1% of the total injures within our query, previous studies have shown that those with dentoalveolar trauma also suffered from concomitant soft tissue injuries, and bone fractures.[10] This data emphasizes that helmets alone are likely not sufficient in preventing facial trauma and therefore a multifaceted approach to developing adequate facial protection may be necessary.
Our future research goals would be to design a prospective precise classification of midface fractures as the influence of the helmet type on the fracture type. Unfortunately, the NEISS data only allowed retrospective data collection. It would be interesting and beneficial to the public to team with manufacturers in order to develop specific protective equipment to prevent common injuries such as concussions, spine injuries and facial fractures.
Conclusion
Although the majority of skiing-related injuries reported are minor to moderate, concussions, facial fractures, and soft tissue injuries sustained during high velocity falls and collisions among skiers have the ability to severely impact aesthetics, function, and quality of life. Thus, it is out of necessity that the nature of skiing-related accidents and their long term sequelae are well understood by otolaryngologists and plastic surgeons and that their expertise are used to influence the development of sound protective gear. By providing preventative counseling and emphasizing the need for facial protection on the slopes, we can impact the culture surrounding the use of such equipment and thus reduce the potential for serious craniofacial trauma.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Haider, A.H.; Saleem, T.; Bilaniuk, J.W.; Barraco, R.D. An evidence-based review: efficacy of safety helmets in the reduction of head injuries in recreational skiers and snowboarders. J Trauma Acute Care Surg. 2012, 73, 1340–1347. [Google Scholar] [CrossRef] [PubMed]
- Mueller, B.A.; Cummings, P.; Rivara, F.P.; Brooks, M.A.; Terasaki, R.D. Injuries of the head, face, and neck in relation to ski helmet use. Epidemiology. 2008, 19, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Provance, A.J.; Daoud, A.K.; Tagawa, A.; Rhodes, J. Pediatric and adolescent injury in skiing. Res Sports Med. 2018, 26 (Suppl. S1), 150–165. [Google Scholar] [CrossRef] [PubMed]
- Wasden, C.C.; McIntosh, S.E.; Keith, D.S.; McCowan, C. An analysis of skiing and snowboarding injuries on Utah slopes. J Trauma. 2009, 67, 1022–1026. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, S.; Khodaee, M.; VanBaak, K. Common skiing and snowboarding injuries. Curr Sports Med Rep. 2019, 18, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Svider, P.F.; Bobian, M.; Hojjat, H.; et al. A chilling reminder: pediatric facial trauma from recreational winter activities. Int J Pediatr Otorhinolaryngol. 2016, 87, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Stuart, C.A.; Brubacher, J.R.; Yau, L.; Yip, R.; Cripton, P.A. Skiing and snowboarding head injury: a retrospective centre-based study and implications for helmet test standards. Clin Biomech (Bristol, Avon). 2020, 73, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Tuli, T.; Haechl, O.; Berger, N.; et al. Facial trauma: how dangerous are skiing and snowboarding? J Oral Maxillofac Surg. 2010, 68, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Polites, S.F.; Mao, S.A.; Glasgow, A.E.; Moir, C.R.; Habermann, E.B. Safety on the slopes: ski versus snowboard injuries in children treated at United States trauma centers. J Pediatr Surg. 2018, 53, 1024–1027. [Google Scholar] [CrossRef] [PubMed]
- Gassner, R.; V`asquez Garcia, J.; Leja, W.; Stainer, M. Traumatic dental injuries and alpine skiing. Endod Dent Traumatol. 2000, 16, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Exadaktylos, A.K.; Eggensperger, N.M.; Eggli, S.; Smolka, K.M.; Zimmermann, H.; Iizuka, T. Sports related maxillofacial injuries: the first maxillofacial trauma database in Switzerland. Br J Sports Med. 2004, 38, 750–753. [Google Scholar] [CrossRef] [PubMed]
- NEISS Frequently Asked Questions. CPSC.gov. Published April 8, 2020. Available online: https://www.cpsc.gov/ResearchStatistics/NEISS-Injury-Data/Neiss-Fre quently-Asked-Questions (accessed on 22 May 2020).
- Bailly, N.; Afquir, S.; Laporte, J.D.; et al. Analysis of injury mechanisms in head injuries in skiers and snowboarders. Med Sci Sports Exerc. 2017, 49, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sulheim, S.; Holme, I.; Ekeland, A.; Bahr, R. Helmet use and risk of head injuries in alpine skiers and snowboarders. JAMA. 2006, 295, 919–924. [Google Scholar] [CrossRef] [PubMed]
- Bailly, N.; Laporte, J.D.; Afquir, S.; et al. Effect of helmet use on traumatic brain injuries and other head injuries in alpine sport. Wilderness Environ Med. 2018, 29, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Weber, C.D.; Horst, K.; Lefering, R.; Hofman, M.; Dienstknecht, T. Pape HC. Major trauma in winter sports: an international trauma database analysis. Eur J Trauma Emerg Surg. 2016, 42, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Shealy, J.; Johnson, R.; Ettlinger, C.; Scher, I. Role of Helmets in Mitigation of Head Injuries: Epidemiologic Study of Head Injuries to Skiers. In Skiing Trauma and Safety: 20th Volume; Johnson, R., Shealy, J., Greenwald, R., Eds.; ASTM International: West Conshohocken, PA, USA, December 2015; pp. 22–36. [Google Scholar] [CrossRef]
- Kanwar, R.; Delasobera, B.E.; Hudson, K.; Frohna, W. Emergency department evaluation and treatment of cervical spine injuries. Emerg Med Clin North Am. 2015, 33, 241–282. [Google Scholar] [CrossRef] [PubMed]
- Willick, S.E.; Wagner, G.; Ericson, D.; Josten, G.; Teramoto, M.; Davis, J. Helmet use and risk-taking behavior among skiers and snowboarders. Clin J Sport Med. 2019, 29, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Ružić, L.; Tudor, A. Risk-taking behavior in skiing among helmet wearers and nonwearers. Wilderness Environ Med. 2011, 22, 291–296. [Google Scholar] [CrossRef] [PubMed]
© 2021 by the author. The Author(s) 2021.