Abstract
Purpose: The maxillary advancement using Le Fort I osteotomy directly affects in the positioning of the upper lip (UL) and the nasolabial angle (NLA), which plays an important role in facial expression and aesthetics, because of this, the aim of this study was to evaluate the ability of Dolphin Imaging 11.8 software in predicting changes to the UL position and NLA in patients undergoing maxillary advancement. Materials and Methods: It was a retrospective cohortstudy. Predictive and final tracings using pre- and postoperative Cone beam computed tomography (CBCT) of 24 patients undergoing maxillary advancement, regardless of mandibular movement, were compared. Whether the amount of advancement changes this predictability was also analyzed. The predictive and the 12-month postoperative data were evaluated using Dolphin Imaging 11.8 software and compared. Student t test was used to get the results. Results: The vertical analysis of the incisal tip and cementoenamel junction of the upper central incisor (UCI) and of the UL were statistically significant (p = 0.001 for all). The horizontal measurements of the same variables (p = 0.238, p = 0.516, p = 0.930, respectively) and the NLA (p = 0.060) showed no statistical significance. The amount of advancement did not interfere with the variables analyzed, except for the exposure (p = 0.009) and inclination of the UCI (p = 0.010). Conclusion: It was concluded that the amount of maxillary advancement does not interfere with the UL prediction; the prediction capacity of the software was good for the horizontal measurements, but had a significant error index for vertical measurements.
Introduction
The main factors that lead a patient to resort to orthognathic surgery are facial esthetics and malocclusion. This procedure aims to correct the dentofacial deformities with movement of the bone base. Due to this movement, soft tissue changes will also occur, and it is one of the factors of greatest concern to patients [1].
Maxillary advancement with Le Fort type-I osteotomy directly interferes with the positioning of the upper lip (UL) and the nasolabial angle (NLA), which play an important role in facial expression and esthetics [2,3,4].
Due to edema, the UL repositioning result can only be evaluated from the sixth postoperative month. Final soft tissue stability will only occur after orthodontic treatment completion, with final repositioning of the upper incisors [5].
In addition to the vertical and horizontal repositioning of the maxilla, other factors may influence UL position, such as soft tissue deformities, nasal deformities, facial trauma, and previous facial surgeries with increase or decrease in thickness, length, and tone of the soft tissues of the face [6].
The development of virtual and 3-D planning software provides surgeons with greater security in surgical planning and works as a tool for clarifying to the patient the procedure that will be performed [7,8].
In this way, it is possible to digitize the data. Even so, most of the studies are still restricted to the comparison of pre- and postoperative images and, hence are considered imprecise [9].
Many studies discussing the efficacy and predictability of software report difficulty in predicting results due to several types of osteotomy and the variability of the methods used to evaluate the results [10,11].
The objective of this study was to verify whether Dolphin Imaging 11.8 3-D Surgery software (Dolphin Imaging & Management Solutions, Patterson Technology, Chatsworth, California) can predict changes in UL positioning in patients undergoing maxillary advancement and whether the amount of advancement changes this predictability. The hypothesis is that it’s accurate, but it’s necessary to know the level of accuracy. So, the specific aims of the study were whether (1) it is good at prediction capacity of the positioning of the UL after maxilla advancement and (2) the amount of the advancement interferes with the predictability.
Materials and Methods
It was a retrospective cohort study in which preoperative and postoperative CBCT scans of patients undergoing orthognathic surgery were evaluated. These were analyzed by a previously calibrated single evaluator.
Approval of the project by the Research Ethics Committee of the Faculty of Dentistry of Bauru, University of São Paulo, Bauru, São Paulo, Brazil, under Protocol CAAE 66261717.2.0000.5417, was received prior to the beginning of the study.
To perform this study, 24 patients were selected from a bank of 500 CBCT obtained from I-Cat Cone Beam (Imaging Science, Hatfield, Pennsylvania) with field of view of 23 × 17 cm, 120 kVp, 36.90 mA, acquisition time of 40 s, and voxel of 0.40 mm. Based on preoperative and postoperative examinations and inclusion criteria, all operations were performed by a single oral maxillofacial surgeon.
Patients aged 17 to 65 years, both genders, with maxillary deficiency treated with Le Fort type-I osteotomy alone or associated with sagittal mandible osteotomy[12] were included in the study. These patients had initial and postoperative CBCT obtained at least 1 year after surgery, with orthodontic treatment completed, and did not undergo intervention in the UL for correction of thickness or in the width of the alar base. Patients who underwent surgical procedures in the nasal region and those who presented lip-palatine fissures were excluded from the study.
The CBCT scans of each patient were imported into the Dolphin Imaging 3-D Surgery software, and sagittal reformations were obtained. With the “digitize” tool, markings were made of the cephalometric points required for the analysis described by Arnett et al. [13].
The tracings were performed by the software in the reformations by lateral view, like a teleradiograph, obtained from the CBCT scan. Analysis described by Arnett et al.[13] was used as reference. This CBCT scan was performed according to the team protocol: without the use of a chinstrap, relaxed lips, and natural head position.
The points and measurements used were incisal tip of the upper central incisor (UCI)—U1 tip; cementoenamel junction of the UCI (CEJ)—U1 labial gingival border; the anterior-most point of the UL curvature; NLA; effective UL length—UL length; upper incisor exposure; upper incisor inclination. Two standardized lines, perpendicular to each other, were used to perform the measurements and used as reference for linear measurements.
After marking the points, the “superimpose” tool was used to overlap the predictive traced images, created in the “treatment simulation”, with the 1-year postoperative images. This overlap was performed using the sella and soft glabella points as reference.
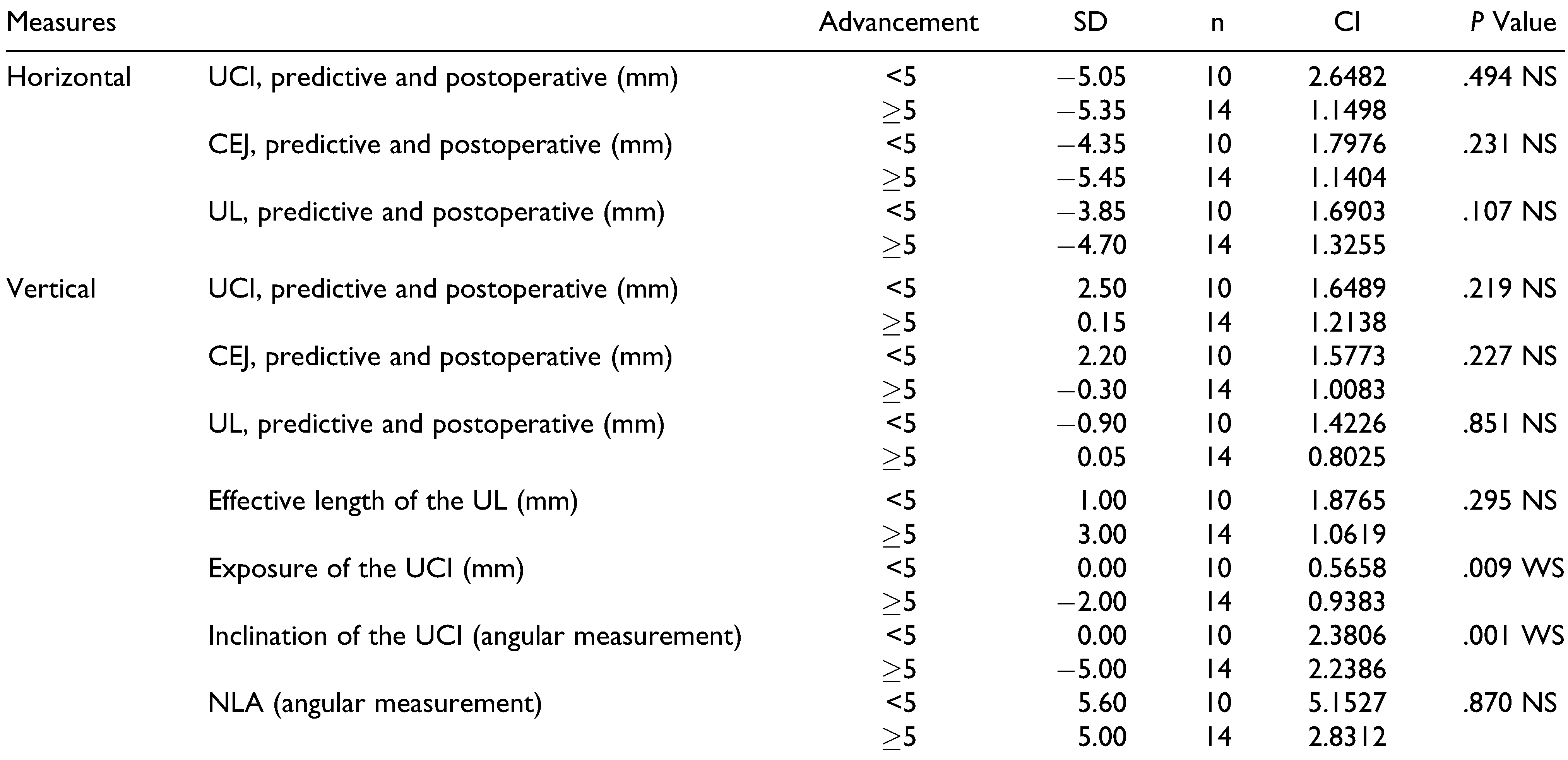
The image was concealed after the overlap, keeping only the outline. From this, the “annotations and/or measurements” tool was calibrated based on the true vertical line, tracing reference lines perpendicular to each other and measuring the distances of the previously mentioned points to the x and y lines (Figure 1, Figure 2, Figure 3 and Figure 4).
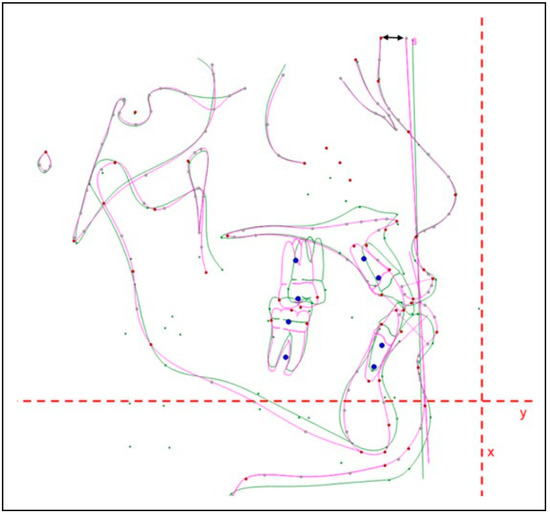
Figure 1.
Calibration based on true vertical line and “x” and “y” reference lines.
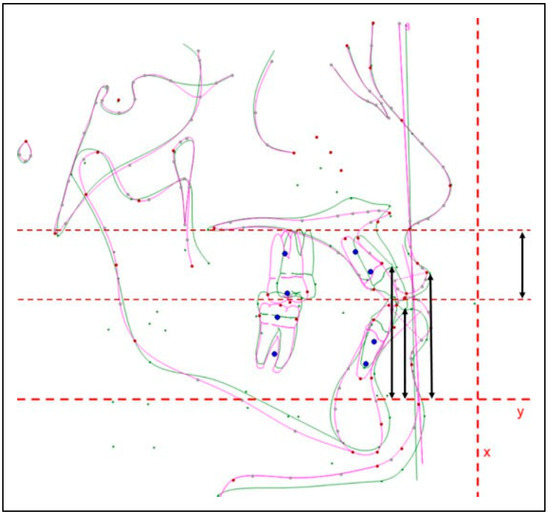
Figure 2.
Vertical distances up to the “y” line and effective length of the UL. UL indicates upper lip.
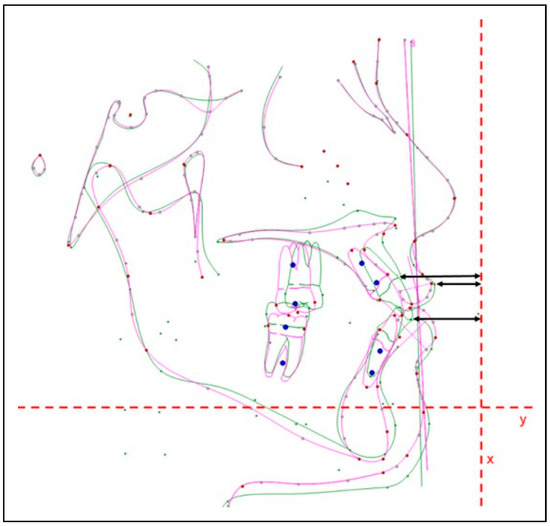
Figure 3.
Horizontal distances up to the “x” line.
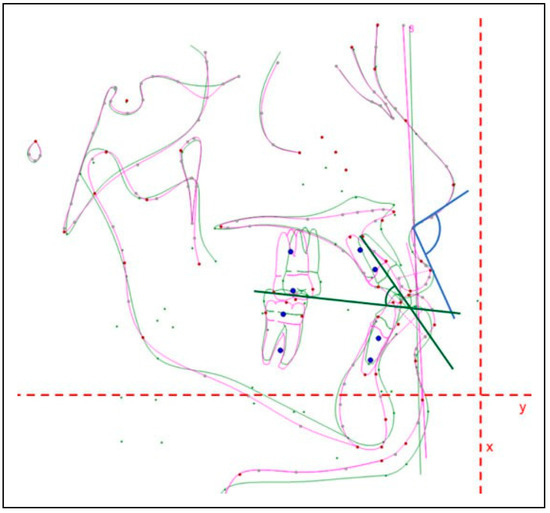
Figure 4.
NLA and inclination of the UCI. NLA indicates nasolabial angle; UCI, upper central incisor.
The measurements were performed with the purpose of evaluating whether (1) the UL advancement is proportional to the UCI; (2) the prediction of the NLA, effective UL length, and upper incisor exposure is compatible with the normality pattern; and (3) the amount of the advancement interferes with the predictability.
After all measurements were performed, results were separated into groups based on advancement of < or ≥5 mm, allowing no induction of outcome. These values were used because they are related to greater stability of the obtained results [14,15,16].
Systematic and random errors for each measure were independently assessed. The paired t test was used to calculate the systematic error. To estimate the casual error, Dahlberg’s formula[17] was applied. All tests were performed with the SPSS V20 program (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0, Armonk, NY: IBM Corp.) and Minitab 16 (Minitab 16 Statistical Software 2010. Computer software, State College, PA: Minitab, Inc.), adopting a significance level of 5%. Of interest were results showing no statistically significant difference between the predictive and the postoperative tracings.
Results
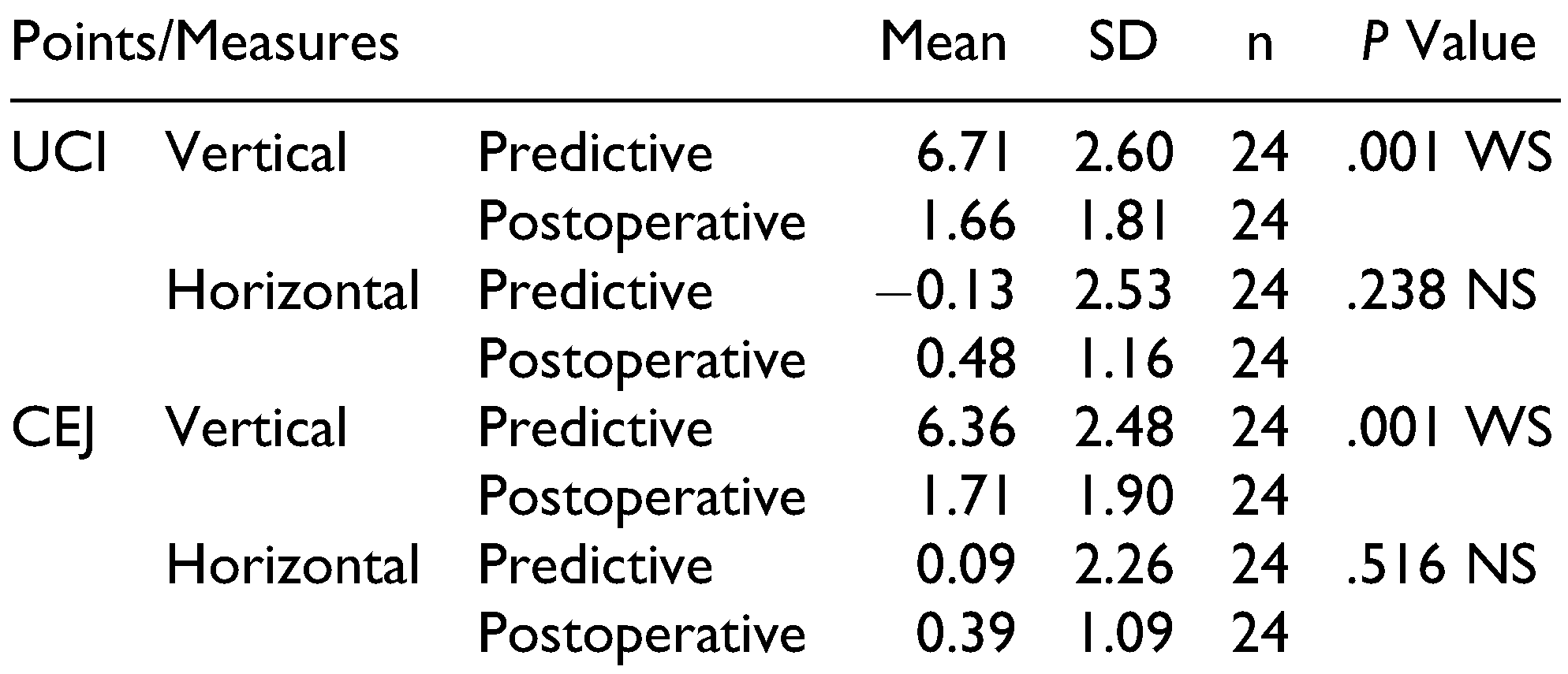
Initially, the vertical and horizontal distances of the two points were evaluated, from the UCI to the reference lines (Table 1). Based on this, it was possible to verify whether the planned position for the incisors was the one observed, a year after orthognathic surgery. This comparison was done using the Student paired t test.

Table 1.
Distance Between the UCI and CEJ of the UCI to the Reference Line “x” and “y,” in the Predictive and Postoperative Tracings.
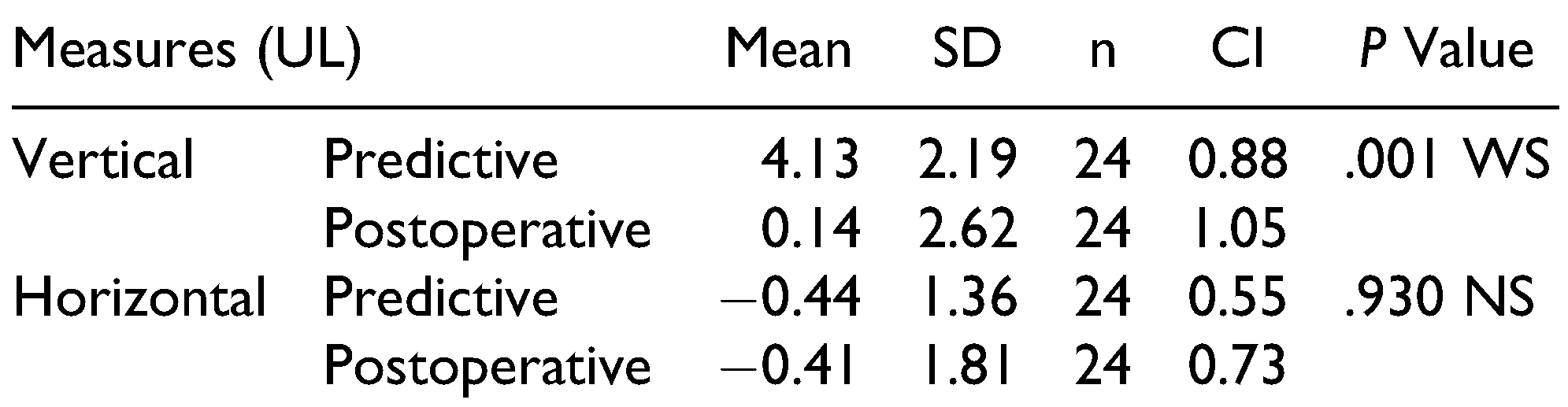
The measurements of the UL position in the predictive and postoperative tracings and the comparisons were performed using the Student paired t test (Table 2).

Table 2.
Distance Between the UL to the Reference Line “x” and “y,” in the Predictive and Postoperative Tracings.
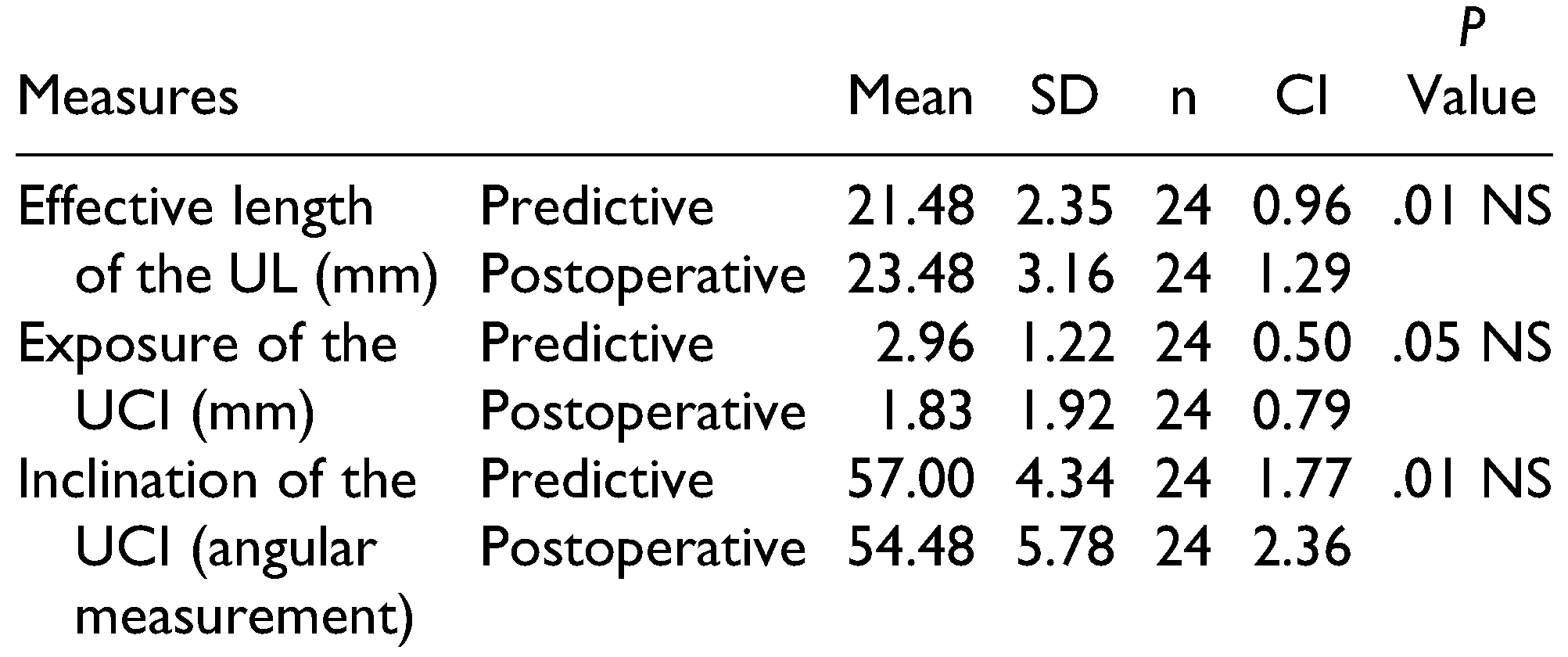
The Student paired t test (Table 3) was used to compare the effective UL length, incisor exposure, and upper incisor inclination provided by the software and that obtained in the postoperative period.

Table 3.
Effective Length of the UL, Exposure and Inclination of the UCI.
To evaluate the NLA, the Student paired t test was used and did not present statistical difference (p = 0.06).
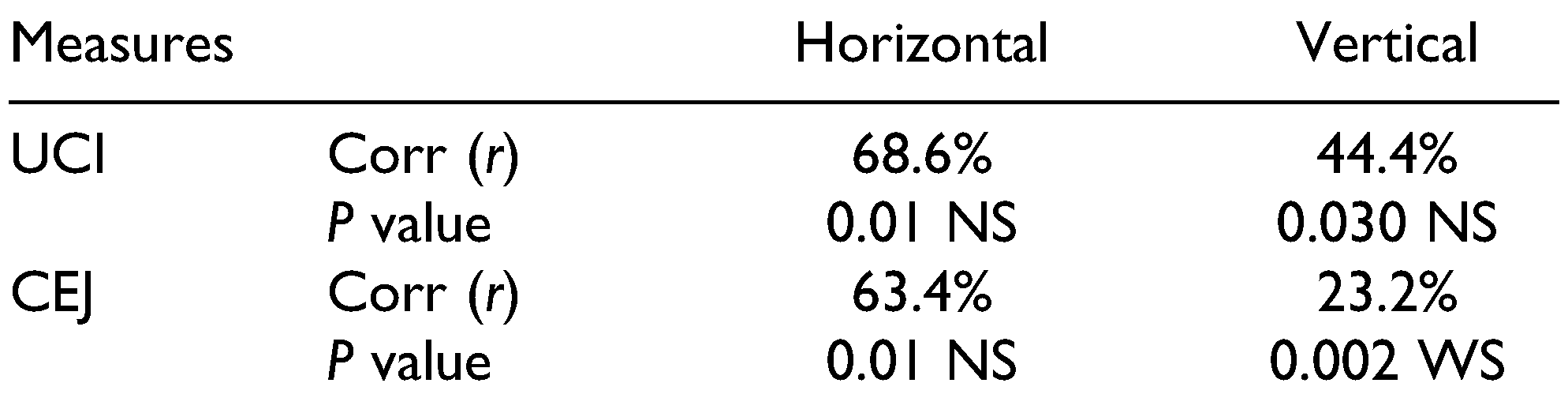
To evaluate the influence of the positioning of the upper incisor on the positioning of the UL, the Pearson correlation test (Table 4) was applied.

Table 4.
Correlation of the UL Position with the UCI.
To evaluate whether the amount of advancement would interfere with predictability, the ANOVA test was used.
Table 5 presents all the variables mentioned above, separating them based on advancement of less than 5 mm or greater/equal to 5 mm.

Table 5.
Interference of the Amount of Advancement with the Prediction.
Discussion
Considering that the objective of this study was to verify whether Dolphin Imaging 11.8 3-D Surgery software could predict changes in UL positioning in patients undergoing maxillary advancement of both genders and whether the amount of advancement changes this predictability, the results were satisfying.
The CT scans used were those of patients who had undergone maxillary or maxillary–mandibular advancement, performed by the same surgeon, using the same type of osteotomy and fixation of the bone bases with titanium miniplates, obtaining a standardization of the cases.
Using the results obtained, with the support of the literature, it was possible to perform a critical analysis of Dolphin Imaging 11.8 3-D Surgery software.
In the evaluation of the UCI, in the incisal tip and CEJ, no statistical difference was observed in the horizontal movements, between the predictive and postoperative tracings, indicating that the software has good predictability. The software was not an effective prediction of the vertical movement, as there was a statistically significant difference between the points.
These results differ from those of Sun et al.[18] and Zhang et al.,[19] as the guides used by them were prototyped and had vertical and horizontal movement limiters, different from those used in this study that limit only the most commonly used horizontal (anteroposterior) movements. Often, the vertical movement is modified by face analysis in the trans-operative, which may alter planning [18,19].
In the analysis of the inclination of the UCI, there was no statistical significance, and therefore, the incisors practically did not undergo predicted changes until orthodontic finalization, showing that the labial support by the inclination of the incisor was maintained. The ideal values for this inclination are between 54.3° and 59.3°.[20] In the present study, the mean ranged from 54.48° (predictive angulation) to 57° (postoperative), thus being within normal range.
Regarding the exposure of the UCI, there was no statistically significant difference, that is, what was predicted was achieved postoperatively. This was due to the correct positioning of the incisors in the bone base and shows the importance of previous orthodontic preparation, since the inclination of the incisor influences the exposure and transoperative evaluation.
To understand this question, a clinical view is needed. In the trans-operative period, after conducting maxillary movement, bone interferences can be found that need to be removed before fixation. These interferences do not exist in the software, even in 3-D manipulation, since it usually occurs in the inner part of the jaw, which explains the imprecise vertical values. When the interference is removed, jaw fixation position starts to be guided vertically by the incisor exposure and no longer by the positioning previously planned [19].
The analyzed point of the UL was the most anterior one and no significant difference was observed between the predictive and postoperative tracings. This can be considered a good result of the software with respect to the horizontal prediction, different from the vertical measurements conducted, which presented statistical difference, and so were not accurate.
Studies such as those by Chew[21] and Muradin et al.[22] already present the imprecision of vertical measurements, in comparison with horizontal ones, mainly in relation to the nasal, subnasal, and UL points.
A meta-analysis performed in 2014 by Khamashta-Ledezma and Naini[23] started with 979 articles. According to the inclusion criteria, only 15 fit the study. Of the 15, only 3 evaluated vertical measurements, still highlighting the difficulty and the variability of the results [21,22,23].
The measurement of effective UL length when comparing the predictive and postoperative tracings using the Student paired t test did not result in statistical significance, so the software predictability was considered good.
The favorable result obtained in this study in relation to this variable is mainly due to the care in observing whether the UL is relaxed during the acquisition of the images. If the lips are contracted, they can interfere directly in this measurement. This fact was also highlighted in the previously mentioned meta-analysis as one of the factors that hinder vertical measurements [23].
Regarding the NLA, it was observed that the difference between the predictive and the postoperative trajectory was not statistically significant. Hence the software was considered accurate for this variable. This result is due, for the most part, to the correct positioning of the incisors in the orthodontic preparation. In cases where surgery is performed before orthodontic preparation, there is no good predictability of occlusion or facial esthetics.[24] On this subject, articles such as that of Uribe et al.[7] report that patients submitted to the “surgery first” procedure have a harmonic face, but without measuring the stability of occlusion and soft tissues.
When analyzing whether there was a relationship between the movement of the UCI and the UL positioning, it was observed that the software correctly predicted the UL positioning even when there was variation of the horizontal position of the incisal tip and CEJ of the upper incisors. Conversely, in the vertical positioning changes of the UCI, the presented result, despite not presenting statistical significance, was considered regular or less precise.
To verify the software accuracy in predicting the positioning of the analyzed variables in patients who had advancement < or ≥5 mm, the results were separated according to the amount of advancement according to the preoperative and predictive traces. This was done after performing all the measurements, so that there was no induction of results. This separation in advancements < or ≥5 mm was established based on the studies of Araujo et al.,[14] Louis et al.,[15] and Costa et al.[16] who considered 5 mm as the main parameter of surgical stability [14,15,16].
In this comparison, there was statistical significance only in relation to the exposure and inclination of the UCI. These variables, although highly clinically relevant, can be evaluated in the trans-operative and in the preoperative evaluation, avoiding complications in the surgical planning.
Conclusion
It is concluded that the software Dolphin Imaging 11.8 3-D Surgery presented good predictive capacity for the horizontal measurements, but there is still a significant error index for the vertical measurements. The amount of the advancement does not interfere with the predictability of the results, except for the inclination and exposure of the UCI. Clinically, the advancement can be safely done by surgeons. Vertical movements still need the help of external reference.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Shafi, M.I.; Ayoub, A.; Ju, X.; Khambay, B. The accuracy of three-dimensional prediction planning for the surgical correction of facial deformities using Maxilim. Int J Oral Maxillofac Surg. 2013, 42, 801–806. [Google Scholar]
- Rosen, H.M. Lip-nasal aesthetics following Le Fort I osteotomy. Plast Reconstr Surg. 1988, 81, 171–182. [Google Scholar] [PubMed]
- McFarlane, R.B.; Frydman, W.L.; McCabe, S.B.; Mamandras, A.M. Identification of nasal morphologic features that indicate susceptibility to nasal tip deflection with the Le Fort I osteotomy. Am J Orthod Dentofacial Orthop. 1995, 107, 259–267. [Google Scholar] [PubMed]
- Bailey, L.J.; Collie, F.M.; White, R.P., Jr. Long-term soft tissue changes after orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1996, 11, 7–18. [Google Scholar]
- Stella, J.P.; Streater, M.R.; Epker, B.N.; Sinn, D.P. Predictability of upper lip soft tissue changes with maxillary advancement. J Oral Maxillofac Surg. 1989, 47, 697–703. [Google Scholar] [PubMed]
- Mitchell, C.; Oeltjen, J.; Panthaki, Z.; Thaller, S.R. Nasolabial aesthetics. J Craniofac Surg. 2007, 18, 756–765. [Google Scholar]
- Uribe, F.; Janakiraman, N.; Shafer, D.; Nanda, R. Three-dimensional cone-beam computed tomography-based virtual treatment planning and fabrication of a surgical splint for asymmetric patients: Surgery first approach. Am J Orthod Dentofacial Orthop. 2013, 144, 748–758. [Google Scholar]
- Adolphs, N.; Liu, W.; Keeve, E.; Hoffmeister, B. Rapid splint: Virtual splint generation for orthognathic surgery—Results of a pilot series. Comput Aided Surg. 2014, 19, 20–28. [Google Scholar]
- Olate, S.; Zaror, C.; Mommaerts, M.Y. A systematic review of soft-to-hard tissue ratios in orthognathic surgery. Part IV: 3D analysis—Is there evidence? J Craniomaxillofac Surg. 2017, 45, 1278–1286. [Google Scholar]
- Nkenke, E.; Vairaktaris, E.; Kramer, M.; et al. Three-dimensional analysis of changes of the malar-midfacial region after Le Fort I osteotomy and maxillary advancement. Oral Maxillofac Surg. 2008, 12, 5–12. [Google Scholar]
- Nadjmi, N.; Tehranchi, A.; Azami, N.; Saedi, B.; Mollemans, W. Comparison of soft-tissue profiles in Le Fort I osteotomy patients with Dolphin and Maxilim softwares. Am J Orthod Dentofacial Orthop. 2013, 144, 654–662. [Google Scholar] [CrossRef] [PubMed]
- Sant’Ana, E.; Souza, D.P.E.; Temprano, A.B.; Shinohara, E.H.; Faria, P.E.P. Lingual short split: A bilateral sagittal split osteotomy technique modification. J Craniofac Surg. 2017, 28, 1852–1854. [Google Scholar] [CrossRef]
- Arnett, G.W.; Jelic, J.S.; Kim, J.; et al. Soft tissue cephalometric analysis: Diagnosis and treatment planning of dentofacial deformity. Am J Orthod Dentofacial Orthop. 1999, 116, 239–253. [Google Scholar] [CrossRef] [PubMed]
- Araujo, A.; Schendel, S.A.; Wolford, L.M.; Epker, B.N. Total maxillary advancement with and without bone grafting. J Oral Surg. 1978, 36, 849–858. [Google Scholar] [PubMed]
- Louis, P.J.; Waite, P.D.; Austin, R.B. Long-term skeletal stability after rigid fixation of Le Fort I osteotomies with advancements. Int J Oral Maxillofac Surg. 1993, 22, 82–86. [Google Scholar] [CrossRef]
- Costa, F.; Robiony, M.; Sembronio, S.; Polini, F.; Politi, M. Stability of skeletal Class III malocclusion after combined maxillary and mandibular procedures. Int J Adult Orthodon Orthognath Surg. 2001, 16, 179–192. [Google Scholar]
- Dahlberg, G. Statistical methods for medical and biological students. Br Med J. 1940, 2, 358–359. [Google Scholar]
- Sun, Y.; Luebbers, H.T.; Agbaje, J.O.; et al. Accuracy of upper jaw positioning with intermediate splint fabrication after virtual planning in bimaxillary orthognathic surgery. J Craniofac Surg. 2013, 24, 1871–1876. [Google Scholar] [CrossRef]
- Zhang, N.; Liu, S.; Hu, Z.; Hu, J.; Zhu, S.; Li, Y. Accuracy of virtual surgical planning in two-jaw orthognathic surgery: Comparison of planned and actual results. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016, 122, 143–151. [Google Scholar] [CrossRef]
- Tweed, C.H. A philosophy of orthodontic treatment. Am J Orthod. 1945, 31, 74–103. [Google Scholar] [CrossRef]
- Chew, M.T. Soft and hard tissue changes after bimaxillary surgery in Chinese Class III patients. Angle Orthod. 2005, 75, 959–963. [Google Scholar] [PubMed]
- Muradin, M.S.; Seubring, K.; Stoelinga, P.J.; vd Bilt, A.; Koole, R.; Rosenberg, A.J. A prospective study on the effect of modified alar cinch sutures and V-Y closure versus simple closing sutures on nasolabial changes after Le Fort I intrusion and advancement osteotomies. J Oral Maxillofac Surg. 2011, 69, 870–876. [Google Scholar] [PubMed]
- Khamashta-Ledezma, L.; Naini, F.B. Systematic review of changes in maxillary incisor exposure and upper lip position with Le Fort I type osteotomies with or without cinch sutures and/or VY closures. Int J Oral Maxillofac Surg. 2014, 43, 46–61. [Google Scholar] [PubMed]
- Jeon, J.H. Timing of orthognathic surgery: Paradigm shift by surgery-first approach? J Korean Assoc Oral Maxillofac Surg. 2017, 43, 61–62. [Google Scholar] [CrossRef]
© 2020 by the author. The Author(s) 2020.