Abstract
Study Design: Retrospective cohort study. Objective: The purpose of this study was to evaluate and share our experience with the surgery first approach (SFA) for correction of skeletal malocclusion. Methods: After consultation with the department of orthodontics, 45 patients with skeletal malocclusions suitable to undergo SFA were enrolled in this study (14 bimaxillary protrusion and 31 skeletal class III malocclusion). Le Fort I maxillary osteotomy, bilateral sagittal split ramus osteotomy, subapical osteotomy, and genioplasty were performed as required. After a healing period of 2 weeks, postoperative orthodontic treatment was started to achieve the final occlusion. Results: The mean duration of postoperative orthodontic treatment was 15.2 months, which is much shorter than the conventional orthodontic first approach (OFA) where presurgical orthodontic duration alone takes 12-24 months according to an individual. In the bimaxillary protrusion group, it was 18 months, which was significantly longer than for the other group (P < .05). Conclusions: SFA offers an efficient alternative to conventional OFA with shorter total treatment duration, immediate marked improvement in facial profile, reduced biological costs, and similar operative stability. However, it comes at the cost of heightened challenges regarding case selection, accurate prediction, and surgical precision. With a joint venture between skilled and experienced surgeons and orthodontists, the outcome can be very promising.
1. Introduction
Orthognathic surgery is now a well-established and commonly used treatment approach for patients with skeletal discrepancies beyond the scope of routine orthodontic treatment. Hullihen in 1849 was the first to perform the orthognathic surgery for correction of mandibular prognathism. However, it was in 1957 when Trauner and Obwegeser successfully performed bilateral sagittal split osteotomy of the mandible which marked the beginning of modern era of orthognathic surgery.[1] Since then several additions and modifications have been introduced to improvise the outcome.
It was not until the early 1970s that presurgical orthodontics started to being routinely practiced mainly due to the increased desire of the surgeons and patients for optimal esthetic and occlusal results.[2] This “orthodontics first” concept was expanded to all orthognathic cases, including mandibular prognathism, mandibular retrognathism, and vertical skeletal discrepancy with anterior open bite or deep bite, and emphasized that optimal surgical repositioning of the jaw is only possible following the removal of all dental compensation prior to surgery.[3] But with this approach, tremendous patience was needed to finally achieve the desired outcome of treatment. Later, a surgery was performed for correction of skeletal class III without orthodontic preparation, followed by regular postoperative dental alignment. This approach was termed as “surgery first.”[4] There was a significant decrease in the overall treatment period and the patient greatly appreciated the immediate profile improvement after surgery. Thereafter, similar approach was applied for bimaxillary orthognathic surgery.[5]
2. Patients and Methods
This retrospective cohort study was conducted after prior approval from the Institutional Ethical Committee following the Declaration of Helsinki. Data were extracted from the medical records of 45 patients treated with surgery first approach (SFA) between January 2015 and December 2018: 14 bimaxillary protrusion and 31 skeletal class III malocclusion cases (Table 1). Among them, 28 were females and 17 were males with a mean age of 21.9 years.

Table 1.
Patient characteristics.
On the basis of clinical data, dental models, and cephalometric analysis, SFA was planned. Presurgical orthodontic alignment was avoided in all cases. A splint was made following model surgery. Then the orthognathic surgery was performed under general anesthesia. Le Fort I maxillary osteotomy, sagittal split ramus osteotomy, subapical osteotomy, and genioplasty were performed as required (Table 2 and Table 3; Figure 1 and Figure 2). Intraoperative teeth extraction was done in cases requiring segmental osteotomy. There were no significant surgical complications. Orthodontic treatment was started after a postoperative healing period of 2 weeks and the duration of postoperative orthodontic treatment was recorded.

Table 2.
Surgical modalities for bimaxillary protrusion.

Table 3.
Surgical modalities for skeletal class III malocclusion.
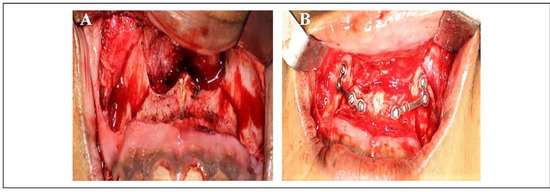
Figure 1.
Maxillary osteotomy (A) and stabilization (B).
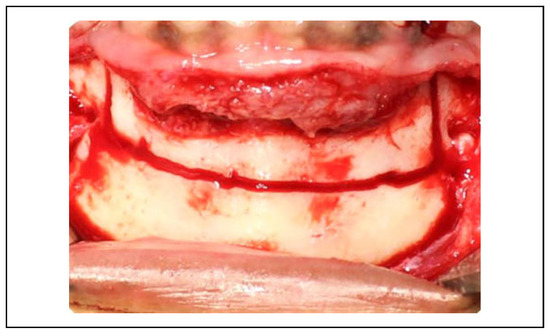
Figure 2.
Mandibular subapical osteotomy.
One-way analysis of variance was used for comparisons among the groups. The statistical analysis was performed using SPSS 20.0 software package. Significance was set at P < .05
3. Results
The mean duration of postoperative orthodontic treatment was about 15 months, which is much shorter than the conventional orthodontic first approach (OFA) where presurgical orthodontic duration alone takes 12-24 months according to an individual. In the bimaxillary protrusion group, it was 18 months, which was significantly longer than for the other group (P < .05). In those cases, following tooth extraction, space was created which needs to be closed. This might have increased the treatment duration. The end result was a satisfactory facial profile and occlusion (Figure 3 and Figure 4). No relapse was recorded during 6-12 months of follow-up.

Figure 3.
Comparison of frontal and lateral views of the facial profile: Pretreatment (A and B) and posttreatment (C and D).

Figure 4.
Comparison of occlusion: Pretreatment (A to C) and posttreatment (D to F).
4. Discussion
Conventional OFA is a three-staged treatment procedure, namely presurgical orthodontics, orthognathic surgical procedure, and postsurgical orthodontics.[6] The time period of presurgical orthodontic preparation greatly varies which may last 12-24 months.[7] Orthodontics prior to surgery reveals the true skeletal discrepancy and relieves dental compensation preoperatively. Decompensated arch allows to further setback the mandible compared to the compensated one. It also makes easier to fit the maxilla and mandible to a solid occlusion after surgery.[8] Next is the surgical phase where the actual orthognathic surgery is performed. This is followed by postsurgical orthodontic phase which lasts from 6 months up to 1 year.[9,10,11] The main aim is to finish and settle the occlusion. Also, minor surgical relapse can be managed during this period.
Although the conventional approach often produces satisfactory results and is considered routine, it has several drawbacks. The overall treatment time period is prolonged as it requires 2 phases of orthodontic therapy. Then there is temporary worsening of facial appearance and delay in addressing the chief complaint which is discouraging for the patient resulting poor compliance. The removal of natural dental compensation in these patients often results in advancement of the lower lip as well as retrusion of the upper lip which together accentuate the soft tissue disharmony.[12] Due to the long-term orthodontic preparation, there may be complications such as masticatory discomfort, dental caries, gingival recession, and root resorption as well.[13]
A new approach to correct dental and skeletal malocclusions: “the surgery first approach (SFA)” involves an orthognathic surgical intervention without presurgical step; the surgery of skeletal bases is performed as a first step and it is followed by postsurgical orthodontics, which is usually of very short duration.[4] Hence, the overall treatment duration is greatly reduced. Postsurgical orthodontic movement can be based on an already corrected skeletal pattern and does not interfere with compensatory biological responses. Also, some surgical relapse can be managed during this phase. However, in both SFA and OFA, cephalometric prediction is same, only order of procedure is different.
In SFA, the timing of orthognathic surgery is entirely up to the patient. It provides an opportunity to choose the timing of surgery to allow for the postoperative healing period as the orthognathic surgery precedes orthodontic treatment. Presurgical dentoalveolar decompensation is very difficult as it is opposite to the biological compensatory mechanism of hard and soft tissues.[14] With surgery first, there is simultaneous resolution of soft tissue and skeletal imbalance. This includes increased tone of the upper lip to maxillary incisors and tongue to mandibular incisors. Once the physiological restraints are relived, dental decompensation can be performed efficiently and effectively. Difficult dental movements, such as torque of the maxillary incisors, can be achieved through segmental osteotomies and repositioning of the skeletal segments.[15] Also, patients appreciate immediate improvement in facial appearance, thus avoiding the exacerbation of their profiles and occlusions.
By far the most important reason for popularity of SFA is the much shorter total treatment time than the conventional approach. Presurgical tooth movement and alignment is the most time consuming and bothersome phase. Tooth movement becomes much faster and efficient following surgery first. Much of this is due to the regional accelerated phenomenon (RAP). RAP is a tissue reaction to a noxious stimulus that increases the healing capacities of the affected tissues. It is typical not only of hard tissues, such as bone and cartilage, but also of soft tissues.[16] Orthodontists can utilize this period of rapid metabolic activity within the tissues for efficient and accelerated tooth movement by performing surgery first. To utilize the maximum potential of the RAP, two jaw surgeries are preferred. Alveolar osteotomy procedures increase cortical bone porosity and decrease resistance to tooth movement.[17] During healing process postsurgery, there is increased blood flow above the presurgical levels that facilitates healing process and stimulates bone turnover. This speeds up the orthodontic tooth movement.[18] Orthognathic surgery triggers 3-4 months of higher osteoclastic activity and metabolic changes (Ca depletion) in dentoalveolus.[19] This window period can be utilized for orthodontic treatment to its fullest only with SFA. In addition to this, in SFA, the unlikely event of a surgical error and a possible postsurgical relapse can be compensated during the postsurgical orthodontics. Also, studies have shown stability of results equal to, or in some cases superior to, those achieved using the more traditional OFA.[9,20]
Published reports include SFA for almost every type of malocclusion and dentofacial deformity that do not require too much presurgical orthodontic alignment/decompensation and also depending on the specific characteristics.[12] In ideal situation, the malocclusion accompanying the skeletal deformity represents mild to moderate crowding, a flat to mild curve of Spee, normal to mild proclination and retroclination of upper and lower incisors, and minimal transverse discrepancies. The major indications include skeletal class II/III malocclusion, skeletal open bite, bimaxillary protrusion, and facial asymmetry. It is also applied to correct maxillary hypoplasia and its associated complications like obstructive sleep apnea (OSA), orofacial clefts, and maxillary atrophy. Even though the surgery first technique can be applied to class II as well as class III malocclusions, the majority of cases treated using this approach have been cases with class III malocclusion meeting the above criteria.[9,12] A possible explanation is that a class III skeletal relationship results in a more pronounced soft tissue imbalance. Often, class II skeletal deformities can be masked as the patient shifts the mandible forward, but the equivalent backward shift of the mandible to mask class III deformities is physically impossible. In the traditional approach, decompensation of the arches results in an even more disfiguring profile for class III patients. Hence, these patients seem to see the benefit of the SFA to a greater extent than class II cases. It is also likely that for class II patients, advancing a retrognathic mandible into the correct position will create an anterior crossbite temporarily worsening the patient’s appearance until orthodontic treatment can upright and retract the lower incisors.
Maxillomandibular advancement is an invasive yet potentially effective surgical option in the treatment of OSA for patients who have difficulty tolerating continuous positive airway pressure and whose OSA has been refractory to other surgical modalities. In sleep disordered breathing (stage of OSA) cases, SFA using early advancement procedures helps immediately increase dimension of upper airway and facilitate breathing.
SFA is mainly contraindicated in cases of skeletal malocclusion with severe crowding. It is not widely used in class II cases, especially class II division 2 with deep overbite, because advancing a retrognathic mandible into correct position will create an anterior crossbite which temporarily worsens the patient’s appearance. This contradicts the principle of SFA.[6,15] SFA is also avoided in cases of severe transverse discrepancy. Cleft lip and palate is associated to significant skeletal class III, narrow dental arch, and palatal collapse. Conventionally, this is corrected by performing Le Fort I osteotomy with advancement. However, there are high rates of relapse. Therefore, segmental Le Fort I osteotomy with orthodontic rapid palatal expansion is widely being performed nowadays.[9]
While significantly reducing treatment time, the SFA has several disadvantages. First of all, it is a complicated approach that requires high expertise and experience of both surgeons and orthodontists. Even minutest error in treatment planning and predicting occlusion can be difficult to correct. From an orthodontist’s point of view providing precise diagnosis, detailed treatment planning and skillful orthodontic treatment is more demanding using SFA than traditional OFA.[21] Predicting the final occlusion is the hardest challenge with SFA as occlusion cannot serve as a guide due to multiple dental interferences at the beginning of pre-op treatment plan. Cases requiring extractions are especially very difficult to plan when performing surgery first. This limits SFA to cases that need less leveling, alignment, and decompensation. Hence, the most important step is case selection.
Even after the final occlusion has been determined carefully by the orthodontist, surgical perfection is must since any minor surgical error can compromise the final result. Skeletal components must be arranged to match the skeletal positions and occlusion precisely. It is difficult to perform disgrated osteotomy and intermaxillary fixation (IMF) without occlusal bite plane on malaligned arches and provide stability after skeletal reposition.
It is a Herculean task to obtain a stable occlusion immediately after orthognathic surgery without presurgical orthodontics. Factors causing instability in the SFA include a larger overbite, a deeper curve of Spee, a greater negative overjet, and a greater mandibular setback. The initial overbite may be an indicator of a possible skeletal relapse of the mandibular setback.[22] Also, the mandible tends to rotate counterclockwise more in SFA group, which indicate a poorer postoperative stability than in conventional group.
Although total treatment duration is shortened in SFA, the treatment planning becomes bothersome and more time consuming, so does the postoperative orthodontic phase. Timing of surgery relates to jaw growth.[20] So, patients would have to delay correction (surgical) until adolescent mandibular growth completes. The rate of complication related to SFA may be slightly higher than those associated with traditional orthognathic surgery, since the rate of complications of segmental osteotomies must be added to the complication rate of basal osteotomies. Severe transverse discrepancies sometimes lead to two-piece or three-piece Le Fort I osteotomies. The increase in number and complexity of osteotomy procedures poses a greater risk to the patient. This also indicates that skilled surgeons are required to perform these surgeries meticulously.
5. Conclusion
Orthognathic surgery is performed to fulfil more of an esthetic than functional need. Patient’s chief complaint and expectation should be clear from the very beginning and given the topmost priority during treatment planning while avoiding false assurance. In this era where time means money, results need to be achieved within least possible duration. However, treatment quality cannot be compromised. In this regard, the surgery first approach has added a new dimension in the field of orthognathic surgery. It offers an efficient alternative to conventional OFA with shorter total treatment duration, immediate marked improvement in facial profile, reduced biological costs, similar operative stability, and other surgical results. However, it comes at the cost of heightened challenges regarding case selection, accurate prediction, and surgical precision. With a joint venture between skilled and experienced surgeons and orthodontists, the outcome can be very promising.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Trauner, R.; Obwegeser, H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1957, 10, 677–689. [Google Scholar]
- Worms, F.W.; Meskin, L.H.; Isaacson, R.J. Open-bite. Am J Orthod. 1971, 59, 589–595. [Google Scholar] [PubMed]
- Worms, F.W.; Isaacson, R.J.; Speidel, T.M. Surgical orthodontic treatment planning: profile analysis and mandibular surgery. Angle Orthod. 1976, 46, 1–25. [Google Scholar] [PubMed]
- Nagasaka, H.; Sugawara, J.; Kawamura, H.; Nanda, R. “Surgery first” skeletal class III correction using the skeletal anchorage system. J Clin Orthod. 2009, 43, 97–105. [Google Scholar]
- Alfaro, F.H.; Martinez, R.G.; Coral, A.M.; Escriche, C.B. “Surgery first” in bimaxillary orthognathic surgery. J Oral Maxillofac Surg. 2011, 69, e201–e207. [Google Scholar]
- Uribe, F.; Adabi, S.; Janakiraman, N.; et al. Treatment duration and factors associated with the surgery-first approach: a twocenter study. Prog Orthod. 2015, 16, 29–32. [Google Scholar]
- Luther, F.; Morris, D.O.; Hart, C. Orthodontic preparation for orthognathic surgery: How long does it take and why? A retrospective study. Br J Oral Maxillofac Surg. 2003, 41, 401–406. [Google Scholar]
- Chiu, Y.T.; Huang, C.S.; Ko, E.W.C.; Chen, Y.R. Presurgical orthodontics versus no presurgical orthodontics: treatment outcome of surgical-orthodontic correction for skeletal class III open bite. Plast Reconstr Surg. 2010, 126, 2074–2083. [Google Scholar]
- Huang, C.S.; Hsu, S.S.; Chen, Y.-R. Systematic review of the surgery–first approach in orthognathic surgery. Biomed J. 2014, 37, 184–190. [Google Scholar]
- Dowling, P.A.; Espeland, L.; Krogstad, O.; Stenvik, A.; Kelly, A. Duration of orthodontic treatment involving orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1999, 14, 146–152. [Google Scholar]
- Diaz, P.M.; Garcia, R.G.; Gias, L.N.; et al. Time used for orthodontic surgical treatment of dentofacial deformities in white patients. J Oral Maxillofac Surg. 2010, 68, 88–92. [Google Scholar] [PubMed]
- Zeitoun, D. Surgery first: Which protocols for which results? J Dentofacial Anom Orthod. 2017, 20, 407–422. [Google Scholar]
- Sugawara, J. Surgery-first approach vs traditional approach. Am J Orthodon and Orthopaed Society. 2013, 25, 537–544. [Google Scholar]
- Ko, E.W.; Lin, S.C.; Chen, Y.R.; Huang, C.S. Skeletal and dental variables related to the stability of orthognathic surgery in skeletal class III malocclusion with a surgery-first approach. J Oral Maxillofac Surg. 2013, 71, e215–e223. [Google Scholar]
- Wirthlin, J.O.; Shetye, P.R. Orthodontist’s role in orthognathic surgery. Semin Plast Surg. 2013, 27, 137–144. [Google Scholar]
- Verna, C. Regional acceleratory phenomenon. Front Oral Biol. 2016, 18, 28–35. [Google Scholar]
- Wilcko, M.T.; Wilcko, W.M.; Pulver, J.J.; Bissada, N.F.; Bouquot, J.E. Accelerated osteogenic orthodontics technique: a 1-stage surgically facilitated rapid orthodontic technique with alveolar augmentation. J Oral Maxillofac Surg. 2009, 67, 2149–2159. [Google Scholar]
- Justus, T.; Chang, B.I.; Bloomquist, D.; Ramsay, D.S. Human gingival and pulpal blood flow during healing after Le Fort I osteotomy. J Oral Maxillofac Surg. 2001, 59, 2–7. [Google Scholar]
- Sebaoun, J.D.; Ferguson, D.J.; Wilcko, M.T.; Wilcko, W.M. Alveolar osteotomy and rapid orthodontic treatments. Orthod Fr. 2007, 78, 217–225. [Google Scholar]
- Yang, L.; Xiao, Y.; Liang, Y.; Wang, X.; Li, J.V.; Liao, G. Does the surgery-first approach produce better outcomes in orthognathic surgery? A systematic review and meta-analysis. J Oral Maxillofac Surg. 2017, 75, 2422–2429. [Google Scholar]
- Hernandez-Alfaro, F.; Guijarro-Martinez, R.; Peiro-Guijarro, M.A. Surgery first in orthognathic surgery: What have we learned? A comprehensive workflow based on 45 consecutive cases. J Oral Maxillofac Surg. 2014, 72, 376–390. [Google Scholar] [CrossRef]
- Baek, S.H.; Ahn, H.W.; Kwon, Y.H.; Choi, J.Y. Surgery first approach in skeletal class III malocclusion treated with 2jaw surgery: evaluation of surgical movement and postoperative orthodontic treatment. J Craniofac Surg. 2010, 21, 332–338. [Google Scholar]
© 2020 by the author. The Author(s) 2020.