On the 31st of December 2019, Wuhan Municipal Health Commission, Hubei province, China reported a series of cases of pneumonia caused by coronavirus [
1]; the World Health Organization classified COVID-19 as a pandemic on the 11th of March 2020.[
2]
Oral and Maxillofacial Surgery in the United Kingdom
OMFS is the smallest surgical specialty within the UK employing approximately 500 consultants within the NHS. Traditionally single units operated independently providing a breadth of treatments. A drive to centralize services started with reducing the number of units performing surgical oncology with the aim of improving surgical outcomes.[
3] This was further reinforced by Getting it Right First Time (GIRFT) OMFS Speciality Report 2018 [
4] which aimed to provide consultant led facial trauma services and European Working Time Directive compliant rotas for junior doctors/dentists. One model recommended by GIRFT was the hub and spoke model. This model allows for a central hub to co-ordinate patient care and assets reducing the duplication of physical and staffing resources; see
Figure 1.
The Oxford Hub and Spoke
In line with recommendations from GIRFT 2018, the Oxford network operates as a hub and spoke model. Oxford University Hospitals (OUH) NHS Foundation Trust operates as the central hub in the Thames Valley region. Within the OUH there are 3 OMFS sites: the John Radcliffe Hospital (JR) the Churchill Hospital (CH) in Oxford and the Horton Hospital (HH) in Banbury. Surgical oncology is based at the CH with MDTs, head and neck clinics and 3 operating days per week for OMFS. All non-oncology services including emergency work is located at the JR with daily clinics, MDTS and 6 all day operating lists and additional peripheral clinics and day case procedures at the HH once weekly.
The spoke units within the network are (
Figure 2):
- -
Stoke Mandeville Hospital, Aylesbury, Buckinghamshire Healthcare
- -
Royal Berkshire Hospital, Reading, Royal Berkshire NHS Foundation Trust
- -
Great Western Hospital, Swindon, Great Western Hospitals NHS Foundation Trust
OMFS consultants are Oxford based and cover nominated spoke hospitals. The OUH OMFS hub and spoke serves a population of approximately 1.8 million people and the extended craniofacial trauma catchment of approximately 2.5 million people.
The John Radcliffe is a level 1 Major Trauma Centre for adult and pediatric patients. The catchment area extends to overlap with other OMFS units such as Northampton General Hospital, Milton Keynes University Hospital and Wexham Park Hospital for craniofacial trauma. All inpatient operating is conducted within the JR and CH sites with the spokes providing outpatient clinics, diagnostics and day case operating capacity. There is a formalized regional cancer MDT and an informal regional orthognathic network that includes consultant orthodontists who work in the spoke hospitals.
On call provision at the spoke hospitals is provided between 0900-1700 by on call non training grade colleagues and an OMFS consultant. If the patient requires admission they are referred to the JR. The JR provides 24-hour on call cover with a FY2 (Foundation Year 2: a singly qualified medical doctor in their second year after graduation) doctor acting first on, Specialist Training Registrar (StR: a dual qualified trainee in higher surgical training prior to OMFS consultancy) as second on call and an OMFS consultant of the week as third on call. Out of hours referrals from the spokes are seen at the JR as clinically necessary or arrangements are made for the patient to be seen at the spoke hospital the next working day if appropriate.
The Oxford Response
On March 16th, 2020, all OUH employees received an update from the Chief Executive, within this email they detailed that all inpatient elective operating was to cease; this was further updated on March 18th, 2020, all elective operating to stop. All outpatient clinics were to be delayed with the potential for provision of telephone/video clinics; cancer services were to remain as normal. Following a consultant meeting on March 17th, 2020, daily video conferencing was conducted to keep the OMFS team up to date with the latest developments.
The JR site is split into 2 interlinked large buildings the main JR building and the West Wing. The West Wing hosts OMFS inpatients and accepts emergency referrals which for adults are seen for assessment on a GP Referral Unit (GPRU) and for pediatric patients on a childrens’ daycare unit (CDU). The main JR building was the designated COVID positive site. OMFS FY2 doctors were redeployed to cover Trauma and Vascular inpatients. Therefore, there were not enough juniors to cover the first on-call rota; the StRs covered first on-call out of hours with resident on-call 24 hour shifts.
A daily consultant delivered emergency clinic was established. The CH oncology site, aimed to be a COVID free site, the service had reduced operating capacity but continued to run the service with oncology consultants freed from emergency work to flexibly take up these lists. The emergency operating and COVID tracheostomy service was provided by non-oncologists.
Aims
The aim of this study was to analyze the presentations to the OMFS hub in Oxford from March 16th, 2020, when all inpatient elective operating ceased, compared to the same period of time the previous year.
Methods
This is a single OMFS hub and spoke study. All patients who required emergency review and/or admission during a 10-week period (16th of March 2020-18th of March 2020) from the local announcement of ceasing elective operating were included. The data was collected prospectively and stored on a central database. Data from the same time period in 2019 was collected retrospectively from inpatient and emergency review data. Data listed from 2020 will be labeled as “COVID” and data from 2019 as “non-COVID.” To compare the data Fisher’s exact p = 0.05 was used to deem statistical significance.
Results
Emergency Inpatient Admissions
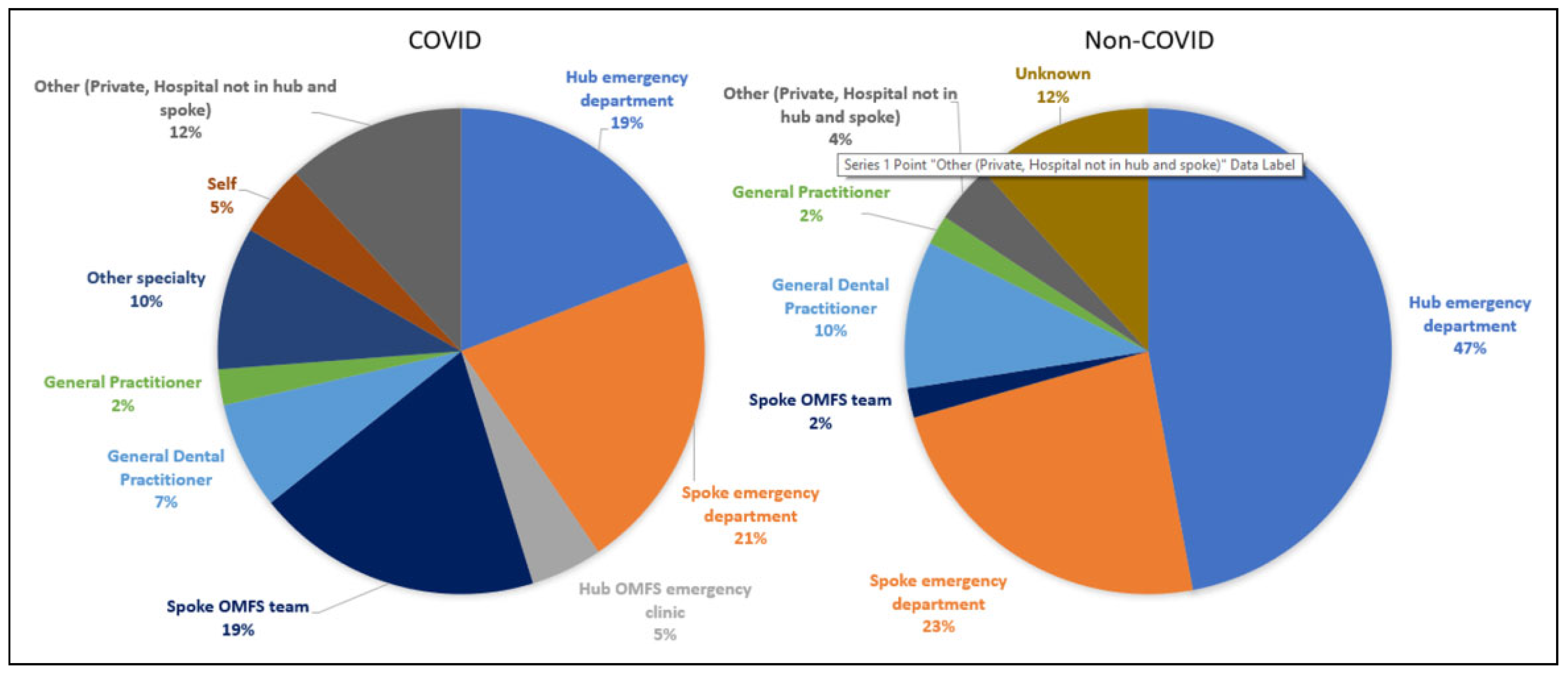
A total of 42 patients (average age 42; range 1-80 (
Figure 3)) were admitted in the 10-week time period during COVID in the 2020 period compared to 51 (average age 37; range 8-87) in 2019. The average length of stay was 1.7 (median 1.5, range 0.5-4.5) days during COVID and 2.4 (median 2, range 0.5-3.5) days. Of all the patients admitted 31 had an unknown diagnosis of COVID due to a lack of testing at the time, 10 swabbed negative and 1 patient was suspected but swabbed negative.
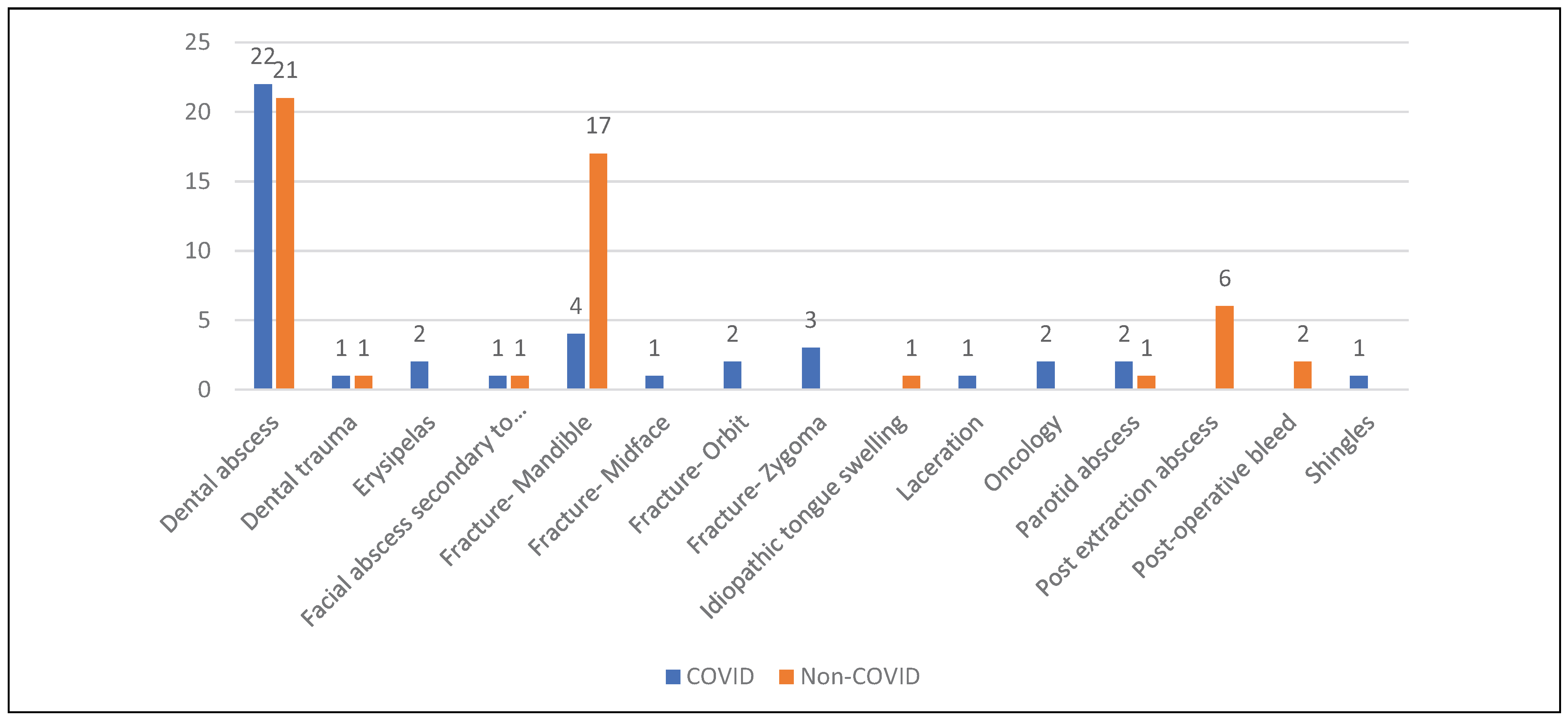
The OUH unit admitted statistically significant less mandibles (
Figure 4), p = 0.0067 during COVID. There was no statistical significance between the number of dental abscesses admitted between the 2 time periods.
On March 15th, 2020 the British Association of Oral and Maxillofacial Surgeons released guidance on personal protective equipment (PPE) that coincided with local OMFS policy released on the same date. After this date, every case had the appropriate level of PPE; OUH NHS FT was fortunate to not experience any shortage throughout the pandemic. There was access to a daily emergency OMFS operating list staffed by the consultant who would normally operate that day.
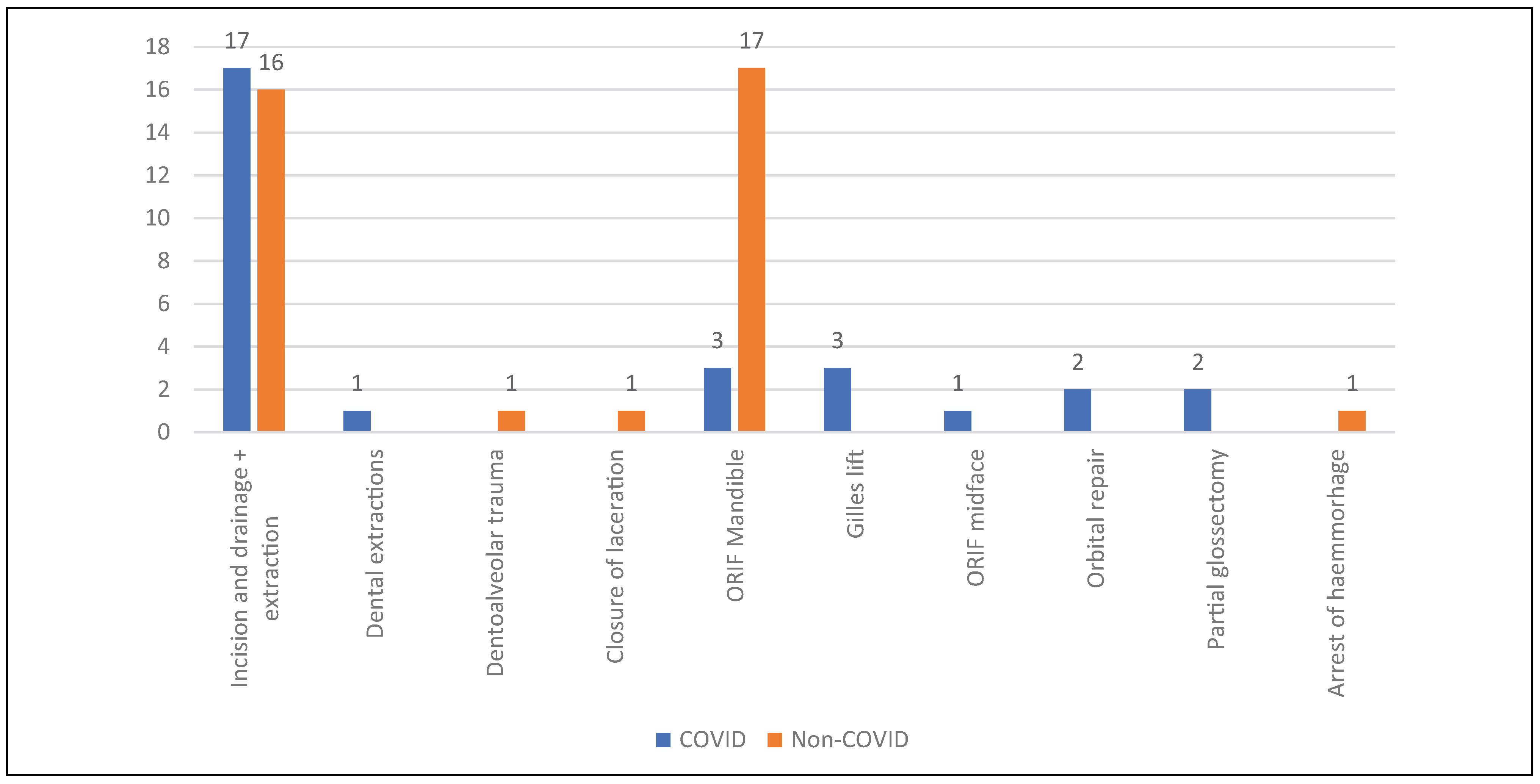
In the year prior to COVID, 32 patients did not require follow up in outpatients, 17 were reviewed face to face at the hub and 2 at the spokes following discharge. With the use of telemedicine during COVID, 21 patients required no follow up, 5 required face to face review at the hub and 5 at spokes, 10 patients were followed up with telephone reviews and 1 with a video consultation. Thus less patients were followed up face to face following discharge during COVID p = 0.026, with clinicians conducting telemedicine reviews where appropriate.
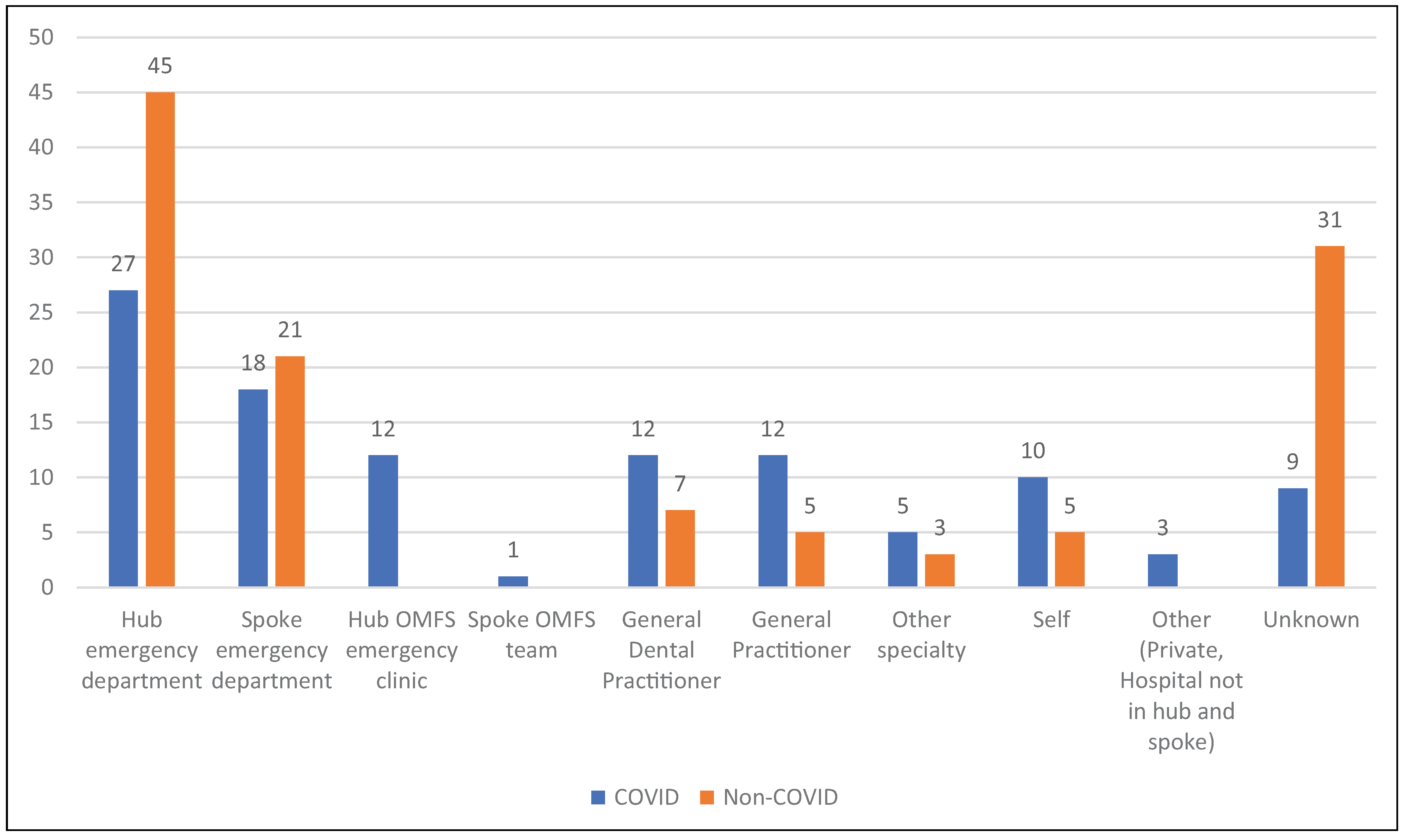
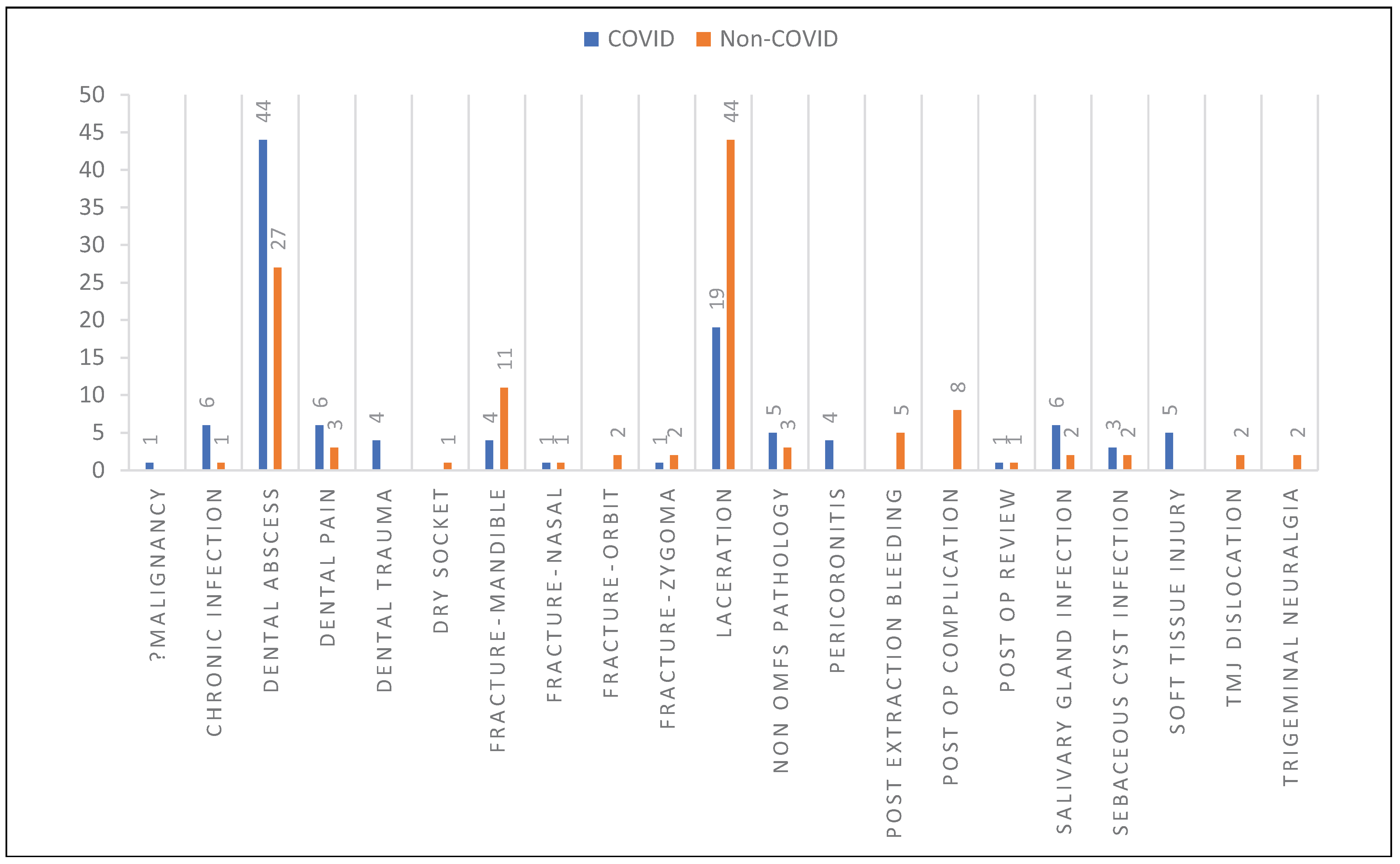
Outpatient Reviews on GP Referral Unit
A total of 110 patients (
Figure 6 and
Figure 7) were reviewed on the GP referral unit, average age 43 (range 16-100) and 27 of these patients required admission during COVID. A total of 117 patients, average age 43 (range 16-87) and 33 of these patients required admission during non-COVID.
Outpatient reviews on the GP referral unit saw an increased number of dental abscesses reviewed p = 0.0067 and significantly less lacerations p = 0.0007 (
Figure 7). There were no post extraction complications seen on the unit during COVID and a reduced amount of facial lacerations p = 0.0073.
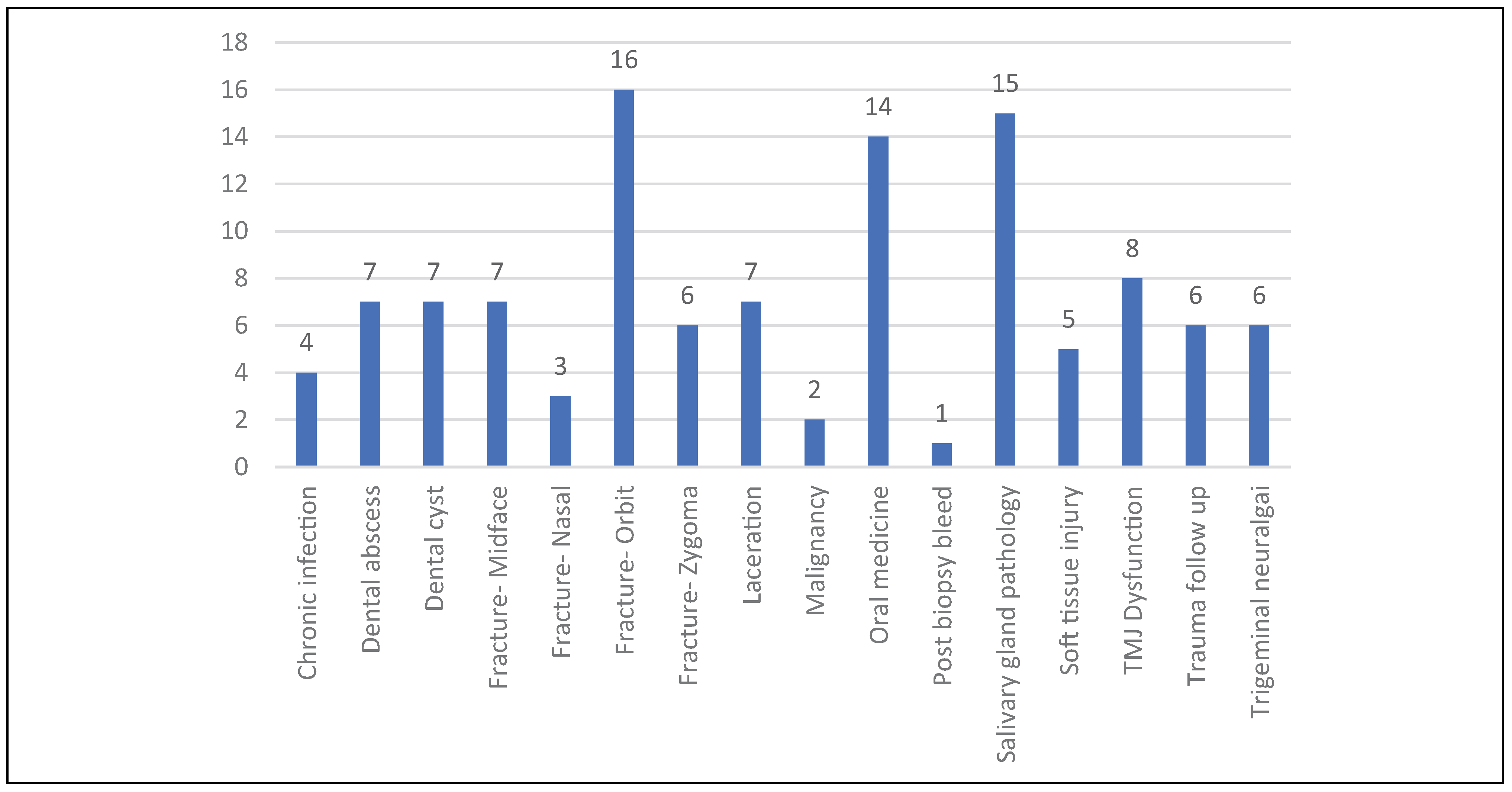
Consultant Led Emergency Clinic Reviews
A total of 114 patients were reviewed in clinic average age 45 (range 3-90;
Figure 8), 15 patients did not attend.
Discussion
The bulk of emergency maxillofacial surgery admissions are due to trauma and orofacial infections, we saw a statistical significance in the reduction of both of these during COVID and a reduction in the number of patients requiring admission. The reduction in presentations may be due to a number of factors such as government restrictions including the lockdown, working from home, social distancing, closure of entertainment venues and patients not wanting to come into hospital due to perceived real and apparent risks. We saw a statistically significant reduction in the number of fractured mandibles and lacerations seen. Prior to COVID lacerations at night were reviewed by the OMFS FY2 or plastics cross-cover and booked into GPRU the following day for closure; during the COVID period, StRs performed first on call duties at night and a small reduction in numbers may be attributed to the StRs closing wounds in the emergency department rather than bringing patients back the next day.
Unlike most units in the UK, the Oxford hub relies on FY2 doctors for first on-call rather than dental juniors. This was a potential disadvantage as the loss of the FY2s impacted on the OMFS service. We have 4 dental core training (DCT) posts, these juniors were able to help with dental emergencies and facial lacerations during the day during the COVID period. The use of more senior decision makers as first on call overnight and covering emergency clinics may have reduced our number of admissions. The average length of stay of inpatients during COVID was reduced from 2.4 days to 1.7 days. The reduction in length of stay can be attributed partly to utilizing our GPRU to ambulate patients for treatment with IV antibiotics and performing some emergency surgery as day case procedures. As well as a conscious effort to reduce inpatient stay, telemedicine was utilized in the follow ups of inpatient admissions. The patients who required face to face consults were those with complex facial trauma and oncology.
Patients who required emergency management of fractures were treated in a similar manner to the non COVID period as there was good access to theater for emergency care, the right level of PPE was always available and patients were counseled about the risks but operated in a COVID light environment. Plans were in place to delay or manage patients with non-operative interventions if required, however, the capacity of the system meant this was not required.
The OMFS service mobilized well and had a plan in place for redeployment of StRs if needed with consultant only delivered OMFS care. The creation of a service that allowed oncology consultants to be freed to manage cancer cases and 2 week waits but utilizing all non-oncology consultants to provide emergency care and perform COVID tracheostomies, allowing for a daily “ghost team” to be called in if staff were unwell, was an effective use of consultant time and limited resources across the region.
Interestingly we did not see a statistically significant reduction or increase of dental abscesses requiring admission. This may be explained by the recommendations to the AAA (Advise, analgesia, Antibiotics) treatment given remotely by General Dental Practitioners.[
6] However, on the GPRU we did see a statistically significant increase in the number of patients requiring face to face review for dental abscesses. The authors feel that this may be due to the delay in the establishment of Urgent Dental Centres (UDCs) locally and once established this information not being locally disseminated effectively to local General Dental Practitioners (GDPs) and NHS 111. Due to a lack of communication within the area NHS 111 and many General Dental Practioners referred patients directly to Accident and Emergency and were therefore assessed by the OMFS team. Of the dental abscesses seen, 62% could have been managed in primary care with a course of oral antibiotics +/— incision and drainage +/— extraction under local anesthetic. The number of orofacial infections requiring review on the GPRU increased significantly and this may be due to General Practitioners reducing the number of face to face consultations at their practice.
This study is limited by the retrospective nature of data from 2019 and lacks data from the spoke units where there was no formal recording of activity. Despite this, the authors experience was that the hub and spoke model enabled the service to quickly adapt to the changes necessary during the COVID pandemic. The use of a centralized hub allowed information to be quickly disseminated and changes to be established across the region, such as establishing daily consultant delivered emergency clinics. As all the StRs were in one location, the FY2s could be redeployed within the trust and senior decision makers managed all patients presenting to the service. Consultants providing outpatient services in the spoke hospitals allowed emergency and review appointments locally, minimizing travel for patients and the burden on hospital transport for transfers and reducing footfall on the hub site. Some of these positive changes will be permanent resulting in improved patient experience. The challenges that the hub and spoke model encountered were administrative ensuring good communication such that review of patients at their local spoke hospital were organized rather than booking them to be seen at the hub. The NHS Trusts in the hub and spokes have different electronic patient record systems and it was not possible to access hub records at the spokes so efficient handover was required. This is a significant disadvantage of the current NHS digital set up that does not have a centralized system for patient records. We plan to institute a hub to spoke referral system to efficiently aid communication with our spoke hospital units as a quality improvement project.
Conclusions
The results of our study confer with Blackhall et al [
7] a UK based study and papers from Italy [
8,
9,
10]: a reduction in trauma load and increase in the number of dental abscesses seen. The hub and spoke model was recommended as a model for OMFS in GIRFT 2018 and the authors believe this model allowed the OMFS team to co-ordinate across multiple trusts effectively, dynamically and in a timely manner. Adapting quickly during COVID was necessary due to the constant change in recommendations and guidelines. Utilizing spoke hospitals for emergency reviews and follow ups reduced the number of patients traveling into the hub, a COVID positive site and reduced the burden on hospital transport. The authors feel that the advantages of this model outweigh any administrative challenges that they encountered and that the Hub and Spoke model allowed their workforce and resources to best serve their patient population.