Abstract
Acromegaly is a medical condition where elevated growth hormone or insulin-like growth factor I levels cause several changes in the craniofacial soft and hard features. We report the correction of facial deformity and posterior open bite with Le Fort I and modified subcondylar osteotomies in a patient affected by acromegaly. Computer-aided design and manufacturing generated saw and drill guides were used to perform osteotomies and segment removal. The placement of the patient-specific implants (PSIs) was guided by predesigned drill holes ensuring the required and planned movement of the jaws and position of the PSIs. After segment removal, the PSIs fitted the predesigned drill holes with high precision and were secured without problems. The planned amount of mandibular and maxillary movement was achieved. The occlusion and osteotomies remained stable for the follow-up of 22 months. The use of PSIs combined with guided surgery can be beneficial for selected cases with asymmetry or posterior open bite enabling new approaches and yielding good functional and aesthetic outcome. The modification of conventional ramus osteotomy combined with utilization of ramus segment removal and the use of PSI for reposition is an interesting and promising technique for rare conditions with ramus height asymmetry.
Introduction
Acromegaly is a progressive medical condition characterized by excess secretion of growth hormone (GF) with raised insulin-like growth factor I (IGF-I) levels.[1] The cause of this disease in most of the patients is a GFsecreting pituitary adenoma, with an annual incidence of 3 to 4 cases per million and an estimated prevalence of 40 to 70 cases per million, with an average age at diagnosis of 44 years.[2] The clinical features are soft-tissue swelling, acral enlargement, arthralgia, jaw prognathism, posterior open bite, hyperhidrosis, osteoarthritis, and frontal bossing. [3] Several cardiovascular and metabolic comorbidities are accompanied with an increased mortality in untreated patients.[4] The disease is usually caused by a pituitary adenoma producing the active hormones[5] with less than 5% of cases caused by hypothalamic or a neuroendocrine tumor.[6] Often the first obvious signs of acromegaly are changes in the facial features due to frontal bossing and mandibular prognathism. Thus, the suspicion of the disease may arise after the evaluation of orthodontists or maxillofacial professionals.
Bilateral sagittal split osteotomy (BSSO) introduced by Trauner and Obwegeser[7] in 1957 and later modified by Dal Pont and Hunsuck[8,9] is the most frequently used osteotomy for correction of mandibular deformities. Several modifications to BSSO have been developed since then.[10] Bilateral sagittal split osteotomy was, however, introduced before the era of rigid osteosynthesis and it first relied upon large bone contact areas and prolonged maxillamandibular fixation. Due to the course of the mandibular nerve, the approach is prone to cause neurosensory disturbances, which is one of the technique’s major drawback[11] besides the risk for unexpected fractures.[12]
Subcondylar ramus osteotomy is another common technique used to correct mandibular prognathism and/or mandibular asymmetry. There are several modifications and differences in approaches to the ramus. The horizontal subcondylar osteotomy of the ramus by an external approach was first introduced by Blair in 1907,[13] and the subcondylar oblique osteotomy was reported by Lindberg in 1925.[14] The intraoral approach for both techniques was later described by Ernst and Mose, respectively.[15] The vertical ramus osteotomy (VRO) was popularized by Caldwell and Letterman in 1954[16] for extraoral approach and later followed by an intraoral approach.[17,18] Rigid fixation has been described for both extra- and intraoral procedures,[19,20] however, it is not often used in intraoral subcondylar osteotomies probably due to technical challenges related to the osteosynthesis.[21]
Case Report
The Patient
The patient was a 30-year-old male with no previous orthodontic treatment, who was referred to our clinic by his orthodontist due to an increasing posterior open bite in the molar region and tooth wear in the anterior area (Figure 1). The patient (height 194 cm and weight 85 kg) had asthma diagnosis and his facial asymmetry was clear at first appearance. His most important complaints were bruxism, snoring, and changes in “s” and “r” sounds. Acromegaly was strongly suspected as a possible cause of his facial features and laboratory screening was carried out. The fasting serum GF (fS-GF) was marginally elevated at 32.4 mU/L (>30 mU/L) and serum insulin-like growth factor-1 (S-IGF-1) clearly elevated at 136 nmol/L (10-32 nmol/L). The patient was referred to an endocrinologist. The magnetic resonance imaging scan revealed a 2.6 cm × 2 cm sized hypophyseal adenoma confirming the diagnosis. However, a clear enlargement of the Sella was not detected in cephalometric radiograph probable due to the lateral growth of the adenoma (Figure 2D). The adenoma was surgically removed and as fS-GF and S-IGF-1 levels were normalized, the orthognathic treatment was initiated.

Figure 1.
Clinical pictures before treatment. The facial pictures before treatment demonstrate mandible ramus growth (A-E). An open bite was clearly noticeable in molar and premolar areas (F-H).
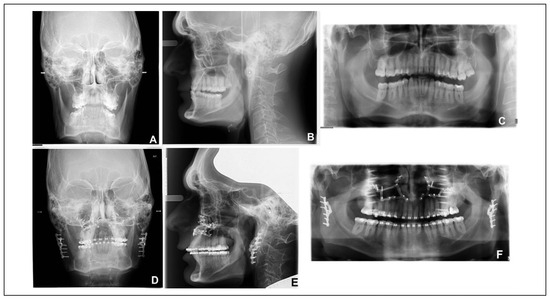
Figure 2.
Pretreatment and postoperative radiographs. Pretreatment anteroposterior skull (A), lateral cephalometric (B), and orthopantomogram (C) X-rays reveal bony deformations related to acromegaly. Similar postoperative radiographs are presented in (D), (E), and (F).
Clinical and Cephalometric Findings at the Beginning of the Treatment
The orthodontic treatment plan was performed based on the clinical findings, the dental casts, as well as the radiographic and cephalometric analysis. The patient had a slightly concave profile, a slight facial asymmetry, and a square shaped lower face. There was an evident asymmetric gummy smile in the premolar region on both sides (right: 8 mm, left: 12 mm) due to excess eruption of the upper premolars and tilting of the maxillary horizontal plane. Although there was a major attrition of the incisors, the anterior smile line was well balanced. The clinical findings revealed angle class III dentition, complete open bite in the molar- and premolar areas, and crossbite from the right upper molar to left central upper incisor −1 mm overjet and −2 to 0 mm overbite (Figure 1). The mouth opening, protrusion and lateral movements were normal. Also the clinical and radiological findings regarding the temporomandibular joints were normal.
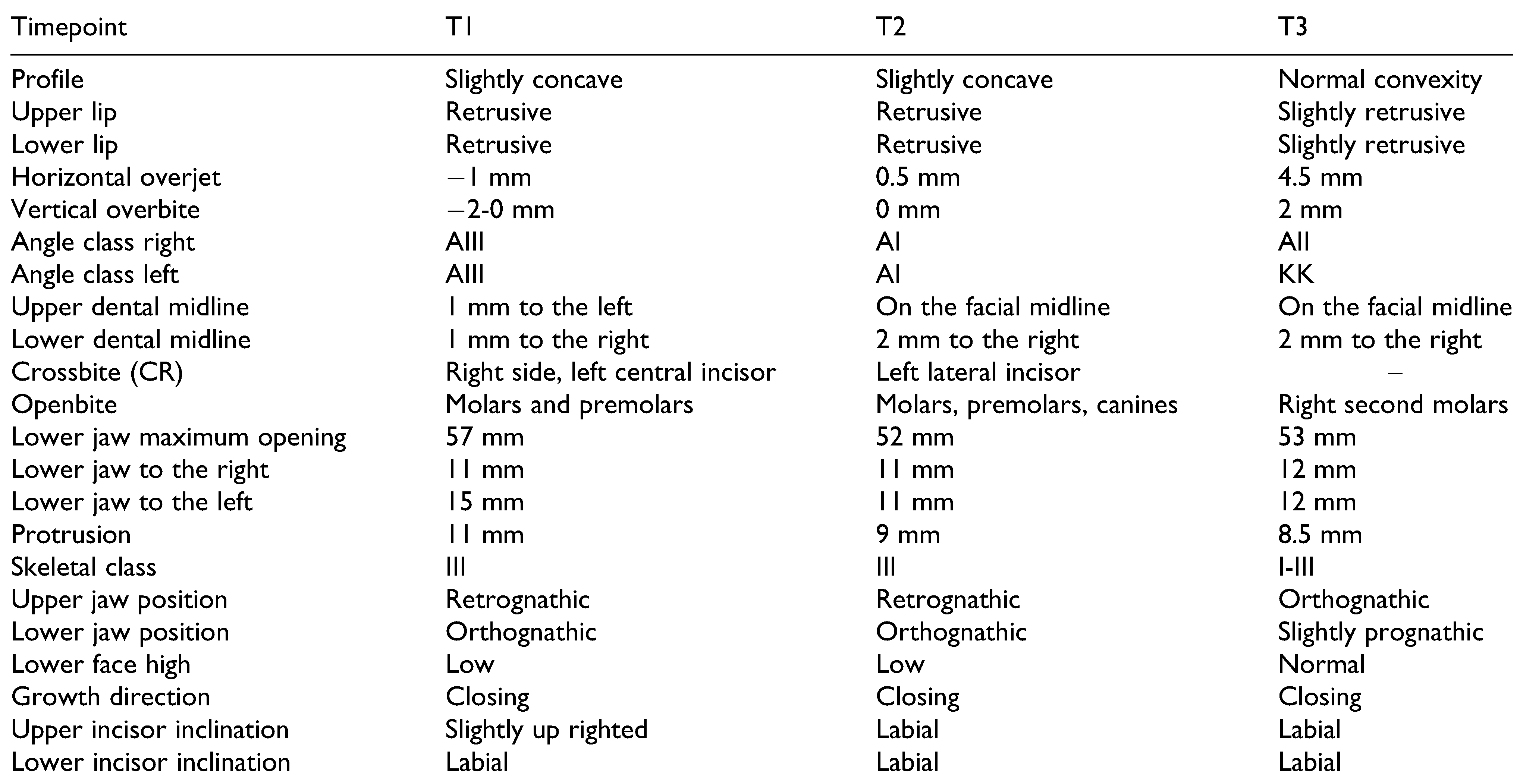
Cephalometric analysis revealed skeletal class III with a retrognathic maxilla and orthodontic mandible, a decreased anterior lower face height with a closing growth direction. The patient had slightly upright anterior teeth and labially inclined lower incisors (Table 1 and Figure 2B). The presurgical orthodontic treatment with conventional fixed appliances (Mini-Mat Roth, Ormco) was completed in 2 years and followed by orthognathic surgery (Figure 3).

Table 1.
Cephalometric Profile and Clinical Status of the Patient During Treatment.a.

Figure 3.
Clinical pictures before surgery. The occlusal pictures before surgery demonstrate the amount of open bite after orthodontic decompensation. Front view (A), right (B), upper jaw (C), and left (D).
Orthognathic Surgery
After clinical analysis of the soft tissue appearance (dental show, smile line, lip closure) and of the preoperative occlusion the surgical treatment plan was made (Figure 4, Figure 5 and Figure 6) based on 3-dimensional (3D) computed tomography scans with the aim to correct the facial bone asymmetries and occlusion utilizing different approaches. During the 3D planning, special attention was paid to preserve the condylar positions and generate sufficient bone contacts at the osteotomy sites. To be able to reduce the asymmetrically and largely inferiorly prolonged angular area of the mandible, only an osteotomy of the ramii was the treatment of choice for the mandible. Achieving exact bone contacts and angulation of the condyles after the osteotomies was found to require rigid fixation. When applying patient-specific implants (PSIs) and securing them to the predrilled holes, they functioned as reposition devices ensuring the correct position between the condylar head and rest of the mandible after the segment removal (Figure 6). An extraoral approach was found to provide better visibility and working space. Furthermore, an extraoral approach was thought to allow management of any complication during the surgery if for some reason our osteotomies planned with computeraided design (CAD) and computer-aided manufacturing (CAM) were to be unsuccessful. The patient was not concerned about possible scaring.
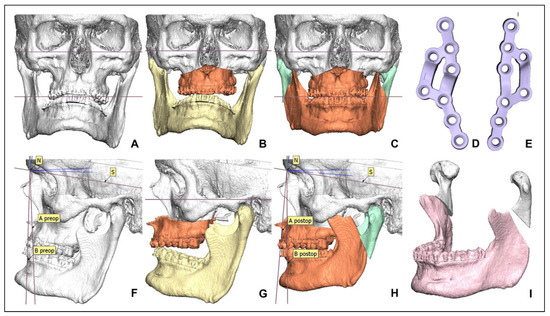
Figure 4.
Three-dimensional planning and CAD/CAM-based osteotomy with mandibular PSIs. Acromegaly has caused clear vertical overgrowth of the mandible ramus generating posteriorly an open bite and discrepancies (A and F). Correction of asymmetry after virtual osteotomies for the upper jaw (B and G) and the final position of both jaws (C and H). The mandibular PSIs where designed to guide alignment between the condylar head and the rest of the mandible after the segment removal ensuring the correct position (E). The mandible shape after virtual removing of bone fragments (I). CAD indicates computer-aided design; CAM, computer-aided manufacturing; PSIs, patient-specific implants.
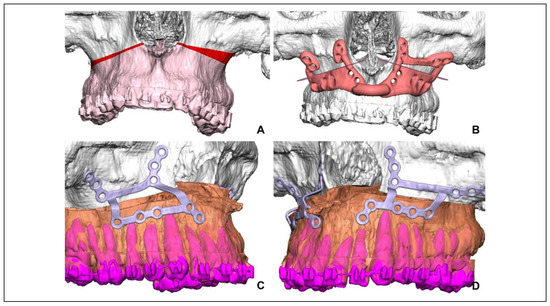
Figure 5.
Design of maxillary CAD/CAM saw and drill guides and patient-specific implants. Amount of bone removal needed for correcting vertical asymmetry (A). Saw and drill guide ensuring bone removal and correct final alignment utilizing predrilled holes (B). The maxilla PSIs were designed to correct midline error and occlusal plane and drill holes are planned to avoid root damage (C and D). CAD indicates computer-aided design; CAM, computer-aided manufacturing; PSIs, patient-specific implants.
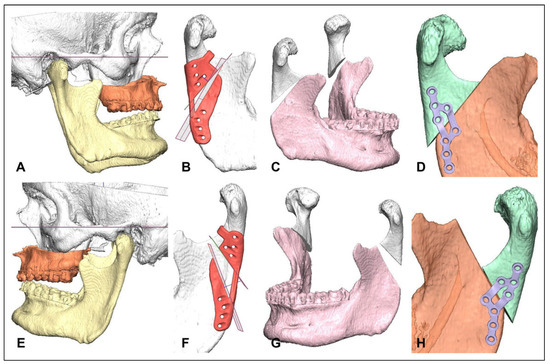
Figure 6.
Design of mandibular CAD/CAM-based osteotomy, saw and drill guides, and PSIs. True amount of mandibular vertical overgrowth after virtual correction of maxilla (A and E). Ramus height had to be reduced by subcondylar osteotomies and a wedgeshaped bone fragment is removed using a saw guide, the same guide also includes a guide for predesigned drill holes (B and F). Amount of bone removal needed for correcting vertical asymmetry (C and G). The mandibular PSIs guiding alignment between the condylar head and rest of the mandible after the segment removal ensuring the correct position. Prominent processus coronoideus and posterior bone border excess needed to be reduced to provide free mandible rotation and symmetric aesthetics at the area of the mandibular angle (D and H). CAD indicates computer-aided design; CAM, computer-aided manufacturing; PSIs, patient-specific implants.
The 3D surgical treatment with CAD/CAM manufactured PSIs was done utilizing the Planmeca ProModel system (Planmeca Ltd) as described earlier.[22] Bimaxillary surgery was indicated for the correction of the occlusal disturbances and skeletal deformities. At first, the skeletal disturbances of the midface, mainly due to asymmetric excess of the maxillary posterior height and occlusal plane inclination, were corrected by LeFort I osteotomy using the conventional intraoral approach (Figure 7F). Le Fort I osteotomy with guided surgery was performed as described earlier.[23] After securing the maxilla with PSIs to desired position, a minimal retromandibular extraoral approach was made bilaterally and saw/drill guides were inserted (Figure 7B and C).
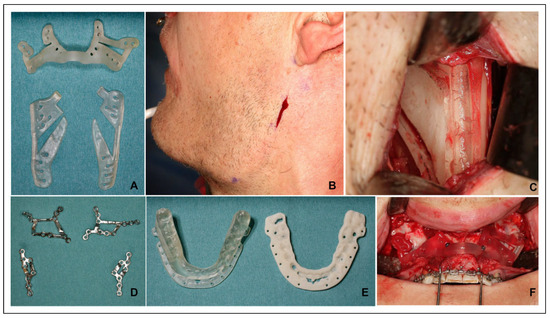
Figure 7.
Perioperative photographs and CAD/CAM: saw and drill guides, wafers, and PSIs. CAD/CAM saw and drill guides and wafers were made from medical plastic (A and E). The mandible osteotomy was performed through a minimal retromandibular approach (B). The amount of bone to be reduced was marked using a mandibular (C) and maxillar guide (F). Maxillar and mandibular PSIs were milled from medical grade titanium (D). CAD indicates computer-aided design; CAM, computer-aided manufacturing; PSIs, patient-specific implants.
An intraoral approach to the ramii was performed as well to enable removal of the coronoid process bilaterally and to secure the correct saw/drill guide position leaning on to the incisure.
The final screw holes for the PSIs were predrilled. The increased ramus height causing posterior vertical excess and mandibular prognathia was corrected by segmental bone removal guided by the saw guides. The correction was performed with a higher and lower oblique subcondylar osteotomy removing the segment in-between through the minimal extra oral approach. Both osteotomies were performed using predesigned saw/drill guides and the final position was acquired by utilizing PSIs as reposition and osteosynthesis device (Figure 7A and D). To maintain good mouth opening and normal jaw function, the height of processus coronoideus had to be reduced (Figure 6D and H), which was done through the intraoral approach. All osteotomies were performed as planned and PSIs fitted the predesigned drill holes with good precision (Figure 2B and C). The mandible was mobilized immediately after surgery. To assure the occlusion intermaxillary fixation with elastics was maintained for 6 to 8 hours/d 4 weeks postoperatively. The aesthetic outcome was good. The patient obtained a normal facial profile and a normal posterior lower facial height was reestablished (Figure 8).
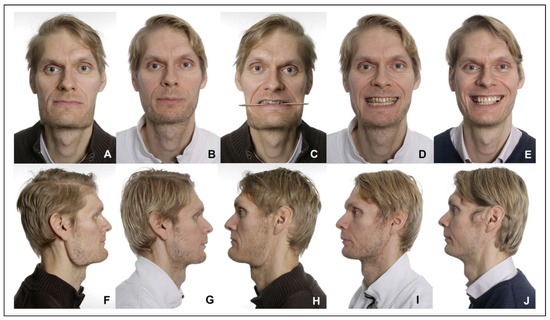
Figure 8.
Clinical pictures before treatment and after retention period. Clinical pictures before treatment (A), (C), (F), and (H) and after 1.5-year follow-up (B), (D), (G), and (I) demonstrate that facial symmetry was obtained. Clinical pictures after completing prosthodontic treatment, 2.5 years (E and J).
Postsurgical Orthodontic and Prosthetic Treatment
The postoperative orthodontic treatment was continued for 1 year and 2 months until a stable occlusion was obtained. The clinical and cephalometric findings were measured before the orthodontic treatment (T1), presurgically before the surgery (T2) and the clinical findings at the end of postsurgical orthodontic treatment, and cephalometric findings and the beginning of postsurgical orthodontics (T3; Table 1 and Figure 9). At the end of the follow-up, the retention period was 1 year and 10 months, and the clinical extra- and intraoral findings remained stable. The prosthodontic treatment was carried out after the retention period correcting the defects due to attrition of the teeth (Figure 10). Superimpositions of patient pretreatment, preoperative, and postoperative kefalograms can be seen in Figure 11.

Figure 9.
Occlusion before, during, and after treatment. Front view. The occlusion at the beginning of the treatment (A). The occlusion before the bimaxillary surgery (B). The occlusion after crown lengthening process and laminate crowns (C and D).

Figure 10.
Postsurgical occlusion after retention period, crown lengthening process, and prosthodontic treatment. Front view (A and C), left (B), and right side (D). Profile picture after retention period, crown lengthening process, and prosthodontic treatment (E and F).
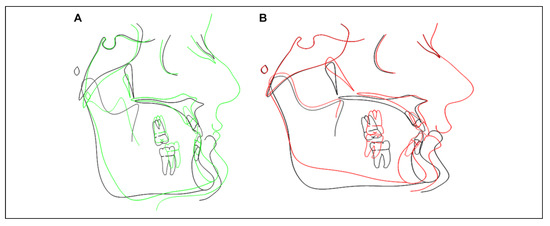
Figure 11.
(A) Cephalometric superimpositions. Cephalometric superimposition at the beginning (presented in green) and preoperatively (presented in black). (B) Equally, superimpositions preoperatively (presented in black) and at the end of active orthodontic treatment (presented in red).
Discussion
Acromegaly in patients causes alterations in size and shape of hard and soft tissues, with enlargement of all orofacial bones except the maxilla. The mandible usually shows the largest enlargement, and the ramus is more affected than the body of the mandible.[2] Our patient showed a proportionally more downward growth of the ramus than forward growth of the corpus causing a counterclockwise rotation, increasing posterior facial height and posterior open bite resulting in somehow special characteristic of the facial appearance.
We did not find the conventional BSSO approach suitable as it offers no possibilities for vertical correction of the angular area, easily resulting in a poor aesthetic result in our patient without additional correction of the mandibular lower border and gonial areas. This resection including extensive muscle stripping also includes the risk for facial nerve disturbances. Furthermore, the BSSO approach would not have had enough impact on the patient’s posterior facial height sufficiently.
The most important advantage of subcondylar osteotomies is the lower incidence of damage to the inferior alveolar nerve[11,24,25] and also technical simplicity, reduced operating time, and the ability to repositioning of the condyle. [24] On the other hand, less bony contact at the osteotomy site and osteosynthesis difficulties make the subcondylar osteotomy to some extent inferior to the BSSO, with regard to the postoperative healing process and duration.[21] Subcondylar osteotomies including the VRO without application of rigid osteosynthesis were considered in this case. However, due to substantial risk for relapse and nonpredictable changes in the condylar position, with required prolonged maxillamandibular fixation, the treatment without osteosynthesis was decided not to be performed. The technique used was found to allow better correction compared to conventional BSSO. Due to the required intrusion of the angular area with extensive overlapping of segments and protruding forces compromising aesthetic and functional outcome was to be expected if a segmental resection was not performed. Problems involving protrusion of the proximal segment may cause the mandibular angle to protrude toward the buccal side,[26] possibly affecting the aesthetic outcome. For reasons mentioned above, a rigid fixation method with bone removal was thus selected. There are some recent publications addressing difficulties associated with procedures concerning condylar position, location, and orientation of the osteotomy[27] with or without the use of positional devices.[28]
Due to the surgical site and osteotomy demands, an extraoral approach was found to provide better visibility and working space. Furthermore, the extraoral approach would allow easier free hand surgery and possible grafting if for some reason our planned CAM/CAD approach was compromised during operation. The patient was also not concerned about possible scaring, which influenced our decision. Some surgeons advocate the extraoral VRO with rigid fixation as an alternative for BSSO to avoid problems associated with intraoral VRO.[21] We acknowledge that with some modifications, the surgical treatment is possible to perform through an intraoral and transbuccal approach only, but in case of complications the extraoral approach would possibly still be necessary.
Since acromegaly affects the maxilla less than other orofacial bones, we assume that the patient had a retrognathic maxilla and possibly a retrognathic mandible before the onset of the disease. Proportionally larger growth of the mandibular ramii causing a CCW rotation and possibly some enlargement of the tongue (even not clearly noticeable clinically) possibly explain the cephalometric findings of the upright incisors and labially inclined lower incisors not very typical for class III patients.
The patient did not express concerns about changed upper facial appearance although over projected and wide supraorbital ridges were clearly noticeable. However, the eyesight was not affected. A correction would have required additional surgery, which the patient was not interested in, so the issue was not addressed. We acknowledge that the facial appearance is somehow feminizing compared to the gross presurgical appearance, but the final result is probably close to the appearance of the patient prior the onset of disease.
The corpus of mandible remained prominent to some extent on the right side which resulted in bulginess of soft tissue appearance on that side after operation. However, the level of asymmetry was considered to be so small that no recontouring of mandibular corpus on the right side was considered in the primary or secondary stage.
The benefits of 3D design and virtual treatment plans are clear when dealing with complex 2-jaw asymmetry cases. The conventional wafer-based jaw repositioning and osteofixation by “on stock” miniplates can, however, be sometimes unpredictable. The prebent plates may help to some extent but true CAD/CAM generated wafers, cutting guides, and predesigned plates can significantly be beneficial especially in maxillary repositioning.[22,23,29] However, there are some drawbacks and concerns regarding true CAM/CAD surgery. Relying only on 3D techniques can distance some surgeons from the traditional approaches. Especially in situations where modern techniques fail, surgeons should always be prepared to master and execute conventional solutions otherwise disastrous consequences could occur. In our case, grafting and securing the subcondylar osteotomies would be challenging if the masterplan failed. Time and cost of 3D can also be an issue. New approaches in the 3D techniques usually require engineering skills that usually has to be acquired outside the clinics and can be time and money consuming. Predictability of the outcome and possibilities that new techniques and approaches offer, however, advocates their use in selected cases. It also seem that PSIs differ little on their complication profile as compared to conventional osteosynthesis and may also have lover risk for reoperations.[30]
Conclusion
The use of PSIs with guided surgery can be beneficial for selected cases with severe asymmetry and posterior open bite. The system enables new approaches and yields predictable functional and aesthetic outcome. We consider our modification of conventional ramus osteotomy with utilization of ramus segment removal in combination of the use of PSI for reposition as an interesting and promising technique for rare conditions involving ramus height asymmetry. Good torque and other physical properties of PSIs are crucial when only limited bony contact exists after osteotomies and ramus segmental removal. In this specific case, the 3D planning and CAD/CAM-based osteotomy with saw/drill guides and PSIs made the outcome of the Le Fort I osteotomy and the nonconventional subcondylar osteotomies predictable and stable. In addition, the rigid fixation with PSIs allowed normal function and immediate mandible mobilization postoperatively. This approach should be considered when planning surgical correction of complex asymmetry and possibly syndrome cases.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank Jani Horelli from Planmeca Ltd for technical assistance and intellectual cooperation, Emil Aaltonen Foundation, Finnish-Norwegian Medical Foundation, The Finnish Medical Foundation, Paulo Foundation, and Helsinki University Hospital Funds.
Authors’ Note
Written informed consent was obtained from the patient presented in the manuscript figures.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Melmed, S. Acromegaly. N Engl J Med. 2006, 355, 2558–2573. [Google Scholar]
- Sala, E.; Ferrante, E.; Locatelli, M.; et al. Diagnostic features and outcome of surgical therapy of acromegalic patients: experience of the last three decades. Hormones. 2014, 13, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Galerneau, L.M.; P´epin, J.L.; Borel, A.L.; et al. Acromegaly in sleep apnoea patients: a large observational study of 755 patients. Eur Resp J. 2016, 48, 1489–1492. [Google Scholar]
- Giustina, A.; Chanson, P.; Kleinberg, D.; et al. Expert consensus document: A consensus on the medical treatment of acromegaly. Nature Rev Endocr. 2014, 10, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Melmed, S. Acromegaly pathogenesis and treatment. J Clin Invest. 2009, 119, 3189–3202. [Google Scholar] [PubMed]
- Katznelson, L.; Laws, E.; Melmed, S.; et al. Acromegaly: an endocrine society clinical practice guideline. J Clin Endocr Metabol. 2014, 99, 3933–3951. [Google Scholar]
- Trauner, R.; Obwegeser, H. The surgical correction ofmandibular prognathism and retrognathia with consideration of genioplasty. Oral Surg Oral Med Oral Path. 1957, 10, 677–689. [Google Scholar]
- Dal Pont, G. Retromolar osteotomy for the correction of prognathism. J Oral Surg Anesth Hosp Dent Serv. 1961, 19, 42. [Google Scholar]
- Hunsuck, E.E. A modified intraoral sagittal splitting technic for correction of mandibular prognathism. J Oral Surg. 1968, 26, 250–253. [Google Scholar]
- Böckmann, R.; Meyns, J.; Dik, E.; Kessler, P. The modifications of the sagittal ramus split osteotomy. Plast Recon Sur Global Open. 2014, 2, e271. [Google Scholar]
- Westermark, A.; Bystedt, H.; von Konow, L. Inferior alveolar nerve function after mandibular osteotomies. Brit J Oral Maxillofac Surg. 1998, 36, 425–428. [Google Scholar]
- Kriwalsky, M.; Maurer, P.; Veras, R.; Eckert, A.W.; Schubert, J. Risk factors for a bad split during sagittal split osteotomy. Brit J Oral Maxillofac Surg. 2008, 46, 177–179. [Google Scholar]
- Blair, V. Operations on the jaw-bone and face. Surg Gynecol Obstetr. 1907, 4, 67–78. [Google Scholar]
- Limberg, A.A. Treatment of open bite by means of plastic oblique osteotomy of the ascending rami the mandible. Dental Cosmos. 1925, 67, 1191. [Google Scholar]
- Moose, S.M. Surgical correction of mandibular prognathism by intraoral subcondylar osteotomy. J Oral Surg Anesth Hosp Dent Serv. 1964, 197–202. [Google Scholar]
- Caldwell, J.B.; Letterman, G.S. Vertical osteotomy in the mandibular raml for correction of prognathism. J Oral Surg. 1954, 12, 185–202. [Google Scholar] [PubMed]
- Winstanley, R.P. Subcondylar osteotomy of the mandible and the intraoral approach. Brit J Oral Surg. 1968, 6, 134–136. [Google Scholar]
- Hebert, J.M.; Kent, J.N.; Hinds, E.C. Correction of prognathism by an intraoral vertical subcondylar osteotomy. J Oral Surg. 1970, 28, 651–653. [Google Scholar]
- Paulus, G.; Steinhauser, E. A comparative study of wire osteosynthesis versus bone screws in the treatment of mandibular prognathism. Oral Surg Oral Med Oral Pathol. 1982, 54, 2–6. [Google Scholar]
- Kraut, R. Stabilization of the intraoral vertical osteotomy using small bone plates. J Oral Maxillofac Surg. 1988, 46, 908–910. [Google Scholar] [CrossRef]
- Ha°gensli, N.; Stenvik, A.; Espeland, L. Extraoral vertical subcondylar osteotomy with rigid fixation for correction of mandibular prognathism. Comparison with bilateral sagittal split osteotomy and surgical technique. J Craniomaxillofac Surg. 2013, 41, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Suojanen, J.; Leikola, J.; Stoor, P. The Use of patient specific implants in ortognatic surgery—a series of 32 maxillary osteotomy patients. J Craniomaxillofac Surg. 2016, 44, 1913–1916. [Google Scholar] [PubMed]
- Mazzoni, S.; Bianchi, A.; Schiariti, G.; Badiali, G.; Marchetti, C. Computer-aided design and computer-aided manufacturing cutting guides and customized titanium plates are useful in upper maxilla waferless repositioning. J Oral Maxillofac Surg. 2015, 73, 701–707. [Google Scholar]
- Ghali, G.; Sikes, J. Intraoral vertical ramus osteotomy as the preferred treatment for mandibular prognathism. J Oral Maxillofac Surg. 2000, 58, 313–315. [Google Scholar] [PubMed]
- Al-Moraissi, E.; Ellis, E. Is there a difference in stability or neurosensory function between bilateral sagittal split ramus osteotomy and intraoral vertical ramus osteotomy for mandibular setback? J Oral Maxillofac Surg. 2015, 73, 360–1371. [Google Scholar]
- Rokutanda, S.; Yamada, S.; Yanamoto, S.; et al. Comparison of osseous healing after sagittal split ramus osteotomy and intraoral vertical ramus osteotomy. Int J Oral Maxillofac Surg. 2018, 47, 1316–1321. [Google Scholar]
- Kaduk, W.; Podmelle, F.; Louis, P. Revisiting the supraforaminal horizontal oblique osteotomy of the mandible. J Oral Maxillofac Surg. 2012, 70, 421–428. [Google Scholar]
- Seeberger, R.; Asi, Y.; Thiele, O.C.; Hoffmann, J.; Stucke, K.; Engel, M. Neurosensory alterations and function of the temporomandibular joint after high oblique sagittal split osteotomy: an alternative technique in orthognathic surgery. Brit J Oral Maxillofac Surg. 2013, 51, 536–540. [Google Scholar]
- Gander, T.; Bredell, M.; Eliades, T.; Rücker, M.; Essig, H. Spintless orthognatic surgery: a novel technique using patient-specific implants (PSI). J Craniomaxillofac Surg. 2016, 43, 319–322. [Google Scholar]
- Suojanen, J.; Järvinen, S.; Kotaniemi, K.V.M.; et al. Comparison between patient specific implants and conventional miniplates in Le Fort I osteotomy with regard to infections: No differences in up to 3-year follow-up. J Craniomaxillofac Surg. 2018, 46, 1814–1817. [Google Scholar]
© 2020 by the author. The Author(s) 2020.