Abstract
Study Design: Mandibular reconstruction is a challenge. Several reconstructive techniques are available, and the individualization of choice for each patient leads to better results and quality of life for the individual. Objective: The aim of this study is to evaluate the characteristics and complications of cases submitted to mandibular reconstruction with autogenous bone graft block of the iliac crest. Methods: Records of 45 patients undergoing mandibular reconstruction with autogenous bone graft block of the iliac crest were analyzed from January 2000 to December 2014. The data collected included age, gender, etiology and graft size, surgical approach, complications, comorbidities, and habits and addictions. Analysis of variance, chi-square test, and Fisher exact test were used for analysis of the variables with a significance level of P < .05. Results: The success rate of the 45 charts analyzed was 75.6%. No statistical differences were found between age and presence of complications, between defect size and presence or absence of complications, and between type of surgical approach and presence or absence of complications. Conclusion: According to our study, medical history may influence postoperative complications and require attention, though further studies should be performed to further elucidate the relationship between diseases and postoperative complications.
Introduction
Mandibular reconstruction is a challenge due to the complexity of its 3-dimensional structure and its involvement with facial aesthetics and function of the stomatognathic system. Currently, several reconstructive techniques are available, and the individualization of choice for each patient leads to better results and quality of life for the individual.
The choice of the best method for mandibular reconstruction is determined by the size, type, and topography of the defect and the conditions at the receptor site. The critical principles of reconstruction are avoiding oral contamination and maintaining bone graft stability during the initial healing phase to avoid increased failure rates caused by infection, fibrous nonunion, and bone graft resorption.[1,2,3,4,5,6]
Its main advantages include bone availability, good quality bone tissue with the presence of cortical and medullary bone, and its curved side surface, and when required, the tricortical graft can be withdrawn.[7,8,9,10,11,12]
Epidemiological studies facilitate understanding of the prevalence, extent, and severity of oral diseases in a population. They allow the implementation of preventive measures to ensure the reduction of the number of cases as well as improve the quality of life of the assisted population. Therefore, the aim of this study is to evaluate the characteristics and complications of cases submitted to mandibular reconstruction with autogenous bone graft of the iliac crest in the Maxillofacial Surgery Service, Department of Surgery, Santa Casa de Sa˜o Paulo.
Methods
After ethical approval (CAE 57962016.0.0000.5479), this observational and retrospective study was conducted in accordance with the Declaration of Helsinki guidelines and according to STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) initiative.
Data from medical records of patients referred to the Department of Surgery, Santa Casa de Sa˜o Paulo, Sa˜o Paulo/Brazil, from January 2000 to December 2014 were collected. Demographic (age and sex) and clinical data (etiology and size of the defect, surgical approach, complications, comorbidities, and habits and addictions [HA]) of 45 patients undergoing mandibular reconstruction using autograft were recorded.
The inclusion criteria were patient have been subjected to mandibular reconstruction with autogenous bone graft block of the iliac crest and there was a maintenance of periosteal barrier in all cases. The exclusion criteria were patients who were unable to undergo resection and those undergoing treatment for malignancy. Malignancies were excluded because most patients underwent postsurgery radiotherapy.
Surgeries were performed under general anesthesia. In cases of segmental defects, the mandibular reconstruction technique involved block graft and osteosynthesis with locking or nonlocking reconstruction plates fixed with at least 3 bicortically anchored screws in each segment (loadbearing). In cases of marginal defect reconstruction, graft fixation was performed with bone grafts supported with positional fixation.
All patients were reassessed regularly after surgery; the follow-up period varied from 6 to 24 months.
Data were initially described through absolute and percentage frequencies (qualitative variables). The analysis of variance test was used to assess the relationship between graft size and presence or complications (yes/no). The associations between qualitative variables were made using chisquare test and Fisher exact test, and all graphs were made with software R, version 3.2.1. Analyzes were made with Jasp 8.0, with a significance level of P < .05.
Results
Demographic Data
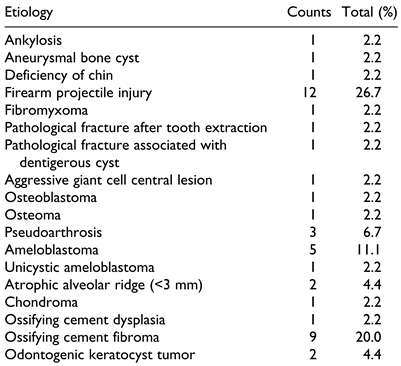
In the 45 charts analyzed, 25 patients were female, and 20 were male. Some records did not show all of the data, and statistical analyses were performed in accordance with each presented variable. The mean age was 38.1 years (ranging from 14-67). The etiology of the defect is given in Table 1.

Table 1.
Etiology of Mandibular Defects.
Clinical Data
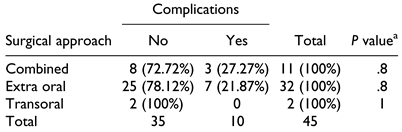
Access was extraoral in 32 (71.11%) patients, intraoral in 2 (4.44%), and combined in 11 (24.44%). Regarding the time of reconstruction, it was performed at the time of resection (ie, primary) in 19 (42.2%) patients and secondary to resection in 26 (57.8%) patients. The success rate was 75.6%; complications are detailed in Table 2.

Table 2.
Type of Complications Before Mandibular Reconstruction.
Another relationship analyzed was that between HA and medical histories (MH) of patients who had complications. No significant differences were found in relation to HA (P ¼ .079). Smokers and patients with positive MH accounted for 46.2% and 13.5% of the sample, respectively. No significant differences were observed between men and women (P ¼ .262).
No relationship was observed between age and incidence of complications, as shown in Figure 1. The mean defect size was 3.70 cm, ranging from 8 to 1.5 cm. No relationship was observed between defect size and incidence of complications (Figure 2). The number of complications was not statistically significant in relation to the type of surgical approach (Table 3).
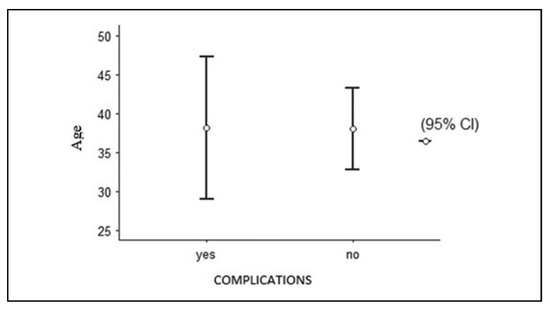
Figure 1.
Age versus complications.
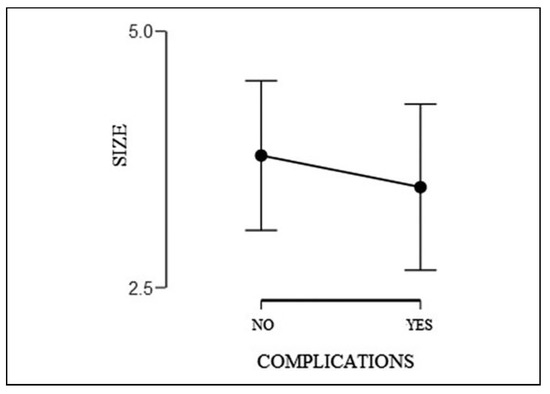
Figure 2.
Defect size (cm) versus complications.

Table 3.
Absence or Presence of Complications According to the Surgical Approach.
Discussion
Autogenous bone is often preferred over xenogeneic and allogeneic grafts due to its osteogenic, osteoinductive, and osteoconductive capacities. These properties make it an ideal graft material and the current standard to which all other grafts are compared.[11,12,13,14] Across the 14 years of this retrospective study, the success rate of the 45 charts analyzed was 75.6%.
Complications can arise and are inherent to both, the patient and the surgeon. It can also include the material used, inadequate surgical technique, failure of the covering tissue (wound dehiscence), failure in the fixing material, resorption, and infection. In the literature, there is no consensus in regard to the success and complication rates when using nonvascularized grafts: The success rate varies between 46% and 100%, and the complication rate ranges from 20% to 35%. One of the inclusion criteria in this study was the maintenance of periosteum, which acts as an osteogenic progenitor cell and provides a vascular supply for the newly formed bone. It is believed that, when intact, the periosteum provides a barrier against the infiltration of granulation tissue, thus creating a permissive environment for osteogenesis.[11,12,13,14] The authors reported complication rates of 17% in patients undergoing extraoral access and 38% in those undergoing intraoral access.
Chiapasco et al[14] reported only one case of a complication, infection with partial graft loss, among 14 mandibular reconstruction surgeries with free bone graft of the iliac crest. Zou et al[15] reconstructed mandibular defects with iliac crest bone grafts in 32 patients and reported 2 complications, both of which were wound dehiscence.
In a study of 51 patients, Ferretti et al[16] found that 45 had grafts that were considered to be successful at their 6-month review. Two of the patients required resection because their tumors recurred (the whole graft in 1 case and partial resection in the other). Four patients developed infection, which required local debridement with partial loss of the graft (for 2, the bone loss was not clinically significant, whereas for the other 2, a new graft was needed to increase the reconstructed area). Three patients lost the whole graft due to infection.
The authors stated that the main complication was dehiscence of intraoral suturing. Dehiscence occurs due to difficulty in covering the graft with soft tissue that is under stress, leading to eventual contamination. Moreover, the presence of dead spaces, saliva, and intraoral access may encourage the development of infection.
Controversy in the literature regarding the optimal timing of reconstruction in 2015, Schelieve and colleagues[1] concluded that primary reconstruction is a viable treatment option. This approach reduces the number of surgical interventions and the length of hospital stay, reduces the time in which the patient has a deformity and the morbidity that the loss of function entails, has a lower treatment cost, and facilitates rehabilitation and a faster return to social life. Authors who advocate secondary reconstruction argue that time is necessary for the healing of soft tissue, especially the oral mucosa, after resection and also in cases of associated infection.[3,4,5,6,7,8,9,10,11,12] However, primary reconstructions show significant advantages, such as the presence of sufficient tension-free soft tissue depending on the origin of the defect and the ease of positioning and shaping of the bone graft.
This type of graft has an advantage in terms of ease of modeling to the defect; however, there are restrictions to the use of large grafts. The use of these grafts has been recommended for defects of up to 6 cm. In 1997, Pogrel et al[8] published a study that evaluated the success rate of reconstructions with free graft and microvascularized flap and concluded that the graft can be used safely for reconstructions up to 6 cm in size. However, there is still controversy in the literature in regard to this factor, as in addition to defect size, the area where the graft will be performed may have an effect, site complications, and success, although there was a trend for more complications when the symphysis was involved. In a study on nonvascularized bone grafting for segmental reconstruction of the mandible, symphyseal involvement was significantly associated with failure. This study found no statistically significant differences in relation to defect size and patients with complications.
Patient-inherent factors (HA and MH) are also of paramount importance for a successful graft. It is known that the heat caused by smoking leads to delayed wound healing, as shown in the study of Levin and Schwartz-Arad.[17] Smoking is the factor most responsible for the loss of flaps in oral cavity reconstruction due to the sympathomimetic effects of nicotine, which lead to increased post-capillary pressure and decreased platelet survival. Furthermore, alcoholism can lead to dehydration and malnutrition, which also retard tissue healing.[1,18,19]
Although the results do not show a statistically significant difference in this study, from a total of 12 patients who had complications, 8 reported some type of habit or addiction (eg, smoking, alcohol, or illicit drugs). Lafrenie`re et al.[19] noted that there are some patient-inherent factors that increase the risk of infection in the postoperative period, such as hypertension, diabetes, and malnutrition. Therefore, blood pressure and blood glucose levels must be controlled preoperatively, along with the patient’s nutritional status (low serum albumin may represent an increased risk factor for postoperative infection, although it is not specific to nutritional deficiency). Patients with hyperglycemia can present electrolytic and dehydration disorders, which can also affect wound healing and predispose patients to infections and ketoacidosis. The preoperative glucose level should remain between 150 and 200 mg/dL.
In a study of 74 patients undergoing mandibular reconstruction with nonvascularized grafts, Gemert et al used extraoral access in 42 cases and intraoral access associated with combined access in 32 cases. The authors reported complication rates of 17% in patients undergoing extraoral access and 38% in those undergoing intraoral access. The authors stated that the main complication was dehiscence of intraoral suturing. In our study, there were no significant differences according to the access type used.[13]
The limitation of this study is its retrospective character. Patients were not randomly assigned to a type of reconstruction; this decision was based on the site and size of the defect.
Conclusion
According to our study covering a 14-year period, the factor that may influence postoperative complications is the patient’s medical history. Mandibular reconstruction with autogenous graft remains a viable option for the treatment of mandibular defects. Further studies should be conducted to address the importance of the relationship between complications and the patient.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
5498- Santa Casa de Miserico´rdia de Sa˜o Paulo; CAAE: 57962016.0.0000.5479.
References
- Schlieve, T.; Hull, W.; Miloro, M.; Kolokythas, A. Is immediate reconstruction of the mandible with nonvascularized bone graft following resection of benign pathology a viable treatment option? J Oral Maxillofac Surg. 2015, 73, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Tidstrom, K.D.; Keller, E.E. Reconstruction of mandibular discontinuity with autogenous iliac bone graft: report of 34 consecutive patients. J Oral Maxillofac Surg. 1990, 48, 336–346. [Google Scholar] [PubMed]
- Jewer, D.D.; Boyd, J.B.; Manktlow, R.T.; et al. Orofacial and mandibular reconstruction with the iliac crest free flap: a review of 60 cases and new method of classification. Plast Reconstr Surg. 1989, 84, 391–406. [Google Scholar] [CrossRef] [PubMed]
- Akinbami, B.O.; Akadiri, O.A. Reconstruction of the mandible following benign tumor ablations: an audit of 20 cases. J Oral Maxillofac Surg Med Pathol. 2015, 27, 650–655. [Google Scholar]
- González-García, R.; Naval-Gías, L.; Rodríguez-Campo, F.J.; Muñoz-Guerra, M.F.; Sastre-Pérez, J. Vascularized free fibular flap for the reconstruction of mandibular defects: clinical experience in 42 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008, 106, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Tin Goh, B.; Lee, S.; Tideman, H.; Stoelinga, P.J.W. Mandibular reconstruction in adults: a review. Int J Oral Maxillofac Surg. 2008, 37, 597–605. [Google Scholar]
- Foster, R.D.; Anthony, J.P.; Sharma, A.; Pogrel, M.A. Vascularized bone flaps versus nonvascularized bone grafts for mandibular reconstruction: an outcome analysis of primary bony union and endosseous implant success. Head Neck. 1999, 21, 66–71. [Google Scholar] [PubMed]
- Pogrel, M.A.; Podlesh, S.; Anthony, J.P.; Alexander, J. A comparison of vascularized and nonvascularized bone grafts for reconstruction of mandibular continuity defects. J Oral Maxillofac Surg. 1997, 55, 1200–1206. [Google Scholar] [CrossRef] [PubMed]
- Karagoz, H.; Eren, F.; Sever, C.; et al. Mandibular reconstruction after hemimandibulectomy. J Craniofac Surg. 2012, 23, 1373–1374. [Google Scholar] [PubMed]
- Olsson, A.B.; Kolokythas, A.; Reddi, S.P. Reconstructive surgery. J Oral Maxillofac Surg. 2012, 70, e272–e309. [Google Scholar] [PubMed]
- Louis, P.J. Bone grafting the mandible. Dent Clin North Am. 2011, 55, 209–227. [Google Scholar]
- Dasmah, A.; Thor, A.; Ekestubbe, A.; Sennerby, L.; Rasmusson, L. Particulate vs. block bone grafts: three-dimensional changes in graft volume after reconstruction of the atrophic maxilla, a 2-year radiographic follow-up. J Craniomaxillofac Surg. 2012, 40, 654–659. [Google Scholar] [CrossRef] [PubMed]
- Van Gemert, J.T.V.; Van Es, R.J.J.; Van Cann, E.M.; Koole, R. Nonvascularized bone grafts for segmental reconstruction of the mandible—a reappraisal. J Oral Maxillofac Surg. 2009, 67, 1446–1452. [Google Scholar] [PubMed]
- Chiapasco, M.; Colletti, G.; Romeo, E.; Zaniboni, M.; Brusati, R. Long-term results of mandibular reconstruction with autogenous bone grafts and oral implants after tumor resection. Clin Oral Implants Res. 2008, 19, 1074–1080. [Google Scholar] [PubMed]
- Zou, D.; Huang, W.; Wang, F. , et al. Autologous ilium grafts: long-term results on immediate or staged functional rehabilitation of mandibular segmental defects using dental implants after tumor resection. Clin Implant Dent Relat Res. 2015, 17, 779–789. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, C.; Muthray, E.; Rikhotso, E.; Reyneke, J.; Ripamonti, U. Reconstruction of 56 mandibular defects with autologous compressed particulate corticocancellous bone grafts. Br J Oral Maxillofac Surg. 2016, 54, 322–326. [Google Scholar] [PubMed]
- Levin, L.; Schwartz-Arad, D. The effect of cigarette smoking on dental implants and related surgery. Implant Dent. 2005, 14, 357–361. [Google Scholar] [CrossRef] [PubMed]
- August, M.; Tompach, P.; Chang, Y.; Kaban, L. Factors influencing the long-term outcome of mandibular reconstruction. J Oral Maxillofac Surg. 2000, 58, 731–737. [Google Scholar] [CrossRef]
- Lafrenière, R.; Bohnen, J.M.A.; Pasieka, J.; Spry, C. Infection control in the operating room: current practices or sacred cows? J Am Coll Surg. 2001, 193, 407–416. [Google Scholar] [PubMed]
© 2020 by the authors. The Authors 2020.