A Comparative Study Between Concentric Single-Needle Puncture Technique and Conventional 2-Needle Technique for Temporomandibular Joint Arthrocentesis Plus Corticosteroid Injections
Abstract
:Introduction
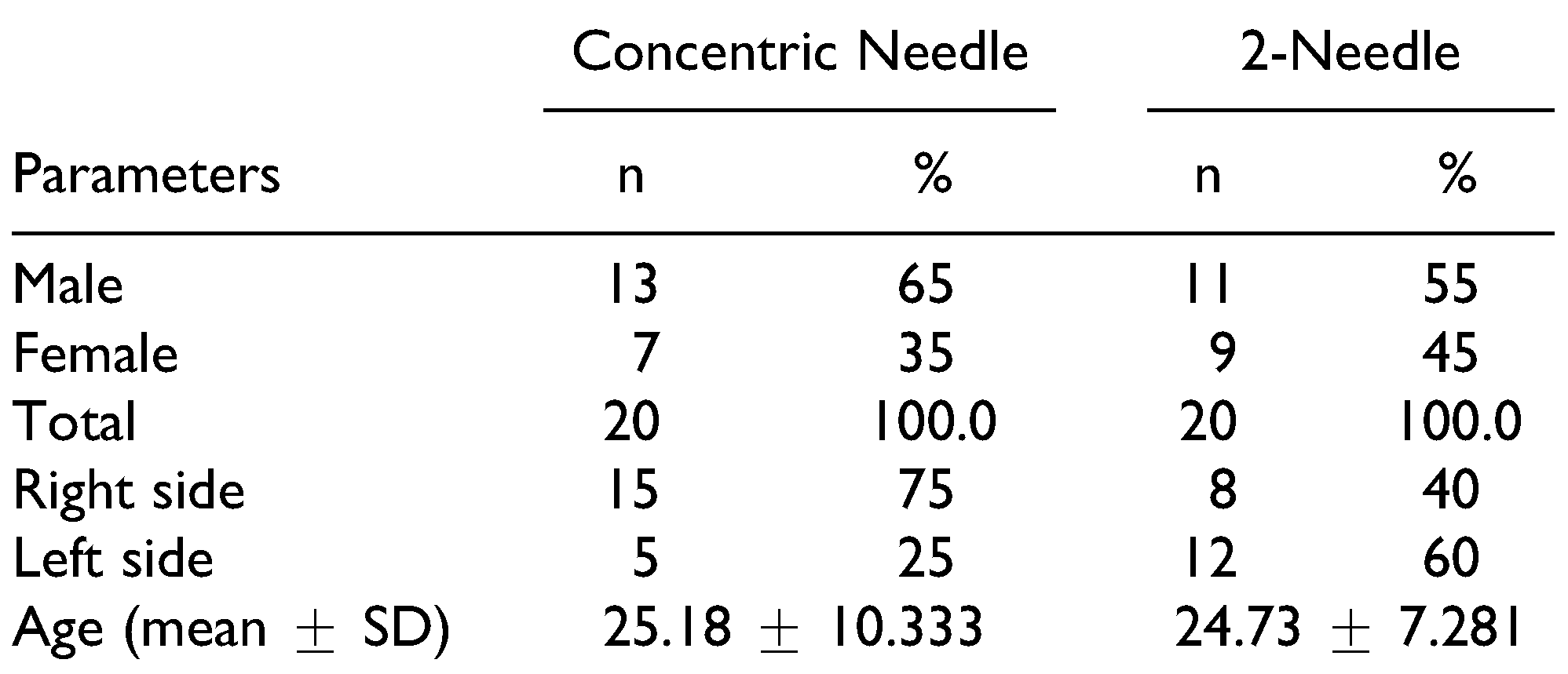
Materials and Method
- Mouth opening was measured with a metallic scale.
- Postoperative pain relief, pain at rest, and pain on chewing were measured by 10-point visual analog scale, as described by Guarda-Nardini et al., with 0 being the absence of pain and 10 being the worst pain ever.
- Subjective chewing efficacy was also measured on a 0- to 10-point visual analog scale (0 being worst efficiency ever and 10 being the best efficiency ever).
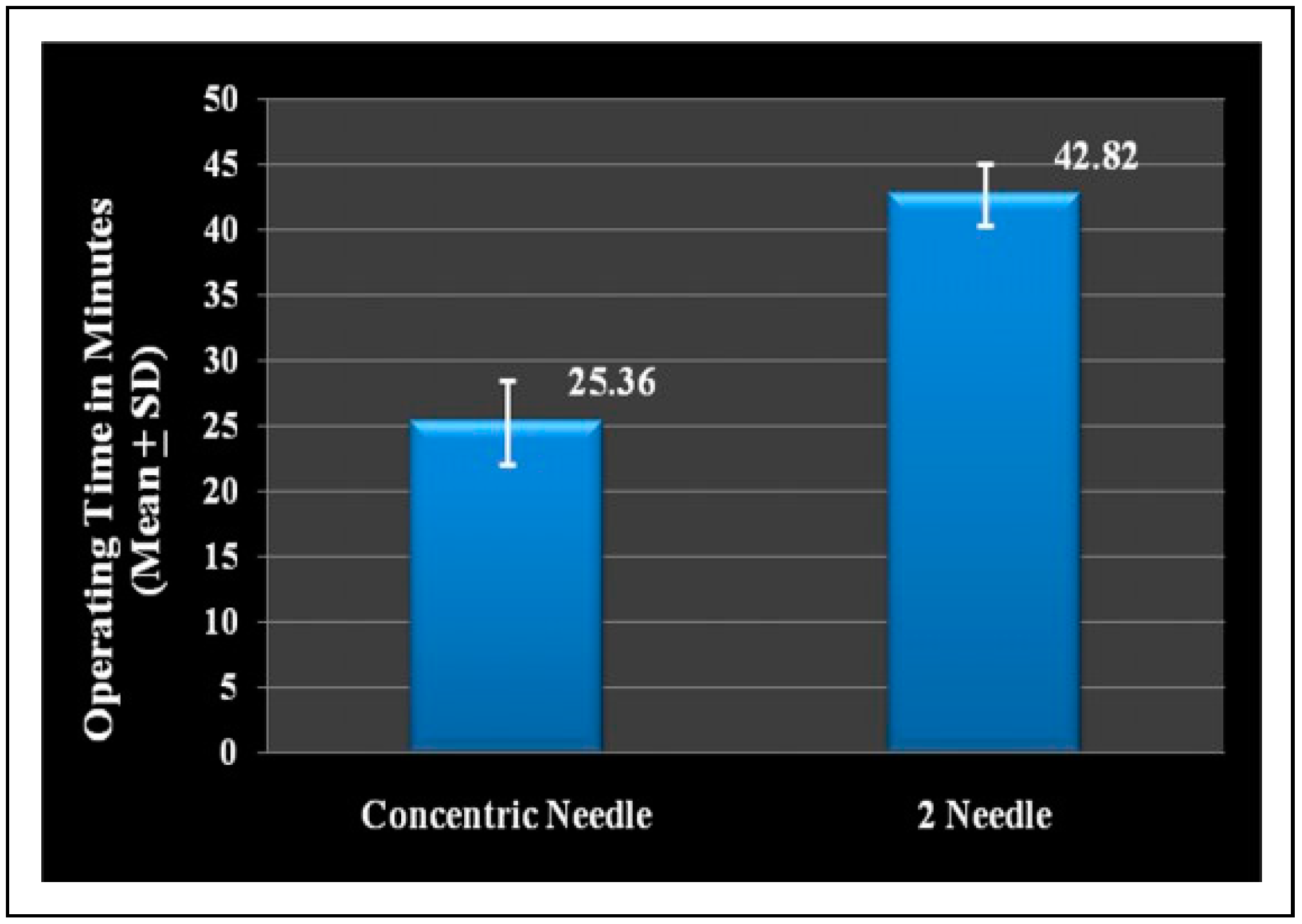
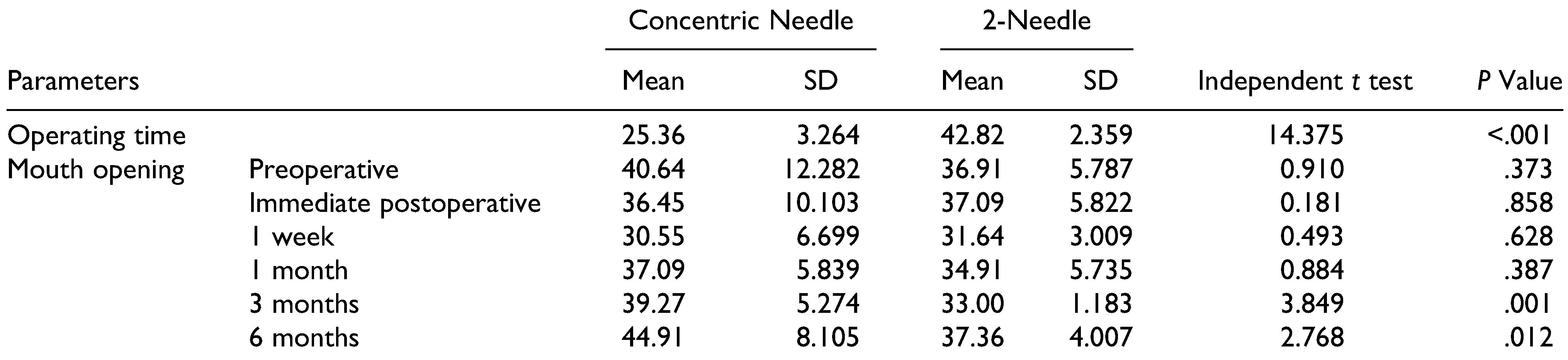
- The operative time was measured in minutes using a simple stopwatch.
- Limitation of jaw functions was measured by Likert type scale (using 5-point scale, with 0 being the absence of limitation and 4 being a severe limitation).
- Tolerance of treatment and the effectiveness of treatment were measured by Likert-type scale (0 being the lowest and 4 the maximum values).
- The lateral deviation was measured in millimeter, as described by Guarda-Nardini et al.
Results
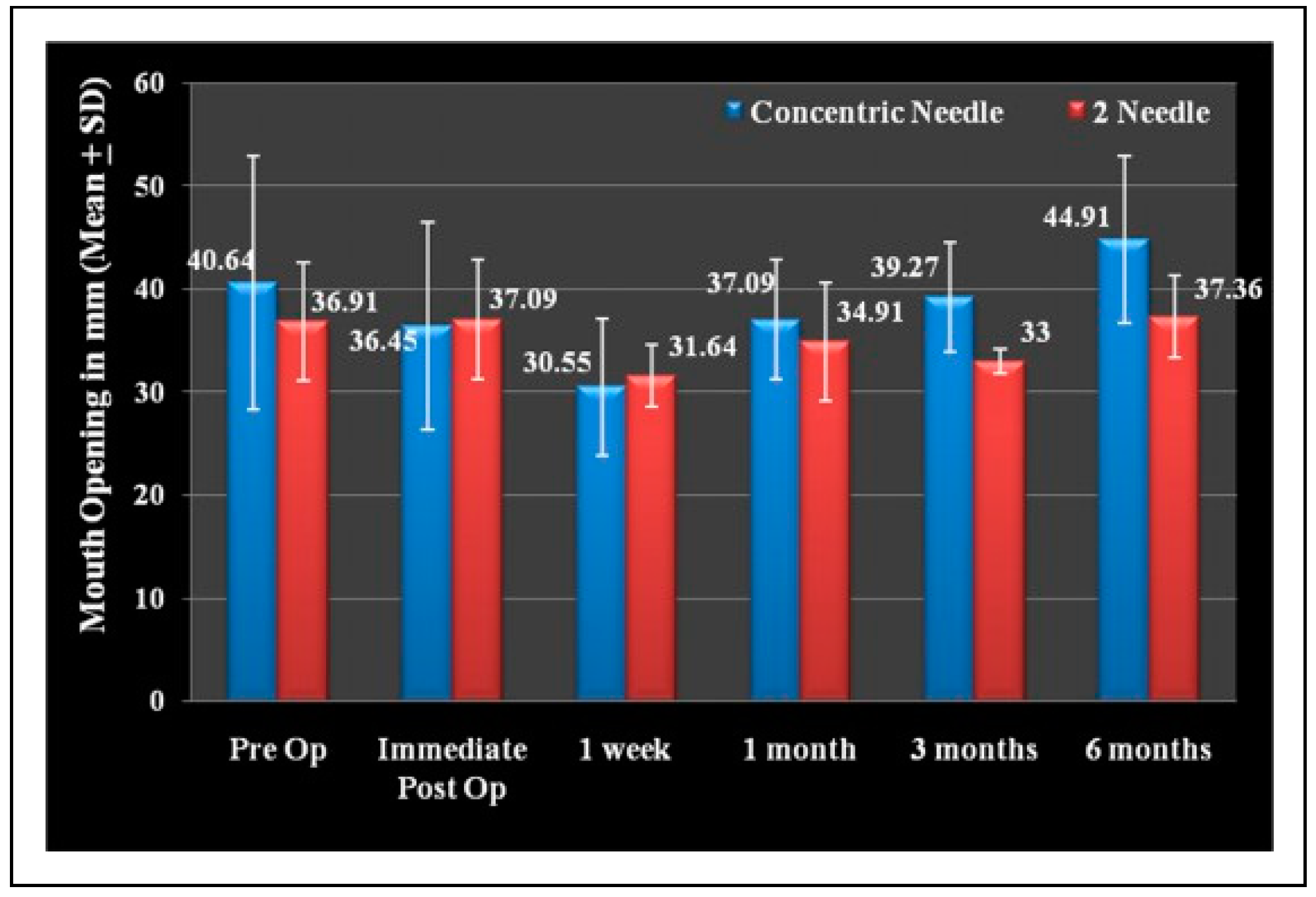
Mouth Opening
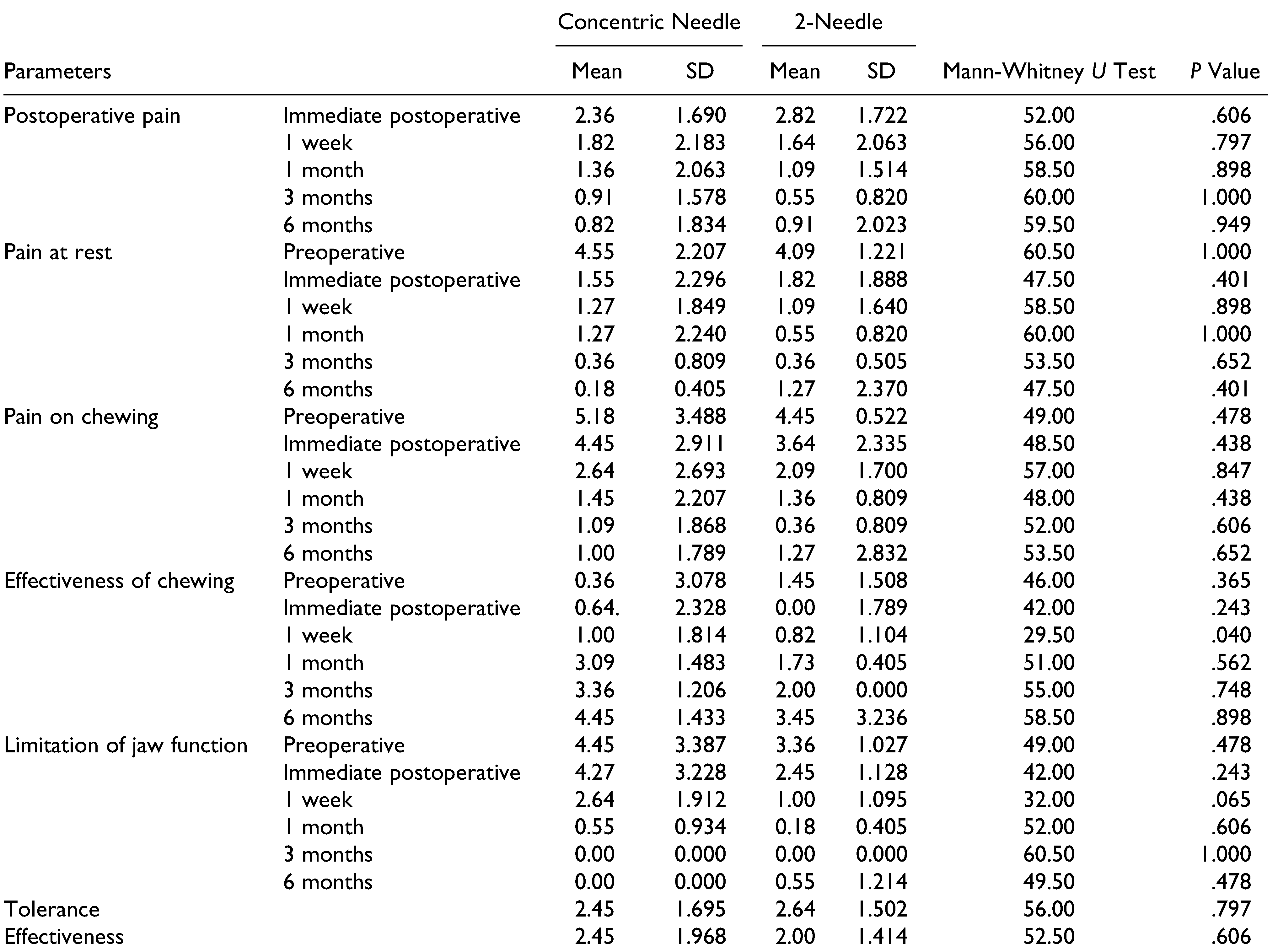
Postoperative Pain
Pain at Rest
Pain on Chewing
Effectiveness of Chewing
Limitation of Jaw Function
Discussion
Conclusion
Funding
Conflicts of Interest
References
- Manemi, R.; Kenchangoudar, R.; Revington, P. Ankylosing spondylitis of temporomandibular joint (TMJ). In Clinical and Molecular Advances in Ankylosing Spondylitis; Bruges-Armas, J., Ed.; In Tech: Barcelona, Spain, 2012. [Google Scholar]
- Nitzan, D.W.; Dolwick, M.F.; Heft, M.W. Arthroscopic lavage and lysis of the temporomandibular joint: A change in perspective. J Oral Maxillofac Surg. 1990, 48, 798–801. [Google Scholar] [CrossRef] [PubMed]
- Nitzan, D.W.; Dolwick, M.F.; Martinez, G.A. Temporomandibular joint arthrocentesis: A simplified treatment for severe limited mouth opening. J Oral Maxillofac Surg. 1991, 49, 1163–1167. [Google Scholar] [PubMed]
- Dimitroulis, G.; Dolwick, M.F.; Martinez, A. Temporomandibular joint arthrocentesis and lavage for the treatment of closed lock: A follow-up study. Br J Oral Maxillofac Surg. 1995, 33, 23–26. [Google Scholar] [PubMed]
- Rehman, K.U.; Hall, T. Single needle arthrocentesis. Br Journal Oral Maxillofac Surg. 2009, 47, 403–404. [Google Scholar]
- Guarda-Nardini, L.; Ferronato, G.; Manfredini, D. Two-needle vs. single-needle technique for TMJ arthrocentesis plus hyaluronic acid injections: A comparative trial over a six-month follow up. Int J Oral Maxillofac Surg. 2012, 41, 506–513. [Google Scholar] [CrossRef] [PubMed]
- Bayoumi, A.M.; Al-Sebaei, M.O.; Mohamed, K.M.; et al. Arthrocentesis followed by intra-articular autologous blood injection for the treatment of recurrent temporomandibular joint dislocation. Int J Oral Maxillofac Surg. 2014, 40, 1224–1228. [Google Scholar]
- Vaira, L.A.; Raho, M.T.; Soma, D.; et al. Complications and post-operative sequelae of temporomandibular joint arthrocentesis. CRANIO. 2017, 2017, 1–4. [Google Scholar]
- Şentürk, M.F.; Yıldırım, D.; Bilgir, E.L.İ.F.; Fındık, Y.; Baykul, T. Long-term evaluation of single-puncture temporomandibular joint arthrocentesis in patients with unilateral temporomandibular disorders. Int J Oral Maxillofac Surg. 2018, 47, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Attia, H.S.; Mosleh, M.I.; Jan, A.M.; Shawky, M.M.; Jadu, F.M. Age, gender and parafunctional habits as prognostic factors for temporomandibular joint arthrocentesis. CRANIO. 2018, 36, 121–127. [Google Scholar] [PubMed]
- Manfredini, D.; Rancitelli, D.; Ferronato, G.; Guarda-Nardini, L. Arthrocentesis with or without additional drugs in temporomandibular joint inflammatory-degenerative disease: Comparison of six treatment protocols. J Oral Rehabil. 2012, 39, 245–251. [Google Scholar] [PubMed]
- Marty, P.; Louvrier, A.; Weber, E.; Dubreuil, P.A.; Chatelain, B.; Meyer, C. Arthrocentesis of the temporomandibular joint and intra-articular injections: An update. J Stomatol Maxillofac Surg Oral Surg 2016, 117, 266–272. [Google Scholar]
- Senturk, M.F.; Yazıcı, T.; Fındık, Y.; Baykul, T. Intraoperative comparison of single- and double-puncture techniques in temporomandibular joint arthrocentesis. Int J Oral Maxillofac Surg. 2018, 47, 1060–1064. [Google Scholar] [CrossRef] [PubMed]
- Nagori, S.A.; Roy Chowdhury, S.K.; Thukral, H.; Jose, A.; Roychoudhury, A. Single puncture versus standard double needle arthrocentesis for the management of temporomandibular joint disorders: A systematic review. J Oral Rehabil. 2018, 45, 810–818. [Google Scholar] [PubMed]
- Oreroglu, A.R.; Özkaya, Ö.; Öztürk, M.B.; Bingöl, D.; Akan, M. Concentric-needle cannula method for single-puncture arthrocentesis in temporomandibular joint disease: An inexpensive and feasible technique. J Oral Maxillofac Surg. 2011, 69, 2334–2338. [Google Scholar] [CrossRef] [PubMed]
- Gouveia, M.V.; Barbalho, J.C.; Pereira Junior, E.D.; Nascimento, M.M.; Vasconcelos, B.C. Effectiveness and satisfaction evaluation of patients submitted to TMJ arthrocentesis: A case series. Braz Oral Res. 2015, 29, 1–5. [Google Scholar]
- Skármeta, N.P.; Pesce, M.C.; Espinoza-Mellado, P.A. A single-puncture arthrocentesis technique, using a peripheral intravenous catheter. Int J Oral Maxillofac Surg. 2016, 45, 1123–1125. [Google Scholar] [PubMed]
- Alkan, A.; Kilic, E. A new approach to arthrocentesis of the temporomandibular joint Int. J Oral Maxillofac Surg. 2009, 38, 85–86. [Google Scholar]
- Dolwick, M.F. The role of temporomandibular joint surgery in the treatment of patients with internal derangement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997, 83, 150–155. [Google Scholar] [PubMed]
 |
 |
 |
© 2020 by the author. The Author(s) 2020.
Share and Cite
Kumar, A.; Gupta, A.; Ghosh, R.; Pandey, R.; Kumar, S. A Comparative Study Between Concentric Single-Needle Puncture Technique and Conventional 2-Needle Technique for Temporomandibular Joint Arthrocentesis Plus Corticosteroid Injections. Craniomaxillofac. Trauma Reconstr. 2020, 13, 99-104. https://doi.org/10.1177/1943387520911826
Kumar A, Gupta A, Ghosh R, Pandey R, Kumar S. A Comparative Study Between Concentric Single-Needle Puncture Technique and Conventional 2-Needle Technique for Temporomandibular Joint Arthrocentesis Plus Corticosteroid Injections. Craniomaxillofacial Trauma & Reconstruction. 2020; 13(2):99-104. https://doi.org/10.1177/1943387520911826
Chicago/Turabian StyleKumar, Amit, Amit Gupta, Rajarshi Ghosh, Rajeev Pandey, and Sanjeev Kumar. 2020. "A Comparative Study Between Concentric Single-Needle Puncture Technique and Conventional 2-Needle Technique for Temporomandibular Joint Arthrocentesis Plus Corticosteroid Injections" Craniomaxillofacial Trauma & Reconstruction 13, no. 2: 99-104. https://doi.org/10.1177/1943387520911826
APA StyleKumar, A., Gupta, A., Ghosh, R., Pandey, R., & Kumar, S. (2020). A Comparative Study Between Concentric Single-Needle Puncture Technique and Conventional 2-Needle Technique for Temporomandibular Joint Arthrocentesis Plus Corticosteroid Injections. Craniomaxillofacial Trauma & Reconstruction, 13(2), 99-104. https://doi.org/10.1177/1943387520911826



