“6 Anatomical Landmarks” Technique for Satisfactory Free-Hand Orbital Reconstruction with Standard Preformed Titanium Mesh
Abstract
:Introduction
Materials and Methods
- ⁻ unilateral orbital fracture ≥2 cm2 involving orbital floor, with or without medial wall fracture;
- ⁻ primary reconstruction using standard preformed titanium meshes;
- ⁻ availability of full clinical documentation, with pre- and post-operative high-quality CT scans (slices thickness ≤1 mm) with coronal, sagittal and 3D reconstructions;
- ⁻ follow-up of at least 12 months. Exclusion’s criteria were:
- ⁻ craniofacial malformation, especially those with orbital asymmetries;
- ⁻ history of previous orbital trauma or surgery;
- ⁻ pre-existing ocular functional defects;
- ⁻ bilateral orbital walls fractures;
- ⁻ reconstruction performed with other solutions (resorbable plates, traditional non-preformed tita- nium plates, Patient Specific Implant or reposition- ing of bony wall fragments);
- ⁻ incomplete pre- and post-operative clinical and radi- ological documentation;
- ⁻ less than 12 months of follow-up.
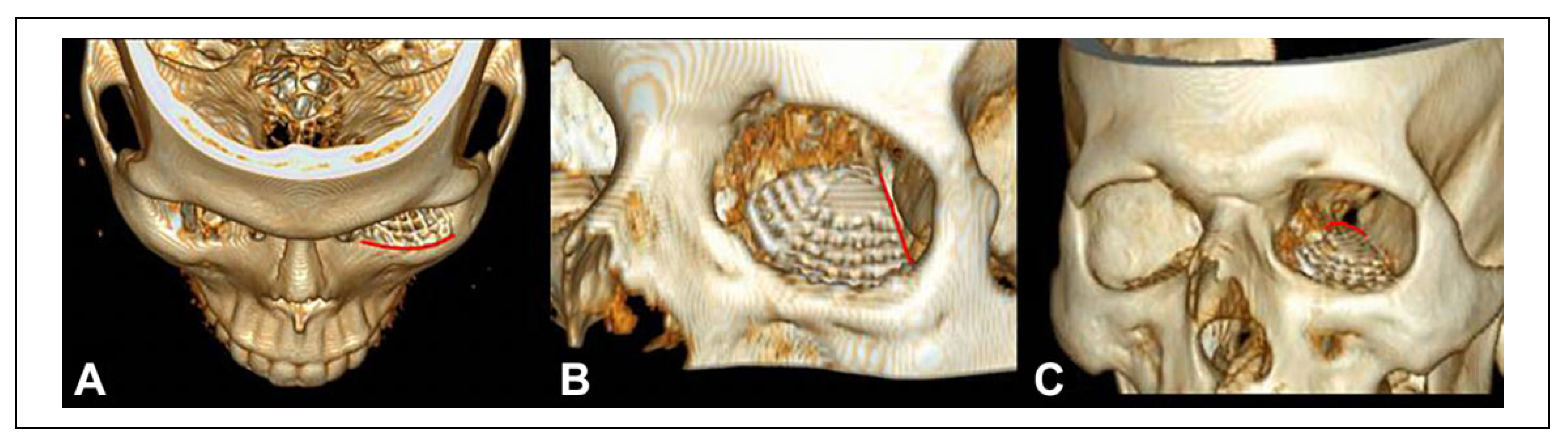
- The inferior orbital rim, which must correspond with the position of the screw holes of the mesh (Figure 1A).
- The inferior orbital fissure, which determines the position of the lateral edge of the mesh (Figure 1B).
- The orbital process of the palatine bone, known as “posterior bony ledge,” as the support structure for the apex of the mesh (Figure 1C).
- 1.
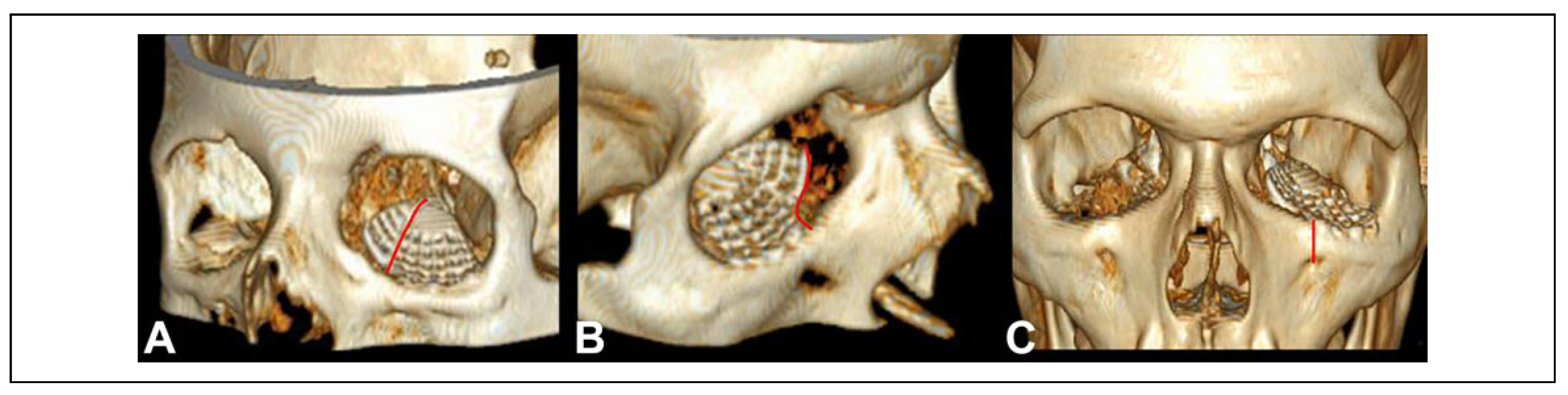
- The transition zone represented by the inferome- dial bony strut, for the position of the inferomedial part of the mesh (Figure 2A).
- 2.
- The lacrimal sac, the posterior lacrimal crest and the origin of the inferior oblique muscle, for the posi- tion of the antero-medial notch of the mesh (Figure 2B).
- x
- The emergence of the infraorbital nerve, which has to be vertically aligned with the first medial screw hole (Figure 2C).
- 1.
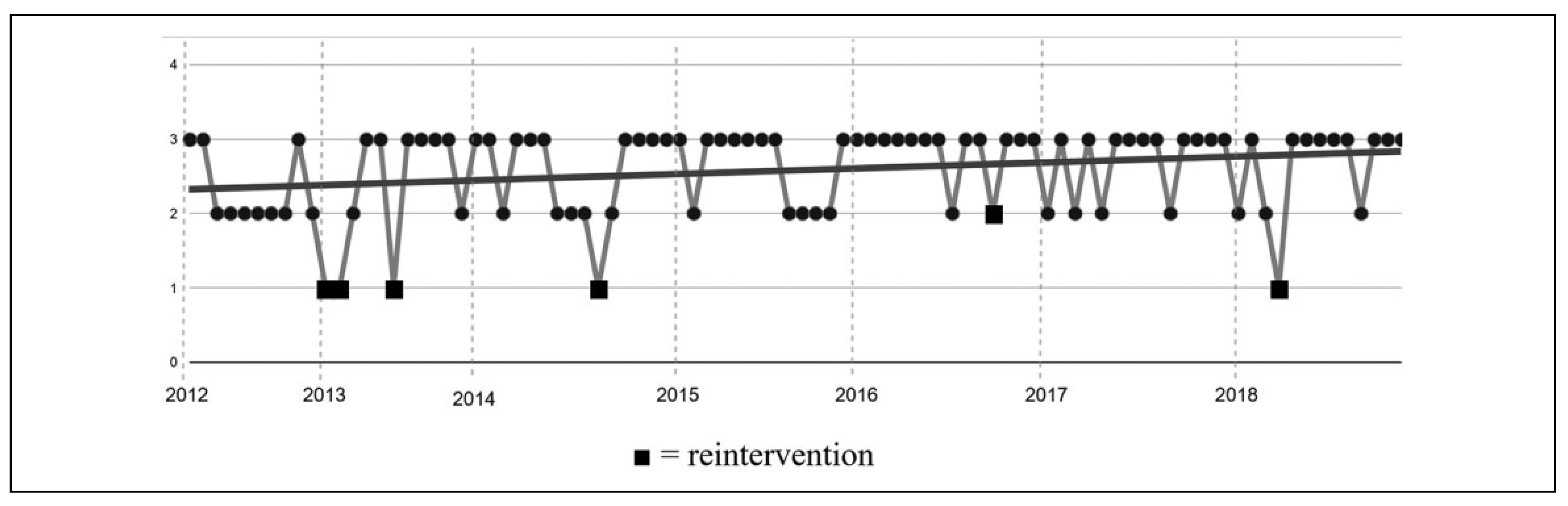
- ¼ Not accurate radiological result (grossly mesh malposition).
- 2.
- ¼Partial accurate radiological result (discrepancy >1 mm compared to controlateral mirrored orbit and/or adherence to less than 6/6 anatomical markers).
- 3.
- ¼ Accurate radiological result (good adherence to controlateral mirrored orbit and/or total adherence to the anatomical markers).
Results
Conclusion
Funding
Conflicts of Interest
References
- Ellis E, III, el-Attar A, Moos KF. An analysis of 2,067 cases of zygomatico-orbital fracture. J Oral Maxillofac Surg, 4: 43(6). [CrossRef]
- Bittermann G, Metzger MC, Schlager S, et al. Orbital recon- struction: prefabricated implants, data transfer, and revision surgery. Facial Plast Surg. [CrossRef] [PubMed]
- Gander T, Essig H, Metzler P, et al. Patient specific implants (PSI) in reconstruction of orbital floor and wall fractures. J Craniomaxillofac Surg. [CrossRef]
- Zavattero E, Ramieri G, Roccia F, Gerbino G.Comparison of the outcomes of complex orbital fracture repair with and without a surgical navigation system: a prospective cohort study with historical controls. Plast Reconstr Surg, 9: 139(4). [CrossRef]
- Sozzi D, Gibelli D, Canzi G, et al. Assessing the precision of posttraumatic orbital reconstruction through “mirror” orbital superimposition: a novel approach for testing the anatomical accuracy. J Craniomaxillofac Surg, 1258. [CrossRef]
- Dubois L, Steenen SA, Gooris PJ, Bos RR, Becking AG. Controversies in orbital reconstruction-III. Biomaterials for orbital reconstruction: a review with clinical recommenda- tions. Int J Oral Maxillofac Surg. [CrossRef]
- Schramm A, Suarez-Cunqueiro MM, Ru¨ cker M, et al. Computer-assisted therapy in orbital and mid-facial recon- structions. Int J Med Robot. [CrossRef]
- Schlittler F, Schmidli A, Wagner F, Michel C, Mottini M, Lieger O. What is the incidence of implant malpositioning and revision surgery after orbital repair? J Oral Maxillofac Surg. [CrossRef]
- Zimmerer RM, Ellis E, 3rd, Aniceto GS, et al. A prospective multicenter study to compare the precision of posttraumatic internal orbital reconstruction with standard preformed and individualized orbital implants. J Craniomaxillofac Surg, 1485. [CrossRef]
- Rana M, Chui CH, Wagner M, Zimmerer R, Rana M, Gellrich NC. Increasing the accuracy of orbital reconstruction with selective laser-melted patient-specific implants combined with intraoperative navigation. J Oral Maxillofac Surg, 1113. [CrossRef] [PubMed]
- Kim YC, Jeong WS, Park TK, Choi JW, Koh KS, Oh TS. The accuracy of patient specific implant prebented with 3D- printed rapid prototype model for orbital wall reconstruction. J Craniomaxillofac Surg. [CrossRef]
- Huempfner-Hierl H, Doerfler HM, Kruber D, Hierl T. Mor- phologic comparison of preformed orbital meshes. J Oral Maxillofac Surg, 1119. [CrossRef]
- Bourry M, Hardouin JB, Fauvel F, Corre P, Lebranchu P, Bertin H.Clinical evaluation of the efficacy of materials used for primary reconstruction of orbital floor defects: meta- analysis [published online ahead of print, 2020 Nov 4]. Head Neck. [CrossRef]
- Scolozzi P, Momjian A, Heuberger J, et al. Accuracy and predictability in use of AO three-dimensionally preformed titanium mesh plates for posttraumatic orbital reconstruction: a pilot study. J Craniofac Surg, 1108. [CrossRef] [PubMed]
- Potter JK, Malmquist M, Ellis E, 3rd. Biomaterials for recon- struction of the internal orbit. Oral Maxillofac Surg Clin North Am. [CrossRef]
- Peng MY, Merbs SL, Grant MP, Mahoney NR. Orbital frac- ture repair outcomes with preformed titanium mesh implants and comparison to porous polyethylene coated titanium sheets. J Craniomaxillofac Surg. [CrossRef] [PubMed]
- Strong EB, Fuller SC, Wiley DF, Zumbansen J, Wilson MD, Metzger MC. Preformed vs intraoperative bending of titanium mesh for orbital reconstruction. Otolaryngol Head Neck Surg. [CrossRef]
- Purnell CA, Vaca EE, Ellis MF. Orbital fracture reconstruc- tion using prebent, anatomic titanium plates: technical tips to avoid complications. J Craniofac Surg. [CrossRef]
- Canzi G, De Ponti E, Novelli G, et al. The CFI score: valida- tion of a new comprehensive severity scoring system for facial injuries. J Craniomaxillofac Surg. [CrossRef]
- Novelli G, Ferrari L, Sozzi D, Mazzoleni F, Bozzetti A. Transconjunctival approach in orbital traumatology: a review of 56 cases. J Craniomaxillofac Surg. [CrossRef]
- Ellis E 3rd, Tan Y. Assessment of internal orbital reconstruc- tions for pure blowout fractures: cranial bone grafts versus titanium mesh. J Oral Maxillofac Surg. [CrossRef] [PubMed]
- Schlittler F, Vig N, Burkhard JP, Lieger O, Michel C, Holmes, S. What are the limitations of the non-patient-specific implant in titanium reconstruction of the orbit? Br J Oral Maxillofac Surg. [CrossRef]
- Shaye DA, Tollefson TT, Strong EB. Use of intraoperative computed tomography for maxillofacial reconstructive sur- gery. JAMA Facial Plast Surg. [CrossRef]
- Canzi G, De Ponti E, Fossati C, et al. Understanding the relevance of comprehensive facial injury (CFI) score: statis- tical analysis of overall surgical time and length of stay out- comes. J Craniomaxillofac Surg, 1456. [CrossRef]
- Reich W, Seidel D, Bredehorn-Mayr T, Eckert AW. Recon- struction of isolated orbital floor fractures with a prefabri- cated titanium mesh. Klin Monbl Augenheilkd. [CrossRef]
| Type of fracture | Number of fractures | % |
| A. Orbital floor | 45 | 50% |
| B. Orbital floor + medial wall | 9 | 10% |
| C. Orbito-zygomatic (CFI = 9) | 17 | 19% |
| D. Orbito-zygomatic (CFI = 9) + medial wall | 5 | 6% |
| E. Orbito-zygomatic (CFI >9) | 12 | 13% |
| F. Orbito-zygomatic (CFI >9) + medial wall | 2 | 2% |
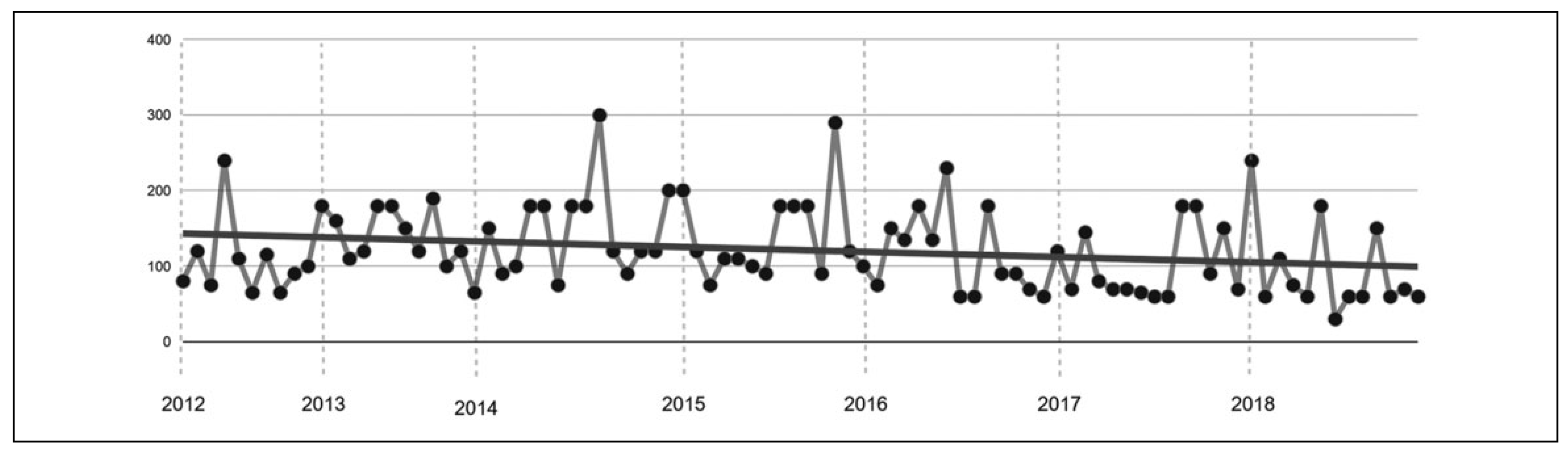
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
| Mean accuracy (SD) | 2.30 (0.48) | 2.27 (0.90) | 2.53 (0.64) | 2.62 (0.51) | 2.80 (0.41) | 2.71 (0.47) | 2.67 (0.65) |
| Surgical revisions | 0 | 3 | 1 | 0 | 1 | 0 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Canzi, G.; Corradi, F.; Novelli, G.; Bozzetti, A.; Sozzi, D. “6 Anatomical Landmarks” Technique for Satisfactory Free-Hand Orbital Reconstruction with Standard Preformed Titanium Mesh. Craniomaxillofac. Trauma Reconstr. 2022, 15, 51-57. https://doi.org/10.1177/19433875211007614
Canzi G, Corradi F, Novelli G, Bozzetti A, Sozzi D. “6 Anatomical Landmarks” Technique for Satisfactory Free-Hand Orbital Reconstruction with Standard Preformed Titanium Mesh. Craniomaxillofacial Trauma & Reconstruction. 2022; 15(1):51-57. https://doi.org/10.1177/19433875211007614
Chicago/Turabian StyleCanzi, Gabriele, Federica Corradi, Giorgio Novelli, Alberto Bozzetti, and Davide Sozzi. 2022. "“6 Anatomical Landmarks” Technique for Satisfactory Free-Hand Orbital Reconstruction with Standard Preformed Titanium Mesh" Craniomaxillofacial Trauma & Reconstruction 15, no. 1: 51-57. https://doi.org/10.1177/19433875211007614
APA StyleCanzi, G., Corradi, F., Novelli, G., Bozzetti, A., & Sozzi, D. (2022). “6 Anatomical Landmarks” Technique for Satisfactory Free-Hand Orbital Reconstruction with Standard Preformed Titanium Mesh. Craniomaxillofacial Trauma & Reconstruction, 15(1), 51-57. https://doi.org/10.1177/19433875211007614



