Abstract
Study Design: There are potential substantive linkages between illicit drug use and the occurrence of injury. Objective: The purpose of our study was to determine the prevalence, class of illicit drugs abused, and demographics in relation to a cohort of patients who sustained facial injury. Methods: The authors undertook a retrospective observational study of a prospectively accessioned cohort of patients who had sustained a facial injury and presented to the John Hunter Hospital (Newcastle, NSW, Australia). The primary predictor variable was the presentation of a facial injury and the secondary outcome variables included illicit drug use, alcohol use, and socioeconomic factors. The study was carried out over a 12-month period. A descriptive analysis was undertaken on the assembled data. Results: Of the 465 patient medical records that were accessed for the study, 348 were male and 117 were female. Their average age was 42.6 years: 5.8% (n = 27) were under the influence of illicit drugs at the time of their presentation and 13.1% (n = 61) admitted to an intercurrent illicit drug habit. Those who were under the combined influence of alcohol and drugs comprised of 2.8% (n = 13). Conclusions: Our study found that illicit drug use plays a small, but nonetheless, demonstrable role in the presentation of maxillofacial trauma patients to an urban level I trauma center. Illicit drug users are an emergent sociodemographic group of patients who can sustain facial trauma and their presentation needs to be appropriately considered, assessed, and managed collectively.
Introduction
Substance abuse is a serious and complex problem that has become a major public health concern in many countries.[1] The use of alcohol and illicit drugs, either individually or synergistically, can impose a significant burden on the delivery of government health and social services. At a community level, these substances predispose to social and family disruption, loss of productivity, and episodes of violence and crime.[1,2] On an individual basis, substance abuse is a major cause of a variety of acute and chronic health conditions, mental illness, dependency, and premature death.[3]
Illicit drugs normally behave as psychoactive chemical mediators and exert their effect by acting either as a surrogate neurotransmitter or by altering established neuronal circuitry which results in evoking feelings of euphoria or pleasure.[3,4] Illicit drugs variably exert their central nervous system effects as a stimulant (amphetamines, cocaine, 3,4-Methylenedioxymethamphetamine.[MDMA]), a depressant (heroin, marijuana), or a hallucinogen (lysergic acid diethylamide). They can therefore affect thought, mood, perception, personality, and behavior in users. As a result, their use can predispose to accidental (through an increase in self-confidence, impulsivity, impaired judgment/reasoning, euphoria, disinhibition) or non-accidental (violence/aggression/selfharm) injury.[3,5]
For the purposes of this investigation, we considered two broad classes of illicit drug usage that have been described in the literature: (I) illegal drugs—a drug that is prohibited from manufacture, sale, or possession, or (II) pharmaceuticals—a drug that is available from a pharmacy either on prescription or over-the-counter.
It has been well-established that injury is one of the leading causes of acute hospitalization.[6,7] It may be sustained intentionally, non-intentionally, or recidivistically. Several studies have shown that up to 40% of patients who attended trauma centers have a positive blood alcohol concentration, and that this figure rises to as much as 60% when polydrug use is identified from the patient’s history.[4,8] As with episodes of general trauma, there are substantive linkages between substance abuse and the occurrence of facial injury.[8,9,10]
In consideration of this emergent problem, two previous studies that were undertaken by the senior author have respectively revealed a 2% (n = 6/300 over 21 months) and 3.46% (n = 20/578 over 60 months) incidence of drug use in a cohort of psychiatric comorbid facially injured patients who attended a Level 1 Trauma Centre.[11,12] The average age of these patients was 36.9 years (range 20–62 years). The group was comprised of 17 males and 3 females. The range of illicit drugs that were identified within the study cohort included the use of cannabis, heroin, marijuana, and methamphetamines, as well as the abuse of prescription drugs, for example, serotoninspecific reuptake inhibitors.[11,12]
These important observations that were recognized within the outcomes of the two aforementioned comprehensive studies (that considered the incidence of preexisting psychopathology in a group of facially injured patients) led us to undertake this specific study (albeit preliminary in nature) into the incidence and range of illicit drug use that might potentially be identified in a similar patient cohort.
The purpose of this study was to determine the number of maxillofacial trauma patients who attended the John Hunter Hospital and who admitted to using illicit drugs. Our hypothesis was that illicit drugs use is a notable comorbidity in the incidence of facial injury presenting to our hospital service.
This study had three specific aims: (i) to determine the prevalence of illicit drug use within the study cohort, (ii) to identify the class of illicit drugs that were used by the patients, and (iii) to determine whether there were any substantive sociodemographic or etiological variables that might be associated with the use of illicit drugs.
Materials and Methods
Study Design and Sample
To address the research purposes, the authors developed and implemented a retrospective observational study of the medical records of a prospectively accessioned cohort of patients who had sustained a facial injury and had presented to either the Accident-Emergency Department or the Maxillofacial (outpatient) Department at the John Hunter Hospital (Newcastle, NSW, Australia) was developed and implemented. Specifically, the medical records were assessed for those admitting to, or under the influence of, illicit drugs. The study was carried out over a 12-month period, November 2017 to October 2018.
Variables
The primary predictor variable was the presentation of a facial injury. The secondary outcome variables included the documentation of illicit drug use, alcohol use, and relevant socioeconomic factors.
Data Collection and Analysis
The relevant data required to undertake the present study were obtained from the patient electronic record system of the hospital network. All patient encounters (outpatient and inpatient) are recorded using the digital medical record. The data were entered on a spreadsheet, and a descriptive analysis was applied to the assembled data.
Ethics Approval
This study was granted ethics approval by the Hunter New England Local Health District Human Research Ethics Review Committee (AU201810-03). All patients were deidentified and therefore, their personal and medical details remained anonymous during the study. Privacy and confidentiality of the patient records were adhered to, in managing the clinical information in the conduct of this research.
Results
A total of 465 patient medical records were accessed from the November 2017 to November 2018 period (Table 1). There were 348 males (74.8%) and 117 females (25.2%). Their average age was 42.6 years. Of the patient records reviewed, 5.8% (21 males, 6 females, n = 27) were under the influence of drugs at the time of presentation. Furthermore, 13.1% (47 males, 14 females, n = 61) admitted to a current illicit drug habit during their medical assessment. A total of 17 patients who were under the influence of drugs and who sustained a facial injury required hospital admission and surgery.

Table 1.
Characteristics of facial trauma patients presenting to the Hospital.
The specific mechanism of injury was noted for the 61 patients either under influence of drugs at the time of injury or admitting to their intercurrent use (Table 2). The vast majority of patients, 67.2%, sustained their injury from an alleged assault (n = 41). With falls, motor vehicle crashes, and sporting-related injuries reported as the mechanism for 26.2% of patients (n = 16).

Table 2.
Trauma etiology in patients admitting to intercurrent drug use.
Of those patients who admitted to illicit drug use (both at the time of injury or on a regular basis) (n = 61), the majority reported use of cannabis (50.7%). The use of amphetamines (15.9%), opioids (13.0%), MDMA (8.7%), benzodiazepines (4.3%), and cocaine (4.3%) was also noted. Of the drugs used, 79.7% (n = 55) were class I (illegal) in nature (Figure 1). Those who were solely under the influence of alcohol at the time of injury were recorded at 12.9% (n = 60) and those who were under the combined influence of alcohol and drugs comprised of 2.8% (n = 13) of the study population.
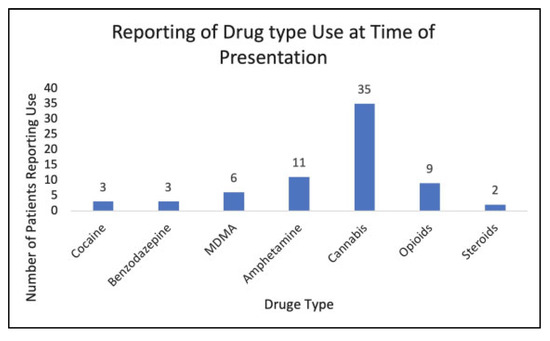
Figure 1.
Facial trauma patients presenting to the Hospital under the influence of illicit drugs.
Seventy-nine (16.1%) patients reported a previously diagnosed history of a psychiatric condition. Of these, the majority of patients reported depression (48.1%) n = 38, while other conditions reported included anxiety, attention deficit hyperactivity disorder, drug dependence, and schizophrenia. Furthermore, of the patients under the influence of illicit drugs at the time of presentation, 59.3% (n = 16) had a previous history of psychiatric illness.
Discussion
The face is a common target for assault and the resultant injury to any of its elements, including the jaws and mouth, is regarded as a prominent marker of interpersonal violence.[4,10] Goulart and coworkers demonstrated that out of 3724 patient records accessed, the use of illicit drugs was reported to be 4.64%.[9] In our study, the percentage of patients with facial injury who reported illicit drug use apparent at the time of emergency assessment was 5.8% (n = 27). The difference in results likely relate to the inclusion of all facial injuries in the current study. To the best of the authors’ knowledge, our study is arguably the first to include all oral and maxillofacial trauma (including soft tissues and/or hard tissue injuries) for these purposes.
There is a well-established association between drugs/alcohol and criminal behavior and violence.[13,14] Cordovilla-Guardia and colleagues in their review of emergency room presentations noted specific associations between violence-related injury and the use of marijuana or cocaine.[14] Our study identifies a clear relationship between interpersonal violence and injury with 67% of patients either admitting to being currently under the influence of drugs or their intercurrent use describing the mechanism of their injury to be assault.
The Australian Institute of Health and Welfare (AIHW) identified in its 2018 report that alcohol and illicit drug use was responsible for 6.7% of the total disease burden in Australia.[6] In our study, those under the influence of alcohol or drugs in patients presenting to the Emergency Department or Maxillofacial Department at John Hunter Hospital was 15.9%. The specific alcohol and drug use breakdown accounted for 12.9% and 5.8%, respectively. John Hunter Hospital is a Level 1 Trauma Center responsible for the management of facial trauma from an urban metropolitan and rural and remote New South Wales, accounting for a catchment population in excess of 850 000.
The Australian Institute of Health and Welfare also reported that Cannabis is the most commonly used illicit drug (class I) in Australia at 10.4% in 2016.[2] This is notably higher than the 8.0% of the patients admitting to the use of Cannabis in our study. Whether or not the differences in general rates of illicit drug use and specific agent used may represent regional variation, as a significant proportion of patients come from rural and remote areas, or occur due to the retrospective nature of the study (with factors such as patient’s self-report bias or poor medical history documentation by the clinician) remains speculative.
Similar studies that have been undertaken in other countries have reported varying incidences of emergency presentations in patient cohorts defined by alcohol and/or drug use. In a US study of 1220 trauma (not isolated to maxillofacial injury) patients, Soderstrom et al. concluded that overall 24.1% of patients were alcohol dependent and 17.7% were dependent on illicit drugs.[7] These results are considerably higher than the current study and this maybe secondary to a regional variation in the 2 cohorts, but a proportion in the discrepancy potentially could be accounted for by the prospective nature of the Soderstrom study and more importantly, the implementation and accuracy of urine and toxicology analysis. However, unlike our study, the Soderstrom study did not include patients who were treated nonoperatively.[7]
In the consideration of a similar demographic, a more recent study of 105 patients found 47% (n = 49) to be under the influence of illicit drugs and 40% to demonstrate the presence of alcohol.[15] However, the smaller sample size should be taken into account.
The sociodemographic characteristics that have been considered in previous studies showed a higher percentage of males to be substance abusers, which is similar to the results of our study.[7,9,10,16] Furthermore, the users of illicit drugs were likely to be younger, unmarried, and poor.[7,9,10]
The literature also suggests a previous psychiatric illness as a contributing factor for the occurrence of facial trauma.[11] A recent study assessed the past psychiatric history of patients with facial trauma in 2 centers, in the UK and Australia.[17] This study reported a psychiatric history of 10% and 17% in the UK and in Australia, respectively.[17] The results of our study identified similar results with 16.1% of patients having a documented psychiatric illness, with one-fifth of those admitting to drug intake at the time of injury.
Our preliminary study has demonstrated that there is a small but well-defined group of patients who admit to illicit drug use and who sustain a facial injury (which requires specialist assessment) while under the influence of that substance.
This highlights the importance of considering the medical status of these patients, enlisting the help of the hospital alcohol and drug service and perhaps give consideration to enlisting a psychiatry liaison consultation in order to optimize the patient’s hospital admission. This study lends support to the premise that in many instances, a coordinated multidisciplinary approach to patient care is required in these circumstances.
The strength of this study is that it provides timely recognition of a cohort of patients who sustain an episode of facial trauma in the context of illicit substance abuse. There is little in the maxillofacial surgical literature addressing this emergent problem. The weakness of the study is that it was not possible to comment on the statistical significance of our findings, notably given the limitations of the study and the small sample size under investigation. Additionally, we did not undertake blood or urine toxicology to ascertain the veracity of the illicit substance abuse. Alcohol, drugs, and psychiatric illness are often synergistic comorbidities and it is difficult to identify the respective individual or collective contributions.
In conclusion, it is our contention that the role of illicit drug use remains an under-considered comorbidity in the acute presentation of a facially injured patient. Male gender, young age, psychiatric comorbidity, and unemployment are likely socioeconomic risk factors that are associated with this group of patients.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Peacock, A.; Gibbs, D.; Sutherland, R.; et al. Australian Drug Trends 2018. Key Findings from the National Illicit Drug Reporting System (IDRS) Interviews; National Drug and Alcohol Research Centre, UNSW: Sydney, Australia, 2018; pp. 53–54. [Google Scholar]
- Australian Institute of Health and Welfare. Australian Burden of Disease Study: Impact and Causes of Illness and Death in Australia 2011; Australian Burden of Disease Study Series No. 3. BOD 4; AIHW: Canberra, Australia, 2016. [Google Scholar]
- Wall, T.; Luczak, S.; Hiller-Sturmhöfel, S. Biology, genetics, and environment: underlying factors influencing alcohol metabolism. Alcohol. Res. 2016, 38, 59–68. [Google Scholar] [PubMed]
- Lee, K.; Olsen, J.; Sun, J.; Chandu, A. Alcohol-involved maxillofacial fractures. Aust. Dent. J. 2017, 62, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Spronk, D.; Verkes, R.; Cools, R.; et al. Opposite effects of cannabis and cocaine on performance monitoring. Eur. Neuropsychopharm 2016, 26, 1127–1139. [Google Scholar] [CrossRef] [PubMed]
- Henley, G.; Harrison, J. Trends in Injury Deaths, Australia, 1999–00 to 2011–12; Injury Research and Statistics Series No. 108. 2017.Cat. No. INJCAT 188; AIHW: Canberra, Australia, 2015. [Google Scholar]
- Soderstrom, C.; Dischinger, P.; Smith, G.; et al. Psychoactive substance dependence among trauma center patients. JAMA 1992, 267, 2756–2759. [Google Scholar] [CrossRef] [PubMed]
- Martins, S.; Copersino, M.; Soderstrom, C.; et al. Sociodemographic characteristics associated with substance use status in a trauma inpatient population. J. Addict. Dis. 2007, 26, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Goulart, D.; Durante, L.; De Moraes, M.; et al. Characteristics of maxillofacial trauma among alcohol and drug users. Arch. Craniofac Surg. 2015, 26, 783–786. [Google Scholar] [CrossRef] [PubMed]
- Murphy, D. Substance use and facial injury. Oral. Maxillofac. Surg. Clin. N. Am. 2010, 22, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.; Hooi, H.; Hoffman, G. Presence of pre-existing psychological comorbidity in a group of facially injured patients: a preliminary investigation. J. Oral. Maxillofac. Surg. 2009, 67, 1889–1894. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, G.; Islam, S. Facial trauma patients with preexisting psychiatric illness: a 5-year study. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Pathol. 2013, 116, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Lee, K. Interpersonal violence and facial fractures. J. Oral. Maxillofac. Surg. 2009, 67, 1878–1883. [Google Scholar] [CrossRef] [PubMed]
- Cordovilla-Guardia, S.; Garcıa-Jimenez, C.; Fernandez-Mondejar, E.; et al. Association between the detection of alcohol, illicit drugs and/or psychotropic medications/opioids in patients admitted due to trauma and trauma recidivism: a cohort study. PLoS One 2018, 13, e0203963. [Google Scholar] [CrossRef] [PubMed]
- McKenna, K.; Harrison, J. Hospital Separations Due to Injury and Poisoning, Australia 2008–09; Injury Research and Statistics Series No. 65. Cat. No. INJCAT 141; AIHW: Canberra, Australia, 2012. [Google Scholar]
- Othman, S.; Cohn, J.; Toscano, M.; et al. Substance use and maxillofacial trauma: a comprehensive patient profile. J. Oral. Maxillofac. Surg. 2019, 78, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.; Ahmed, M.; Walton, G.; et al. The prevalence of psychological distress in a sample of facial trauma victims. A comparative cross-sectional study between UK and Australia. J. Cranio Maxill Surg. 2012, 40, 82–85. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. The Author(s) 2020.