Abstract
Introduction: Assault appears to be the most frequent cause of facial fractures in certain urban trauma centers, possibly due to the ease of acquiring weapons and increasingly aggressive behavior. The objectives of this study were to identify specific demographic, socioeconomic, maxillofacial fracture, and assault patterns in urban versus suburban communities. Methods: A retrospective chart review of patients who sustained maxillofacial fractures from August 2014 through August 2016 at one urban campus, Einstein Medical Center, Philadelphia, and two suburban campuses, Einstein Medical Center Montgomery and Elkins Park. The χ2 testing was used to compare the categorical variables between the 2 groups. Results: A total of 259 maxillofacial trauma patients were identified, with 204 (79%) in the urban and 55 (21%) in the suburban environment. Patients in the urban population were more likely to be African American (70% vs. 33%) and Hispanic (15% vs. 6%) but less likely to be Caucasian (12% vs. 55%, p < 0.0001). Urban patients were more likely to be single (70% vs. 47%, p < 0.01), unemployed (64% vs. 44%, p < 0.001), and receive Medicaid coverage (58% vs. 26%, p < 0.001). Urban patients were more likely to be victims of assault (63% vs. 44%), whereas suburban patients were more likely to sustain accidental injuries (16% vs. 2%, p < 0.0001). Urban victims were more likely to be assaulted with an object (30% vs. 12%) or gun (7% vs. 0%, p = 0.05). Conclusion: Maxillofacial trauma patterns were shown to be significantly different in the urban versus suburban environment.
Introduction
Maxillofacial trauma pathology can be challenging to treat due to the unique and complex presentation often requiring a multidisciplinary approach.[1] Patients are prone to long-standing physical deformities, neurological impairment, prolonged management, and psychiatric morbidities.[2,3,4] The advent of advanced diagnostic modalities and surgical techniques has helped alleviate the otherwise devastating impact these patients may incur. However, the relatively frequent incidence coupled with the severity of injury still creates a prominent issue.[5,6,7]
As our understanding of management evolves, research in epidemiological and preventative medicine demands increased efforts. Research has shown that motor vehicle accidents (MVAs), assault, falls, and sports have produced the majority of maxillofacial trauma cases.[7] Furthermore, there is an abundance of information that helps categorize both the general public and specific vulnerable populations, including women, children, and victims of domestic violence. The etiologies of injury are known to vary in frequency based on these specific subpopulations.[7,8,9,10,11,12,13,14,15]
In recent years, the importance of socioeconomic status has been reported across several domains of life, including happiness, education, and health care.[16,17] Traditionally, low socioeconomic status is associated with underserved and urban populations, while suburban areas generally grade higher on this scale.[18] From a facial trauma perspective, the literature has been relatively scarce in describing population classifications and anatomical patterns in this context.[19,20,21,22,23,24] Furthermore, most of the existing research has been reported from centers outside of the United States, where sociocultural variables may serve as profound confounders.[21,22,23,24]
Our study aims to compare particular maxillofacial trauma patterns in our urban and suburban communities of Philadelphia. The urban, North Philadelphia population is particularly vulnerable to maxillofacial trauma due to the high prevalence of criminal activity, aggressive violence, and the frequent utilization of weapons.[25] Additionally, we attempted to highlight the maxillofacial trauma patterns of the domestic abuse population, as well as the incarcerated population that utilize our institutions due to interpersonal violence occurring in the prisons. The findings of this study may be important in laying the groundwork for future studies that aim to assess the impact of maxillofacial injuries on certain communities.
Methods
After institutional review board approval, a retrospective chart review of patients who sustained maxillofacial fractures was conducted through the Einstein Healthcare Network from August 2014 through August 2016. This included one urban campus, Einstein Medical Center Philadelphia (Philadelphia, Pennsylvania, USA), and two suburban campuses, Einstein Medical Center Montgomery (East Norriton, Pennsylvania, USA) and Einstein Medical Center Elkins Park (Elkins Park, Pennsylvania, USA; Figure 1).
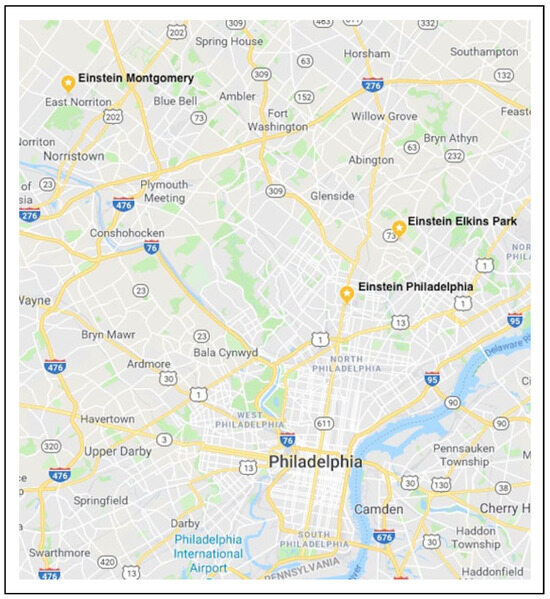
Figure 1.
A map of the Philadelphia region, depicting the 3 medical centers included in this study: 1 urban campus, Einstein Medical Center Philadelphia (Philadelphia, Pennsylvania), and 2 suburban campuses, Einstein Medical Center Montgomery (East Norriton, Pennsylvania, USA) and Einstein Medical Center Elkins Park (Elkins Park, Pennsylvania, USA).
Maxillofacial trauma patients were identified using International Classification of Disease (ICD-10) and Current Procedural Terminology (CPT) codes. Inclusion criteria included patients aged 18 years or older who sustained a maxillofacial fracture confirmed by computed tomography (CT) scan. Exclusion criteria included patients under the age of 18, patients who sustained an isolated nasal bone fracture, and patients who were found to have an old/chronic maxillofacial fracture. Information abstracted from medical records included patient age, gender, race, month and time of presentation, zip code, as well as marital, employment, and insurance status. Diagnostic workup information, including physical examination and CT results, were also collected. The type of maxillofacial fracture(s) and mechanism of injury were recorded. For assaulted patients, the mode of assault and occurrence of domestic abuse were noted including whether the patient knew their attacker and the relationship that existed between them. Additionally, we aimed to identify maxillofacial trauma patterns of the incarcerated population. Finally, population data on income and poverty rates by postal code were collected from the 2012–2016 US Census Bureau.[26]
Descriptive statistics including frequency, percentages, and mean were used to categorize the 2 groups: urban and suburban. The χ2 testing including confidence intervals set at 95% was used to compare the categorical variables between the 2 groups. Multivariate analysis using logistic regression was used to identify potential confounders. A p value ≤0.05 was considered statistically significant. Statistical analysis was performed with IBM SPSS (Armonk, New York) for macOS.
Results
A total of 259 maxillofacial trauma patients were identified, with 204 (79%) in the urban and 55 (21%) in the suburban environment. Between our 2 populations, we did not find any significant differences with regard to age, gender, or season of presentation. In both the urban and suburban cohorts, the patients were predominately male (72% vs. 69%) between 26 and 60 years of age (65% vs. 62%) with increased trauma events during the spring and summer months (59% vs. 49%), respectively (Table 1).

Table 1.
Patient Demographics and Socioeconomic Status.
The 2 most common urban neighborhoods identified for maxillofacial trauma were postal codes 19120 and 19141, which accounted for 25% of cases (Figure 2). According to the 2012–2016 US Census Bureau, the median income for postal code 19120 was US$34 720, with 30.1% of the population living below the poverty line. The median income for postal code 19141 was $29 235, with 30.8% of the population living below the poverty line. Other common postal codes included 19140, 19144, and 19138, all of which had similar income and poverty data. The 2 most common suburban neighborhoods identified for maxillofacial trauma were postal codes 19403 and 19401 (Figure 3). The median income for postal code 19403 was $79 455, with 5.1% of the population living below the poverty line. The median income for postal code 19401 was $48 466, with 19.4% of the population living below the poverty line.[26]
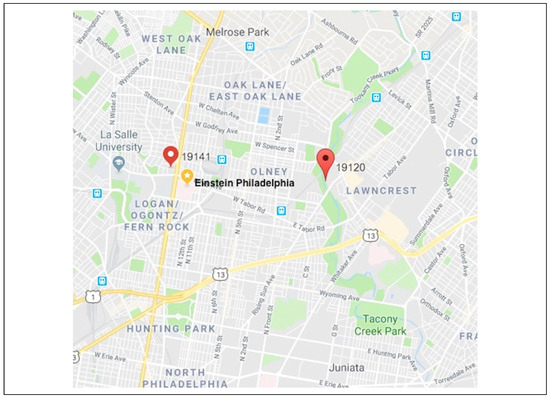
Figure 2.
A map of the urban neighborhoods, by zip code, with the most identified cases of maxillofacial trauma.
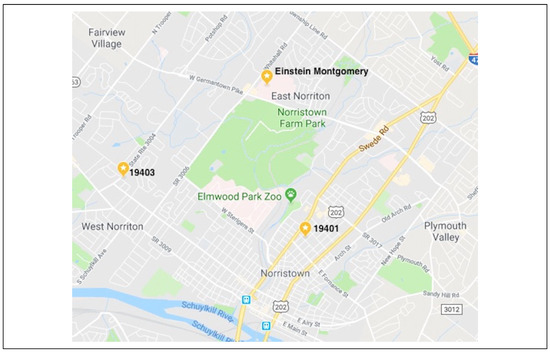
Figure 3.
A map of the suburban neighborhoods, by zip code, with the most identified cases of maxillofacial trauma.
In the urban environment, the most common fracture type was mandible and multiple (24%), followed by maxilla (16%), orbit (15%), zygomaticomaxillary complex (ZMC, 10%), zygoma (5%), nasoorbitoethmoid (NOE, 4%), and frontal sinus (<1%). In the suburban environment, the most common fracture type was mandible and orbit (26%), followed by multiple (20%), zygoma (7%), ZMC (7%), and NOE (4%). In the suburban setting, there were no maxilla or frontal sinus fractures. However, there were no other significant differences between the 2 environments with regard to the fracture type (Table 2).

Table 2.
Fracture Patterns in the Urban and Suburban Settings.
In our 2 cohorts, the distribution of race was shown to be significantly different (χ2 = 55.5, p < 0.0001). Patients in the urban population were more likely to be African American (70% vs. 33%) and Hispanic (15% vs. 7%) but less likely to be Caucasian (12% vs. 55%) compared to the suburban population. The urban population was more likely to present to the hospital overnight during the hours of 10 PM to 6 AM compared to the suburban population (44% vs. 24%, χ2 = 6.8, p < 0.01). Urban patients were more likely to be single (70% vs. 47%, χ2 = 16.5, p < 0.01), unemployed (64% vs. 44%, χ2 = 18.7, p < 0.001), and receive Medicaid coverage (58% vs. 26%, χ2 = 25.6, p < 0.001) compared to suburban patients (Table 1).
The method of injury between our 2 cohorts was also distinctive (χ2 = 24.9, p < 0.0001). Urban patients were more likely to be victims of assault (63% vs. 44%), whereas suburban patients were more likely to sustain accidental injuries (16% vs. 2%). There were notable differences between the 2 groups regarding the method of assault (χ2 = 5.8, p = 0.05). Although the most common method of assault in urban and suburban settings was by hands and feet (63% and 88%, respectively), urban victims were more likely to be assaulted with an object (30% vs. 12%) or gun (7% vs. 0%; Table 3).

Table 3.
Analysis of Assault Patterns.
Nineteen (7%) of the total study population were victims of domestic abuse. There appears to be appreciable differences in fracture type based on domestic abuse status (χ2 = 16.1, p < 0.05). Victims of domestic abuse were more likely to sustain isolated orbital fractures (47% vs. 15%) and less likely to sustain multiple fractures (11% vs. 25%) compared to nondomestic violence victims. We did not identify any notable maxillofacial trauma patterns in incarcerated patients.
Discussion
A scant number of international studies have examined urban and suburban maxillofacial trauma in the literature. One study examining maxillofacial trauma patterns in the suburban setting found that the majority of incidents occurred as a result of MVAs, with mandibular fractures being the most common fracture (57.1%).[23] The data are more robust from the urban perspective. Multiple studies across several African and European nations, as well as Brazil, have found the male sex and mandibular fractures to be the most frequent in incidence, consistent with the suburban data. However, etiology differs among these, as some have found MVAs to have the largest frequency of root cause, while others report higher rates of violence and assault.[21,22,27,28,29,30]
Fewer domestic studies have categorized trauma by population breakdown in the urban and suburban settings. An early study in an urban Kentucky center was one of the first to identify assault as a primary mechanism of maxillofacial trauma, with the majority of patients being male with mandibular fractures.[31] Another urban series identified assault to be the most common mechanism of injury for zygoma fractures. The majority of patients in this series were male (80%).[20] Further domestic urban studies have redemonstrated males to be the most common victims, assault the most common etiology, and the mandible the injured facial bone, which are consistent with the above discussed international data.[19,32,33]
In our study, patients from both the urban and suburban environments were predominately male between 26 and 60 years of age with increased trauma events during the spring and summer months. Urban patients were more likely to be victims of assault, whereas suburban patients were more likely to sustain accidental injuries. Although the most common method of assault in urban and suburban settings was by hands and feet, urban victims were more likely to be assaulted with an object or gun. Both populations had a significant number of mandibular fractures. The urban victims were more likely to have multiple fractures, while the suburban victims were more likely to sustain orbital fractures. However, this was not statistically significant.
We propose several reasons for assault being the primary mechanism of injury in the urban setting. The urban community in Philadelphia has fewer highways. As a result, there are fewer motor vehicle collisions. Furthermore, assault victims are more likely to be affected by socioeconomic and behavioral health issues, including domestic abuse, drugs, gang violence, and poverty.[32] In our study, we identified several urban neighborhoods where maxillofacial trauma was prevalent. The urban population was composed more of African American and Hispanic individuals compared to the suburban population. The urban population was more likely to present to the hospital overnight, between the hours of 10 PM and 6 AM, compared to the suburban population. Additionally, urban patients were more likely to be single, unemployed, and receive Medicaid coverage compared to suburban patients. This was further supported by the income and poverty data from the US Census Bureau. The urban neighborhoods identified had lower incomes, with higher percentages of patients living below the poverty line. However, one suburban population had significantly lower incomes and higher percentages of patients living below the poverty line compared to a neighboring suburban community.[26] This may demonstrate a more heterogenous environment and patient population.
Every year millions of people sustain injuries, in some instances, fatal ones, from domestic and community violence. Violence is a major cause of death in people aged 15 to 44 years worldwide. There are several forms of violence, including domestic situations among family members or intimate partners or those associated with criminal behavior, such as assaults, fights, kidnappings, and murders that occur among individuals who may or may not know one another.[22] In our study, 7% of individuals were victims of domestic abuse. This was consistent with the literature, which shows that the majority of violence occurs in the community rather than in the form of domestic abuse.[22] Our series also showed that victims of domestic abuse were more likely to sustain orbital fractures and less likely to sustain multiple fractures compared to nondomestic violence victims. These results are consistent with previous studies.[34,35,36]
Trauma in prisons has been studied; however, particular focus on maxillofacial trauma has not been conducted. Prisons are violent environments and injuries among prisoners occur at a significantly higher rate compared to the general population. Additionally, prisoners are more likely to have issues with anger and impulsivity resulting in violent behaviors.[37] In the most recent study looking at trauma patterns in New York City prisoners, the most common injuries were mandible fractures (46.5%) and other facial
fractures (14.9%). Injuries were a result of violent conduct in 75.7% of cases. However, the specific fracture patterns were not identified.[37] In contrast, a study conducted at 2 Australian prisons reported that the most common causes of injury were sports-related.[38] Another study in Michigan reported that accidental injuries outnumbered violent injuries 4-fold.[39] A study in Canada revealed that the majority of traumatic injuries were reported as accidents and no maxillofacial fractures were noted.[40] This further supports the notion that maxillofacial trauma patterns are influenced by the environment. We cannot identify any notable maxillofacial trauma patterns in incarcerated patients due to the small sample size (n = 8, 3%) of incarcerated individuals in our study.
Knowledge of traumatic etiology patterns allows physicians and hospital administrators to adapt more appropriate measures and encourages legislative change. Previous research has indicated that hospital-initiated programs centered upon trauma-informed care have resulted in community-wide reductions in trauma and encouraged legislative change.[41] Comprehension of current societal issues in various settings allows for more appropriate legal and medical reform to further combat and mitigate traumabased pathology.
The results of this study should be interpreted within the context of certain limitations. This study is somewhat limited due to the fact that it is retrospective and lacked a control group. Additionally, the data are skewed because of the populations studied. For example, the patterns observed in this study can be a result of socioeconomic trends in that region. However, it will serve as a pilot to a more comprehensive study that will include control data from the National Trauma Data Bank.
Conclusions
Maxillofacial trauma patterns were shown to be significantly different in the urban versus suburban environment. Patients in the urban environment are more susceptible to assault due to several factors including age, race, and socioeconomic status. Providers should also be aware of victims of domestic abuse and prison violence.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Vrinceanu, D.; Banica, B. Principles of surgical treatment in the midface trauma—Theory and practice. Maedica (Buchar). 2014, 9, 361–366. [Google Scholar]
- Braun, T.L.; Maricevich, R.S. Soft tissue management in facial trauma. Semin Plast Surg. 2017, 31, 73–79. [Google Scholar]
- Elbaih, A.H.; El-Sayed, D.A.; Abou-Zeid, A.E.; Elhadary, G.K. Patterns of brain injuries associated with maxillofacial fractures and its fate in emergency Egyptian polytrauma patients. Chin J Traumatol. 2018, 21, 287–292. [Google Scholar] [CrossRef]
- Sahni, V. Psychological impact of facial trauma. Craniomaxillofac Trauma Reconstr. 2018, 11, 15–20. [Google Scholar] [CrossRef]
- Radabaugh, J.P.; Zhang, P.; Wang, D.; et al. Barriers to repair in maxillofacial trauma. JAMA Facial Plast Surg. 2016, 18, 177–182. [Google Scholar] [CrossRef] [PubMed]
- VandeGriend, Z.P.; Hashemi, A.; Shkoukani, M. Changing trends in adult facial trauma epidemiology. J Craniofac Surg. 2015, 26, 108–112. [Google Scholar] [CrossRef]
- Allareddy, V.; Allareddy, V.; Nalliah, R.P. Epidemiology of facial fracture injuries. J Oral Maxillofac Surg. 2011, 69, 2613–2618. [Google Scholar] [CrossRef] [PubMed]
- Hanba, C.; Svider, P.F.; Chen, F.S.; et al. Race and sex differences in adult facial fracture risk. JAMA Facial Plast Surg. 2016, 18, 441–448. [Google Scholar] [CrossRef]
- Vazquez, M.P.; Kadlub, N.; Soupre, V.; et al. Facial trauma and injury in children [in French]. Ann Chir Plast Esthet. 2016, 61, 543–559. [Google Scholar] [CrossRef]
- Reckdenwald, A.; Szalewski, A.; Yohros, A. Place, injury patterns, and female-victim intimate partner homicide. Violence Against Women. 2019, 25, 654–676. [Google Scholar] [CrossRef]
- Vidal, H.G.; Caldas, I.M.; Coelho Junior, L.; et al. Orofacial injuries in children and adolescents (2009–2013): A 5-year study in Porto, Portugal. Braz Dent J 2018, 29, 316–320. [Google Scholar] [CrossRef] [PubMed]
- Conceicao, L.D.; Da Silveira, I.A.; Nascimento, G.G.; Lund, R.G.; da Silva, R.H.A.; Leite, F.R.M. Epidemiology and risk factors of maxillofacial injuries in brazil, a 5-year retrospective study. J Maxillofac Oral Surg. 2018, 17, 169–174. [Google Scholar] [PubMed]
- Yu, Y.R.; DeMello, A.S.; Greeley, C.S.; Cox, C.S.; Naik-Mathuria, B.J.; Wesson, D.E. Injury patterns of child abuse: Experience of two level 1 pediatric trauma centers. J Pediatr Surg. 2018, 53, 1028–1032. [Google Scholar] [PubMed]
- Sarkar, R.; Ozanne-Smith, J.; Bassed, R. Systematic review of the patterns of orofacial injuries in physically abused children and adolescents. Trauma Violence Abuse 2021, 22, 136–146. [Google Scholar]
- Manodh, P.; Prabhu Shankar, D.; Pradeep, D.; Santhosh, R.; Murugan, A. Incidence and patterns of maxillofacial trauma—A retrospective analysis of 3611 patients-an update. Oral Maxillofac Surg. 2016, 20, 377–383. [Google Scholar]
- Assari, S. Race, education attainment, and happiness in the United States. Int J Epidemiol Res. 2019, 6, 76–82. [Google Scholar]
- Fournier, M.A. Dimensions of hierarchy as determinants of health and happiness. Curr Opin Psychol. 2019, 15, 110–114. [Google Scholar] [CrossRef]
- Davidson, L. Socioeconomic status of city and suburban populations. Stat Bull Metropol Life Insur Co. 1964, 45, 1–3. [Google Scholar]
- Ogundare, B.O.; Bonnick, A.; Bayley, N. Pattern of mandibular fractures in an urban major trauma center. J Oral Maxillofac Surg. 2003, 61, 713–718. [Google Scholar] [CrossRef]
- Scherer, M.; Sullivan, W.G.; Smith, D.J.; Phillips, L.G.; Robson, M.C. An analysis of 1423 facial fractures in 788 patients at an urban trauma center. J Trauma. 1989, 29, 388–390. [Google Scholar]
- Batista, A.M.; Marques, L.S.; Batista, A.E.; Falci, S.G.; Ramos-Jorge, M.L. Urban-rural differences in oral and maxillofacial trauma. Braz Oral Res. 2012, 26, 132–138. [Google Scholar] [CrossRef]
- Bernardino, Í.M.; Barbosa, K.G.N.; Nebrega, L.M.; Cavalcante, G.M.; d’Ávila, S. Interpersonal violence, circumstances of aggressions and patterns of maxillofacial injuries in the metropolitan area of Campina Grande, State of Paraíba, Brazil (2008–2011). Cien Saude Colet. 2017, 22, 3033–3044. [Google Scholar] [CrossRef] [PubMed]
- Ogunmuyiwa, S.A.; Gbolahan, O.O.; Ayantunde, A.A.; Odewabi, A.A. Patterns, severity, and management of maxillofacial injuries in a suburban South Western Nigeria tertiary center. Niger J Surg. 2015, 21, 38–42. [Google Scholar] [PubMed]
- Ugboko, V.; Udoye, C.; Ndukwe, K.; Amole, A.; Aregbesola, S. Zygomatic complex fractures in a suburban Nigerian population. Dent Traumatol. 2005, 21, 70–75. [Google Scholar] [CrossRef] [PubMed]
- City of Philadelphia. Community health assessment. Philadelphia Department of Public Health. Available online: https://www.phila.gov/doc uments/community-health-assessment/ (accessed on 19 December 2018).
- United States Census Bureau. 2012–2016 American Community Survey 5-Year Estimates. Available online: https://www.census.gov/acs/ www/data/data-tables-and-tools/data-profiles/2016/ (accessed on 19 December 2018).
- Starkhammar, H.; Olofsson, J. Facial fractures: A review of 922 cases with special reference to incidence and aetiology. Clin Otolaryngol Allied Sci. 1982, 7, 405–409. [Google Scholar] [CrossRef]
- Beaumont, E.; Lownie, J.F.; Cleaton-Jones, F.E.; Neetyon, N.P. An analysis of fractures of the facial skeleton in three populations in the Johannesburg urban area. J Dent Assoc S Afr. 1985, 40, 633–638. [Google Scholar]
- Brook, I.M.; Wood, N. Aetiology and incidence of facial fractures in adults. Int J Oral Surg. 1983, 12, 293–298. [Google Scholar] [CrossRef]
- Olayemi, A.B.; Adeniyi, A.O.; Samuel, U.; Emeka, O.A. Pattern, severity, and management of cranio-maxillofacial soft-tissue injuries in Port Harcourt, Nigeria. J Emerg Trauma Shock. 2013, 6, 235–240. [Google Scholar] [CrossRef]
- Neal, D.C.; Wagner, W.F.; Fielder, L.D.; Alpert, B. The epidemiology of facial fractures. J Ky Med Assoc. 1978, 76, 275–278. [Google Scholar]
- Greene, D.; Raven, R.; Carvalho, G.; Maas, C.S. Epidemiology of facial injury in blunt assault. Determinants of incidence and outcome in 802 patients. Arch Otolaryngol Head Neck Surg. 1997, 123, 923–928. [Google Scholar] [CrossRef]
- Kelley, P.; Crawford, M.; Higuera, S.; Hollier, L.H. Two hundred ninety-four consecutive facial fractures in an urban trauma center: Lessons learned. Plast Reconstr Surg. 2005, 116, 42e–49e. [Google Scholar] [CrossRef] [PubMed]
- Arosarena, O.A.; Fritsch, T.A.; Hsueh, Y.; Aynehchi, B.; Haug, R. Maxillofacial injuries and violence against women. Arch Facial Plast Surg. 2009, 11, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Gayford, J.J. Wife-battering: A preliminary survey of 100 cases. Br Med J. 1975, 1, 194–197. [Google Scholar] [CrossRef][Green Version]
- Hill, C.M.; Crosher, R.F.; Carroll, M.J.; Mason, D.A. Facial fractures: The results of a prospective four-year study. J Maxillofac Surg. 1984, 12, 267–270. [Google Scholar] [CrossRef]
- Henning, J.; Frangos, S.; Simon, R.; Pachter, H.L.; Bholat, O.S. Patterns of traumatic injury in New York City prisoners requiring hospital admission. J Correct Health Care. 2015, 21, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Butler, T.; Kariminia, A.; Trevathan, L.; Bond, J. Injury surveillance in the New South Wales prison system. Health Promot J Aust. 2004, 15, 151–154. [Google Scholar] [CrossRef]
- Green, L.; Hutchinson, C.; Lamb, D.; Johnson, D.; Wilcox, K. Injury surveillance in correctional facilities—Michigan, April 1994-March 1995. Morb Mortal Wkly Rep. 1996, 45, 69–72. [Google Scholar]
- O’Connor, H.M.; Stringer, D.G. Review of traumatic injuries in regional federal penitentiaries. Can Med Assoc J. 1985, 133, 204–205. [Google Scholar]
- Bowen, E.A.; Murshid, N.S. Trauma-informed social policy: A conceptual framework for policy analysis and advocacy. Am J Public Health. 2016, 106, 223–229. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2020 by the author. The Author(s) 2020.