The Use of a Novel CAD-CAM Splint to Simplify Open Reduction and Internal Fixation of Mandibular Angle Fracture: A Technical Note
Abstract
Introduction
Case Report
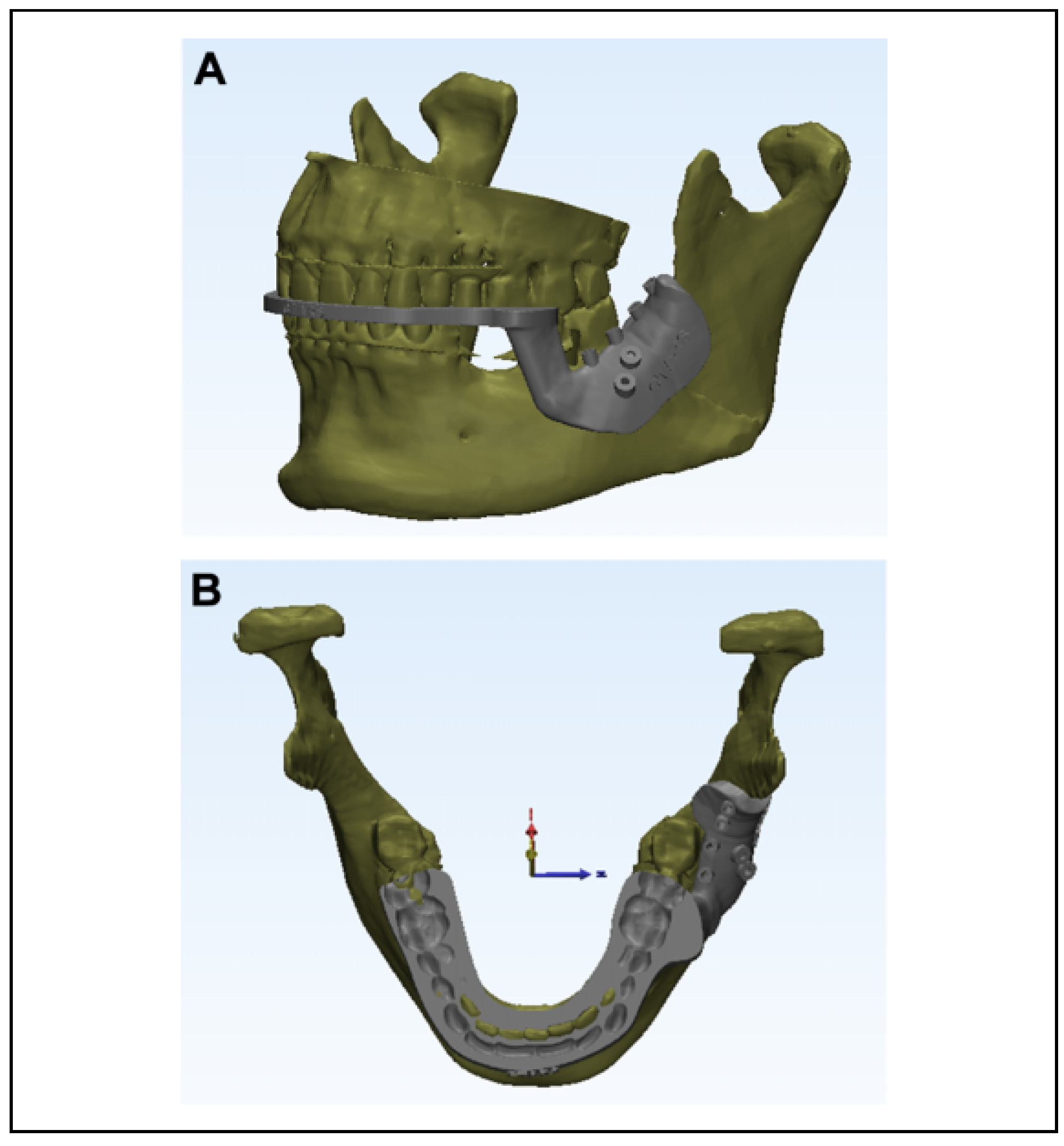
Preoperative Fabrication of Splint and Surgical Guide by CAD/CAM Technique
Intraoperative Procedure
Postoperative Outcome
Discussion
Conclusion
Funding
Acknowledgments
Conflicts of Interest
References
- Elavenil, P.; Mohanavalli, S.; Sasikala, B.; Prasanna, R.; Krishnakumar, R. Isolated bilateral mandibular angle fractures: An extensive literature review of the rare clinical phenomenon with presentation of a classical clinical model. Craniomaxil- lofac Trauma Reconstr. 2015, 8, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E.I.I.I. Treatment methods for fractures of the mandibular angle. Int J Oral Maxillofac Surg. 1999, 28, 243–252. [Google Scholar] [CrossRef] [PubMed]
- Wan, K.; Williamson, R.A.; Gebauer, D.; Hird, K. Open reduction and internal fixation of mandibular angle fractures: Does the transbuccal technique produce fewer complications after treatment than the transoral technique? J Oral Maxillofac Surg. 2012, 70, 2620–2628. [Google Scholar] [CrossRef] [PubMed]
- Seemann, R.; Schicho, K.; Wutzl, A.; et al. Complication rates in the operative treatment of mandibular angle fractures: A 10-year retrospective. J Oral Maxillofac Surg. 2010, 68, 647–650. [Google Scholar] [CrossRef] [PubMed]
- Hsu, E.; Crombie, A.; To, P.; Marquart, L.; Batstone, M. Manual reduction of mandibular fractures before internal fixation leads to shorter operative duration and equivalent outcomes when compared with reduction with intermaxillary fixation. J Oral Maxillofac Surg. 2012, 70, 1622–1626. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.; Cleaton-Jones, P.; Lownie, J. Relative efficiencies of various wiring configurations commonly used in open reduc- tions of fractures of the angle of the mandible. Oral Surg Oral Med Oral Pathol. 1990, 70, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Batbayar, E.; Van Minnen, B.; Bos, R. Non-IMF mandibular fracture reduction techniques: A review of the literature. J Craniomaxillofac Surg. 2017, 45, 1327–1332. [Google Scholar] [CrossRef] [PubMed]
- el-Gengehi, M.; Seif, S. Evaluation of the accuracy of computer-guided mandibular fracture reduction. J Craniofac Surg. 2015, 26, 1587–1591. [Google Scholar] [CrossRef] [PubMed]
- Mimi, M.; Mizuno, A.; Nakano, Y.; Motegi, K. Reduction and fixation of jaw fractures using acrylic splints. Br J Oral Max- illofac Surg. 1989, 27, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Luebbers, H.; Politis, C. Three-dimensional virtual model surgery to fabricate the digital intermediate splint. J Craniofac Surg. 2013, 24, 563–565. [Google Scholar] [CrossRef] [PubMed]
- Aboul-Hosn Centenero, S.; Herna´ndez-Alfaro, F. 3D planning in orthognathic surgery: CAD/CAM surgical splints and prediction of the soft and hard tissues results—Our experience in 16 cases. J Cranio-Maxillo-Facial Surg. 2012, 40, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Choi, B.; Nam, O.; Kwon, Y. Minimal invasive treatment using patient-specific template for mandibular fractures in children: “Wing-splint” by CAD/CAM technology. Br J Oral Maxillofac Surg. 2016, 54, 1140–1141. [Google Scholar] [CrossRef] [PubMed]
- Levine, J.; Patel, A.; Saadeh, P.; Hirsch, D. Computer-aided design and manufacturing in craniomaxillofacial surgery. J Craniofac Surg. 2012, 23, 288–293. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Frost, C.; Cusano, A.; Dorafshar, A. Management of bilateral edentulous mandible fractures through an intraoral approach using CAD/CAM technology: A case report. J Oral Maxillofac Surg. 2018, 76, e1–e1056. [Google Scholar] [CrossRef] [PubMed]






© 2020 by the author. The Author(s) 2020.
Share and Cite
Ramanathan, M.; Panneerselvam, E.; Ganesh, S.K.; Raja, K.K. The Use of a Novel CAD-CAM Splint to Simplify Open Reduction and Internal Fixation of Mandibular Angle Fracture: A Technical Note. Craniomaxillofac. Trauma Reconstr. 2021, 14, 74-78. https://doi.org/10.1177/1943387520904897
Ramanathan M, Panneerselvam E, Ganesh SK, Raja KK. The Use of a Novel CAD-CAM Splint to Simplify Open Reduction and Internal Fixation of Mandibular Angle Fracture: A Technical Note. Craniomaxillofacial Trauma & Reconstruction. 2021; 14(1):74-78. https://doi.org/10.1177/1943387520904897
Chicago/Turabian StyleRamanathan, Mrunalini, Elavenil Panneerselvam, Sriraam Kasi Ganesh, and Krishna Kumar Raja. 2021. "The Use of a Novel CAD-CAM Splint to Simplify Open Reduction and Internal Fixation of Mandibular Angle Fracture: A Technical Note" Craniomaxillofacial Trauma & Reconstruction 14, no. 1: 74-78. https://doi.org/10.1177/1943387520904897
APA StyleRamanathan, M., Panneerselvam, E., Ganesh, S. K., & Raja, K. K. (2021). The Use of a Novel CAD-CAM Splint to Simplify Open Reduction and Internal Fixation of Mandibular Angle Fracture: A Technical Note. Craniomaxillofacial Trauma & Reconstruction, 14(1), 74-78. https://doi.org/10.1177/1943387520904897


