Virtual Surgical Planning and Hardware Fabrication Prior to Open Reduction and Internal Fixation of Atrophic Edentulous Mandible Fractures
Abstract
:Case Presentation
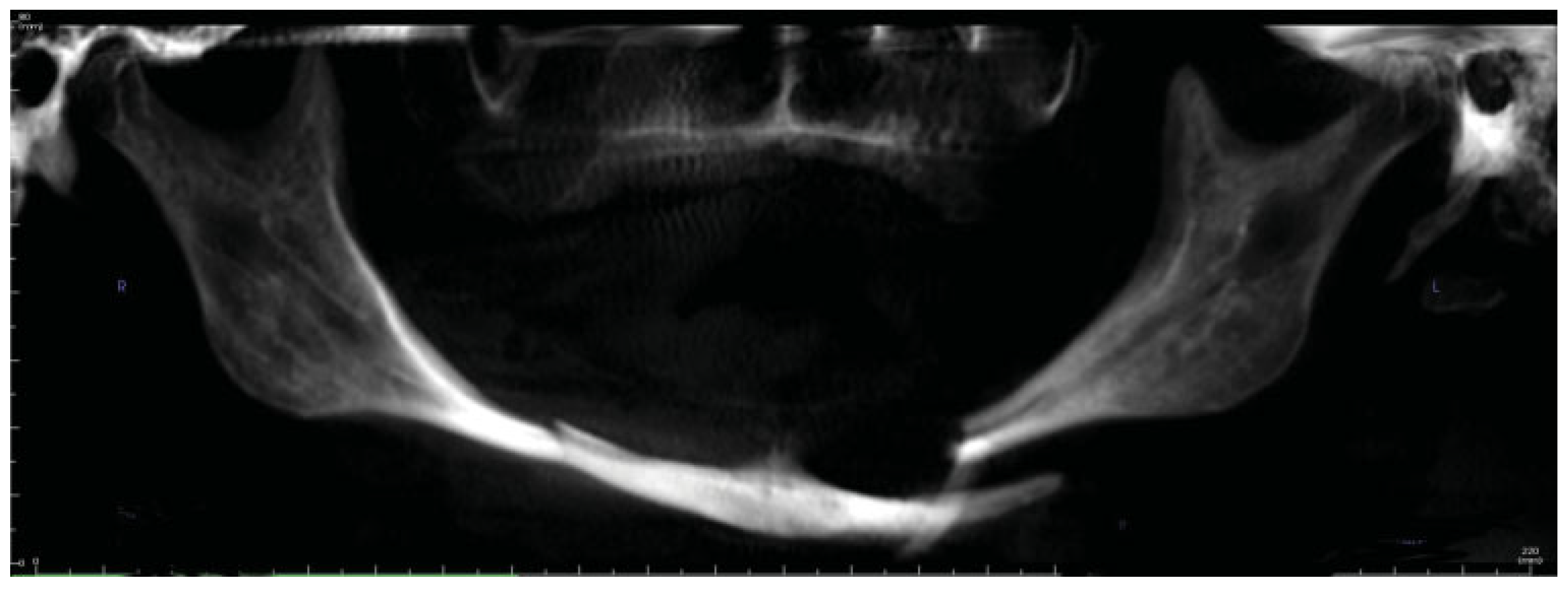
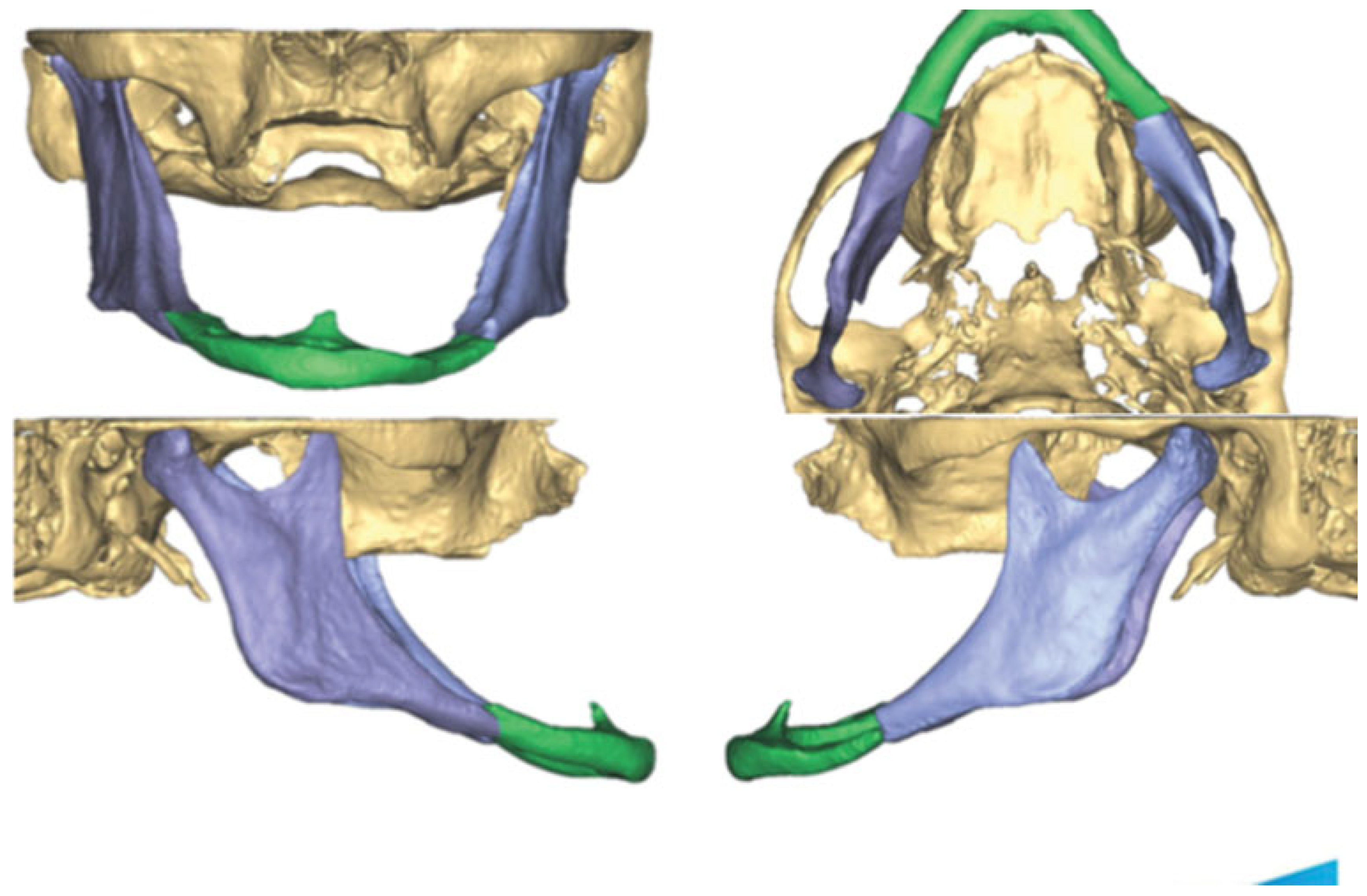
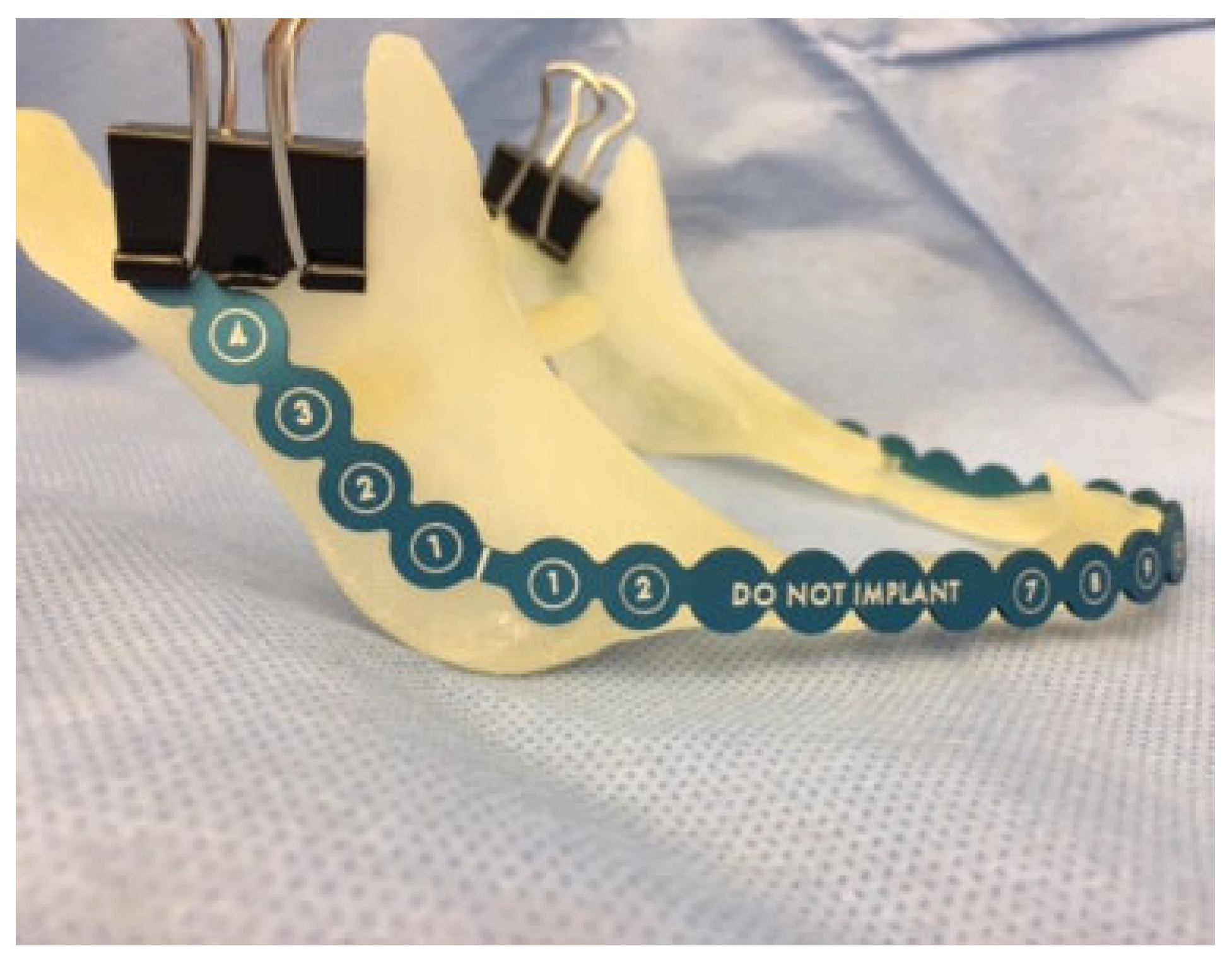
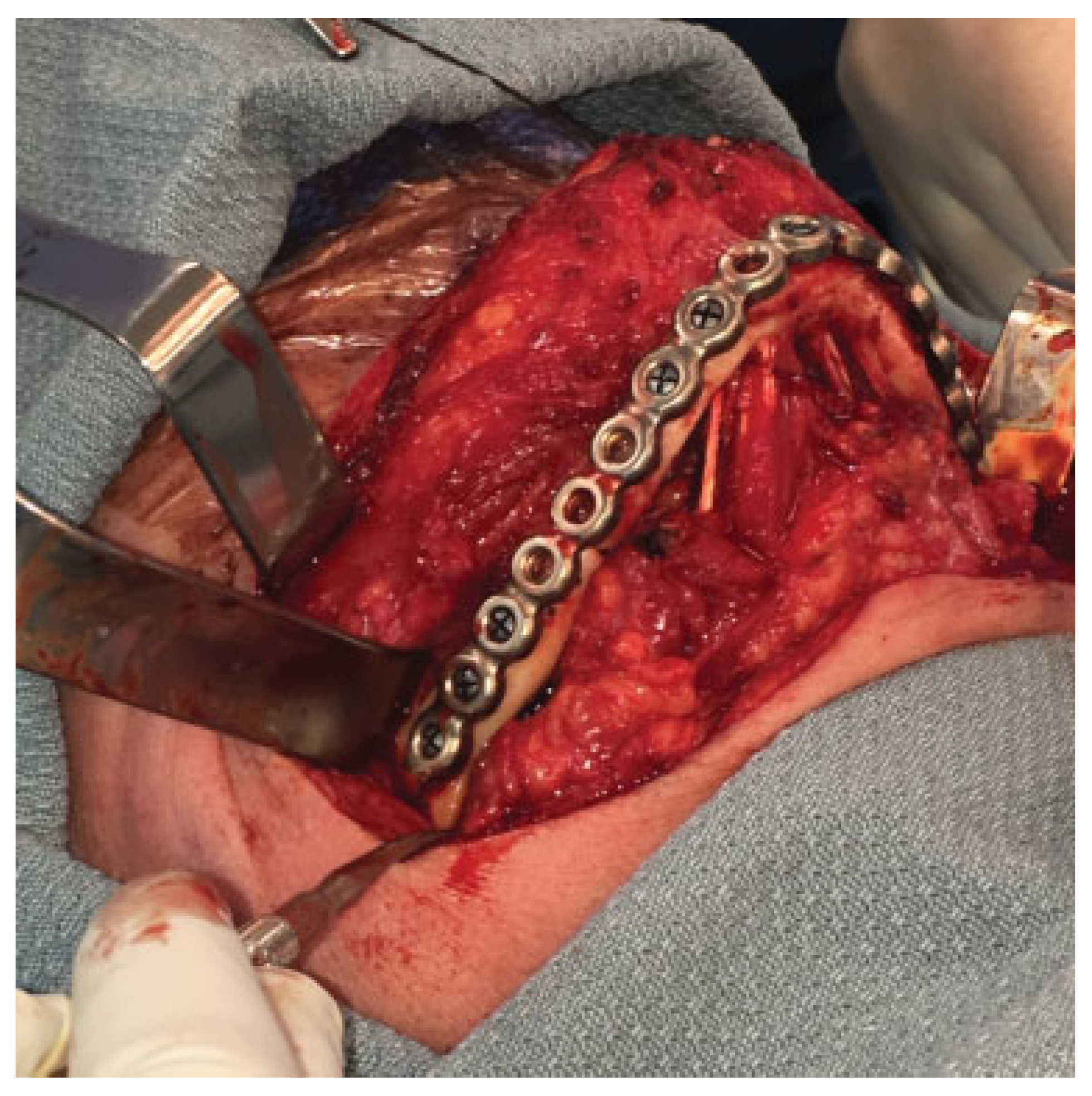
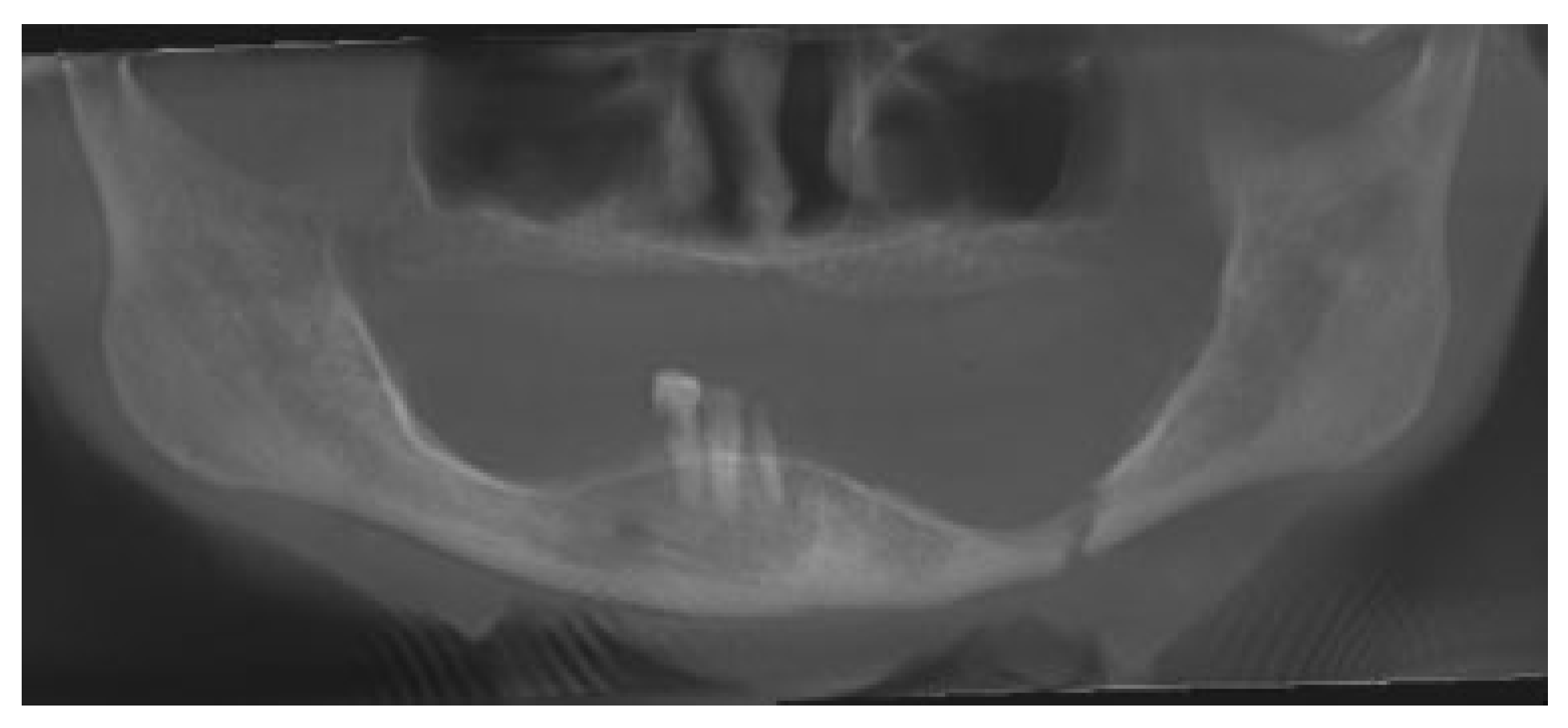
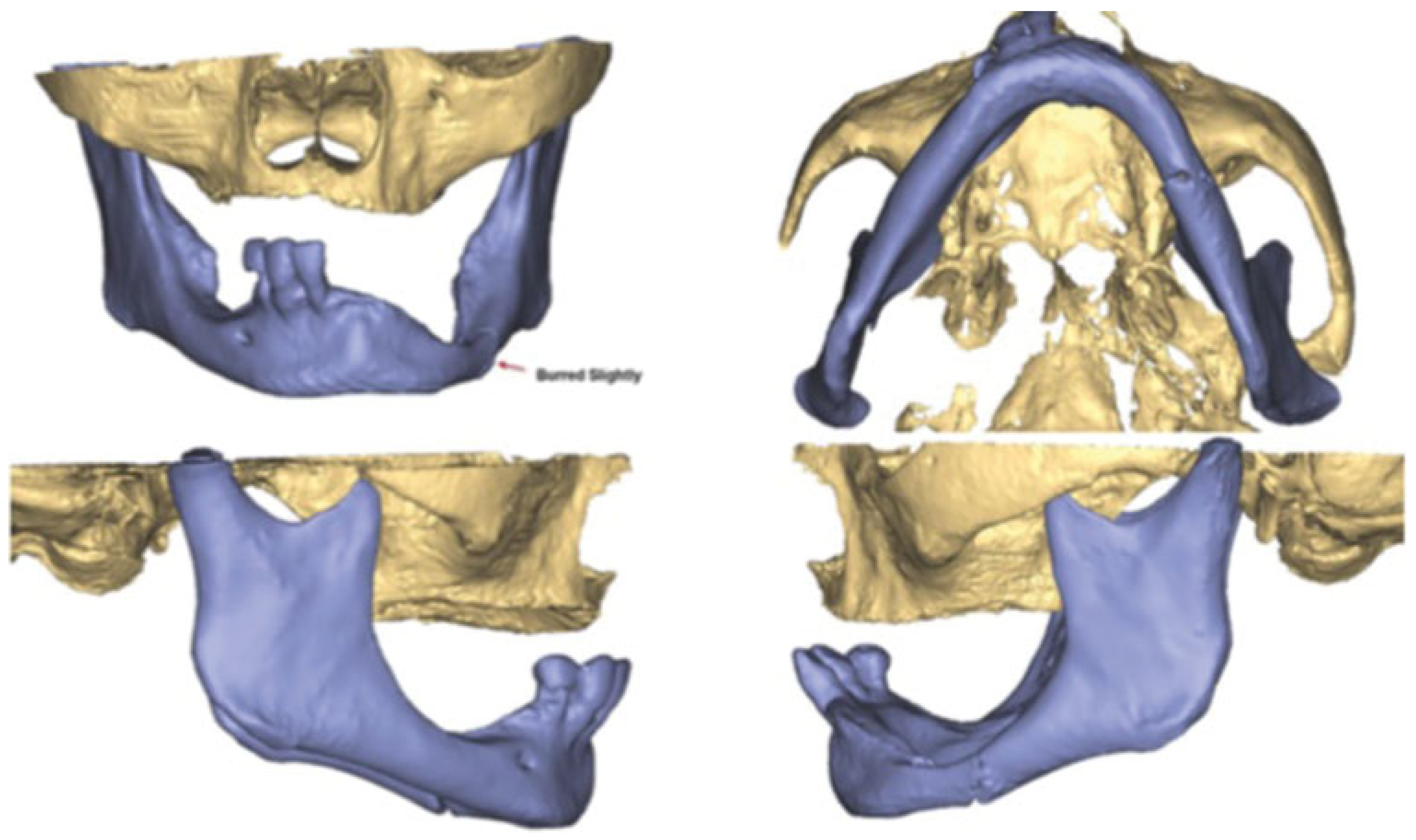
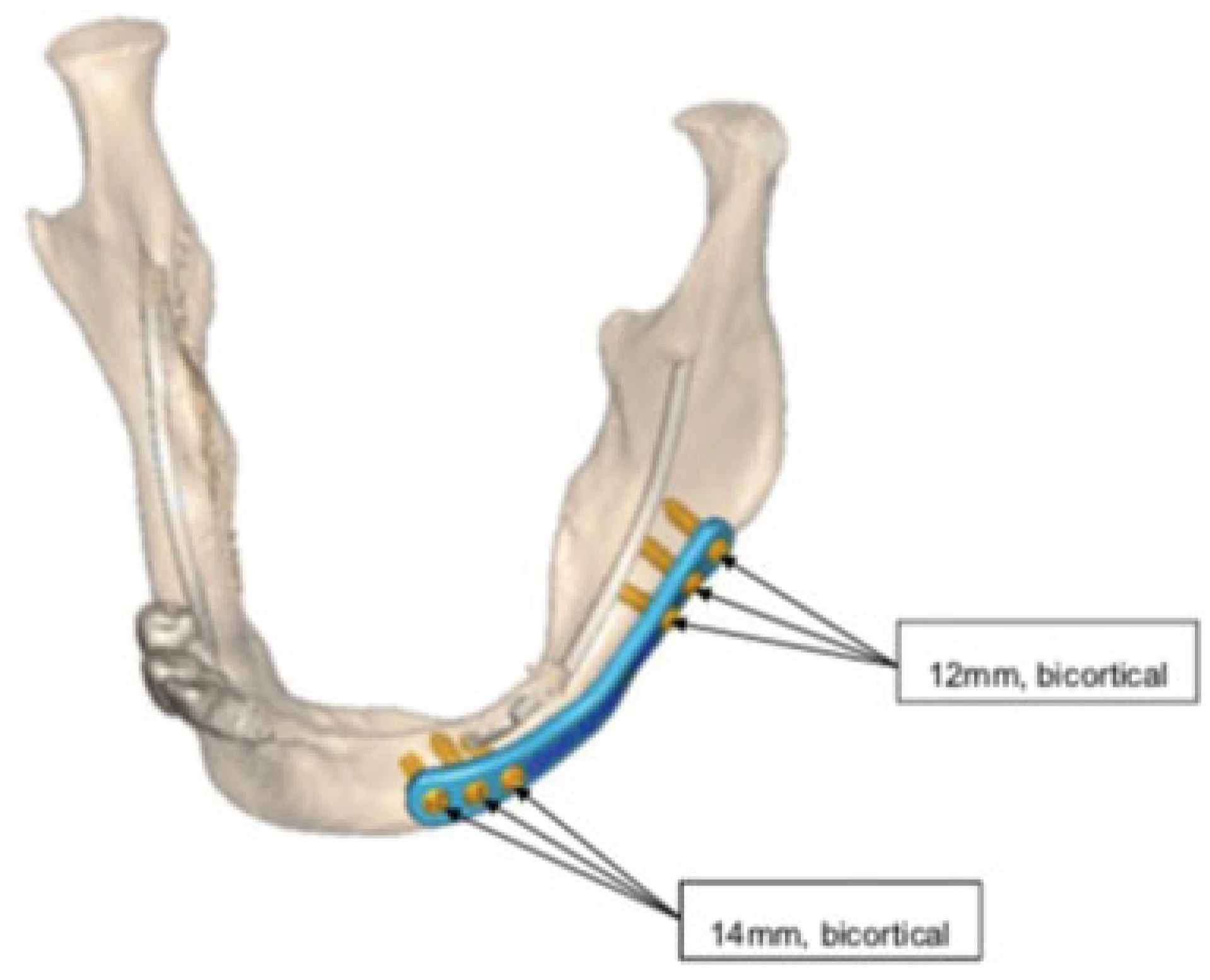
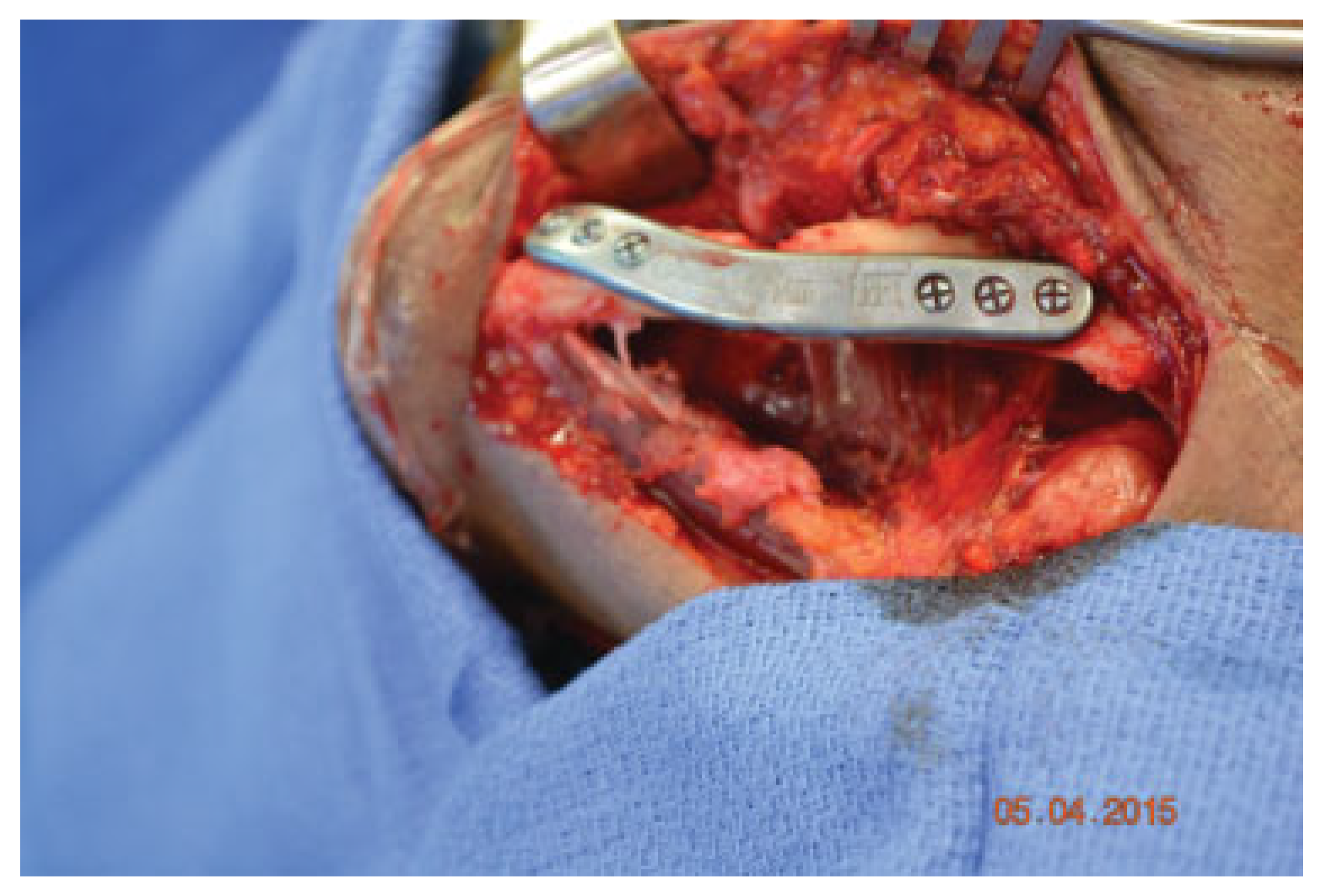
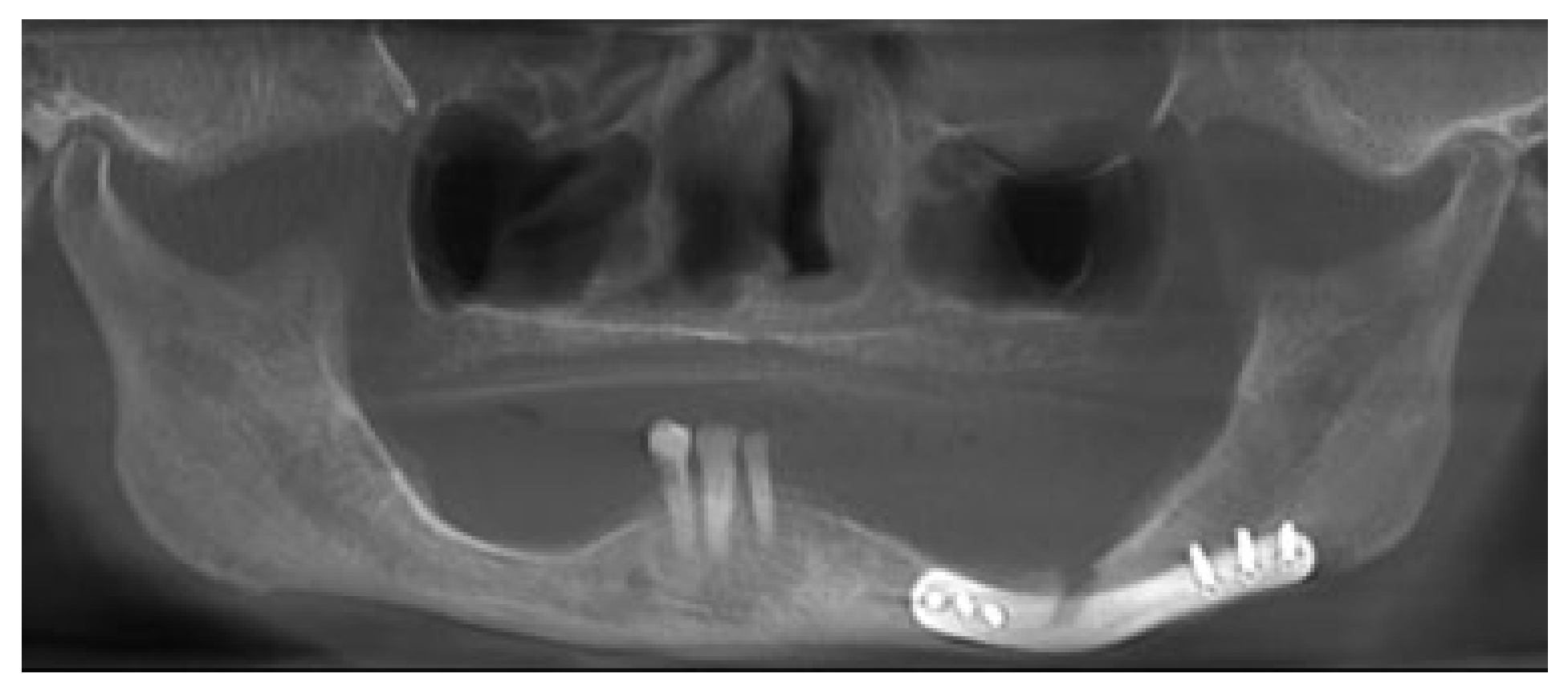
Case 1
Case 2
Discussion
Conflicts of Interest
References
- Farrell, B.B. Virtual surgical planning for intraoperative efficiency and accuracy with orthognathic surgery. J Oral Maxillofac Surg 2014, 72, e49–e50. [Google Scholar]
- Wang, Y.Y.; Fan, S.; Zhang, H.Q.; Lin, Z.Y.; Ye, J.T.; Li, J.S. Virtual surgical planning in precise maxillary reconstruction with vascularized fibular graft after tumor ablation. J Oral Maxillofac Surg 2016, 74, 1255–1264. [Google Scholar]
- Roser, S.M.; Ramachandra, S.; Blair, H.; et al. The accuracy of virtual surgical planning in free fibula mandibular reconstruction: Comparison of planned and final results. J Oral Maxillofac Surg 2010, 68, 2824–2832. [Google Scholar]
- Choi, C.C.; Nale, J.C.; et al. Virtual surgical planning for custom TMJ prosthetic joint replacement with simultaneous orthognathic surgery. J Oral Maxillofac Surg 2013, 71, e27–e28. [Google Scholar]
- Li, Y.; Jiang, Y.; Ye, B.; Hu, J.; Chen, Q.; Zhu, S. Treatment of dentofacial deformities secondary to osteochondroma of the mandibular condyle using virtual surgical planning and 3-dimensional printed surgical templates. J Oral Maxillofac Surg 2016, 74, 349–368. [Google Scholar]
- Steinbacher, D.M. Three-dimensional analysis and surgical planning in craniomaxillofacial surgery. J Oral Maxillofac Surg 2015, 73 (Suppl. 12), S40–S56. [Google Scholar]
- Kupfer, P.; Saadat, N.; et al. Open reduction and internal fixation of bilateral atrophic mandible fractures utilizing virtual surgical planning, custom cutting guides and reconstruction plate. A case report. J. Oral Maxillofac Surg 2016, 74, e89. [Google Scholar]
- Orentlicher, G.; Goldsmith, D.; Horowitz, A. Applications of 3-dimensional virtual computerized tomography technology in oral and maxillofacial surgery: Current therapy. J Oral Maxillofac Surg 2010, 68, 1933–1959. [Google Scholar]
- Bradley, J.C. Age changes in the vascular supply of the mandible. Br Dent J 1972, 132, 142–144. [Google Scholar]
- Bradley, J.C. A radiological investigation into the age changes of the inferior dental artery. Br J Oral Surg 1975, 13, 82–90. [Google Scholar]
- Luhr, H.G.; Reidick, T.; Merten, H.A. Results of treatment of fractures of the atrophic edentulous mandible by compression plating: A retrospective evaluation of 84 consecutive cases. J Oral Maxillofac Surg 1996, 54, 250–254, discussion 254–255. [Google Scholar] [CrossRef]
- Tiwana, P.S.; Abraham, M.S.; Kushner, G.M.; Alpert, B. Management of atrophic edentulous mandibular fractures: The case for primary reconstruction with immediate bone grafting. J Oral Maxillofac Surg 2009, 67, 882–887. [Google Scholar] [CrossRef]
- Castro-Núñez, J.; Cunningham, L.L.; Van Sickels, J.E. Atrophic mandible fractures: Are bone grafts necessary? An update. J Oral Maxillofac Surg 2017, 75, 2391–2398. [Google Scholar]
- Van Sickels, J.E.; Cunningham, L.L. Management of atrophic mandible fractures: Are bone grafts necessary? J Oral Maxillofac Surg 2010, 68, 1392–1395. [Google Scholar] [CrossRef]
- Schilli, W.; Stoll, P.; Bähr, W.; et al. Mandibular fractures. In Manual of Internal Fixation in the Cranio-Facial Skeleton: Techniques Recommended by the AO/ASIF Maxillofacial Group; Prein, J., Ed.; Springer: New York, NY, USA, 1998; p. 87. [Google Scholar]
- Scott, R.F. Oral and maxillofacial trauma in the geriatric patient. In Oral and Maxillofacial Trauma, 2nd ed.; Fonseca, R.J., Walker, R.V., Eds.; Saunders: Philadelphia, PA, USA, 1997; pp. 1045–1072. [Google Scholar]
- Wittwer, G.; Adeyemo, W.L.; Turhani, D.; Ploder, O. Treatment of atrophic mandibular fractures based on the degree of atrophy– experience with different plating systems: A retrospective study. J Oral Maxillofac Surg 2006, 64, 230–234. [Google Scholar] [CrossRef]
- Thoma, K.H. New methods for immobilization of the mandible. Oral Surg Oral Med Oral Pathol 1948, 1, 98–107. [Google Scholar]
- Mallett, S.P. Surgical reduction of multiple fractures in edentulous mandible: Report of case. J Oral Surg (Chic) 1956, 14, 155–158. [Google Scholar]
- Frost, D.; Tucker, M.; White, R. Small plate fixation for fixation of mandibular fractures. In Rigid Fixation in Maxillofacial Surgery; Tucker, M.R., Terry, B.C., White, R.P., et al., Eds.; Lippincott: Philadelphia, PA, USA, 1991; pp. 104–121. [Google Scholar]
- Ellis, E., III; Price, C. Treatment protocol for fractures of the atrophic mandible. J Oral Maxillofac Surg 2008, 66, 421–435. [Google Scholar] [CrossRef]
- Kunz, C.; Hammer, B.; Prein, J. Fractures of the edentulous atrophic mandible. Fracture management and complications[in German]. Mund Kiefer Gesichtschir 2001, 5, 227–232. [Google Scholar] [CrossRef]
- Levine, P.A. AO compression plating technique for treating fractures of the edentulous mandible. Otolaryngol Clin North Am 1987, 20, 457–477. [Google Scholar] [CrossRef]
- Bruce, R.A.; Strachan, D.S. Fractures of the edentulous mandible: The Chalmer, J. Lyons Academy study. J Oral Surg 1976, 34, 973–979. [Google Scholar] [CrossRef] [PubMed]
- Bruce, R.A.; Ellis, E., III. The second Chalmers, J. Lyons Academy study of fractures of the edentulous mandible. J Oral Maxillofac Surg 1993, 51, 904–911. [Google Scholar] [CrossRef]
- Batbayar, E.-O.; Bos, R.R.M.; van Minnen, B. A treatment protocol for fractures of the edentulous mandible. J Oral Maxillofac Surg 2018, 76, 2151–2160. [Google Scholar]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2019 by the author. The Author(s) 2019.
Share and Cite
Maloney, K.D.; Rutner, T. Virtual Surgical Planning and Hardware Fabrication Prior to Open Reduction and Internal Fixation of Atrophic Edentulous Mandible Fractures. Craniomaxillofac. Trauma Reconstr. 2019, 12, 156-162. https://doi.org/10.1055/s-0039-1677723
Maloney KD, Rutner T. Virtual Surgical Planning and Hardware Fabrication Prior to Open Reduction and Internal Fixation of Atrophic Edentulous Mandible Fractures. Craniomaxillofacial Trauma & Reconstruction. 2019; 12(2):156-162. https://doi.org/10.1055/s-0039-1677723
Chicago/Turabian StyleMaloney, Karl Daniel, and Torin Rutner. 2019. "Virtual Surgical Planning and Hardware Fabrication Prior to Open Reduction and Internal Fixation of Atrophic Edentulous Mandible Fractures" Craniomaxillofacial Trauma & Reconstruction 12, no. 2: 156-162. https://doi.org/10.1055/s-0039-1677723
APA StyleMaloney, K. D., & Rutner, T. (2019). Virtual Surgical Planning and Hardware Fabrication Prior to Open Reduction and Internal Fixation of Atrophic Edentulous Mandible Fractures. Craniomaxillofacial Trauma & Reconstruction, 12(2), 156-162. https://doi.org/10.1055/s-0039-1677723


