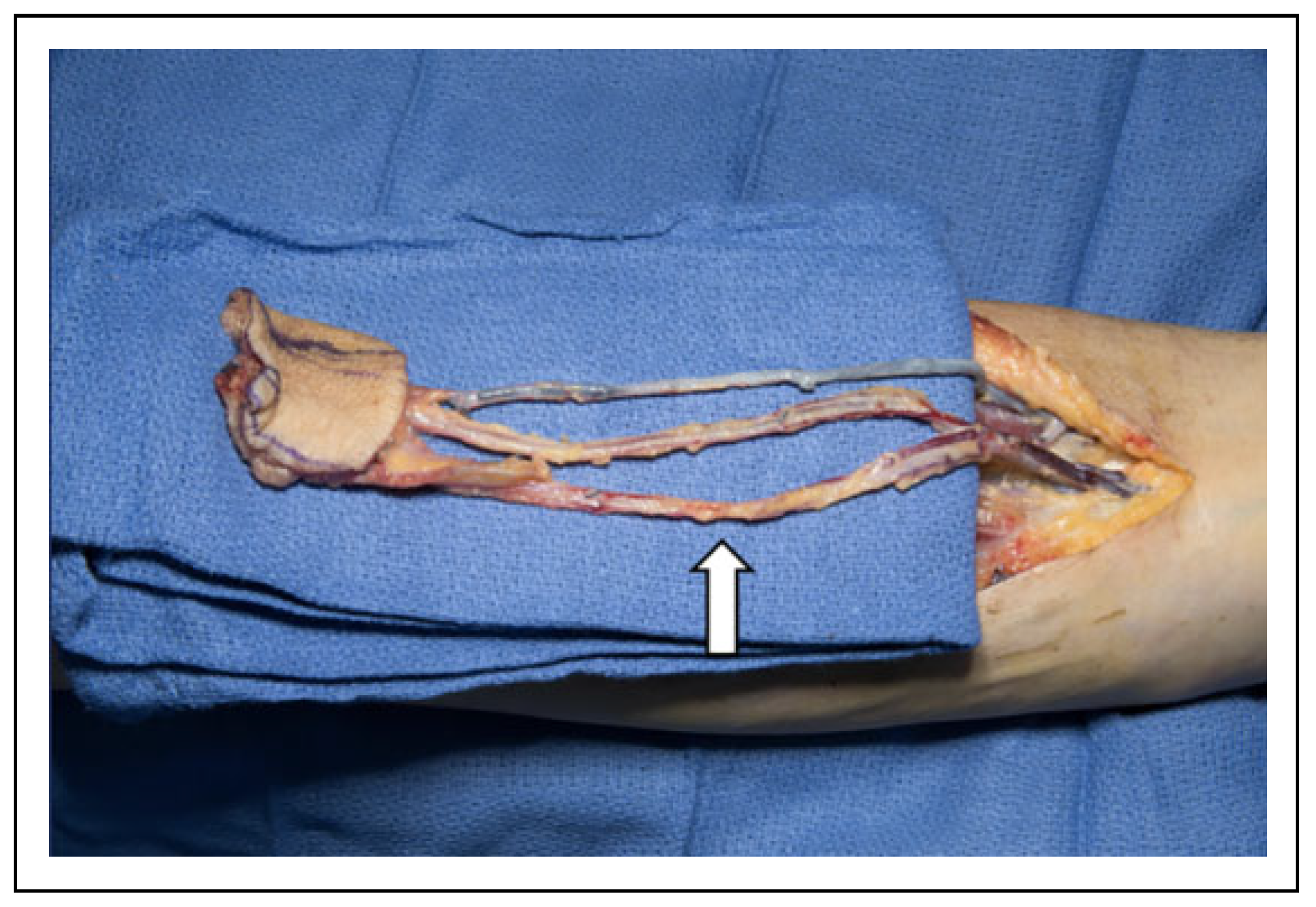
The Anomalous Radial Artery: A Rare Vascular Variant and Its Implications in Radial Forearm Free Tissue Transfer
Abstract
:Introduction
Discussion
Conclusion
Funding
Conflicts of Interest
Authors’ Note
References
- Mardini, S.; Wei, F.-C. Flaps and Reconstructive Surgery; Saunders: Philadelphia, Pennsylvania, 2009. [Google Scholar]
- Martín-Granizo, R.; Gómez, F.; Sánchez-Cuéllar, A. An unusual anomaly of the radial artery with potential significance to the forearm free flap. Case report. J Craniomaxillofac Surg. 2002, 30, 189–191. [Google Scholar]
- Gray, H.; Williams, P.L.; Warwick, R. Gray’s anatomy; Churchill Livingstone: London, England, 2008. [Google Scholar]
- Foreman, A.; de Almeida, J.R.; Gilbert, R.; Goldstein, D.P. The Allen’s test: revisiting the importance of bidirectional testing to determine candidacy and design of radial forearm free flap harvest in the era of trans radial endovascular access procedures. J Otolaryngol Head Neck Surg. 2015, 44, 47. [Google Scholar]
- Lo, N.; Leung, P.; Lau, K.; Yeung, C. Congenital cardiovascular malformations in Chinese children with Down’s syndrome. Chin Med J. 1989, 102, 382–386. [Google Scholar]
- Bass, J. Radial artery hypoplasia: a further association with the VATER syndrome? J Urol. 1991, 146, 824–825. [Google Scholar]
- Lee, W.-T.; Wang, P.-J.; Young, C.; Lai, M.-W.; Shen, Y.-Z. Thenar hypoplasia in Klippel-Feil syndrome due to aberrant radial artery. Pediatr Neurol. 1995, 13, 343–345. [Google Scholar]
- McCormack, L.J.; Cauldwell, E.W.; Anson, B.J. Brachial and antebrachial arterial patterns; a study of 750 extremities. Surg Gynecol Obstet. 1953, 96, 43–54. [Google Scholar]
- Uglietta, J.P.; Kadir, S. Arteriographic study of variant arterial anatomy of the upper extremities. Cardiovasc Intervent Radiol. 1989, 12, 145–148. [Google Scholar]
- Mordick, T.G. Vascular variation of the radial forearm flap: a case report. J Reconstr Microsurg. 1995, 11, 345–346. [Google Scholar]
- Sasaki, K.; Nozaki, M.; Aiba, H.; Isono, N. A rare variant of the radial artery: clinical considerations in raising a radial forearm flap. Br J Plast Surg. 2000, 53, 445–447. [Google Scholar]
- Bhatt, V.; Green, J.; Grew, N. Dealing with aberrant vessels in radial forearm flaps–report of a case and review of literature. J Craniomaxillofac Surg. 2009, 37, 87–90. [Google Scholar]
- Madaree, A.; McGibbon, I.C. Anatomic variation in the blood supply of the radial forearm flap. J Reconstr Microsurg. 1993, 9, 277–279. [Google Scholar] [CrossRef]
- Acarturk, T.O.; Newton, E.D. Aberrant branch of the radial artery encountered during elevation of the radial forearm free flap. J Reconstr Microsurg. 2004, 20, 611–614. [Google Scholar]
- Kadanoff, D.; Balkansky, G. 2 cases with rare variations of arteries of the upper extremities [In German]. Anat Anz. 1966, 118, 289–296. [Google Scholar]
- Li, L.; Zeng, Z.-Y.; Zhong, J.-M.; et al. Features and variations of a radial artery approach in southern Chinese populations and their clinical significance in percutaneous coronary intervention. Chin Med J (Engl). 2013, 126, 1046–1052. [Google Scholar]
- Small, J.; Millar, R. The radial artery forearm flap: an anomaly of the radial artery. Br J Plast Surg. 1985, 38, 501–503. [Google Scholar]
- Morris, L.G.; Rowe, N.M.; Delacure, M.D. Superficial dorsal artery of the forearm: case report and review of the literature. Ann Plast Surg. 2005, 55, 538–541. [Google Scholar] [CrossRef]
- Hedén, P.; Gylbert, L. Anomaly of the radial artery encountered during elevation of the radial forearm flap. J Reconstr Microsurg. 1990, 6, 139–141. [Google Scholar]
- Rodríguez-Niedenführ, M.; Vazquez, T.; Nearn, L.; Ferreira, B.; Parkin, I.; Sanudo, J. Variations of the arterial pattern in the upper limb revisited: a morphological and statistical study, with a review of the literature. J Anat. 2001, 199, 547–566. [Google Scholar]
- Venkatanarasimha, N.; Manghat, N.; Wells, I. Unusual presentation of ulnar artery aneurysm and dissection with associated anomalous radial artery: appearances on multi-detector row CT angiography. Emerg Radiol. 2007, 14, 101–104. [Google Scholar]
- Otsuka, T.; Terauchi, M. An anomaly of the radial artery—relevance for the forearm flap. Br J Plast Surg. 1991, 44, 390–391. [Google Scholar]
- Funk, G.F.; Valentino, J.; McCulloch, T.M.; Graham, S.M.; Hoffman, H.T. Anomalies of forearm vascular anatomy encountered during elevation of the radial forearm flap. Head Neck. 1995, 17, 284–292. [Google Scholar]
- Icten, N.; Süllü, Y.; Tuncer, I. Variant high-origin radial artery: a bilateral case. Surg Radiol Anat. 1996, 18, 63–66. [Google Scholar] [CrossRef]
- Konarik, M.; Knize, J.; Baca, V.; Kachlik, D. Superficial brachioradial artery (radial artery originating from the axillary artery): a case report and embryological background. Folia Morphol (Warsz). 2009, 68, 174–178. [Google Scholar]
- Yoo, B.-S.; Yoon, J.; Ko, J.-Y.; et al. Anatomical consideration of the radial artery for transradial coronary procedures: arterial diameter, branching anomaly and vessel tortuosity. Int J Cardiol. 2005, 101, 421–427. [Google Scholar]
- Coleman, S.S.; Anson, B.J. Arterial patterns in the hand based upon a study of 650 specimens. Surg Gyneco Obste. 1961, 113, 409–424. [Google Scholar]
- Loukas, M.; Louis, R.G.; Almond, J.; Armstrong, T. A case of an anomalous radial artery arising from the thoracoacromial trunk. Surg Radiol Anat. 2005, 27, 463–466. [Google Scholar]
- Porter, J.C.; Mellow, C.G. Anatomically aberrant forearm arteries: an absent radial artery with co-dominant median and ulnar arteries. Br J Plast Surg. 2001, 54, 727–728. [Google Scholar]
- Bumbaširević, M.; Lešić, A.; Filipović, B. Duplication of the radial artery in the radial forearm flap. Clin Anat. 2005, 18, 305–307. [Google Scholar]
- Gober, C.A.; Mujadzic, T.; Hershman, J.E.; Mujadzic, M.M. Anomalous radial artery as an incidental finding during a routine carpal tunnel release. Hand (N Y). 2017, 12, NP101–NP103. [Google Scholar]
- Mersa, B.; Ozcelik, B.; Kuvat, S.; Pilanci, O. An anomalous course of the radial artery: dissect rather than resect. Indian J Plast Surg. 2010, 43, 228–229. [Google Scholar]
- Gwynne-Jones, D.P.; Hartnett, N.I. Aberrant radial artery seen in the carpal tunnel at carpal tunnel decompression: case report. J Hand Surg. 2008, 33, 885–887. [Google Scholar]
- Vadodaria, S.; Brotherston, T.; Page, R. Best use of anomaly of radial artery. British Journal of Plastic Surgery. 2001, 54, 180–181. [Google Scholar] [CrossRef] [PubMed]

| Radial Artery Anomaly | Source |
|---|---|
| Duplication of radial artery | [15,16] |
| Radial artery passing deep to pronator teres | [17] |
| Superficial dorsal antebrachial artery | [8,11,18,19,20] |
| Hypoplasia of radial artery | [6,7,21] |
| Aberrant dorsal course of radial artery around Lister’s tubercle | [22] |
| Absence of perforators from the radial artery to the skin | [13] |
| Distal origin of radial artery deep to pronator teres | [23] |
| Superficial dorsal antebrachial artery | |
| High origin of radial artery | |
| Aberrant midaxial vessel arising directly from the axial artery | [10] |
| High origin of the radial artery | [8,9,10,20,24,25,26,27,28] |
| Absent radial artery | [29] |
| Superficial radial artery lateral to normal vessel originating from it | [2] |
| Accessory branch of the radial artery at the level of mid forearm extending laterally subcutaneously into the dorsal wrist | [14] |
| Accessory branch of the radial artery | [5,26] |
| Duplication of the radial artery close to cephalic vein | [30] |
| Radial artery in the carpal tunnel | [31,32,33] |
© 2020 by the author. The Author(s) 2020.
Share and Cite
Staebler, M.H.; Anzalone, C.L.; Price, D.L. The Anomalous Radial Artery: A Rare Vascular Variant and Its Implications in Radial Forearm Free Tissue Transfer. Craniomaxillofac. Trauma Reconstr. 2020, 13, 215-218. https://doi.org/10.1177/1943387520904206
Staebler MH, Anzalone CL, Price DL. The Anomalous Radial Artery: A Rare Vascular Variant and Its Implications in Radial Forearm Free Tissue Transfer. Craniomaxillofacial Trauma & Reconstruction. 2020; 13(3):215-218. https://doi.org/10.1177/1943387520904206
Chicago/Turabian StyleStaebler, Maximilian H., Charles Lane Anzalone, and Daniel L. Price. 2020. "The Anomalous Radial Artery: A Rare Vascular Variant and Its Implications in Radial Forearm Free Tissue Transfer" Craniomaxillofacial Trauma & Reconstruction 13, no. 3: 215-218. https://doi.org/10.1177/1943387520904206
APA StyleStaebler, M. H., Anzalone, C. L., & Price, D. L. (2020). The Anomalous Radial Artery: A Rare Vascular Variant and Its Implications in Radial Forearm Free Tissue Transfer. Craniomaxillofacial Trauma & Reconstruction, 13(3), 215-218. https://doi.org/10.1177/1943387520904206



