Abstract
Study Design: A two-alternative forced choice design was used to gather perceptual data regarding unicoronal synostosis (UCS). Objective: Cranial vault remodeling aims at improving the aesthetic appearance of infants with UCS by reshaping the forehead and reducing the potential for psychosocial discrimination. People’s perception of craniofacial deformity plays a role in the stigma of deformity. The purpose of this study is to examine the relationship between objective skull deformity in UCS patients and laypersons’ perception of skull normality. Methods: Forty layperson skull raters were recruited from the general public. Skull raters were asked to categorize 45 infant skull images as normal or abnormal. Twenty-one of the images were UCS skulls, and 24 were normal skulls. Skulls were displayed briefly on a computer to simulate a first impression scenario and generate a perceptual response. A χ2 analysis and mixed-effects regression model were used to analyze the response data. Results: Members of the general public were good at distinguishing between skull groups, χ2 (1) = 281.97, p < 0.001. In addition, skull raters’ responses were predicted by the severity of deformity in the UCS skulls (b = −0.10, z = −2.6, p = 0.010, CI: −0.18, −0.02). A skull with a deformity value of 2.8 mm (CI: 1.8, 4.1) was equally likely to be rated normal or abnormal. Conclusions: This is the first study to investigate the relationship between objective skull deformity in UCS and public perception. Laypersons were good at distinguishing the difference between normal and UCS skulls, and their perceptions of normality were predicted by the degree of skull deformity.
Background
Unilateral coronal craniosynostosis (UCS) is a common subtype of craniosynostosis that affects the shape of an infant’s skull resulting in anterior plagiocephaly, a phenotype characterized by an asymmetric forehead appearance.[1] Facial attractiveness ratings of children with cranosynostosis by laypersons are lower than their age and sex-matched peers.[2] As a result, children with untreated craniosynostosis may face psychosocial adjustment challenges.[3] Cranial vault remodeling (CVR) surgery aims at improving the aesthetic appearance of children with UCS by reshaping the bones that form the contour of the forehead.[4] Specifically, fronto-orbital advancement (FOA) consists of reshaping the frontal bones and the superior orbital region and remains a firstline treatment for UCS.[5]
Reported outcomes in the literature regarding surgical treatment for UCS focus attention on the restoration of a normal head shape and an improved aesthetic appearance. Photographic assessment is frequently used to demonstrate an aesthetic improvement as well as reports on the presence of common morphological features associated with UCS.[6,7,8,9,10,11] Similarly, the popular Whitaker scale, a tool used to assess severity of deformity in patients with craniosynostosis, is based on surgeons’ subjective assessment of a patient’s appearance.[12] All of these methods rely on perceptions of experts in craniofacial reconstruction. However, previous studies on facial attractiveness have shown that patients’ perceptions may not always correlate with experts’ perceptions.[13,14]
A primary goal of CVR is to improve the appearance of an infant’s head to prevent psychosocial discrimination later in life. In general, psychosocial discrimination is a consequence of perceptions of the general public as opposed to assessments of craniofacial experts. However, there are no outcome measurements that correlate surgical outcome with laypersons’ perception of skull normality.
Therefore, the goal of this study was to determine whether there is a relationship between an objective value of skull deformity and laypersons’ perceptions of skull appearances. Additional objectives were to determine whether there were other factors influencing peoples’ ratings of skull appearance and to determine if there is a threshold value whereby members of the general public are unable to decipher the difference between a normal and a UCS skull. The primary interest in this study was to simulate and investigate a first impression scenario, thus mimicking a common situation, where rapid judgments are made regarding peoples’ appearances.
Methods
Participants
After Institutional Ethics Review Board approval (Pro85714), there were 2 groups of participants in this study. The first group consisted of 40 layperson skull raters who were recruited from the general public. All skull raters were adults living in Edmonton with nonsurgical backgrounds. The average age of the raters was 33.6 years (standard deviation [SD] = 12.4), consisting of 21 females and 19 males. Most of the raters had a postsecondary level of education (92.5%).
The second group consisted of infants whose skull images were rated by the first group. A waiver of consent was granted to access the infant skull data. This group was subdivided into a UCS cohort and a normal cohort. Infants treated for UCS between 2001 and 2019 were identified and their preoperative computed tomography (CT) scans were extracted from a radiology database. A group of normal controls with CT scans was identified with the same database. The control cohort consisted of CT scan data retrospectively collected from infants less than 2 years of age, had CT head scans with ≤1 mm slices in coronal, axial, and sagittal planes, and had no skeletal craniofacial abnormalities, including skull bone fractures and congenital deformities (i.e., craniosynostosis). Two years was selected as the maximum age cutoff for the skull groups, as this corresponds with when most children with craniosynostosis would be diagnosed by in order to take advantage of optimum surgical timing.[5] The UCS cohort consisted of infants with similar age and sex demographics to the control group who had single suture coronal synostosis in the absence of any additional skeletal abnormalities. Skull data were collected from 45 infants. There were 21 participants in the UCS cohort and 24 participants in the normal skull cohort. The majority of the skull participants were female with right-sided UCS. The 2 cohorts did not significantly differ statistically regarding age (Mann–Whitney U test = 184, p = 0.12) and sex (χ2 = 0.164, p = 0.69) variables. Demographic data for the skull raters and the skull groups are summarized in Table 1 and Table 2. Surface distance values were used to quantify deformity in the UCS cohort and ranged from 1.97 to 10.36 mm, with an average value of 6.06 mm and SD of 2.06 mm. Figure 1 displays the distribution of surface distance values.

Table 1.
Summary of Demographic Data for the Layperson Skull Raters.

Table 2.
Summary of Demographic Data for the Skull Cohorts.
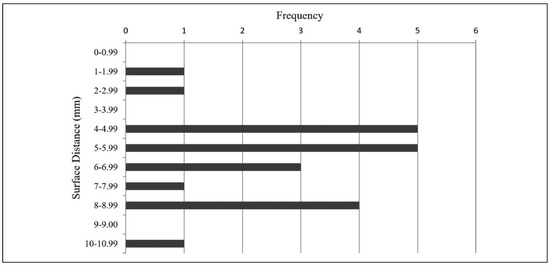
Figure 1.
Distribution of surface distance values among the UCS skull cohort. UCS indicates unilateral coronal craniosynostosis.
Experimental Design
Three-dimensional (3D) skull models were generated for all 45 infant participants using an identical protocol. The digital imaging and communications in medicine data from CT head and/or CT facial bone scans were imported into the open-access software 3D Slicer (version 11.0).[15] In 3D Slicer, the facial skeleton was segmented and a stereolithography (STL) file was generated. Mandibles were removed from the image files to isolate the cranial vault as the region of interest. STL files were imported into KeyShot (version 8.2.80) rendering software to standardize the display environment for all skull models, as shown in Figure 2 (i.e., lighting, color, skull orientation, etc).
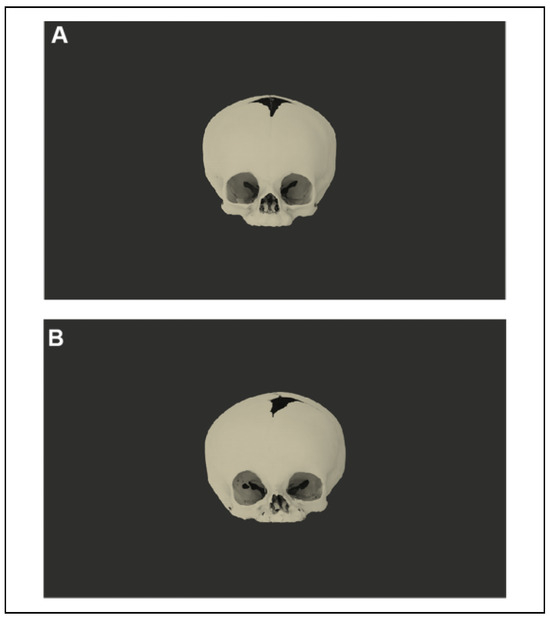
Figure 2.
Examples of a skull model as they appeared on the computer screen. (A) An example of a normal 3D skull model generated for this study. (B) An example of a UCS 3D skull model generated for this study.
A 2-alternative forced choice method was used for this study. Images were displayed to each skull rater on a Microsoft PowerPoint (Microsoft PowerPoint for Mac 2011, version 14.7.7) presentation on the same laptop computer (Figure 3). Each skull model was displayed on the screen for 300 milliseconds in randomized order, followed by 5 s to record a response. Raters were given a recording sheet with the skull number and the letter “N” or “A” to circle, corresponding to “normal” and “abnormal.” Following a brief training session on the features of normal infant skulls, participants began the study and were asked to record whether they thought each displayed skull was normal or abnormal. The experimental design was piloted 5 times to optimize the simulation of a first impression scenario and ensure a smooth flow of events. For the pilot sessions, stimulus duration and interstimulus duration were varied from 0.1 to 3 s and 3 to 5.3 s, respectively, with a 3to 5-s countdown between each stimulus. Based on participant feedback regarding task difficulty, stimulus and interstimulus duration were adjusted.
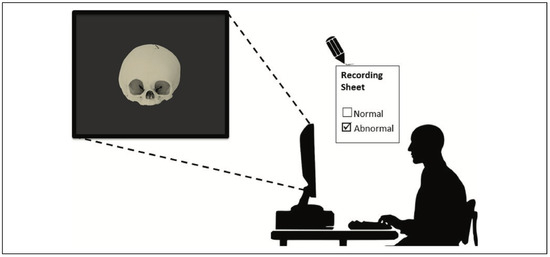
Figure 3.
Experimental setup. Skull raters viewed the skull images on a laptop computer screen and were asked to categorize each skull as “normal” or “abnormal.” Responses were recorded on an answer sheet. Each skull was displayed for 0.3 s, and raters had 5 s to record a response.
Surface Distance Measurement
Frontal bone surface distances were calculated for the UCS cohort in order to assign a quantitative value for cranial vault deformity in each skull. The degree of deformity was determined using the workflow outlined in Figure 4. In 3D Slicer, a CT scan from the UCS cohort was imported along with an age and sex-matched normal CT scan (control skull). The control skull was the only manipulated image in the workflow in order to reduce the possibility of artificially exaggerating or muting the deformity in the UCS skull. The skulls were then manually aligned, followed by an automatic geometry-based rigid registration to obtain the best interskull comparison possible. Once registered, the skull bones were segmented from the CT scans and then further segmented to isolate the frontal bones for each skull. Hausdorff surface distances are standard units in medical image software analysis and were used to quantify UCS deformity at the frontal bone region in this study. In 3D Slicer, distances were automatically calculated in millimeters between the UCS and normal CT frontal bones using the segment comparison module. Using this method, a larger surface distance corresponds to a forehead that is positioned more posteriorly on the synostotic side when compared to an age and sex-matched normal skull. Normal skulls are used as the control skulls and are therefore assumed to have a deformity value of 0 mm. The value generated used this method as a surrogate marker for the severity of anterior plagiocephaly in a UCS skull. Frontal bones were selected as the target area to measure deformity since they constitute the forehead, and therefore represent an area of the facial skeleton that is noticeable to onlookers. In addition, the frontal bones are manipulated in FOA procedures to correct anterior plagiocephaly and are therefore of particular interest.

Figure 4.
Overview of the workflow used to determine surface distance values.
Analyses
A χ2 analysis was used to determine whether skull raters were able to distinguish between abnormal (UCS) and normal skulls. A mixed-effects logistic regression model was fitted to the response data for the UCS skulls to determine whether the objective values of skull deformity impacted raters’ responses. A similar model was used to solve for a threshold value of deformity and was fitted to all available data including the normal skulls. The threshold value was defined as the point along the surface distance scale, where the statistically estimated psychometric response curve assumed a value of 50%. This number represents the objective value of deformity whereby the responses from the skull raters were equally split between normal and abnormal. Skull presentation order was analyzed to determine whether this factor influenced rater responses.
Results
The skull raters were able to accurately distinguish between normal skulls and UCS skulls the majority of the time, χ2 (1, N = 40) = 281.97, p < 0.001. When shown a UCS skull, layperson raters correctly categorized the skull as “abnormal” 71% of the time. Similarly, when shown a normal skull, the raters categorized the skull as “normal” 69% of the time (Figure 5).
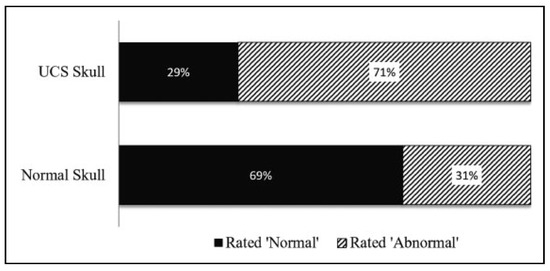
Figure 5.
Results of the χ2 analysis of skull rater responses.
A mixed-effects logistic regression model fitted to the response data for the UCS skulls revealed that the objective values of skull deformity predicted raters’ categorization of the skulls. Larger surface distance values for the UCS skulls, corresponding to more a significant forehead deformity, resulted in layperson raters being more likely to rank a skull as abnormal versus normal (b = 0.10, z = −2.6, p = 0.010 [confidence interval (CI): −0.18, −0.02]).
Based on the mixed-effects regression model that was fitted to all the available data including normal skulls, a threshold value of deformity of 2.8 mm (CI: 1.8, 4.1) was determined based on the degree to which the objective value of deformity impacted responses (b = −0.27, z = −15.6, p = 0.0000 [CI: −0.23, −0.30]). The steeper slope in this model, compared to the model containing only UCS skulls, reflects the homogeneity of the values assigned to the normal skulls (i.e., all zeroes). The skull presentation influenced the rater responses so that skull raters were 1.4% more likely to rank each subsequent skull as normal as they progressed, resulting in a relative increase of “normal” responses toward the end of the experiment.
Discussion
In a simulated first impression scenario, members of the general public were able to differentiate between the normal and the abnormal skulls. This performance is impressive, given the complex geometry of an infant craniofacial skeleton and the very rapid exposure time in this study. This highlights the sensitivity of human visual perception to changes in facial symmetry particularly in the upper third of the face, which has been demonstrated previously.[16]
In addition, UCS skulls with more severe anterior plagiocephaly were visually more salient than the skulls with a more subtle deformity. The methods of quantifying deformity in this study strictly isolated the asymmetry in the frontal bones of the UCS skulls. These findings suggest that while there are a number of skeletal differences between the normal infant and UCS skulls, the characteristic features of contralateral forehead bossing and ipsilateral flattening are a feature driving people’s responses. This is in keeping with findings by Hohman et al. [16] and Kim et al.[17] that report humans are more perceptive to changes in upper versus lower face symmetry.
Another factor that influenced raters’ responses was the order of skull exposure. People were more likely to categorize a skull as normal if it appeared later in the presentation. Response fatigue in 2-alternative forced choice tasks may have contributed to the response pattern in this study.
The threshold value of 2.8 mm determined in this study suggests a degree of UCS deformity that would be difficult to detect by laypersons. This value is consistent with findings in the perception literature and is close to the range determined by previous studies (3–4 mm) looking at perceptions of facial asymmetry and detectable differences.[18,19] Therefore, a 2.8 mm frontal bone discrepancy may serve as a reasonable goal to aim for when planning FOA procedures. Virtual surgical planning (VSP) for CVR is becoming more popular among craniofacial surgeons.[6,7,9,10,20,21,22,23,24,25,26,27,28] VSP has been shown to reduce the subjectivity of surgical decision-making, reduce operating time, and yield aesthetic reconstruction results.[6,23,27] With the development and implementation of cost-effective ways to consistently utilize VSP, it is likely to become an increasingly ubiquitous tool in the surgical planning environment. A quantitative endpoint that is easily measured using cost-free software may be a valuable component in the planning armamentarium for FOA procedures.
CVR procedures are lengthy and associated with several risks such as significant bleeding.[29] The threshold value in this study may be useful information for consultation appointments between surgeons and parents of infants with UCS when considering treatment options. While the mortality and morbidity of these surgeries have improved over the years, the process of considering one’s infant for an invasive procedure involving removal and reshaping of the skull can be considered daunting.
Limitations
One of the limitations of this study is the lack of small surface distance values for the UCS skull cohort (Figure 1) preventing the ability to determine a threshold value based on UCS data alone. However, a craniosynostosis diagnosis requires clinical suspicion based on noticeable deformity, therefore making it unlikely to detect UCS in infants who may have very minimal frontal bone asymmetry. Therefore, UCS data may not, by definition, be available for small deformities.
Additional limitations of this study are the lack of naturalness in the stimuli and the use of CT scans as the imaging modality. Regarding the stimuli, layperson raters were shown 3-D skull models as opposed to pictures of infant faces. The absence of soft tissue in the study stimuli takes away from the applicability of the findings to everyday life. However, the amount of soft tissue overlying the skull in infants less than 2 years of age is minimal, and the deformity present in the facial skeleton is likely to be well reflected in the soft tissue. In addition, while CT scans are used for surgical planning and allow for reliable measurement of the deformity objectively, CT data are not available for all UCS infants and obtaining CT scans after surgery is rarely justified clinically. Hence, using alternative imaging modalities like photogrammetry offers an attractive option for future studies on perception. The use of CT images in this study is consistent with commonly employed virtual planning practices, allowing the threshold information gathered to be related directly to the current planning environment.
Future Direction
Future direction with this research includes conducting a similar experiment using clinical photographs or 3D scanning images of infants with uncorrected UCS to increase the transferability of the findings to a real-life scenario. In addition, while social discrimination is generally viewed as a construct of general public perception, it can be more accurately described as a result of ones’ peers’ perceptions. Futures studies will involve recruiting child peers as skull raters to perform a similar task and determining if there are differences between adult and child raters when it comes to craniofacial morphology.
Conclusions
This study investigated the relationship between objective skull deformity in UCS and public perception. Layperson raters were effective at correctly categorizing normal and abnormal infant skulls when displayed very briefly, simulating a first impression scenario. Laypersons’ perceptions of abnormality were predicted by an objective value of skull deformity, which was determined by surface distance values measured at the forehead region. The perceptual threshold value of deformity identified in this study is in keeping with values determined in other studies investigating perceptual visual thresholds in facial differences. This information may be helpful when counseling parents and patients, and for preoperative surgical planning of CVR surgeries.
Authors’ Note
This work was presented at Advanced Digital Technologies in Head and Neck Reconstruction (ADT) 2019 in Tokyo, Japan. Ethics for this study was approved by the Health Ethics Institutional Review Board (Pro00085714).
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding from the Covenant Research Center SEED Grant was provided for this article.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Campbell, C.; Derderian, C. Jeffrey, E.J., Ed.; Craniosynostosis. In Essentials of Plastic Surgery, 2nd ed; Taylor & Francis Group: Boca Raton, FL, USA, 2014; p. 237. [Google Scholar]
- Collett, B.R.; Gray, K.E.; Kapp-Simon, K.A.; Birgfeld, C.; Cunningham, M.; Rudo-Stern, J.; et al. Laypersons’ ratings of appearance in children with and without single-suture craniosynostosis. J Craniofac Surg. 2013, 24, 1331–1335. [Google Scholar] [CrossRef] [PubMed]
- Snyder, H.; Pope, A.W. Psychosocial adjustment in children and adolescents with a craniofacial anomaly: Diagnosis-specific patterns. Cleft Palate Craniofac J. 2010, 47, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Alford, J.; Derderian, C.A.; Smartt, J.M. Surgical treatment of nonsyndromic unicoronal craniosynostosis. J Craniofac Surg. 2018, 29, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- Tahiri, Y.; Bartlett, S.P.; Gilardino, M.S. Evidence-based medicine: Nonsyndromic craniosynostosis. Plast Reconstr Surg. 2017, 140, 177–191. [Google Scholar] [CrossRef]
- Chim, H.; Wetjen, N.; Mardini, S. Virtual surgical planning in craniofacial surgery. Semin Plast Surg. 2014, 28, 150–158. [Google Scholar] [CrossRef]
- Fisher, M.; Medina, M.; Bojovic, B.; Ahn, E.; Dorafshar, A. Indications for computer-aided design and manufacturing in congenital craniofacial reconstruction. Craniomaxillofac Trauma Reconstr. 2016, 9, 235–241. [Google Scholar] [CrossRef]
- Hilling, D.E.; Vaandrager, J.M. Long-term aesthetic results of frontoorbital correction for frontal plagiocephaly. J Neurosurg. 2006, 105 (Suppl. 1), 21–25. [Google Scholar] [CrossRef]
- Mardini, S.; Alsubaie, S.; Cayci, C.; Chim, H.; Wetjen, N. Three dimensional preoperative virtual planning and template use for surgical correction of craniosynostosis. J Plast Reconstr Aesthet Surg. 2014, 67, 336–343. [Google Scholar] [CrossRef]
- Soleman, J.; Thieringer, F.; Beinemann, J.; Kunz, C.; Guzman, R. Computer-assisted virtual planning and surgical template fabrication for frontoorbital advancement. Neurosurg Focus. 2015, 38, 1–5. [Google Scholar] [CrossRef]
- Taylor, J.A.; Paliga, J.T.; Wes, A.M.; et al. A critical evaluation of long-term aesthetic outcomes of fronto-orbital advancement and cranial vault remodeling in nonsyndromic unicoronal craniosynostosis. Plast Reconstr Surg. 2015, 135, 220–231. [Google Scholar] [CrossRef]
- Whitaker, L.; Pashayan, H.; Reichman, J. A proposed new classification of craniofacial anomalies. Cleft Palate J. 1981, 18, 161–176. [Google Scholar] [PubMed]
- Vargo, J.K.; Gladwin, M.; Ngan, P. Association between ratings of facial attractivess and patients’ motivation for orthognathic surgery. Orthod Craniofacial Res. 2003, 6, 63–71. [Google Scholar] [CrossRef]
- Cochrane, S. A comparison of the perception of facial profile by the general public and 3 groups of clinicians. Int J Adult Orthodon Orthognath Surg. 1999, 14, 291–295. [Google Scholar]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; FillionRobin, J.C.; Pujol, S.; et al. 3D Slicer as an image computing platform for the quantitative imaging network. Magn Reson Imaging. 2012, 30, 1323–1341. [Google Scholar] [CrossRef]
- Hohman, M.H.; Kim, S.W.; Heller, E.S.; Frigerio, A.; Heaton, J.T.; Hadlock, T.A. Determining the threshold for asymmetry detection in facial expressions: Detection of facial asymmetry. Laryngoscope 2014, 124, 860–865. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.W.; Heller, E.S.; Hohman, M.H.; Hadlock, T.A.; Heaton, J.T. Detection and perceptual impact of side-to-side facial movement asymmetry. JAMA Facial Plast Surg. 2013, 15, 411–416. [Google Scholar] [CrossRef]
- Choi, K.Y. Analysis of facial asymmetry. Arch Craniofacial Surg. 2015, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Chu, E.A.; Farrag, T.Y.; Ishii, L.E.; Byrne, P.J. Threshold of visual perception of facial asymmetry in a facial paralysis model. Arch Facial Plast Surg. 2011, 13, 14–19. [Google Scholar] [CrossRef]
- Burge, J.; Saber, N.R.; Looi, T.; French, B.; Usmani, Z.; Anooshiravani, N.; et al. Application of CAD/CAM prefabricated age-matched templates in cranio-orbital remodeling in craniosynostosis. J Craniofac Surg. 2011, 22, 1810–1813. [Google Scholar] [CrossRef]
- Zhao, L.; Patel, P.K.; Cohen, M. Application of virtual surgical planning with computer assisted design and manufacturing technology to cranio-maxillofacial surgery. Arch Plast Surg. 2012, 39, 309. [Google Scholar] [CrossRef]
- Jans, G.; Sloten, J.V.; Gobin, R.; Van der Perre, G.; Audekercke, R.V.; Mommaeits, M. Computer-aided craniofacial surgical planning implemented in CAD software. Comput Aided Surg. 1999, 4, 117–128. [Google Scholar] [CrossRef]
- Seruya, M.; Borsuk, D.E.; Khalifian, S.; Carson, B.S.; Dalesio, N.M.; Dorafshar, A.H. Computer-aided design and manufacturing in craniosynostosis surgery. J Craniofac Surg. 2013, 24, 1100–1105. [Google Scholar] [CrossRef] [PubMed]
- Safran, T.; Viezel-Mathieu, A.; Beland, B.; Azzi, A.J.; Galli, R.; Gilardino, M. The state of technology in craniosynostosis. J Craniofac Surg. 2018, 29, 904–907. [Google Scholar] [CrossRef] [PubMed]
- Queiros, C.; Joly, A.; Paré, A.; Listrat, A.; Travers, n.; Goga, D.; et al. Use of cutting guides during craniosynostosis sequelae surgery: A comparative study between computer-assisted planning and post-operative results. J Cranio-Maxillofac Surg. 2017, 45, 1062–1068. [Google Scholar] [CrossRef]
- LoPresti, M.; Daniels, B.; Buchanan, E.P.; Monson, L.; Lam, S. Virtual surgical planning and 3D printing in repeat calvarial vault reconstruction for craniosynostosis: Technical note. J Neurosurg Pediatr. 2017, 19, 490–494. [Google Scholar] [CrossRef] [PubMed]
- Khechoyan, D.Y.; Saber, N.R.; Burge, J.; Fattah, A.; Drake, J.; Forrest, C.R.; et al. Surgical outcomes in craniosynostosis reconstruction: The use of prefabricated templates in cranial vault remodelling. J Plast Reconstr Aesthet Surg. 2014, 67, 9–16. [Google Scholar] [CrossRef]
- Mommaerts, M.Y.; Jans, G.; Sloten, J.V.; Staels, P.F.J.; Van der Perre, G.; Gobin, R. On the assets of cad planning for craniosynostosis surgery. J Craniofac Surg. 2001, 12, 547–554. [Google Scholar] [CrossRef]
- Lee, H.Q.; Hutson, J.M.; Wray, A.C.; Lo, P.A.; Chong, D.K.; Holmes, A.D.; et al. Analysis of morbidity and mortality in surgical management of craniosynostosis. J Craniofac Surg. 2012, 23, 1256–1261. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2020 by the author. The Author(s) 2020.