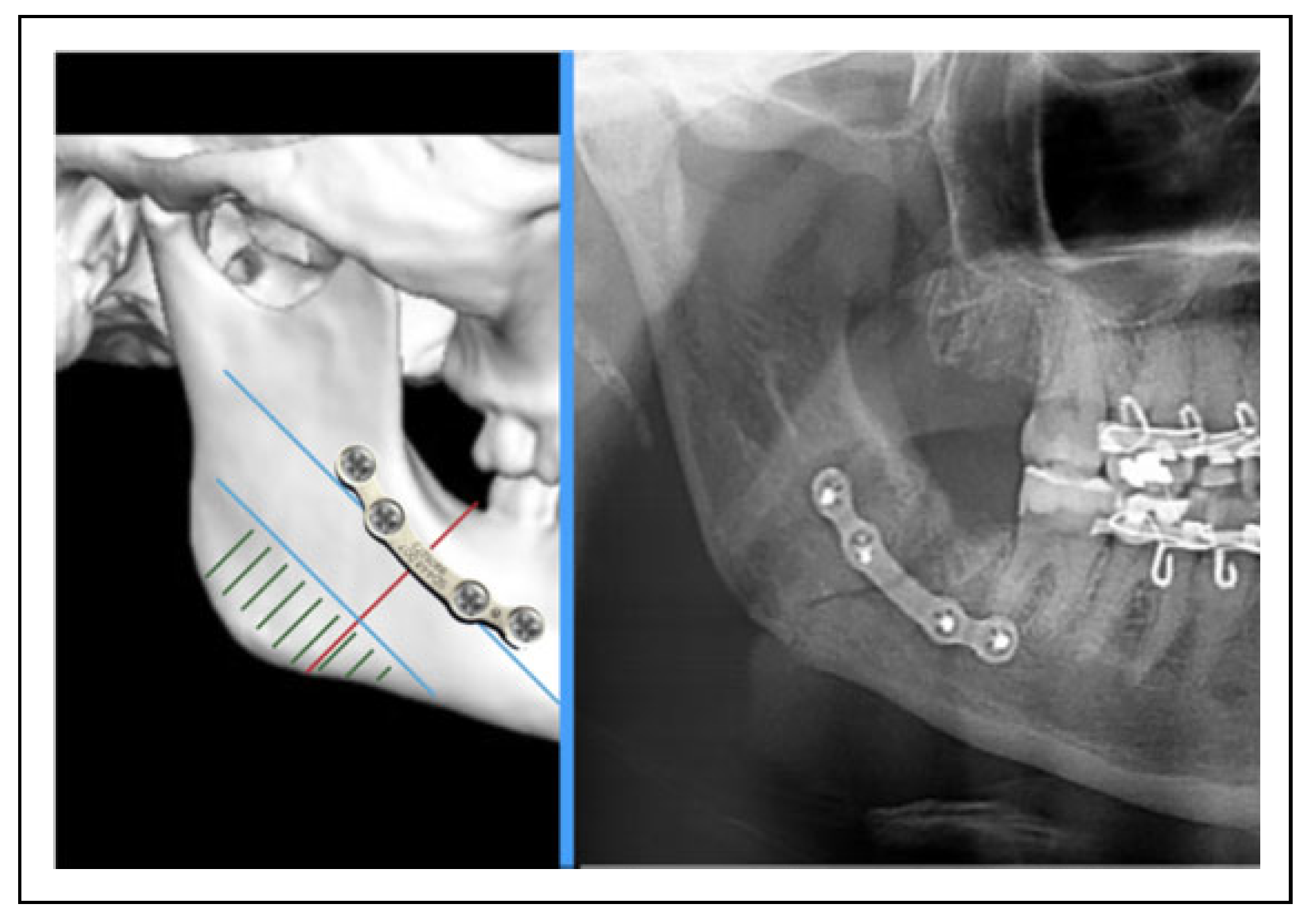
Is There a Safe Zone for Lateral Border Fixation of Mandibular Angle Fractures?
Abstract
:1. Introduction
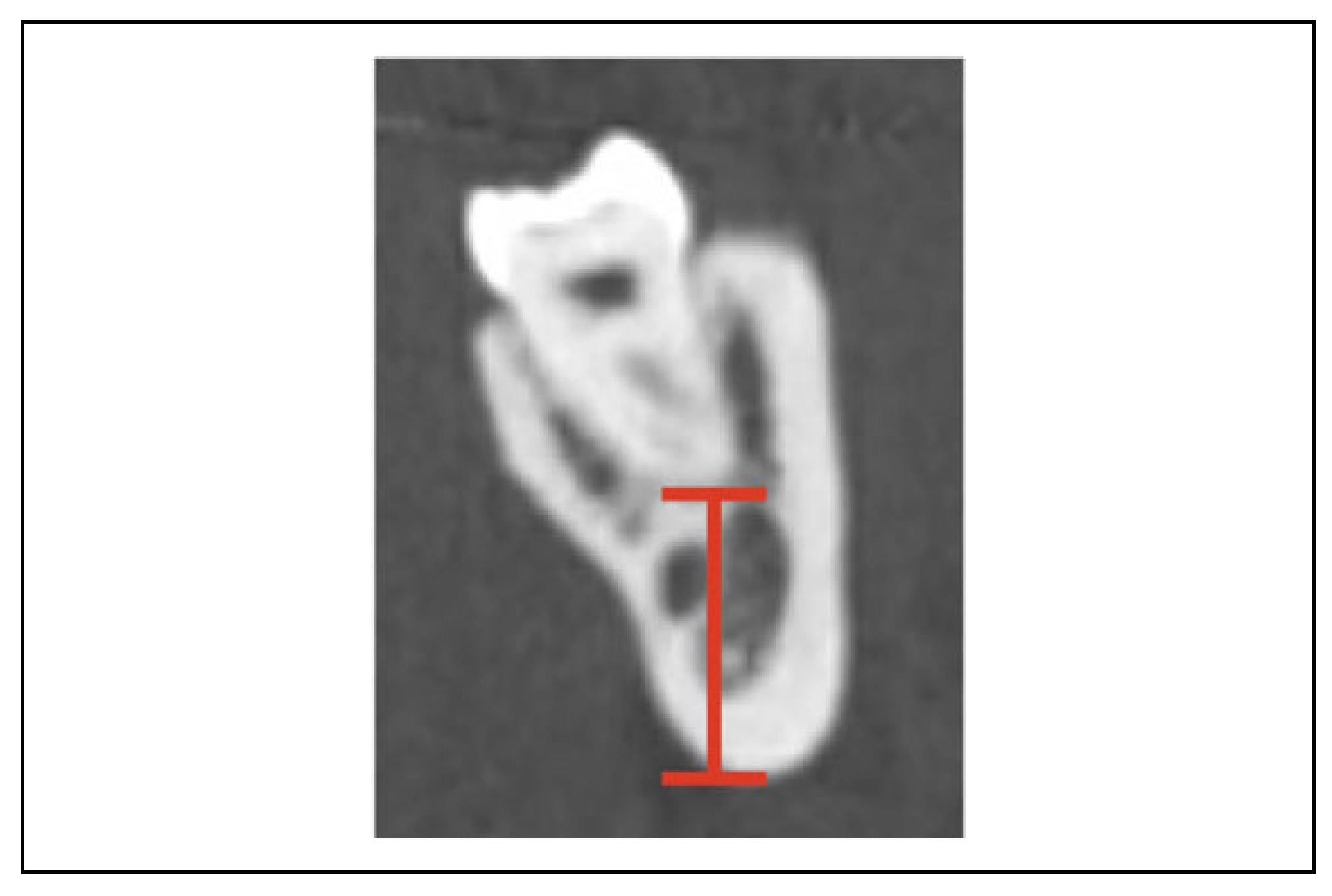
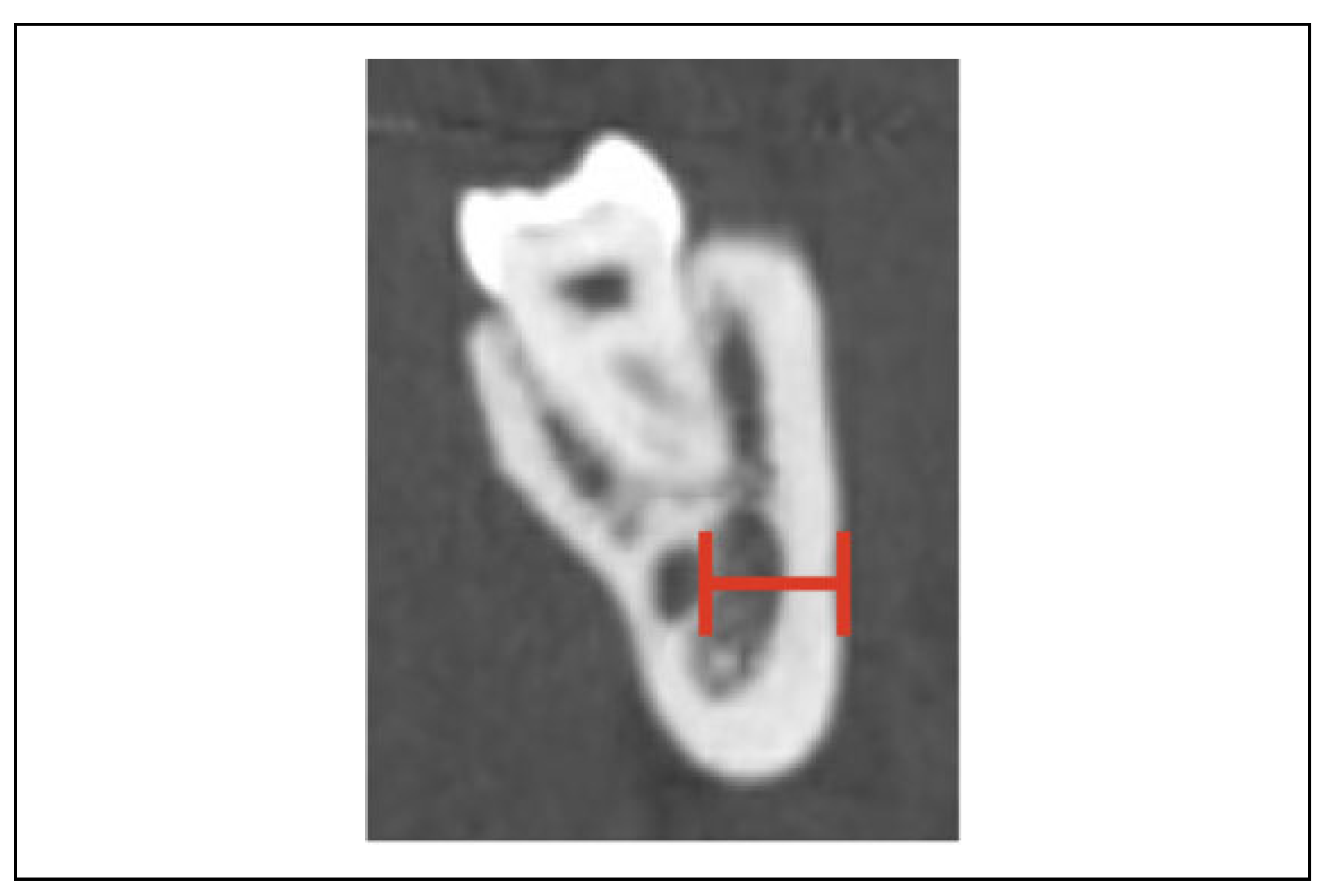
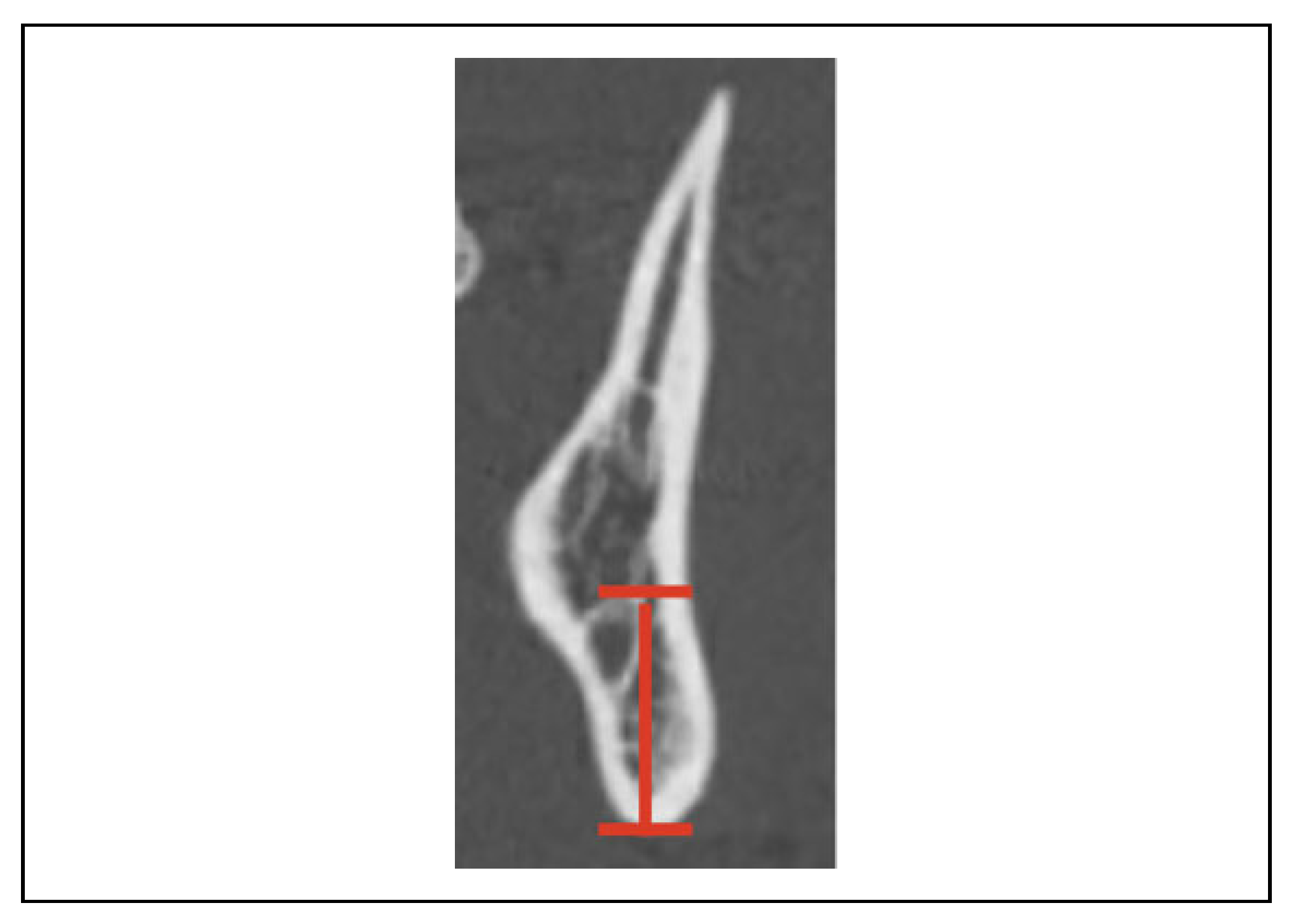
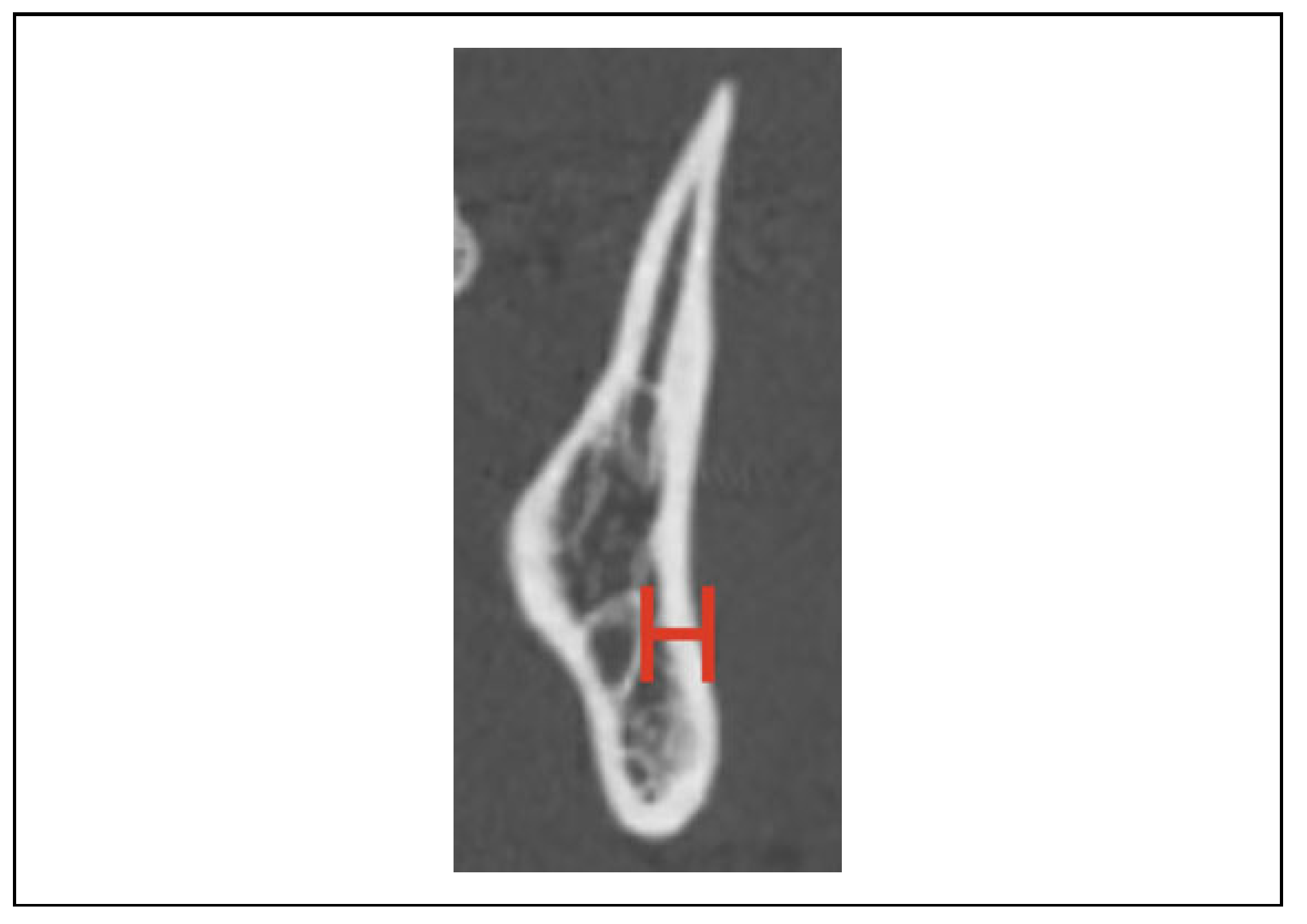
2. Methods
3. Results
4. Discussion
5. Conclusions
Funding
Conflicts of Interest
References
- Mehra, P.; Murad, H. Internal fixation of mandibular angle fractures: A comparison of 2 techniques. J. Oral. Maxillofac. Surg. 2008, 66, 2254–2260. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E., 3rd. Treatment methods for fractures of the mandibular angle. Int. J. Oral. Maxillofac. Surg. 1999, 28, 243–252. [Google Scholar] [PubMed]
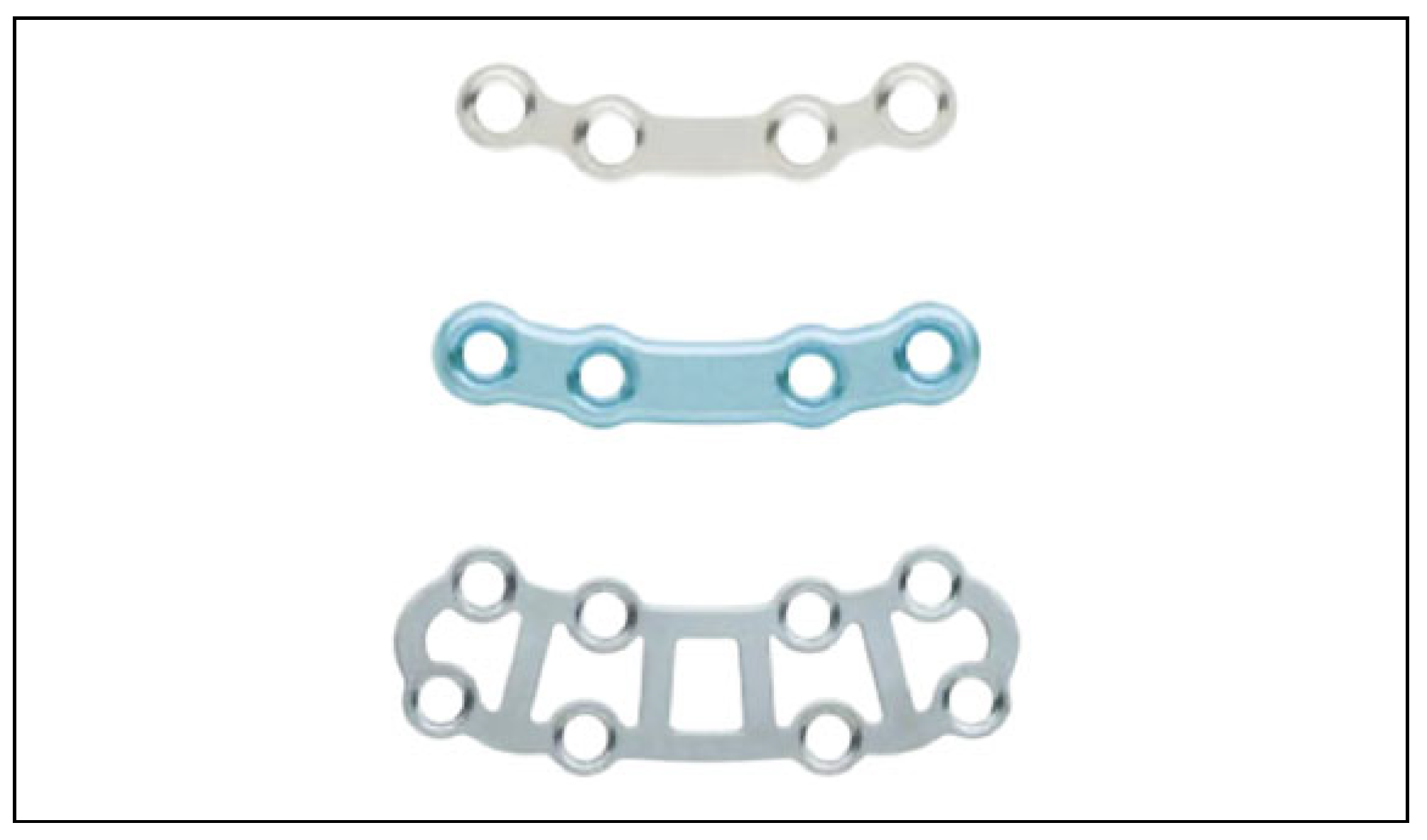
- de Oliveira, J.C.S.; Moura, L.B.; de Menezes, J.D.S.; Gabrielli, M.A.C.; Pereira Filho, V.A.; Hochuli-Vieira, E. Three-dimensional strut plate for the treatment of mandibular fractures: A systematic review. Int. J. Oral. Maxillofac. Surg. 2018, 47, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, A.C.; Rossi, M.A.; Schaffner, I.S.; Machado, L.A.; Sampaio, A.A. Lateral cortical bone thickness of human mandibles in region of mental foramen. J. Oral. Maxillofac. Surg. 2010, 68, 2980–2985. [Google Scholar] [CrossRef] [PubMed]
- Tyndall, D.A.; Price, J.B.; Tetradis, S.; Ganz, S.D.; Hildebolt, C.; Scarfe, W.C. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2012, 113, 817–826. [Google Scholar] [CrossRef] [PubMed]
- Shaik, K.V.; Mohan, A.P.; Kumar, J.; Chari, H. Pre-operative assessment of anatomical position of inferior alveolar nerve and its significance in bilateral sagittal split osteotomy. J. Maxillofac. Oral. Surg. 2017, 16, 453–464. [Google Scholar] [CrossRef] [PubMed]
- Cavalcanti, M.G.; Yang, J.; Ruprecht, A.; Vannier, M.W. Accurate linear measurements in the anterior maxilla using orthoradially reformatted spiral computed tomography. Dentomaxillofac Radiol. 1999, 28, 137–140. [Google Scholar] [CrossRef] [PubMed]
- Coşkun, İ.; Kaya, B. Relationship between alveolar bone thickness, tooth root morphology, and sagittal skeletal pattern: A cone beam computed tomography study. J. Orofac. Orthop. 2019, 80, 144–158. [Google Scholar] [CrossRef] [PubMed]
- Farnsworth, D.; Rossouw, P.E.; Ceen, R.F.; Buschang, P.H. Cortical bone thickness at common miniscrew implant placement sites. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Guimond, C.; Johnson, J.V.; Marchena, J.M. Fixation of mandibular angle fractures with a 2.0-mm 3-dimensional curved angle strut plate. J. Oral. Maxillofac. Surg. 2005, 63,, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Danda, A.K. Comparison of a single noncompression miniplate versus 2 noncompression miniplates in the treatment of mandibular angle fractures: A prospective, randomized clinical trial. J. Oral. Maxillofac. Surg. 2010, 68, 1565–1567. [Google Scholar] [CrossRef] [PubMed]
- Mondal, S.; Singh, G.; Mishra, M.; Gaur, A.; Srivastava, A. Comparative evaluation between single noncompression miniplate and two noncompression miniplates in the treatment of mandibular angle fractures. Craniomaxillofac Trauma. Reconstr. 2019, 12, 122–127. [Google Scholar] [CrossRef] [PubMed]


 |
© 2020 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Press, S.G.; Miller, A.J.; Luschen, M.C. Is There a Safe Zone for Lateral Border Fixation of Mandibular Angle Fractures? Craniomaxillofac. Trauma Reconstr. 2021, 14, 284-288. https://doi.org/10.1177/1943387520983118
Press SG, Miller AJ, Luschen MC. Is There a Safe Zone for Lateral Border Fixation of Mandibular Angle Fractures? Craniomaxillofacial Trauma & Reconstruction. 2021; 14(4):284-288. https://doi.org/10.1177/1943387520983118
Chicago/Turabian StylePress, Steven G., Andrew J. Miller, and Michelle Campbell Luschen. 2021. "Is There a Safe Zone for Lateral Border Fixation of Mandibular Angle Fractures?" Craniomaxillofacial Trauma & Reconstruction 14, no. 4: 284-288. https://doi.org/10.1177/1943387520983118
APA StylePress, S. G., Miller, A. J., & Luschen, M. C. (2021). Is There a Safe Zone for Lateral Border Fixation of Mandibular Angle Fractures? Craniomaxillofacial Trauma & Reconstruction, 14(4), 284-288. https://doi.org/10.1177/1943387520983118




