Isolated Orbital Floor Fracture Management: A Survey and Comparison of American Oculofacial and Facial Plastic Surgeon Preferences
Abstract
:Methods
Results
Demographics
Indications for Surgery
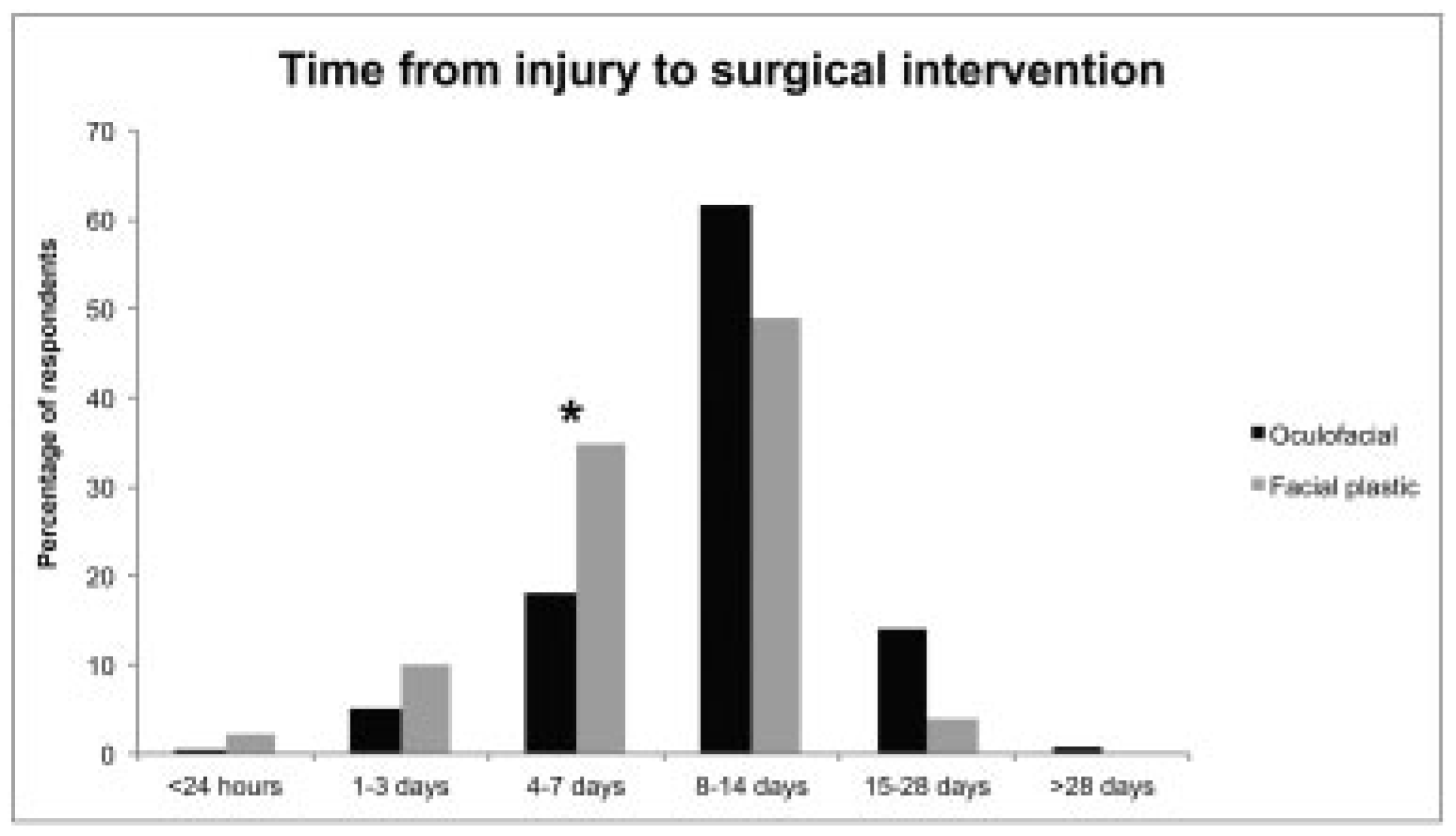
Time to Operation
Surgical Approach
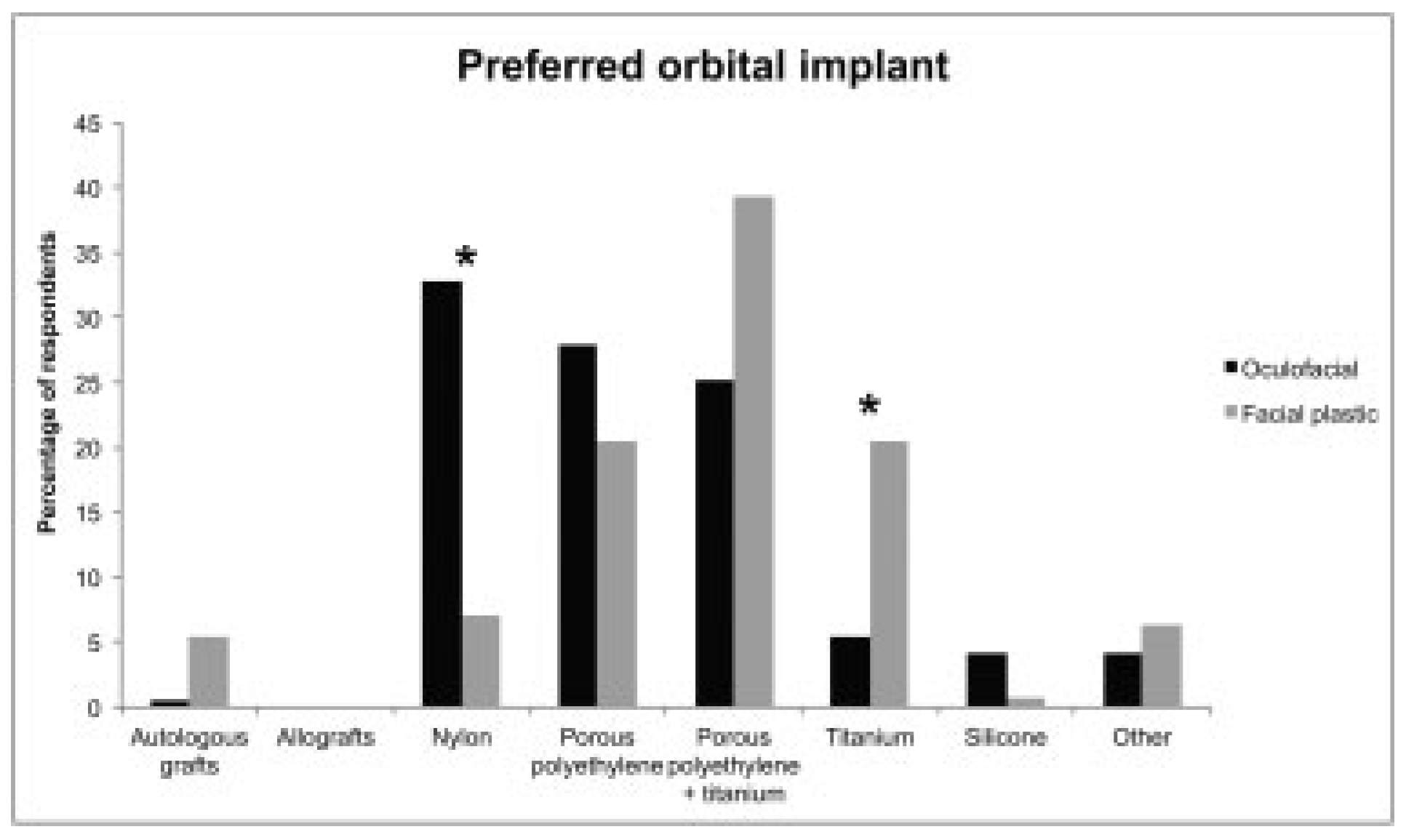
Orbital Implants
Imaging
Follow-up
Discussion
Demographics
Indications for Surgery
Time to Operation
Surgical Approach
Orbital Implants
Imaging
Follow-up
Limitations
Conclusions
Appendix A
| Question | Answer Choices |
|---|---|
| What is your surgical specialty? | Ophthalmology |
| Otolaryngology | |
| Plastic surgery | |
| Oral maxillofacial surgery | |
| Have you completed additional fellowship training? | Yes |
| No | |
| What fellowship training have you completed? | Plastic surgery |
| Facial plastic surgery | |
| Oculofacial surgery | |
| Craniofacial surgery | |
| Other | |
| How many years following training have you been in practice? | 0–5 |
| 6–10 | |
| 11–20 | |
| >20 | |
| Which of the following best describes your type of practice? | Solo |
| Group | |
| Multispecialty | |
| Academic | |
| How many orbital floor fracture repairs do you perform in a year? | 0 |
| 1–5 | |
| 6–10 | |
| 11–20 | |
| >20 | |
| Please indicate the strength of each of these factors in influencing your decision of whether or not to operate (on a scale of very weak, weak, moderate, strong, very strong) | Fracture size |
| Enophthalmos | |
| Motility restriction | |
| Early diplopia | |
| Persistent diplopia (at 2 wk) | |
| Cranial nerve V2 paresthesia | |
| What percentage of fracture patients that you see in the clinic/hospital requires surgery? | 0–10% |
| 11–30% | |
| 31–70% | |
| 71–90% | |
| 91–100% | |
| If surgery is indicated, what is your preferred time from injury to surgical intervention? | <24 h |
| 1–3 d | |
| 4–7 d | |
| 8–14 d | |
| 15–28 d | |
| >28 d | |
| What is your preferred operative approach for orbital floor fracture repair? | Transconjunctival |
| Subciliary | |
| Subtarsal | |
| Infraorbital | |
| Endoscopic | |
| Do you prefer a porous or nonporous implant? | Porous |
| Nonporous | |
| Which is your preferred choice of implant for orbital floor fracture repair? | Autologous grafts (e.g., bone, cartilage) |
| Allografts (e.g., dura mater, demineralized human bone) | |
| Nylon | |
| Porous polyethylene | |
| Porous polyethylene + titanium | |
| Titanium mesh | |
| Silicone | |
| Other | |
| Do you use other materials in addition to your preferred option? | Yes |
| No | |
| How often do you use 3D intraoperative navigation (e.g., Brainlab, fusion) for isolated orbital fracture repair? | Always |
| Sometimes | |
| Rarely | |
| Never | |
| How often do you use intraoperative imaging (CT scan)? | Always |
| Sometimes | |
| Rarely | |
| Never | |
| Do you perform routine postoperative imaging on patients after fracture repair? | Yes |
| No | |
| How long do you routinely follow up uncomplicated orbital fracture patients? | <1 mo |
| 1–3 mo | |
| 4–6 mo | |
| 7–12 mo | |
| 1–3 y | |
| >3 y |
References
- Sloan, B.H. Orbital floor blow-out fractures. Clin. Experiment Ophthalmol. 2004, 32, 3–4. [Google Scholar] [CrossRef] [PubMed]
- Aldekhayel, S.; Aljaaly, H.; Fouda-Neel, O.; Shararah, A.W.; Zaid, W.S.; Gilardino, M. Evolving trends in the management of orbital floor fractures. J. Craniofac Surg. 2014, 25, 258–261. [Google Scholar] [CrossRef]
- Christensen, B.J.; Zaid, W. Inaugural survey on practice patterns of orbital floor fractures for American oral and maxillofacial surgeons. J. Oral. Maxillofac. Surg. 2016, 74, 105–122. [Google Scholar] [CrossRef] [PubMed]
- Koh, V.; Chiam, N.; Sundar, G. Survey of common practices among oculofacial surgeons in the Asia-Pacific region: Management of orbital floor blowout fractures. Craniomaxillofac. Trauma. Reconstr. 2014, 7, 197–202. [Google Scholar] [CrossRef]
- Courtney, D.J.; Thomas, S.; Whitfield, P.H. Isolated orbital blowout fractures: Survey and review. Br. J. Oral. Maxillofac. Surg. 2000, 38, 496–504. [Google Scholar] [CrossRef]
- Lynham, A.J.; Chapman, P.J.; Monsour, F.N.; et al. Management of isolated orbital floor blow-out fractures: A survey of Australian and New Zealand oral and maxillofacial surgeons. Clin. Exp. Ophthalmol. 2004, 32, 42–45. [Google Scholar] [CrossRef]
- R Core Team(2016). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Available online: https://www.R-project.org (accessed on 20 February 2018).
- Ellis, E., III. Orbital trauma. Oral. Maxillofac. Surg. Clin. North. Am. 2012, 24, 629–648. [Google Scholar] [CrossRef] [PubMed]
- Roth, F.S.; Koshy, J.C.; Goldberg, J.S.; Soparkar, C.N. Pearls of orbital trauma management. Semin. Plast. Surg. 2010, 24, 398–410. [Google Scholar] [CrossRef]
- Burnstine, M.A. Clinical recommendations for repair of isolated orbital floor fractures: An evidence-based analysis. Ophthalmology 2002, 109, 1207–1210. [Google Scholar] [CrossRef]
- Dutton, J.J. Management of blow-out fractures of the orbital floor. Surv. Ophthalmol. 1991, 35, 279–280. [Google Scholar]
- Goldberg, R.A. Correlation of preoperative computed tomography and postoperative ocular motility in orbital blowout fractures. Arch. Facial Plast. Surg. 2002, 4, 61–62. [Google Scholar] [CrossRef] [PubMed]
- Hoşal, B.M.; Beatty, R.L. Diplopia and enophthalmos after surgical repair of blowout fracture. Orbit 2002, 21, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Manson, P.N.; Iliff, N. Management of blow-out fractures of the orbital floor. II. Early repair for selected injuries. Surv. Ophthalmol. 1991, 35, 280–292. [Google Scholar] [CrossRef]
- Biesman, B.S.; Hornblass, A.; Lisman, R.; Kazlas, M. Diplopia after surgical repair of orbital floor fractures. Ophthal. Plast. Reconstr. Surg. 1996, 12, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Hartstein, M.E.; Roper-Hall, G. Update on orbital floor fractures: Indications and timing for repair. Facial Plast. Surg. 2000, 16, 95–106. [Google Scholar] [CrossRef]
- Putterman, A.M. Management of blow out fractures of the orbital floor. III. The conservative approach. Surv. Ophthalmol. 1991, 35, 292–298. [Google Scholar] [CrossRef]
- Ridgway, E.B.; Chen, C.; Colakoglu, S.; Gautam, S.; Lee, B.T. The incidence of lower eyelid malposition after facial fracture repair: A retrospective study and meta-analysis comparing subtarsal, subciliary, and transconjunctival incisions. Plast. Reconstr. Surg. 2009, 124, 1578–1586. [Google Scholar] [CrossRef]
- Holtmann, B.; Wray, R.C.; Little, A.G. A randomized comparison of four incisions for orbital fractures. Plast. Reconstr. Surg. 1981, 67, 731–737. [Google Scholar] [CrossRef]
- Bähr, W.; Bagambisa, F.B.; Schlegel, G.; Schilli, W. Comparison of transcutaneous incisions used for exposure of the infraorbital rim and orbital floor: A retrospective study. Plast. Reconstr. Surg. 1992, 90, 585–591. [Google Scholar] [CrossRef]
- Kothari, N.A.; Avashia, Y.J.; Lemelman, B.T.; Mir, H.S.; Thaller, S.R. Incisions for orbital floor exploration. J. Craniofac Surg. 2012, 23 (Suppl. 1), 1985–1989. [Google Scholar] [CrossRef]
- Lee, H.B.; Nunery, W.R. Orbital adherence syndrome secondary to titanium implant material. Ophthal. Plast. Reconstr. Surg. 2009, 25, 33–36. [Google Scholar] [CrossRef] [PubMed]
- Shaye, D.A.; Tollefson, T.T.; Strong, E.B. Use of intraoperative computed tomography for maxillofacial reconstructive surgery. JAMA Facial Plast. Surg. 2015, 17, 113–119. [Google Scholar] [CrossRef] [PubMed]
| Oculofacial Number of Respondents (%) | Facial Plastic Number of Respondents (%) | p-Value | |
|---|---|---|---|
| Number of years in practice | 0.013 | ||
| 0–5 | 33 (14.7) | 37 (27.4) | 0.0058 |
| 6–10 | 34 (15.1) | 25 (18.5) | 0.46 |
| 11–20 | 60 (26.7) | 32 (23.7) | 0.53 |
| > 20 | 98 (43.6) | 43 (31.9) | 0.026 |
| Type of practice | 0.0018 a | ||
| Academic | 59 (26.2) | 56 (41.5) | 0.0034 |
| Solo | 59 (26.2) | 27 (20.0) | 0.2 |
| Group | 89 (39.6) | 34 (25.2) | 0.0059 |
| Multispecialty | 18 (8.0) | 18 (13.3) | 0.11 |
| Number of orbital floor fracture repairs per year | 0.000011 a | ||
| 0 | 5 (2.2) | 13 (9.6) | 0.0044 |
| 1–5 | 68 (30.2) | 61 (45.2) | 0.0046 |
| 6–10 | 62 (27.6) | 37 (27.4) | 1.00 |
| 11–20 | 59 (26.2) | 15 (11.1) | 0.00068 a |
| >20 | 31 (13.8) | 9 (6.7) | 0.039 |
| Percentage of fractures that require operation | 0.38 | ||
| 0–10% (rarely) | 27 (12.1) | 9 (7.1) | 0.15 |
| 11–30% (sometimes) | 82 (36.8) | 47 (37.0) | 1.00 |
| 31–70% (often) | 98 (43.9) | 56 (44.1) | 1.00 |
| 71–90% (mostly) | 14 (6.3) | 13 (10.2) | 0.21 |
| 91–100% (routinely) | 2 (0.9) | 2 (1.6) | 0.62 |
| Oculofacial Number of Respondents (%) | Facial Plastic Number of Respondents (%) | p-Value | |
|---|---|---|---|
| Fracture size | 0.35 | ||
| Very strong | 81 (37.5) | 58 (45.3) | 0.17 |
| Strong | 72 (33.3) | 43 (33.6) | 1.00 |
| Moderate | 53 (24.5) | 24 (18.8) | 0.23 |
| Weak | 9 (4.2) | 2 (1.6) | 0.22 |
| Very weak | 1 (0.5) | 1 (0.8) | 1.00 |
| Enophthalmos | 0.0022 a | ||
| Very strong | 120 (54.8) | 93 (72.7) | 0.00095 a |
| Strong | 71 (32.4) | 28 (21.9) | 0.037 |
| Moderate | 23 (10.5) | 5 (3.9) | 0.039 |
| Weak | 4 (1.8) | 0 (0.0) | 0.3 |
| Very weak | 1 (0.5) | 2 (1.6) | 0.56 |
| Motility restriction | 0.28 | ||
| Very strong | 166 (75.5) | 107 (83.6) | 0.080 |
| Strong | 45 (20.5) | 17 (13.3) | 0.11 |
| Moderate | 7 (3.2) | 4 (3.1) | 1.00 |
| Weak | 2 (0.9) | 0 (0.0) | 0.53 |
| Very weak | 0 (0.0) | 0 (0.0) | 1.00 |
| Early diplopia | 0.13 | ||
| Very strong | 23 (10.9) | 22 (17.3) | 0.10 |
| Strong | 48 (22.8) | 26 (20.5) | 0.68 |
| Moderate | 62 (29.4) | 43 (33.9) | 0.40 |
| Weak | 57 (27.0) | 31 (24.4) | 0.61 |
| Very weak | 21 (10.0) | 5 (3.9) | 0.057 |
| Persistent diplopia at 2 wk | 0.46 | ||
| Very strong | 124 (56.9) | 61 (47.3) | 0.095 |
| Strong | 59 (27.1) | 42 (32.6) | 0.33 |
| Moderate | 29 (13.3) | 22 (17.1) | 0.35 |
| Weak | 4 (1.8) | 2 (1.6) | 1.00 |
| Very weak | 2 (0.9) | 2 (1.6) | 0.63 |
| CN V2 paresthesia | 0.38 | ||
| Very strong | 4 (1.9) | 7 (5.5) | 0.11 |
| Strong | 11 (5.2) | 6 (4.7) | 1.00 |
| Moderate | 34 (16.0) | 24 (18.8) | 0.55 |
| Weak | 58 (27.2) | 29 (22.7) | 0.37 |
| Very weak | 106 (49.8) | 62 (48.4) | 0.82 |
| Oculofacial Number of Respondents (%) | Facial Plastic Number of Respondents (%) | p-Value | |
|---|---|---|---|
| Preferred operative approach | 0.0041 | ||
| Transconjunctival | 207 (94.1) | 112 (85.5) | 0.012 |
| Subciliary | 7 (3.2) | 15 (11.5) | 0.0028 |
| Subtarsal | 3 (1.4) | 1 (0.8) | 1.00 |
| Infraorbital | 3 (1.4) | 1 (0.8) | 1.00 |
| Endoscopic | 0 (0.0) | 2 (1.5) | 0.14 |
| 3D intraoperative navigation (e.g., Brainlab, fusion) | 0.080 | ||
| Always | 2 (0.9) | 1 (0.8) | 1.00 |
| Sometimes | 4 (1.8) | 9 (7.1) | 0.018 |
| Rarely | 33 (15.1) | 15 (11.8) | 0.42 |
| Never | 180 (82.2) | 102 (80.3) | 0.67 |
| Intraoperative imaging (CT scan) | 0.28 | ||
| Always | 9 (4.1) | 8 (6.2) | 0.44 |
| Sometimes | 8 (3.6) | 10 (7.8) | 0.13 |
| Rarely | 22 (10.0) | 12 (9.3) | 1.00 |
| Never | 181 (82.3) | 99 (76.7) | 0.21 |
| Routine postoperative imaging | 0.00000041 a | ||
| Yes | 12 (5.5) | 32 (24.8) | N/A |
| No | 208 (94.5) | 97 (75.2) | N/A |
| Length of follow-up | 0.20 | ||
| < 1 mo | 12 (5.4) | 13 (10.2) | 0.13 |
| 1–3 mo | 101 (45.3) | 53 (41.7) | 0.58 |
| 4–6 mo | 71 (31.8) | 33 (26.0) | 0.27 |
| 7–12 mo | 27 (12.1) | 23 (18.1) | 0.15 |
| 1–3 y | 9 (4.0) | 5 (3.9) | 1.00 |
| > 3 y | 3 (1.4) | 0 (0.0) | 0.56 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2018 by the author. The Author(s) 2018.
Share and Cite
Cohen, L.M.; Shaye, D.A.; Yoon, M.K. Isolated Orbital Floor Fracture Management: A Survey and Comparison of American Oculofacial and Facial Plastic Surgeon Preferences. Craniomaxillofac. Trauma Reconstr. 2019, 12, 112-121. https://doi.org/10.1055/s-0038-1639350
Cohen LM, Shaye DA, Yoon MK. Isolated Orbital Floor Fracture Management: A Survey and Comparison of American Oculofacial and Facial Plastic Surgeon Preferences. Craniomaxillofacial Trauma & Reconstruction. 2019; 12(2):112-121. https://doi.org/10.1055/s-0038-1639350
Chicago/Turabian StyleCohen, Liza M., David A. Shaye, and Michael K. Yoon. 2019. "Isolated Orbital Floor Fracture Management: A Survey and Comparison of American Oculofacial and Facial Plastic Surgeon Preferences" Craniomaxillofacial Trauma & Reconstruction 12, no. 2: 112-121. https://doi.org/10.1055/s-0038-1639350
APA StyleCohen, L. M., Shaye, D. A., & Yoon, M. K. (2019). Isolated Orbital Floor Fracture Management: A Survey and Comparison of American Oculofacial and Facial Plastic Surgeon Preferences. Craniomaxillofacial Trauma & Reconstruction, 12(2), 112-121. https://doi.org/10.1055/s-0038-1639350



