Hemorrhage in Onodi Cell Leading to Traumatic Optic Neuropathy
Abstract
:Introduction
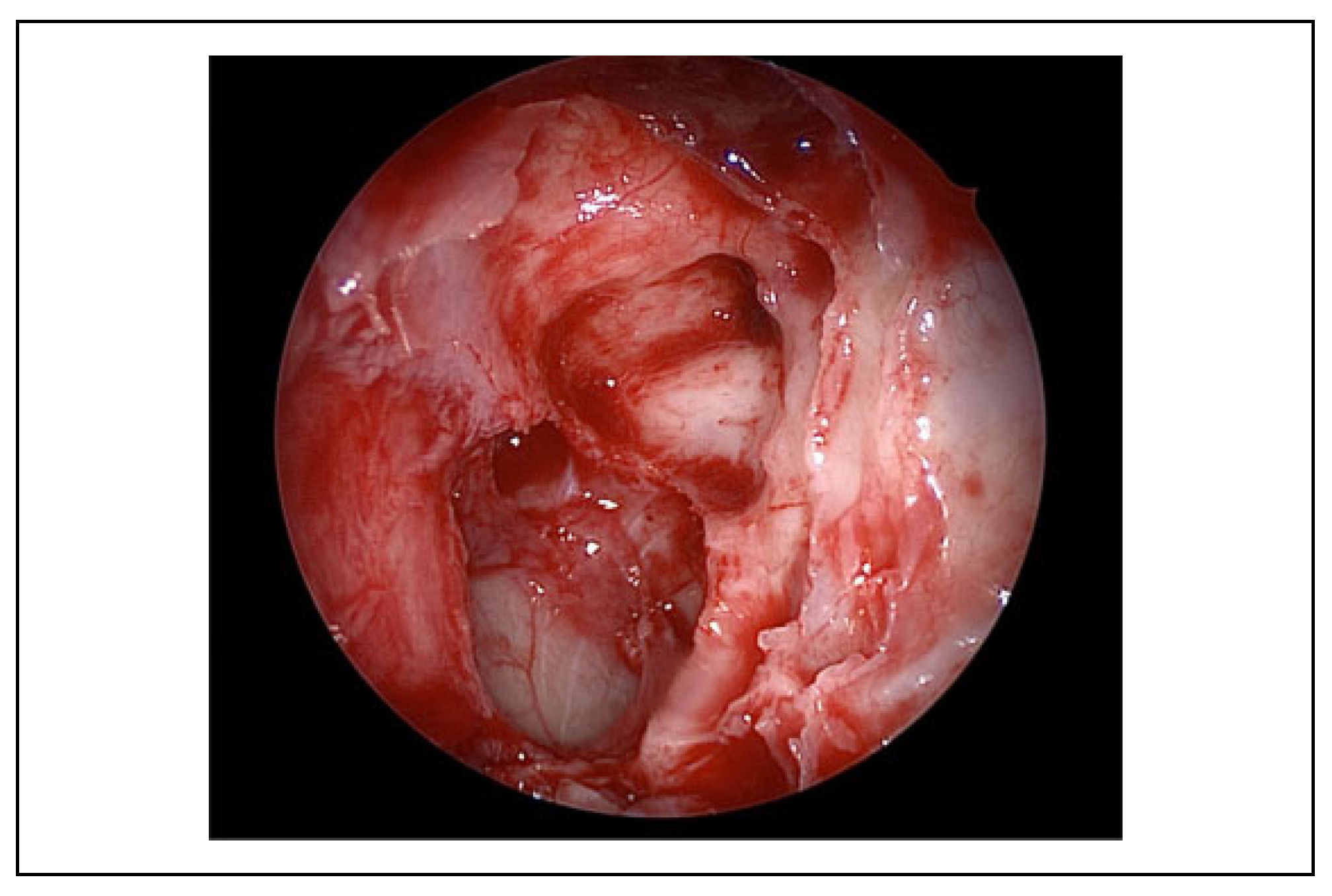
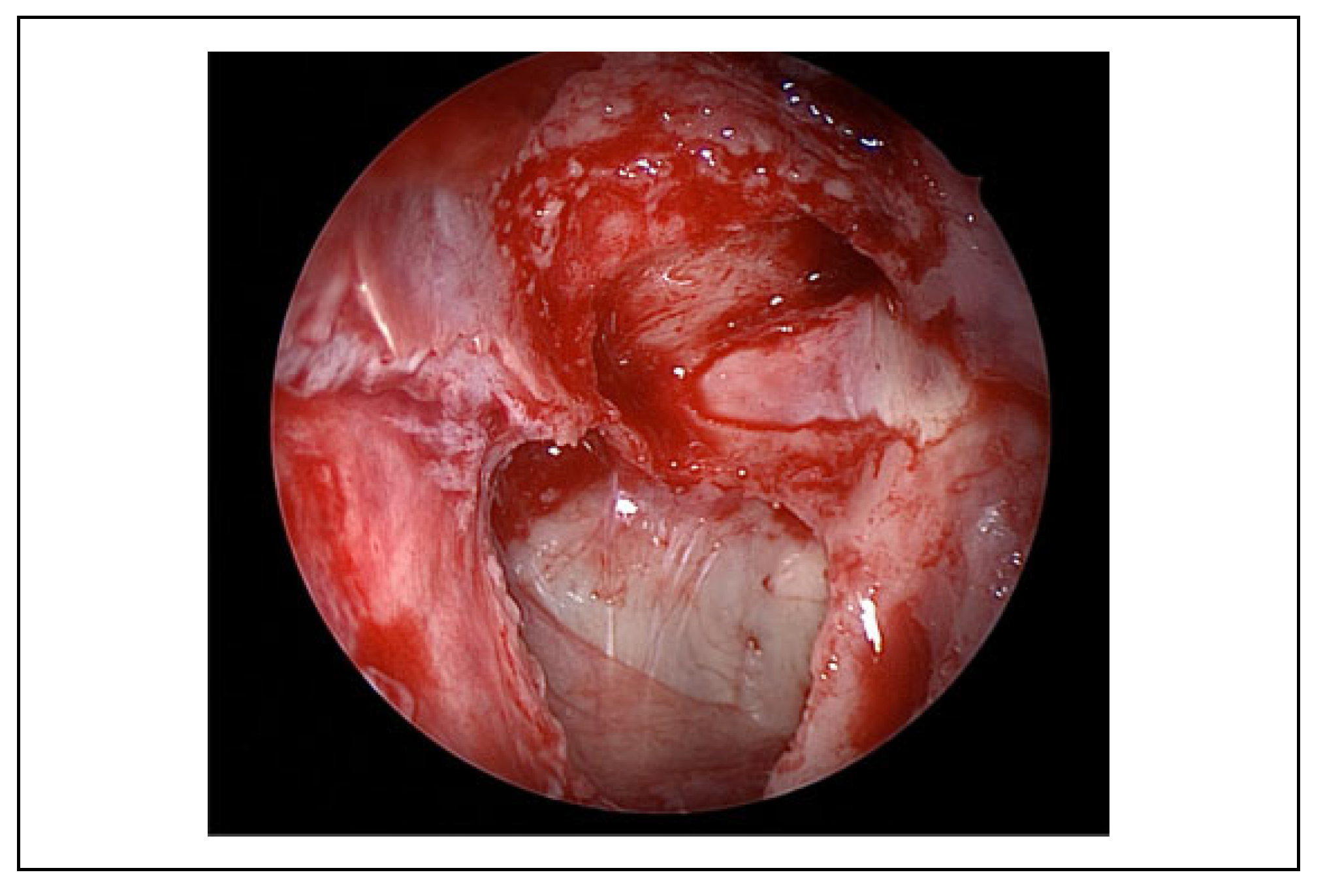
Case Description
Discussion
Conclusion
Funding
Conflicts of Interest
References
- Steinsapir, K.D.; Goldberg, R.A. Traumatic optic neuropathy. Surv Ophthalmol. 1994, 38, 487–518. [Google Scholar] [PubMed]
- Bracken, M.B.; Shepard, M.J.; Collins, W.F.; et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med. 1990, 322, 1405–1411. [Google Scholar] [PubMed]
- Levin, L.A.; Beck, R.W.; Joseph, M.P.; Seiff, S.; Kraker, R. The treatment of traumatic optic neuropathy—the International Optic Nerve Trauma Study. Ophthalmology. 1999, 106, 1268–1277. [Google Scholar] [CrossRef] [PubMed]
- Yu-Wai-Man, P.; Griffiths, P.G. Surgery for traumatic optic neuropathy. Cochrane Database Syst Rev. 2005, 4, CD005024. [Google Scholar]
- Emanuelli, E.; Bignami, M.; Digilio, E.; Fusetti, S.; Volo, T.; Castelnuovo, P. Post-traumatic optic neuropathy: our surgical and medical protocol. Eur Arch Otorhinolaryngol. 2015, 272, 3301–3309. [Google Scholar] [CrossRef] [PubMed]
- Dawoud, M.; Salama, A.; Elatif, H.A.; Ghoneim, A. The role of multidetector computed tomography in the diagnosis of traumatic orbital lesions in emergent settings. Tanta Med J. 2015, 43, 60–65. [Google Scholar]
- Yoshida, K.; Wataya, T.; Yamagata, S. Mucocele in an Onodi cell responsible for acute optic neuropathy. Br J Neurosurg. 2005, 19, 55–56. [Google Scholar] [PubMed]
- Cherla, D.V.; Tomovic, S.; Liu, J.K.; Eloy, J.A. The central Onodi cell: a previously unreported anatomic variation. Allergy Rhinol (Providence). 2013, 4, e49–e51. [Google Scholar] [PubMed]
- Yanagisawa, E.; Weaver, E.M.; Ashikawa, R. The Onodi (sphenoethmoid) cell. Ear Nose Throat J. 1998, 77, 578–580. [Google Scholar] [CrossRef] [PubMed]




© 2020 by the author. The Author(s) 2020.
Share and Cite
Mehta, A.; Rathod, R.; Ahuja, C.; Singh, M.; Virk, R.S. Hemorrhage in Onodi Cell Leading to Traumatic Optic Neuropathy. Craniomaxillofac. Trauma Reconstr. 2021, 14, 70-73. https://doi.org/10.1177/1943387520922021
Mehta A, Rathod R, Ahuja C, Singh M, Virk RS. Hemorrhage in Onodi Cell Leading to Traumatic Optic Neuropathy. Craniomaxillofacial Trauma & Reconstruction. 2021; 14(1):70-73. https://doi.org/10.1177/1943387520922021
Chicago/Turabian StyleMehta, Aditi, Ramya Rathod, Chirag Ahuja, Manpreet Singh, and Ramandeep S. Virk. 2021. "Hemorrhage in Onodi Cell Leading to Traumatic Optic Neuropathy" Craniomaxillofacial Trauma & Reconstruction 14, no. 1: 70-73. https://doi.org/10.1177/1943387520922021
APA StyleMehta, A., Rathod, R., Ahuja, C., Singh, M., & Virk, R. S. (2021). Hemorrhage in Onodi Cell Leading to Traumatic Optic Neuropathy. Craniomaxillofacial Trauma & Reconstruction, 14(1), 70-73. https://doi.org/10.1177/1943387520922021


