Abstract
Study Design: Retrospective cohort. Objective: Traumatic facial fractures (FFs) often require specialty consultation with Plastic Surgery (PS) or Otolaryngology (ENT); however, referral patterns are often non-standardized and institution specific. Therefore, we sought to compare management patterns and outcomes between PS and ENT, hypothesizing no difference in operative rates, complications, or mortality. Methods: We performed a retrospective analysis of patients with FFs at a single Level I trauma center from 2014 to 2017. Patients were compared by consulting service: PS vs. ENT. Chi-square and Mann-Whitney-U tests were performed. Results: Of the 755 patients with FFs, 378 were consulted by PS and 377 by ENT. There was no difference in demographic data (p > 0.05). Patients managed by ENT received a longer mean course of antibiotics (9.4 vs 7.0 days, p = 0.008) and had a lower rate of open reduction internal fixation (ORIF) (9.8% vs. 15.3%, p = 0.017), compared to PS patients. No difference was observed in overall operative rate (15.1% vs. 19.8%), use of computed tomography (CT) imaging (99% vs. 99%), time to surgery (65 vs. 55 hours, p = 0.198), length of stay (LOS) (4 vs. 4 days), 30-day complication rate (10.6% vs. 7.1%), or mortality (4.5% vs. 2.6%) (all p > 0.05). Conclusion: Our study demonstrated similar baseline characteristics, operative rates, complications, and mortality between FFs patients who had consultation by ENT and PS. This supports the practice of allowing both ENT and PS to care for trauma FFs patients, as there appears to be similar standardized care and outcomes. Future studies are needed to evaluate the generalizability of our findings.
Introduction
Facial fractures (FFs) are a common reason for emergency room visits, accounting for over 400,000 annual visits in the United States alone.[1,2] The face is comprised of 14 different bones and FFs are the result of a spectrum of fracture patterns that can occur in isolation or in conjunction with other injuries.[2] In addition, the management of FFs represents an area of significant overlap across specialties and may be performed by otolaryngology (ENT), oral and maxillofacial surgery (OMFS), and plastic surgery (PS).[3,4,5]
Though modern medicine has made significant advances regarding the management of FFs, treatment approaches differ depending on hospital, treating service, and physician.[6,7,8] For instance, a study on fractures of the zygomaticomaxillary complex (ZMC) found that PS used a 3-point fixation technique regardless of fracture severity, whereas ENT and OMFS were less inclined to fixate as many points in less comminuted or displaced fractures.[9] Similarly, studies by Choi (2017) and Kim (2017) found differences between specialties in the management of frontal sinus fractures with PS favoring obliteration and ENT favoring ORIF.[6,10] Hence with different training, skills, and local political climates, referral patterns vary among institutions, with some hospitals referring to either ENT, PS or OMFS based upon provider preference or fracture location.[8] On the contrary, our Level I trauma center does not have an OMFS service, but alternates weeks of facial injury call between PS and ENT with no deviation based upon injury location or any other referral factors. It has been the authors’ anecdotal experience that care rendered and outcomes are similar between these different specialties.
However, due to the varied management of FFs based on specialty in the literature, we sought to conduct a study comparing management patterns and outcomes between patients with FFs managed by PS and ENT at our institution. [3,6,7,8,9,10,11] Since ENT and PS function independently without shared staff, residents or collaborative protocols at our institution, we sought to compare management between the 2 specialties. We hypothesized no difference in operative rates, antibiotic use, complications or mortality between the 2 services at our institution.
Methods
This study was approved by our local institutional review board (HS# 2018-4208). We performed a retrospective analysis of all adult trauma patients with FFs admitted to a single Level I trauma center between January 2014 to December 2017. All diagnoses were made by an attending radiologist after reviewing CT imaging of the head and/or face. Two groups were compared: trauma patients with FFs managed by either the ENT or PS service. At our institution there is no OMFS service, so ENT and PS split caring for trauma patients with FFs 1 week at a time, switching on Mondays. The primary outcome was operative intervention.
Demographic variables collected included age, sex, race, alcohol level, body mass index (BMI), admission status, admitting service, mechanism of injury, and type of fracture. Comorbidities included smoking, drug use, hypertension, congestive heart failure, myocardial infarction, coronary artery disease, chronic obstructive pulmonary disease, cerebrovascular disease, and end stage renal disease. The injury profile included the mechanism of injury, injury severity score and abbreviated injury scale for the head, face, thorax and abdomen. Type of FFs included orbital floor, mandible, frontal sinus, nasal bone/septum, zygomatic, and LeFort classification.
Additional variables measured included the specific type of radiographic imaging (e.g. computed tomography (CT) head, CT Maxillofacial, X-ray face, etc.), operative interventions, time to surgery, use of plates/screws, and closed reduction in the emergency department. Operative interventions included open reduction internal fixation (ORIF), intermaxillary fixation (IMF) (reducing or stabilizing a maxillary or mandibular fracture using arches, ligatures or screws alone or prior to ORIF), maxillomandibular fixation (MMF) (binding the mandible and maxilla with elastic bands or wire alone or prior to ORIF), and soft tissue injury repair. Antibiotic usage considered factors such as antibiotic name/class, duration, and whether the antibiotic was used for prophylaxis (antibiotics given without surgical intervention), pre-operative (antibiotics given prior to surgical intervention), peri-operative (antibiotics given intra-operatively or within 24 hours after surgery), or post-operative (antibiotics given greater than 24 hours after surgery). Outcomes were recorded for the hospitalization and at 30-day follow-up chart review. These included hospital length of stay, intensive care unit length of stay, discharge disposition, returns to the hospital, readmissions, and if the patient attended their follow-up appointment. 30-day complications included malocclusion, paresthesia, surgical site infection (SSI), return to the operating room, bleeding, venous thromboembolism (VTE), acute respiratory distress syndrome, pneumonia, sepsis, and death.
All variables were coded as present or absent. Descriptive statistics were performed for all variables. A Mann- Whitney-U test was used to compare continuous variables and a chi-square was used to compare categorical variables for bivariate analysis. Categorical data was reported as percentages, and continuous data was reported as medians with interquartile range. All P values were 2-sided, with a statistical significance level of <0.05. All missing data points were not imputed but treated as missing data. All analyses were performed with IBM SPSS Statistics for Windows (Version 24, IBM Corp., Armonk, NY).
Results
Demographics
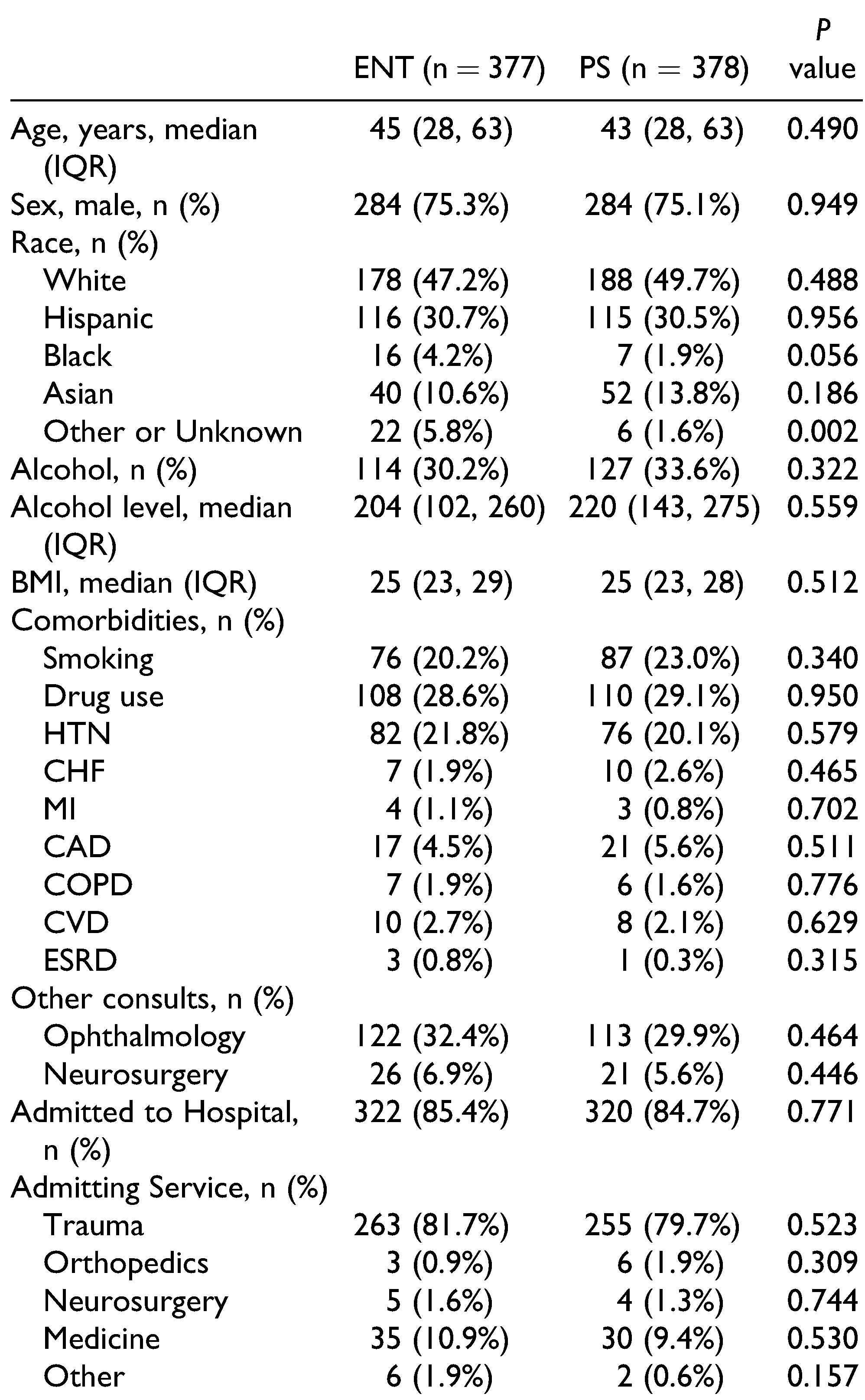
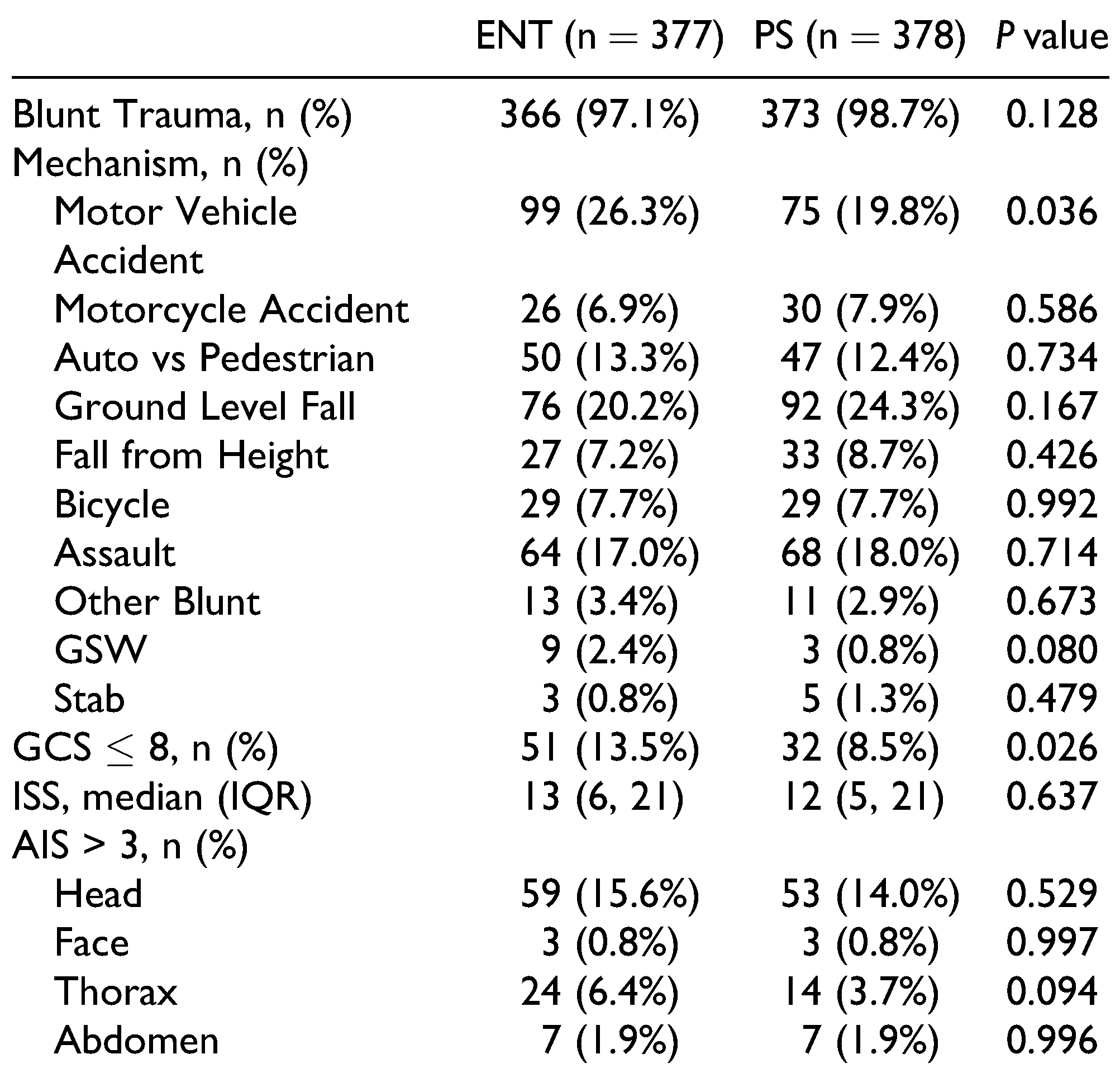
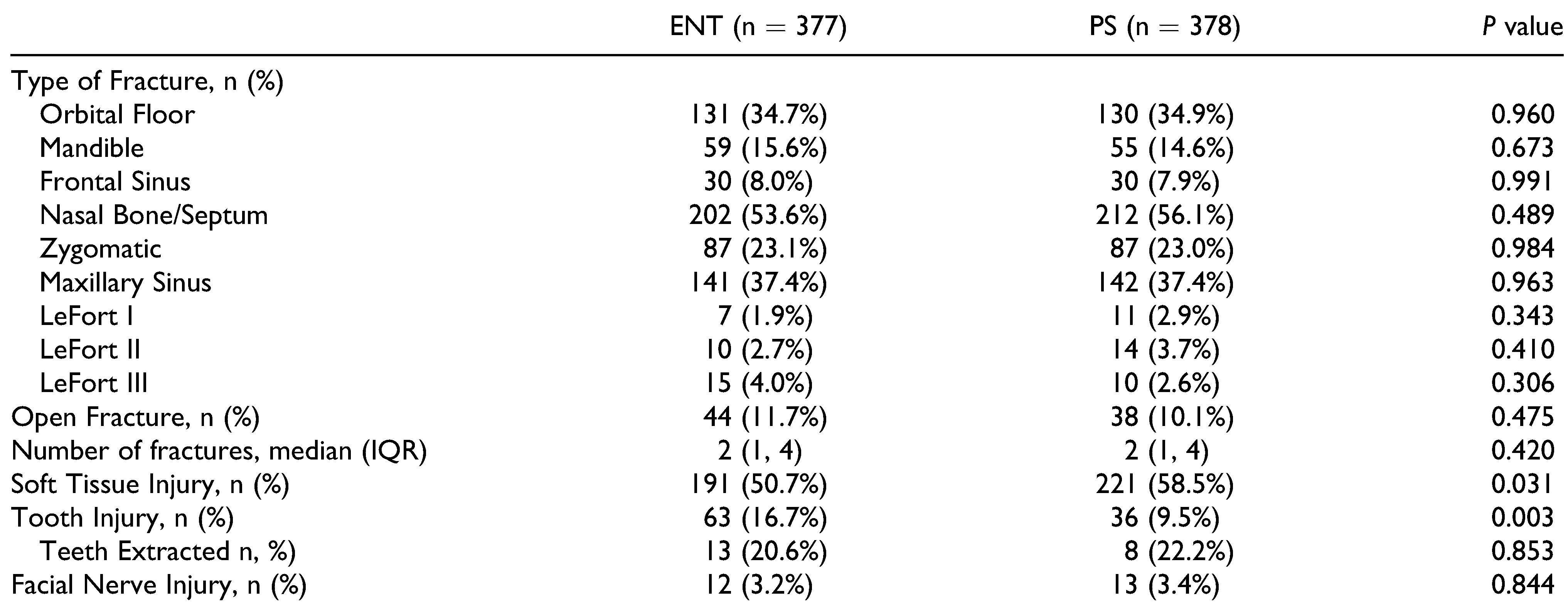
Of the 755 patients with FFs, ENT managed 377 (49.9%) and PS managed 378 patients (50.1%). Between the 2 cohorts, there were no differences in age (ENT: 45, PS: 43), male sex (ENT: 75.3%, PS: 75.1%), BMI (ENT: 25 kg/m2, PS: 25 kg/m2) or any medical comorbidities (all P > 0.05) (Table 1). PS admitted 23 patients (7.2%, P < 0.001) to its service whereas ENT admitted only 9 (2.8%, P = 0.003). There was no difference in the rate of patients sustaining blunt trauma (ENT: 97.1%, PS: 98.7%, P = 0.128) between the cohorts (Table 2). In addition, we found no difference in the rate of FF injury patterns: orbital floor (ENT: 34.7%, PS 34.9%, P = 0.960), mandible (ENT: 15.6%, PS: 14.6%, P = 0.673), frontal sinus (ENT: 8%, PS: 7.9%, P = 0.991), nasal bone (ENT: 53.6%, PS: 56.1%, P = 0.489), zygomatic (ENT: 23.1%, PS: 23.0%, P = 0.984), maxillary sinus (ENT: 37.4%, PS: 37.4%, P = 0.963), or any type of LeFort fracture (all P > 0.05). Both services had similar rates of open fractures (ENT: 11.7%, PS: 10.1%, P = 0.475), median number of fractures (ENT: 2, PS: 2, P = 0.42), and rate of facial nerve injury (ENT: 3.2%, PS: 3.4%, P = 0.844). However, the PS cohort exhibited a higher rate of soft tissue injury (ENT: 50.7%, PS: 58.5%, P = 0.031), whereas the ENT cohort had a higher rate of concurrent tooth injury (ENT: 16.7%, PS: 9.5%, P = 0.003) (Table 3) (Figure 2).

Table 1.
Comparison of Patient Demographics Between Otolaryngology (ENT) and Plastic Surgery (PS) Consults.

Table 2.
Comparison of Mechanism of Injury and Injury Profile.

Table 3.
Comparison of Traumatic Facial Fracture Characteristics.

Figure 2.
Injury patterns managed by otolaryngology and plastic surgery. ENT = Otolaryngology consult, PS = Plastic Surgery consult.
Diagnostics and Interventions
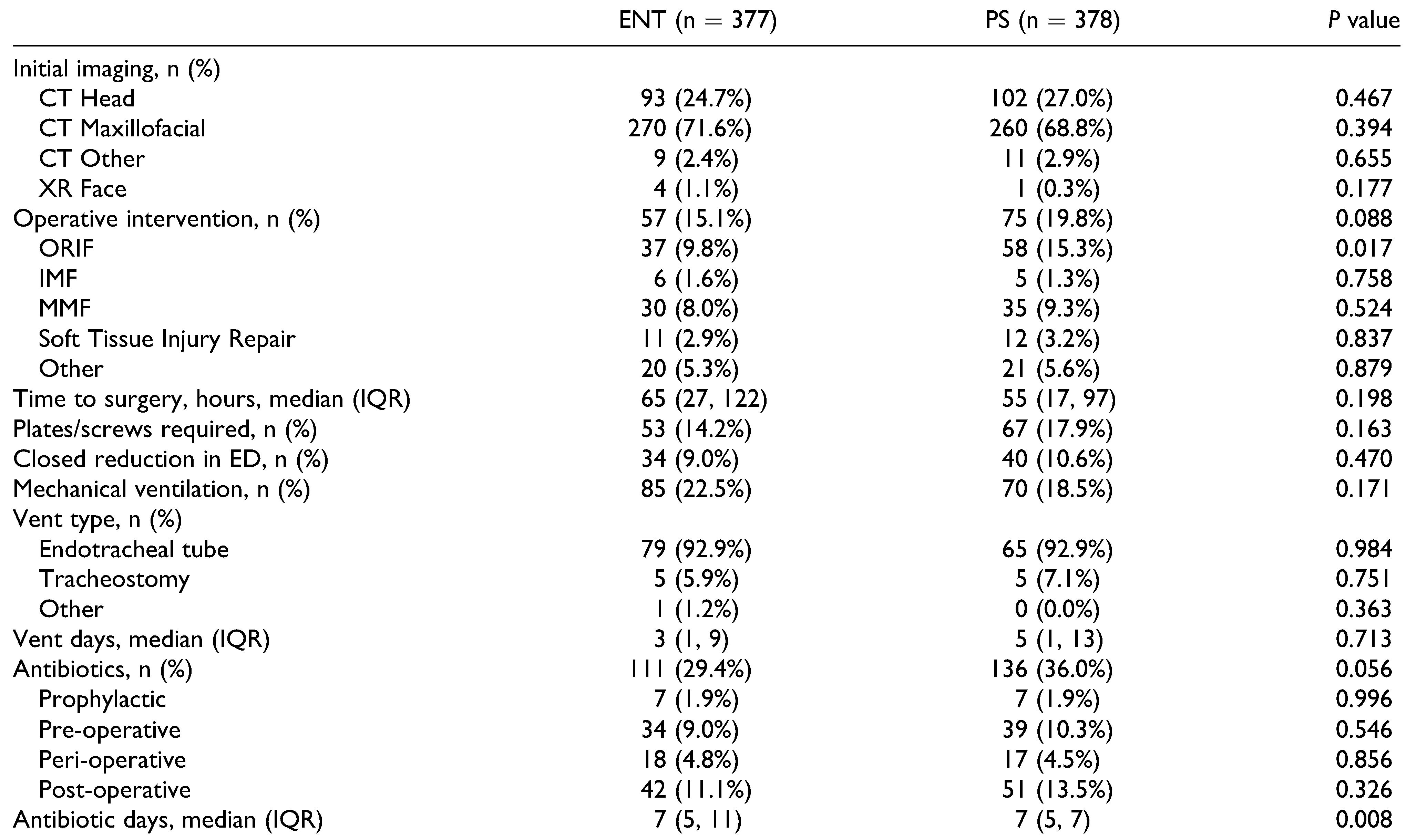
When comparing ENT patients to PS patients, there was no difference in the use of imaging modalities: CT head imaging (ENT: 24.7%, PS 27.0%, P = 0.467), CT maxillofacial imaging (ENT: 71.6%, PS: 68.8%, P = 0.394), head x-rays (ENT: 1.1%, 0.3%, P = 0.177). From an operative factors standpoint, both services had similar rates of overall operative intervention (ENT 15.1%, PS: 19.8%, P = 0.088), time to surgery (ENT: 65 hours, PS: 55 hours, P = 0.198), use of plates/screws (ENT: 14.2%, PS: 17.9%, P = 0.163), and closed reduction in the emergency department (ENT: 9.0%, PS: 10.6%, P = 0.470). ORIF was more commonly performed by PS compared to ENT (15.3% vs. 9.8%, P = 0.017) (Table 4).

Table 4.
Comparison of Facial Fracture Diagnosis and Management.
Antibiotics
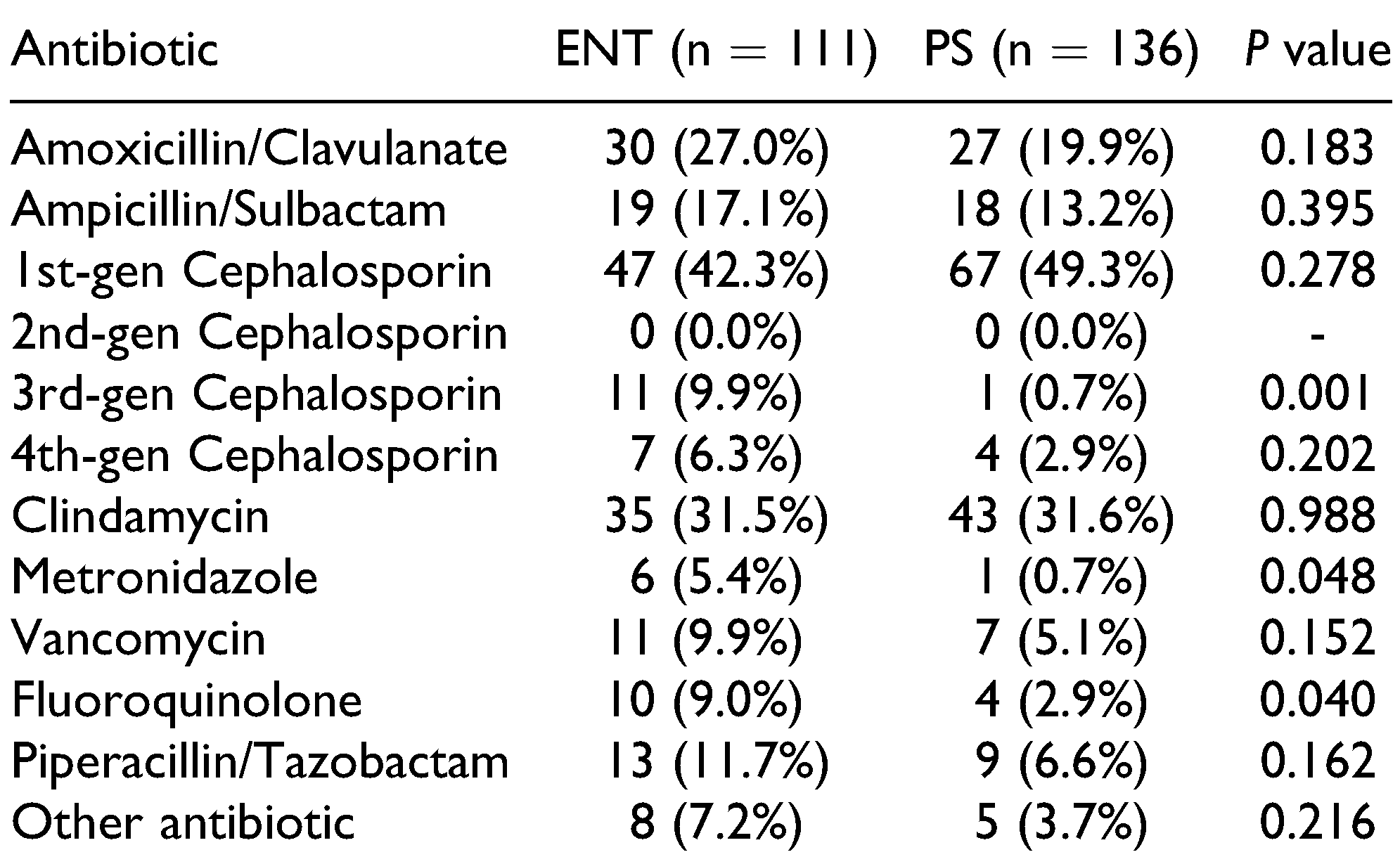
The 3 most common antibiotics used by both ENT and PS were 1st generation cephalosporins (ENT: 42.3%, PS: 49.3%), clindamycin (ENT: 31.5%, PS: 31.6%), and amoxicillin/ clavulanate (ENT: 27.0%, PS: 19.9%) (all P > 0.05). There were similar rates of patients treated with prophylactic (ENT: 1.9%, PS: 1.9%, P = 0.996), pre-operative (ENT: 9.0%, PS: 10.3%, P = 0.546), peri-operative (ENT: 4.8%, PS: 4.5%, P = 0.856) and post-operative (ENT: 11.1%, PS: 13.5%, P = 0.326) antibiotics. However, ENT patients were treated with a longer mean duration of antibiotics (9.4 vs 7.0 days, P = 0.008). ENT patients were more often treated with 3rd generation cephalosporins (9.9% vs 0.7%, P = 0.001) or fluoroquinolones (9.0% vs 2.9%, P = 0.040) compared to PS patients, but had similar rates of use for all other antibiotics (all P > 0.05) (Table 4 and Table 5) (Figure 1).

Table 5.
Antibiotics Prescribed for Facial Fractures by Otolaryngology and Plastic Surgery.
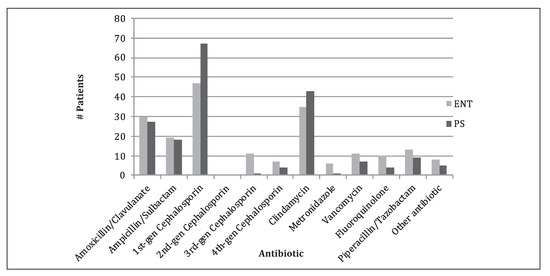
Figure 1.
Antibiotics prescribed by otolaryngology and plastic surgery. ENT = Otolaryngology consult, PS = Plastic Surgery consult, gen = generation.
Outcomes
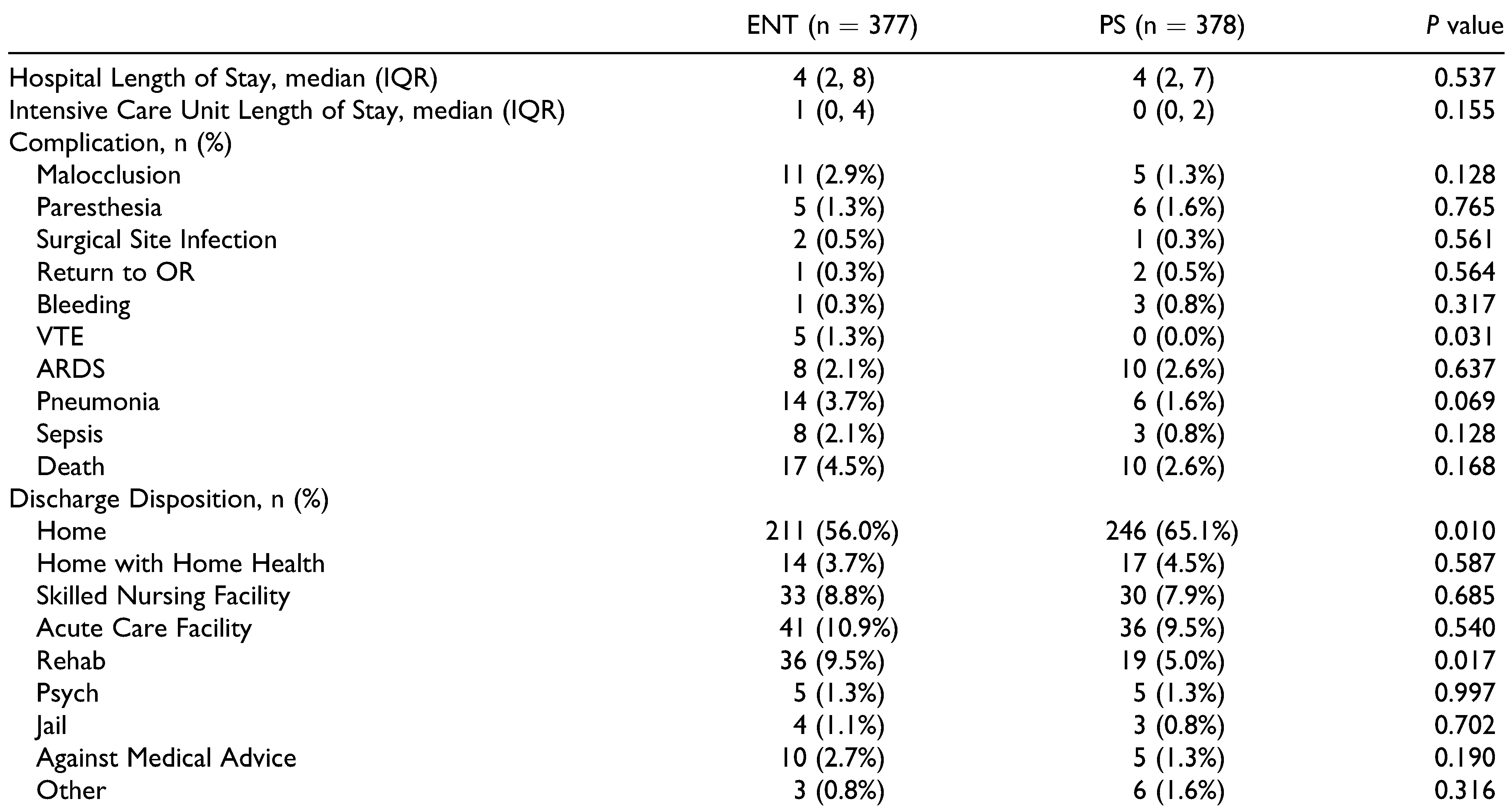
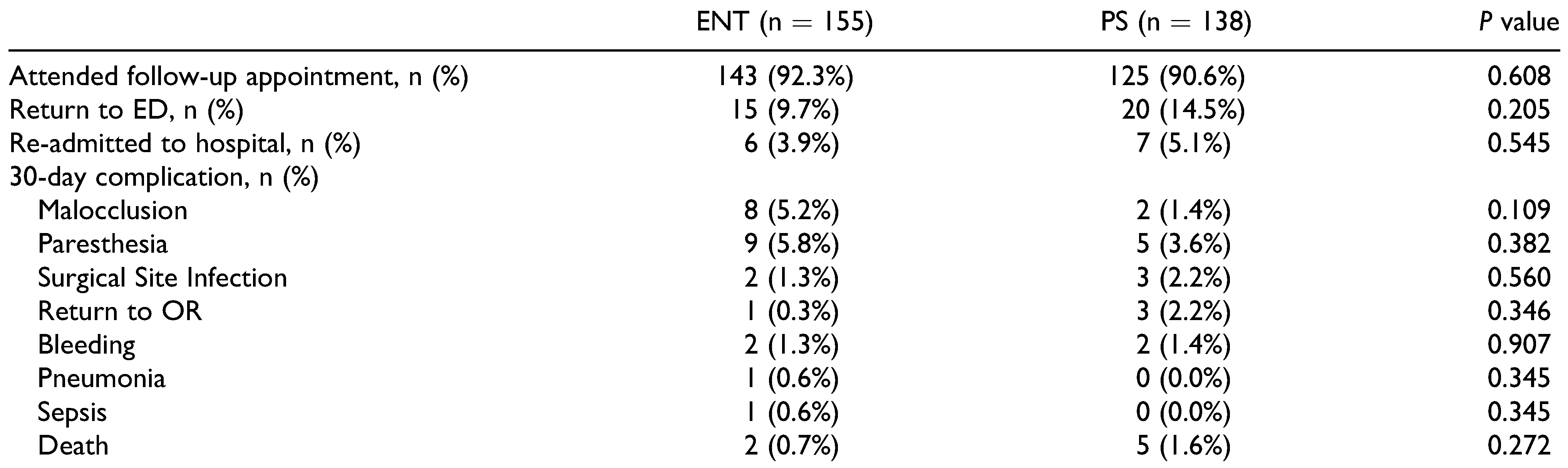
There was no difference between the 2 specialties with regard to hospital length of stay (ENT: 4 days, PS: 4 days, P = 0.537), intensive care unit length of stay (ENT: 1 day, PS: 0 days, P = 0.155) and ventilator days (ENT: 3, PS: 5, P = 0.713). Although ENT patients did sustain a higher rate of VTE (1.3% vs 0%, P = 0.031), there were no differences in the rates of FF-related complications: malocclusion (ENT: 2.9%, PS 1.3%, P = 0.128), facial paresthesia (ENT: 1.3%, PS: 1.6%, P = 0.765), SSI (ENT: 0.5%, PS: 0.3%, P = 0.561), return to the operating room (ENT: 0.3%, PS: 0.5%, P = 0.564), bleeding (ENT: 0.3%, PS: 0.8%, P = 0.317), or mortality (ENT: 4.5%, PS: 2.6, P = 0.168) (Table 6) (Figure 3). Regarding patient disposition, significantly more PS patients were discharged home (65.5% vs 56.0%, P = 0.010), while a greater proportion of ENT patients were discharged to rehab (9.5% vs 5.0%, P = 0.017) compared to PS patients (Table 6). 30- day follow-up data demonstrated no difference in the rate of patients who attended their follow-up appointment (ENT: 92.3%, PS: 90.6%, P = 0.608), patients returning to the ED (ENT: 9.7%, PS: 14.5%, P = 0.205), and patients readmitted to the hospital (ENT: 3.9%, PS: 5.1%, P = 0.545). In addition, there were no significant differences in any 30-day complications (all P > 0.05) (Table 7) (Figure 4).

Table 6.
Comparison of In-Hospital Outcomes.

Figure 3.
In-hospital complications for otolaryngology and plastic surgery. ENT = Otolaryngology consult, PS = Plastic Surgery consult, VTE = venous thromboembolism, ARDS = acute respiratory distress syndrome.

Table 7.
Comparison of 30-Day Follow-Up Outcomes.

Figure 4.
30-Day complications for otolaryngology and plastic surgery. ENT = Otolaryngology consult, PS = Plastic Surgery consult, OR = operating room.
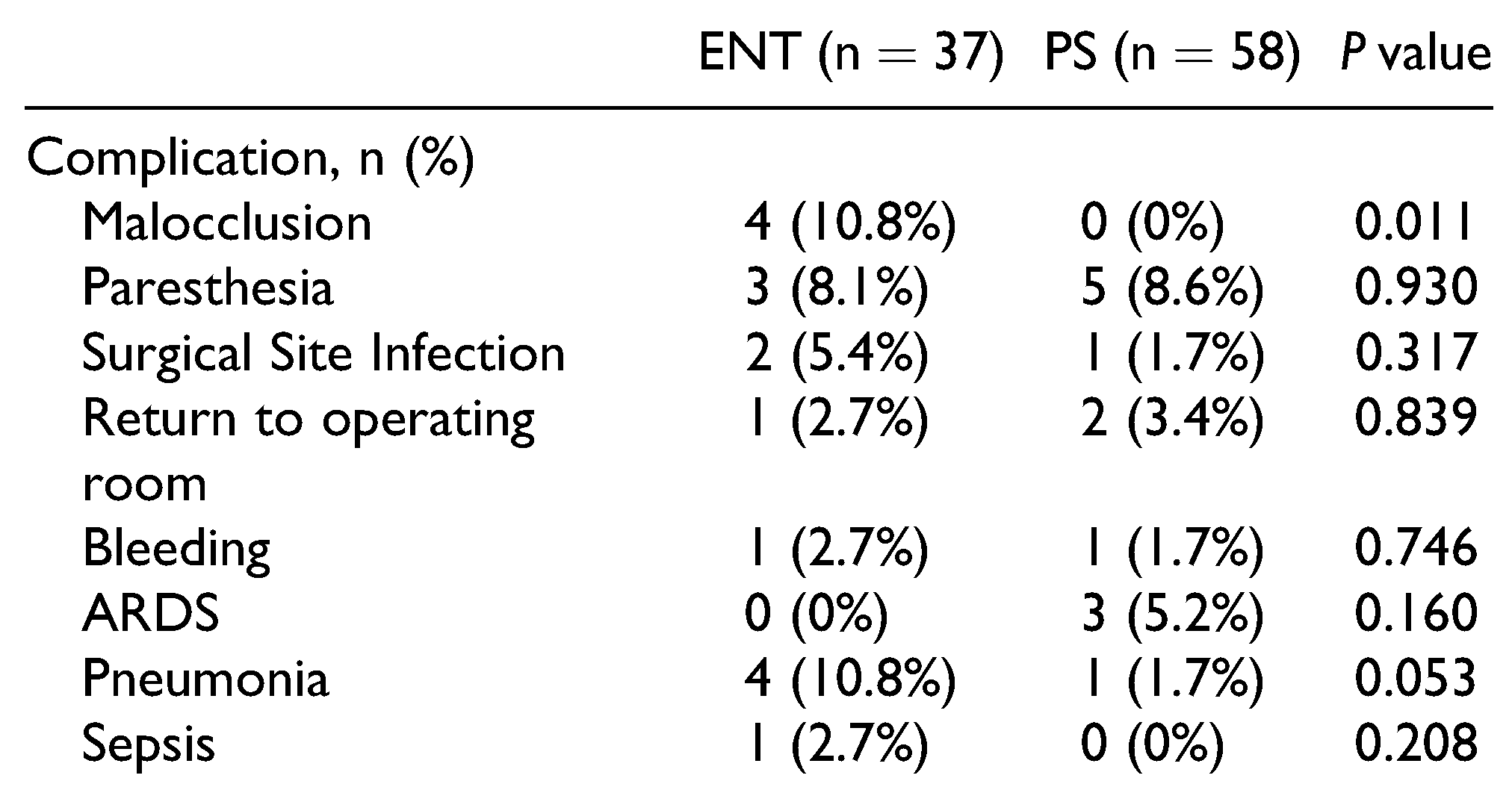
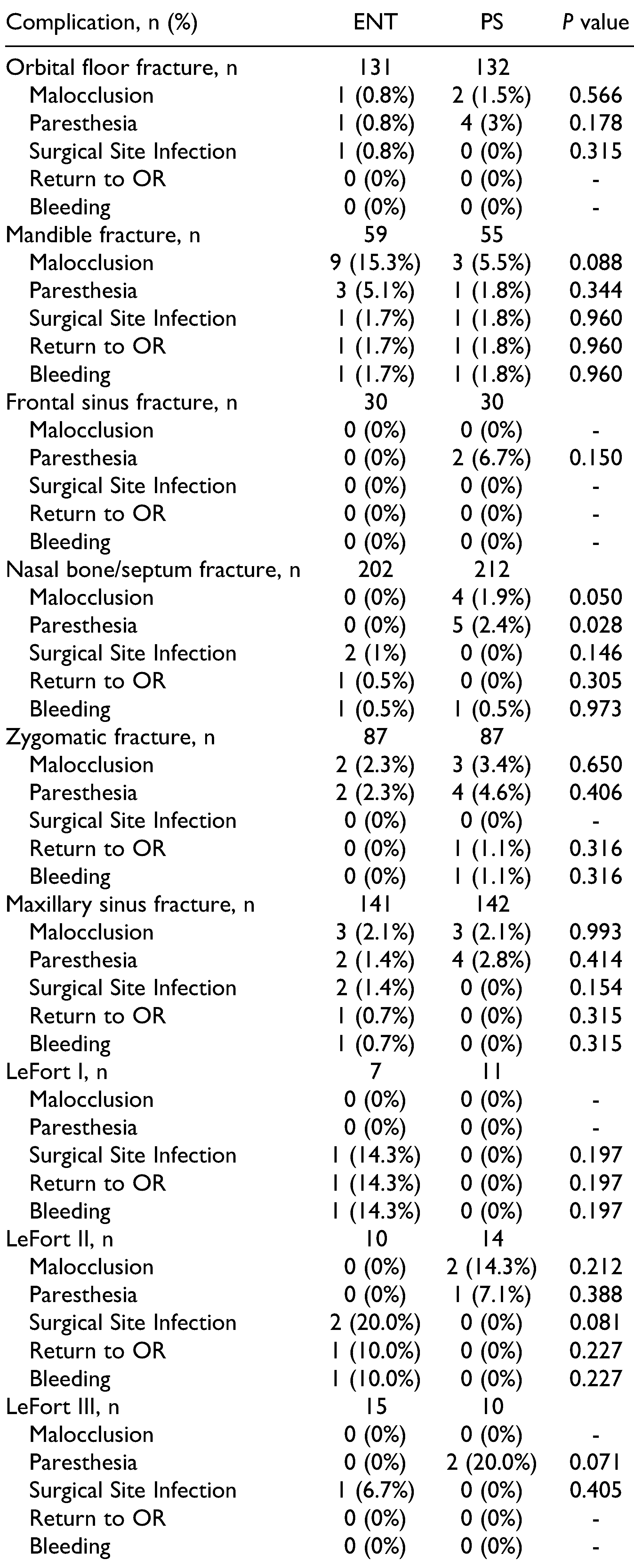
Upon performing subgroup analyses for in-hospital complications and fracture patterns, differences were observed between patients managed by ENT compared to PS. With regard to managing patients undergoing ORIF, ENT performed ORIF on 37 occasions and PS performed ORIF on 58 occasions. Comparing these 2 groups, there was a higher incidence of malocclusion in patients managed by ORIF performed by ENT than performed by PS (ENT 10.8%, PS: 0%, P = 0.011). No differences in the remaining in-hospital complications were observed between patients undergoing ORIF with ENT compared to PS (Table 8). In Table 9, a subgroup analysis contains complication rates across different fracture patterns as managed by ENT and PS. PS was found to have a higher rate of malocclusion when managing nasal bone/septum fractures (ENT: 0%, PS 1.9%, P = 0.050). However, across the remainder of defined fracture patterns and complications, no significant differences were observed when comparing patients managed by ENT versus PS (all P > 0.05).

Table 8.
Comparison of In-Hospital Outcomes for Patients Undergoing ORIF with Either ENT or PS.

Table 9.
Analysis of In-Hospital Complications Across Different Fracture Patterns When Managed by ENT or PS.
Discussion
Historically, traumatic FFs have been managed predominantly by 3 different specialties: PS, OMFS, and ENT.[3,4,5] In this single-center analysis spanning 4 years, we found largely no difference in patient demographics, operative factors, and outcomes between patients managed by ENT and those managed by PS. We did identify small differences in management such as more ORIFs performed by PS, a higher incidence of malocclusion in ORIFs performed by ENT and longer antibiotic regimens prescribed by ENT. However, despite differences in training background, our data showed far more similarities in management and outcomes between the 2 services. To our knowledge, this is the first paper to directly compare a wide spectrum of FF outcomes between these 2 specialties.
Standardization of care has previously been demonstrated to improve outcomes in many areas throughout surgery. [12,13,14] However, prior studies have also demonstrated differences in care based upon the particular specialty guiding the management of FFs.[6,7,9,10,11] Our single-center study found similar outcomes whether a patient was managed by ENT or PS. Both services had less than a 2% mortality rate with no significant difference in hospital length of stay, intensive care unit length of stay, or most complications. A particular difference observed in our data set involved PS performing ORIF more often than ENT, and noting that when patients underwent ORIF, their course was more likely to be complicated by malocclusion when performed by ENT. However, across most other measures there were no significant differences in outcomes between patients managed by ENT or PS. In support of this finding, Susarla et al compared subspecialty management of ZMC fractures, and concluded that it did not matter which subspecialty managed FFs, as long as the surgeon routinely managed such injuries.[4] At our institution, PS and ENT surgeons have varying levels of experience and training managing traumatic FFs, with only 1 attending in PS who underwent designated fellowship training in craniofacial surgery and 1 ENT surgeon who underwent fellowship training in facial plastic and reconstructive surgery. Having such fellowship training likely improves experience and may improve outcomes, and thus would be an interesting topic for future study. Despite similar outcomes, perceptions vary regarding which specialty should manage FFs. Le et al received survey responses from 41 Trauma and Emergency Medicine chiefs and found that they overwhelmingly preferred OMFS over ENT or PS when patients presented with isolated mandible fractures.8 However, these preferences were simply based upon perceptions of timeliness, efficiency and competency.8 While this study lacks generalizability, our data supports the need for a large multicenter study that also incorporates OMFS.
Trauma patients have previously been shown to have poor outpatient follow-up following injuries.[15] Therefore, many studies regarding FFs only report data from the index hospitalization, although in reality this may be inaccurate as many complications occur post-discharge. For instance, among patients with mandible fractures, 7% to 29% suffer complications, of which a majority of these complications are malocclusion and have delayed presentations.[16,17] Thus, our data, which demonstrated no difference in 30-day complications or re-admission between patients managed by either ENT or PS at our institution, further emboldens our perspective that management by either ENT or PS results in similar patient outcomes, and that we can reassure patients that they will receive similar care regardless of which specialty is managing their FFs.[4] The only exception being a difference in malocclusion when performing ORIF, which merits further study. To further apply the implications of our study, facial injury trauma call at Level I trauma centers can be quite burdensome. A survey of over 300 California Medical Association members reported by Rudkin et al, which included data from ENT, PS, and OMFS, found that 79% of on-call specialists reported significant difficulty obtaining payment for on-call services and 20% have stopped taking call altogether.[18] In addition, these consult services were far more difficult to reach on weekends and nights.[18] Thus, employing multidisciplinary teams to relieve this burden can help spread the load across multiple specialties and providers and promote collegiality, while maintaining equivalent outcomes.
One of the most debated practices involving FF management is the use of antibiotics, and it is also one area where our study noted minor differences between ENT and PS.[2,19,20,21] In our study, both ENT and PS most commonly prescribed a 1st generation cephalosporin, followed by clindamycin and then amoxicillin/clavulanate, which was very similar to findings by Brooke et al who also found that 1st generation cephalosporins were most commonly prescribed, followed by amoxicillin/clavulanate and clindamycin. [20] Though our 2 services provide similar antibiotic regimens as seen in the literature, ENT patients received an over 2 day longer mean course of antibiotics compared to PS patients. A review of 44 FF studies performed by Mundinger et al found that the average duration of antibiotics for FFs was between 3.7-4.6 days depending on the kind of FFs present.[19] Though some studies advocate 5- day courses of antibiotics, other authors suggest no benefit to an extended course of antibiotics and that antibiotics beyond 24 hours provide no significant benefit.[2,19,20,21] In fact, a meta-analysis of antibiotic prophylaxis for FFs managed by ORIF written by Delaplain et al demonstrated no improvement in SSI for any FFs receiving ORIF repair with prolonged antibiotic prophylaxis.[22] Thus, improved standardization of care and adherence to existing data recommendations may provide an opportunity for improved quality of care for all FF patients at our institution and potentially more nationwide.
As a retrospective single-institution study there are inherent limitations such as lack of generalizability and the limited documentation in the medical records. In addition, at our institution, 80% of FF patients were admitted to the trauma service with ENT/PS consultation, so it is not always clear who made major management decisions regarding imaging, timing of operation, and antibiotics, since patients could have many other traumatic injuries that could influence FF management. Similarly, we are unable to evaluate the rationale behind decision making such as the indication for prolonged antibiotics beyond what was documented in the chart. Although we provide basic information regarding operative interventions, details regarding patient decision-making for timing of operation (inpatient surgery vs conservative management vs outpatient surgery) and operative tact are missing within the electronic medical records. This study does not capture all patients presenting to the ED with FFs, but only those patients who were evaluated by the trauma team. Hence it represents patients with higher injury burden and/or stronger mechanisms of injury. Though we were able to evaluate 30-day outcomes, we were unable to evaluate complications that would be observed after a longer time period. Finally, since our hospital does not have an inpatient OMFS service, a significant limitation is that we are unable to compare outcomes between the 3 services that most commonly manage traumatic FFs. [3,4,5]
Conclusion
This single-center analysis spanning 4 years of data found similar baseline characteristics, overall operative rate, timing of operations, complication rate, and mortality between trauma patients with FFs managed by ENT and PS. The most notable difference is the increased number of malocclusions occurring when patients are managed by ORIF with ENT. We also noted a 2-day increased mean duration of antibiotics for the ENT cohort, although both services appeared to have prolonged antibiotic usage compared to the literature, identifying an area for continued improvement. Overall, this study supports the practice of allowing both ENT and PS to care for trauma patients with FFs, as there appears to be similar standardized care and outcomes. It also raises the question regarding the optimal use and timing of antibiotic regimens in the treatment of traumatic FFs. Future studies are needed to evaluate the generalizability of our findings and to determine whether any differences in outcomes with patients managed by OMFS exist.
Author Contributions
All authors made substantial contributions to this study. Data collection was performed by Beatrice Sun, Nima Khoshab, Christina Cantwell, Sean Melucci, and Allison Hu. Areg Grigorian performed the data analysis. The first draft of the manuscript was written by Ashton Christian and critical revisions were made by Jeffry Nahmias, Catherine Kuza, Areg Grigorian, and Michael Lekawa. All authors read and approved the final manuscript.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Institutional Review Board Statement
This study was approved by the Institutional Review Board at the University of California, Irvine.
Code Availability
All analyses were performed with IBM SPSS Statistics for Windows (Version 24, IBM Corp., Armonk, NY).
Data Availability Statement
Data acquired from a single, Level 1 trauma center.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Allareddy, V.; Allareddy, V.; Nalliah, R.P. Epidemiology of facial fracture injuries. J Oral Maxillofac Surg. 2011, 69, 2613–2618. [Google Scholar] [CrossRef]
- Chukwulebe, S.; Hogrefe, C. The diagnosis and management of facial bone fractures. Emerg Med Clin North Am. 2019, 37, 137–151. [Google Scholar] [CrossRef] [PubMed]
- Baylan, J.M.; Jupiter, D.; Parker, W.L.; Czerwinski, M. Management of zygomatic fractures: a national survey. J Craniofac Surg. 2016, 27, 1571–1575. [Google Scholar] [CrossRef] [PubMed]
- Susarla, S.M.; Mundinger, G.S.; O’Brien-Coon, D.; et al. Does training background influence decision-making in the management of zygomaticomaxillary complex fractures? J Oral Maxillofac Surg. 2016, 74, 995–1012. [Google Scholar] [CrossRef]
- Bagheri, S.C.; Dimassi, M.; Shahriari, A.; Khan, H.A.; Jo, C.; Steed, M.B. Facial trauma coverage among level-1 trauma centers of the United States. J Oral Maxillofac Surg. 2008, 66, 963–967. [Google Scholar] [CrossRef]
- Choi, K.J.; Chang, B.; Woodard, C.R.; Powers, D.B.; Marcus, J.R.; Puscas, L. Survey of current practice patterns in the management of frontal sinus fractures. Craniomaxillofac Trauma Reconstr. 2017, 10, 106–116. [Google Scholar] [CrossRef]
- Cohen, L.M.; Shaye, D.A.; Yoon, M.K. Isolated orbital floor fracture management: a survey and comparison of American oculofacial and facial plastic surgeon preferences. Craniomaxillofac Trauma Reconstr. 2019, 12, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Le, B.T.; Holmgren, E.P.; Holmes, J.D.; Ueeck, B.A.; Dierks, E.J. Referral patterns for the treatment of facial trauma in teaching hospitals in the United States. J Oral Maxillofac Surg. 2003, 61, 557–560. [Google Scholar] [CrossRef]
- Farber, S.J.; Nguyen, D.C.; Skolnick, G.B.; Woo, A.S.; Patel, K.B. Current management of zygomaticomaxillary complex fractures: a multidisciplinary survey and literature review. Craniomaxillofac Trauma Reconstr. 2016, 9, 313–322. [Google Scholar] [CrossRef]
- Kim, I.A.; Boahene, K.D.; Byrne, P.J. Trauma in facial plastic surgery: frontal sinus fractures. Facial Plast Surg Clin North Am. 2017, 25, 503–511. [Google Scholar] [CrossRef]
- Marinheiro, B.H.; de Medeiros, E.H.; Sverzut, C.E.; Trivellato, A.E. Frontal bone fractures. J Craniofac Surg. 2014, 25, 2139–2143. [Google Scholar] [CrossRef] [PubMed]
- Gomi, H.; Solomkin, J.S.; Schlossberg, D.; et al. Tokyo Guidelines 2018: antimicrobial therapy for acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2018, 25, 3–16. [Google Scholar] [CrossRef]
- Gúerin, C.; Reignier, J.; Richard, J.C.; et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013, 368, 2159–2168. [Google Scholar] [PubMed]
- Ko, A.; Harada, M.Y.; Barmparas, G.; et al. Association between enoxaparin dosage adjusted by anti-factor Xa trough level and clinically evident venous thromboembolism after trauma. JAMA Surg. 2016, 151, 1006–1013. [Google Scholar] [PubMed]
- Rosenberg, G.M.; Shearer, E.J.; Zion, S.R.; et al. Implementation challenges using a novel method for collecting patientreported outcomes after injury. J Surg Res. 2019, 241, 277–284. [Google Scholar] [CrossRef]
- Boljevic, T.; Vukcevic, B.; Pesic, Z.; Boljevic, A. The quality of life of patients with surgically treated mandibular fractures and the relationship of the posttraumatic pain and trismus with the postoperative complications: a prospective study. Medicina (Kaunas). 2019, 55, E109. [Google Scholar]
- Pickrell, B.B.; Hollier, L.H., Jr. Evidence-based medicine: mandible fractures. Plast Reconstr Surg. 2017, 140, 192e–200e. [Google Scholar] [CrossRef]
- Rudkin, S.E.; Oman, J.; Langdorf, M.I.; et al. The state of ED on-call coverage in California. Am J Emerg Med. 2004, 22, 575–581. [Google Scholar]
- Mundinger, G.S.; Borsuk, D.E.; Okhah, Z.; et al. Antibiotics and facial fractures: evidence-based recommendations compared with experience-based practice. Craniomaxillofac Trauma Reconstr. 2015, 8, 64–78. [Google Scholar]
- Brooke, S.M.; Goyal, N.; Michelotti, B.F.; et al. A Multidisciplinary evaluation of prescribing practices for prophylactic antibiotics in operative and nonoperative facial fractures. J Craniofac Surg. 2015, 26, 2299–2303. [Google Scholar]
- Dougherty, W.M.; Christophel, J.J.; Park, S.S. Evidence-based medicine in facial trauma. Facial Plast Surg Clin North Am. 2017, 25, 629–643. [Google Scholar] [PubMed]
- Delaplain, P.T.; Phillips, J.L.; Lundeberg, M.; et al. No reduction in surgical site infection obtained with post-operative antibiotics in facial fractures, regardless of duration or anatomic location: a systematic review and meta-analysis. Surg Infect (Larchmt). 2019, 21, 112–121. [Google Scholar] [PubMed]
© 2021 by the author. The Author(s) 2021.