Introduction
Management of maxillofacial fractures has gone through various phases of advancement in the past century. With the development of osteosynthesis, in the plethora of commercially available types of plates and screws that principally tend to become smaller and simpler to handle, it is for the clinician to choose one that best suits his needs. While doing this, the design of various screws should be taken into consideration for the load application on the mandible.[
1] Since different designs of screws are available, there is a need to know the potential of each type of screw as well as its pattern of stress distribution in bone.
Self-tapping screws are routinely used for fixation of mandibular fractures that are inserted after drilling a pilot hole with a minimum diameter size equal to the screw’s core. Self-drilling screws are the recent modification in screw geometry, which looks like a simple wood screw that eliminates drilling the pilot hole.[
2]
Also one of the most commonly encountered postoperative complications in miniplate semi-rigid fixation is screw loosening resulting in infection.[
1] Thus, studying the screw performance can provide an insight into the success of semi-rigid internal fixation in the healing of fractures.
Since in vivo assessment of screw performance in healing of fracture is merely impossible per the ethical concern; in this regard, the finite element analysis (FEA) has impressed medical and dental researchers and is now one of the most successful engineering computational methods. The purpose of this study was to evaluate the efficacy of self-tapping and self-drilling screws in terms of stability/ retention ability in internal fixation of the fractured fragments of the mandible by performing pullout test, torque test, and torsional effect at the screw–bone–plate interface using 3D FEA.
Materials and Methods
This study was conducted in the Department of Oral and Maxillofacial Surgery, FDS, RUAS, Bangalore, Karnataka, India. The finite element method (FEM) is a quantitative numerical analysis technique that involves three stages of processing: the preprocessing stage, the solving stage, and the post-processing stage.
Our study involved construction of 3D geometric model which represented the biological properties of the mandible and the screws. The computer-aided design (CAD) model of the mandibular bone block was translated into a 3D trilaminate FEA block using CATIA software (Version 6), where thresholding and editing functions were used to create entities for cortical and cancellous bone (
Figure 1). The finite element model is the representative component of the original geometry in terms of finite number of elements and nodes. In this study, the finite element model generation was done according to the ANSYS (version 14.5) software.
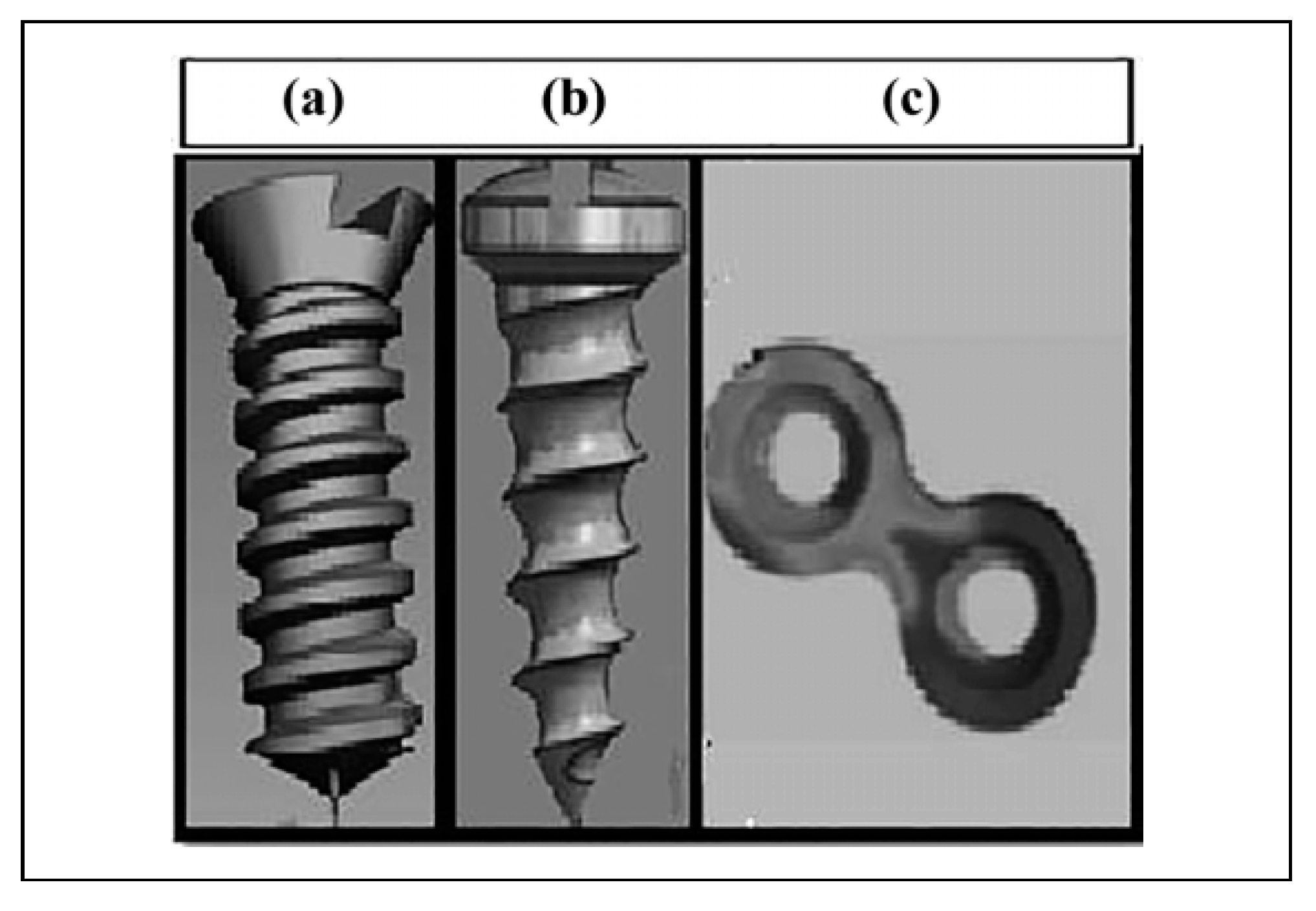
A 3D geometric model of a screw and plate was simulated per the specification with respect to the length of the screw, diameter of the screw head and body, number of threads, pitch size, shape, and design of the screws using reverse engineering. The self-drilling and self-tapping screws of 2 mm diameter, 8 mm length, and pitch distance of 1 mm were constructed along with the CAD model of 2 × 2 hole miniplate using CATIA software (
Figure 2).
Assignment of material properties to a finite element model is much necessary to simulate the behavior of the study object. Since the bone was assumed to have linear elastic property, the material properties were assigned accordingly to the trilaminate finite element model of bone to simulate the behavior of natural mandible.
Orthotropic properties were assigned for cortical bone according to Schwartz-Dabney and Dechow, whereas an isotropic property for the cancellous portion of bone is same throughout according to J. R. Fernandez et al.[
1] In the present study, the orthotropic properties of parasymphysis region were considered. The screws and plate were considered to be made of the same material, that is, titanium alloy, hence the material properties of titanium were assigned according to FE study done by Cox et al (
Table 1 and
Table 2).[
1,
3]
A numerical model of the bone–screw interface was generated with eight threaded joints to simulate an engaging length of 8 mm between the screw, cortical bone, and cancellous bone to have uniform transfer of force between the screw edge and the bone. A global coordinate system was defined with the
Y-axis along the longitudinal axis of the screw and the
X- and
Z-axes acting radially (
Figure 3).
A fracture line was simulated on the trilaminate mandibular model, where a miniplate was virtually adapted and fixed with screws on either side of the fracture line. The simulation was done in concordance with the clinical situation, so that the plate and screws did receive/transfer the stresses directly from/to the bone.
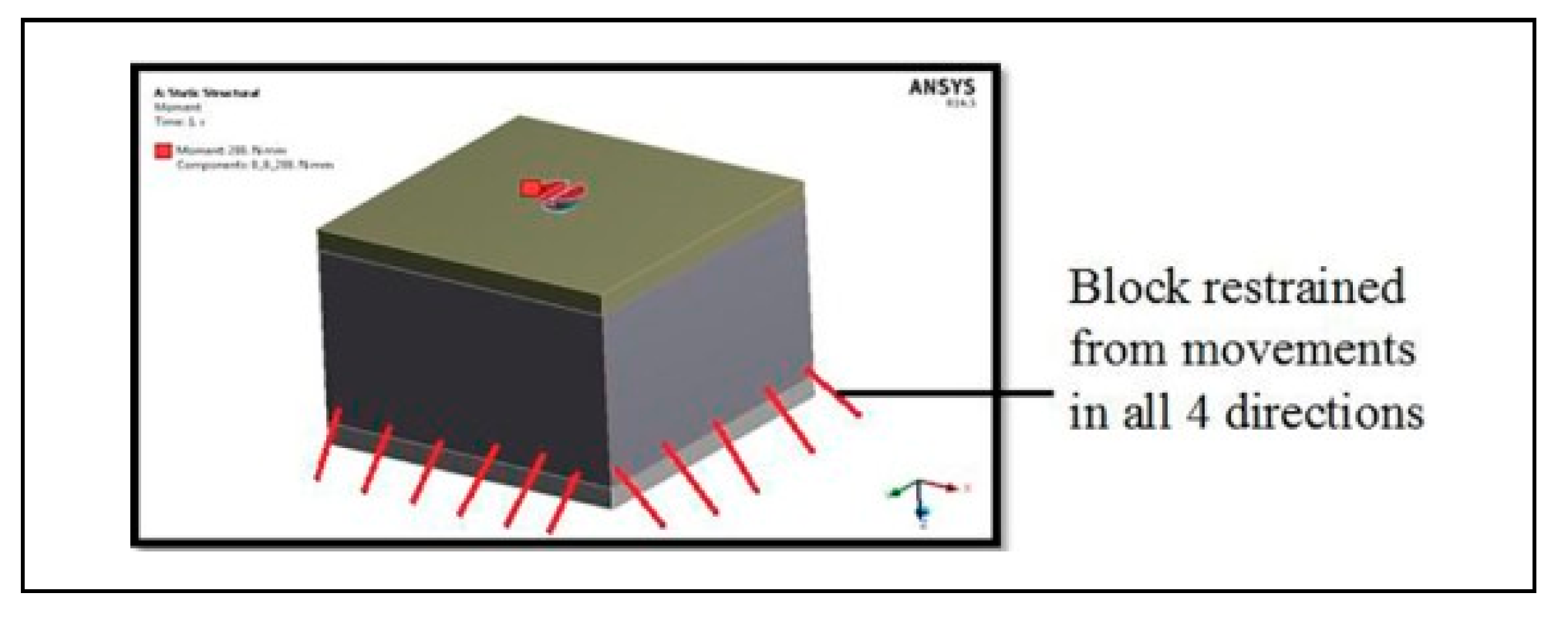
The boundary condition was defined according to the tests performed. For torque and pullout tests, the assembled trilaminate block model was restrained from its movement in all degrees of freedom (
Figure 4), whereas for torsional effect test, both the fragments were free for rotation, and boundary condition was defined at the screw–plate–bone interface to simulate the actual constraint from the free bodily movement of fractured segments.
The amount of stress and strain was calculated at each nodal point using Hypermesh 13.0 version and ANSYS software version 14.5 to generate models and postprocessing the results, respectively.
Application of Forces
Torque test. The test involves effective insertion of the screw within the trilaminate block with the sequential increase from minimal torque power up to 100 N in uniaxial direction. The stress concentration and deformation occurring at the screw bone interface was observed.
Pullout test. The negative force of 50 N was applied arbitrarily onto the head of the screw assuming it could be the maximum torsional force acting on the screws during mastication, while maximum masticatory force generated in the mandibular anterior region is 90 to 100 N (
Figure 5).
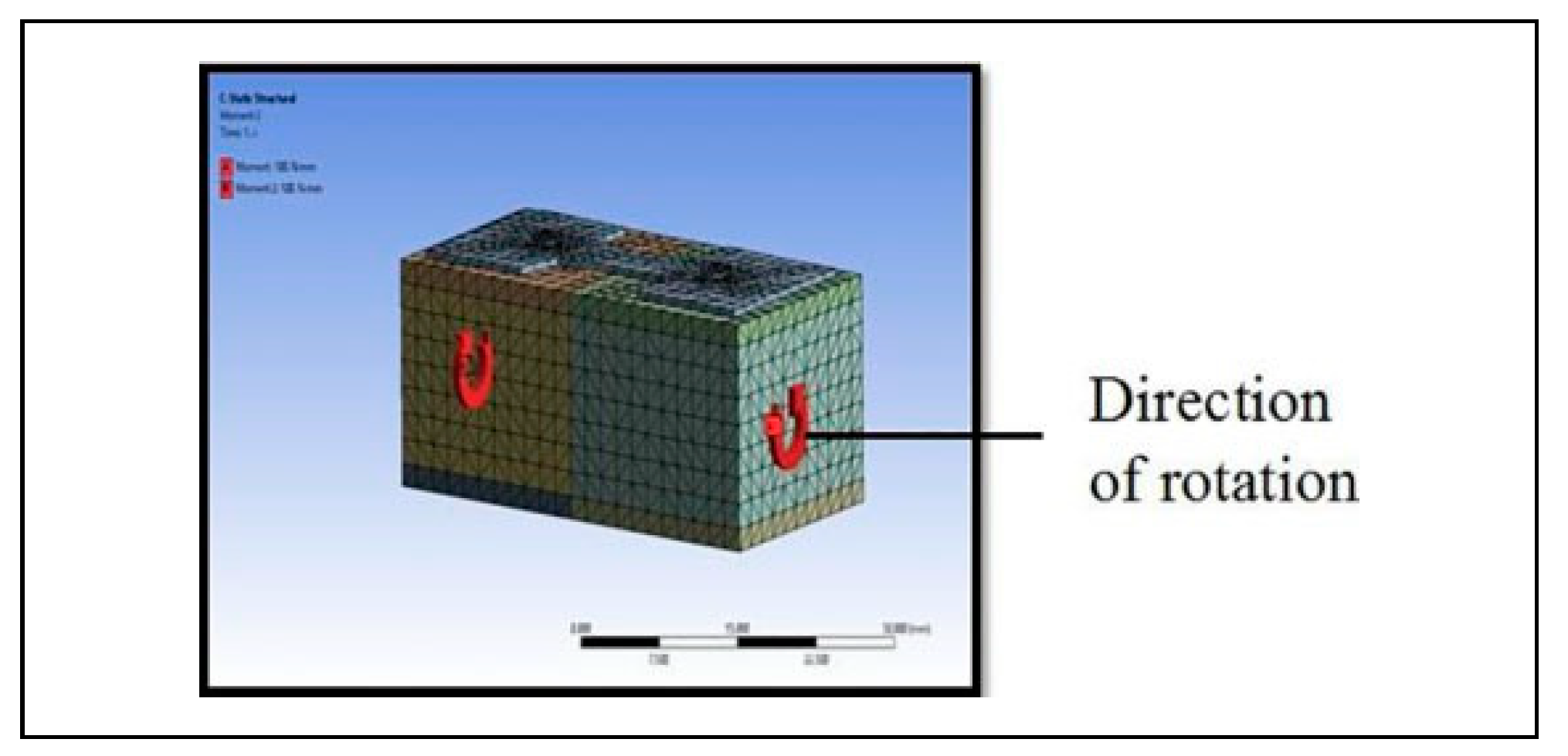
Torsional effect on screw upon application of angular force. The trilaminate blocks fixed with miniplate and screws were subjected to rotational force, that is, clockwise on one side and anticlockwise rotation on the other side of the fracture line and assessed for deformation and stress concentration at the screw–bone–plate interface (
Figure 6).
Discussion
There has been a gradual shift toward the use of simpler and smaller implants for fixation of fractures in the recent days.
The success in healing of the fractured bone with respect to screw depends upon the shape of the screw, pitch distance, number of threads, and retention ability in the host bone to withstand the dynamic masticatory load. Therefore, it is of pivotal importance to design a study which assesses all the primary factors and ascertains the stability for success of the screws. There is insufficient data regarding the efficacy of self-drilling and self-tapping screw design on fixation of fractures.
In medical and dental research, the strain gauge technique, photoelastic test, and FEM are commonly used to analyze the stress of structural objects with complex morphology. The strain gauge technique allows only measurement of discontinuous surface areas and cannot provide measurement of internal stress. The photoelastic test can determine internal stress, but construction of the model is difficult and its accuracy is also limited.[
3]
The FEM is a stress analysis technique used to determine overall stress and displacement by dividing the continuous region of the structural object into finite number of elements and by calculating the dynamic equilibrium among these elements.
Hence, the present study was undertaken to determine the efficacy of self-drilling and self-tapping screws on fixation of mandibular parasymphysis fractures, which brings about primary stability as well as retention of screw within the bone using FEA.
The use of self-drilling screws was first described by Heidemann and Gerlach et al. (1996, 1999) later by Guntermann et al.[
5] and Schimming et al. (1998, 1999).
Self-tapping screws require drilling of the pilot hole which is associated with thermal damage, possibly leading to infection, loosening of hardware, and nonunion. Damage to subjacent nerves, tooth roots, and drill bit breakage has also been reported. On the contrary, self-drilling screws can be inserted without initial drilling of the pilot hole, as they have sharp tip and threads that follow an axis of rotation up to the screw head, thereby decreasing the operative time.[
4] Heidemann et al. in their animal study suggested that self-drilling screws can be used into bone up to 2 mm in thickness without any difficulty. In bone greater than 2 m of thickness self-drilling screws have an increased risk of screw fracture.[
5]
The present study utilized CAD models of the self-tapping and self-drilling screws along with the trilaminate block to simulate the behavior of cortical and cancellous properties of parasymphysis region of the natural mandibular bone with the help of CATIA software. The material properties for CAD models were assigned according to Naresh Chaudhary et al for virtual simulation of titanium metal and the bone.
Numerous biomechanical studies have revealed that there is a direct correlation between highly stressed regions and bone resorption. It is well accepted that due to constant increase in the stress concentration around the screw–bone interface, there will be increased osteoclastic activity over a period of time resulting in screw loosening or implant failure/breakage. Hence, high stress distribution/concentration in the bone should be avoided to achieve stable osseointegration and long-term stability.
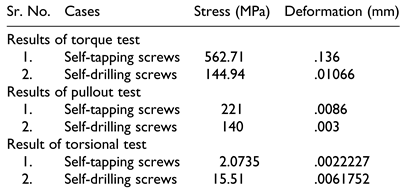
In the present FEA study, the parameters considered to check the efficacy of screws were torque test, pullout test, and torsion test, which were measured in terms of maximum stress concentration around the screw–bone interface which helped us to assess the efficacy of screw design.
The bone–screw thread interface and bone remodeling after the insertion of self-drilling and self-tapping screws were assessed by Juliana Gonc¸alves Goelzer et al. using scanning electron microscopy in rabbit’s calvaria, where they stated that the contact between bone and screw threads with the self-drilling screw was much superior with no deformation of the apex after its insertion as it exhibited an active cut at the tip.[
6]
The screw–bone interface of the self-drilling screws was greater than 88% of the total surface area of the screw threads and about 55% contact in case of self-tapping screws without causing much harm to the surrounding bone[
5]
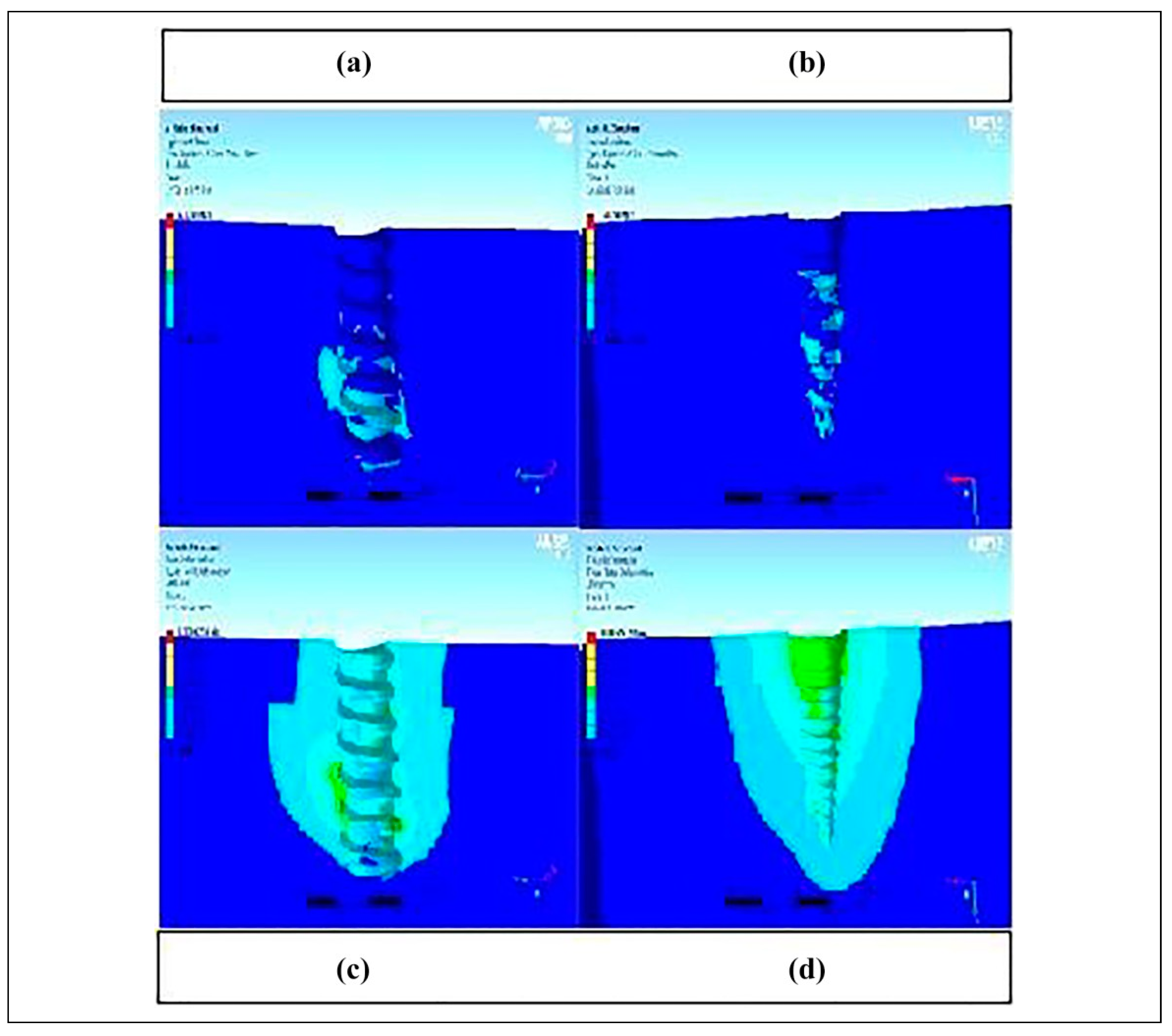
The stress changes occurring at the screw–bone interface while inserting/driving the screw within the bone are one of the factors for spinning, loosening, or fracture of the screw. In the present study, the Von Mises stress and deformation at the screw–bone interface of torque test was largely distributed around the crestal and body region in self-tapping screw model, and at the apical region, in case of self-drilling screw at a given amount of force indicating minimal damage to the surrounding bone in the later model. In the field of neurosurgery, a comparison between self-drilling and self-tapping screws was done to assess their efficacy in terms of insertion torque and pullout strength on cadaveric cervical vertebrae with MTS systems corporation. They found no significant difference in pullout strength between the screw designs of any length, but the density of bone significantly influenced the screw performance.[
7]
The pullout strength with self-tapping and self-drilling screws conducted at the AO center utilizing cadaver bone showed threefold increase in retentiveness of self-drilling screws when compared with self-tapping screws in the cancellous bone, and this is presumably due to compression of bone rather than cutting the bone around the threads of the screws[
8]
The pullout strength in the present study showed lesser degree of stress concentration and deformation at the screw–bone interface with the self-drilling screw model as compared to the self-tapping screw model. This indicates lesser degree of bone resorption and failure of implants with self-drilling screws.
The failure of osteosynthesis was attributed to loosening of the screws and loss of anchorage between the plate and the screws. A study was done to assess the efficacy of plate retention with the help of self-drilling screws that suggested the best resistance offered at a maximum force, that is, self-drilling screw could withstand slightly more load by increasing the anchorage in bone.[
9]
Higher stress and deformational values at given amount of torsion were observed at the apical region of the self-drilling screw in contrast to the entire length of the self-tapping screw, we could infer that there could be less chance of screw loosening with self-drilling screws. Torsional effect at the screw–plate–bone interface in the present study showed slightly higher stress and deformational values with self-drilling screws at given amount of torsion, but it was observed only at the apical region with negligible changes along the entire length of screw unlike with self-tapping screw indicating lesser chance of screw loosening or screw fatigue and fracture.