Abstract
This study was conducted to compare the outcome of single noncompression miniplate versus two noncompression miniplates in the treatment of mandibular angle fracture. A total of 40 patients were divided into two groups: Group I (n = 20), patients were treated by single miniplate at superior border of mandible by intraoral approach; Group II (n = 20), patients were treated by one miniplate at superior border miniplate of mandible, intraorally, and another at the lateral aspect of angle, transbuccally by trocar and cannula. Comparative evaluation was done at 1, 2, 4, 6, and 12 weeks and 6 months. The findings of this study suggest that there was no significant difference in postoperative complications (malocclusion, pain, swelling, infection, facial nerve injury, wound dehiscence, plate exposure) and bite force between the two groups.
In past decades, many techniques for the treatment of mandibular angle fractures have undergone a gradual evolution. Various techniques for the treatment of mandibular angle fractures have been reported in the literature. Ideal treatment for mandibular angle fractures still remains controversial, and these fractures are prone to high complication rates. Modern traumatology is based on the concept of osteosynthesis. Miniplate osteosynthesis was first introduced by Michelet et al.[1] in 1973 and further developed by Champy et al.[2] in 1975 who recommended a single noncompression miniplate along the “ideal line of osteosynthesis” in mandibular angle fracture.
Several biomechanical studies based on 3D models have challenged the stability of single-miniplate fixation of angle fractures with controversial results. Kroon et al.[3] and Choi et al.[4] both observed bony gaps along the inferior fracture border, and movement at fractured site resulted in subsequent complications, including infection. A second plate was suggested to reduce anterior-posterior separation of the fracture line as well as lateral displacement.[4,5,6]
The aim of this study is to compare the outcome of single noncompression miniplate versus two noncompression miniplates in the treatment of mandibular angle fracture.
Materials and Methods
This prospective randomized study was conducted on 40 patients (American Society of Anesthesiologist grade I, aged 18 years or above) with noncomminuted unilateral mandibular angle fracture reported to the Department of Oral and Maxillofacial Surgery, Sardar Patel Post Graduate Institute of Dental and Medical Sciences and Dr. O.P. Chaudhary Hospital and Research Centre, Lucknow, India. The institutional ethical committee approved the study design and written informed consent was obtained from all the patients.
Preoperatively, detailed medical/dental history of the patients was recorded and routine blood/urine investigations were done. Patients were diagnosed on the basis of the clinical examination and radiographic interpretation (orthopantomogram, posteroanterior view mandible).
Patients with insufficient dentition to reproduce occlusion, with anyother associated fractures, pathological fractures, and fracture more than 7 days old, and patients who underwent radiotherapy in the past 5 years were excluded from the study.
In this study, patients were randomly divided into two groups (20 patients in each group) and were operated under general anesthesia. In Group I patients, a single noncompression miniplate was fixed at the superior border as suggested by Champy et al.[2] through an intraoral approach. In Group II, patients were treated with two noncompression miniplates, one miniplate at superior border of mandible (intraoral approach) and another at the lateral aspect of angle using trocar and cannula (transbuccal approach). All patients were kept on maxillomandibular fixation (MMF) with elastics for 14 days. Patients in both the groups were given antibiotics (cefotaxime 1 g intravenously before induction and postoperatively 12 hourly for 3 days, followed by oral antibiotics for 7 days) and analgesic as Diclofenac sodium 50 mg, 12 hourly for 5 days postoperatively. Chlorhexidine oral rinse (0.2%) was prescribed for 2 weeks. Patients were strictly on liquid diet for the initial 4 weeks and then gradually resume normal diet over a period of additional 3 to 4 weeks.
Patients were assessed by comparing operative time (from incision to closure); postoperative occlusion; infection; pain (on visual analog scale),[7] swelling (according to Pöllmann);[8] facial nerve injury; wound dehiscence; and plate exposure at follow-up periods 1, 2, 4, 6, and 12 weeks. Bite force measurements were recorded preoperatively and 3 and 6 months postoperatively.
Bite force measurements were made using an indigenous bite force recorder. The recorder consists of four strain gauges mounted on steel bars, forming a Wheatstone bridge circuit, based on the principle of Tate et al.[9] Load changes in the steel bar produce a measurable voltage change across the four strain gauges. Readings displayed on the digital monitor were converted into kilopond. All measurements were taken with the patient seated upright with an unsupported natural head position and looking in forward direction. The patients were asked to remain in this position throughout the trial and to refrain from extraneous movements. Bite force was recorded at the right and left molar regions. The patients were instructed to bite as forcefully as possible on the pads of bite force gauge to the maximum level and bite force values were recorded. Data were analyzed using Statistical Package for Social Sciences (SPSS) version 15.0.
Results
In this study, a total of 40 patients with isolated noncomminuted mandibular angle fracture were randomly selected as per inclusion criteria and divided into two groups: Group I (n = 20) and Group II (n = 20). There were 33 male and 7 female patients in the study; therefore, the male:female ratio was 4.7:1. There were 17 males (85%) and 3 females (15%) in Group I, whereas 16 males (80%) and 4 females (20%) in Group II. There was no significant difference in gender predilection between the groups (p > 0.05). Mean age of patients in Group I was 30.25 ± 9.50 years, whereas mean age of patients in Group II was 29.71 ± 8.36 years. No statistically significant difference was found on comparing the mean age of the patients of both groups (p > 0.05).
In this study, road traffic accident (RTA) was found to be the most common etiology in both the groups followed by fall from height. Work place–related trauma was the least common etiology (Figure 1).
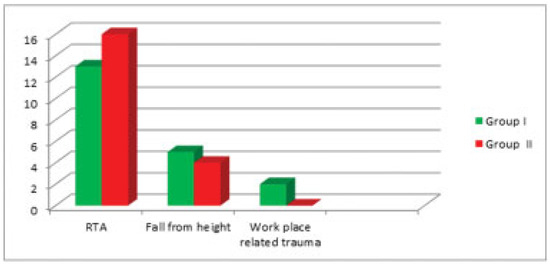
Figure 1.
Etiology of Group I and Group II patients. RTA, road traffic accident.
In this study, the mean operative time for Group I is 38 min (range: 26–60 min) and for Group II, it is 81 min (range: 64–105 min). The mean operative time taken in Group II is significantly more (p < 0.001) than in Group I (Figure 2).
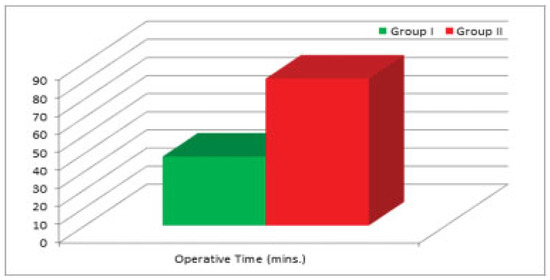
Figure 2.
Mean operative time of Group I and Group II.
In both the groups, majority of the cases presented with deranged occlusion. In Group I, 16 (80%) cases had deranged occlusion and 4 (20%) cases had intact occlusion, while in Group II, 18 (90%) cases had deranged occlusion and 2 (10%) cases had intact occlusion. The functionally stable occlusion was achieved in all patients (in both the groups) in postoperative period. Hence, there is no significant difference in occlusion for Group I and Group II (p > 0.05).
Preoperatively, the mean pain score in Group I was 4.30 ± 1.26 and in Group II it was 4.40 ± 1.14. In postoperative first and second weeks, there was decrease in pain score in both groups. From the postoperative fourth week onwards, all patients (both groups) had no significant pain. No statistically significant (p > 0.05) difference was observed between Group I and Group II in the postoperative period (Table 1, Figure 3).

Table 1.
Evaluation of pain.
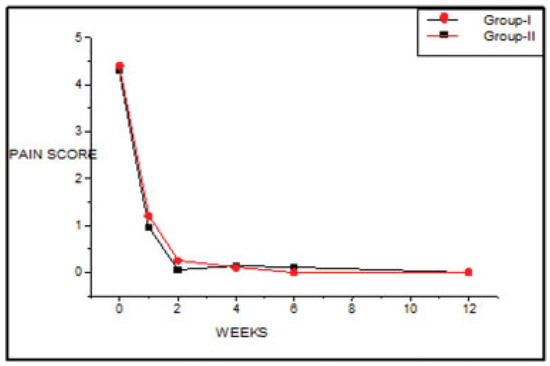
Figure 3.
Mean pain score in preoperative and postoperative period.
Swelling was maximal in postoperative first week; thereafter it slowly diminished during subsequent postoperative period in both the groups (Table 2, Figure 4). No statistically significant difference was found between the two groups (p > 0.05).

Table 2.
Evaluation of swelling (tragus–pogonion in centimeter).
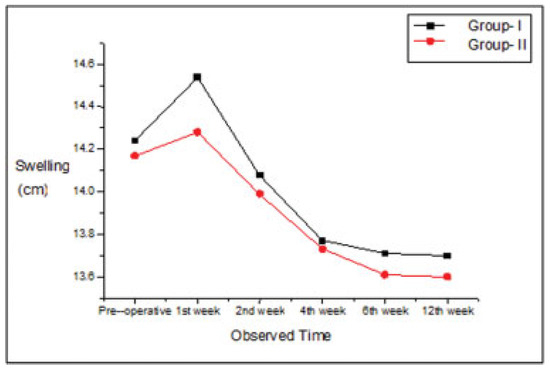
Figure 4.
Mean swelling in preoperative and postoperative period.
Bite force was recorded on fractured and nonfractured site of the patients, preoperatively as well as 3 and 6 months postoperatively. There was no significant difference (p > 0.05) in bite force in preoperative period between both groups on fractured site and nonfractured site (Table 3, Figure 5). In each group, there was highly significant difference (p < 0.001) in bite force between fractured site and nonfractured site during preoperative and postoperative periods (Table 4).

Table 3.
Evaluation of bite force (in kilopond).
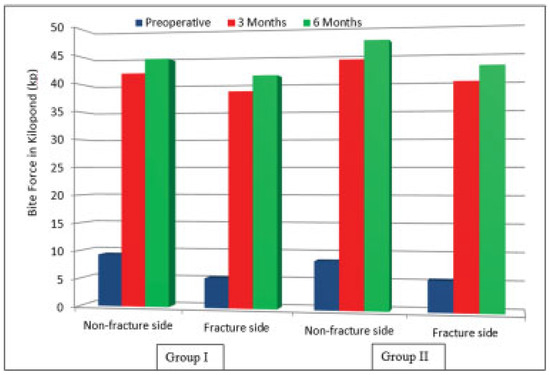
Figure 5.
Bite force in preoperative and postoperative period in both groups.

Table 4.
Comparison of bite force between fractured site and nonfractured site in both groups.
Bite force significantly improved from preoperative to postoperative periods in nonfractured site and fractured site in both groups (p < 0.001). Between 3 and 6 months postoperatively, significant improvement (p < 0.01) in bite force was found on both sites in Group I and Group II (Table 5). There was no significant difference (p > 0.05) in bite force in postoperative period on fractured site and nonfractured site between both groups (Table 3).

Table 5.
Comparison of bite force between preoperative and postoperative periods in both groups by paired t-test.
In this study, three patients were reported for surgical site infection, two patients in Group I and one patient in Group II which was managed conservatively with antibiotics. None of the patients in either group reported with facial nerve injury, wound dehiscence, and plate exposure.
Discussion
In several biomechanical studies based on 3D models, the stability of single-miniplate fixation in the management of angle fractures was challenged.[3,4,6,10,11] Bony gaps at the inferior border and movement at fractured site has been reported in single-miniplate fixation technique which contributes to subsequent complications, including infection.[3,4] A second plate was suggested to reduce anterior-posterior separation of the fracture line as well as resist torsional forces, which provides increased stability. According to biomechanical studies, single-plate fixation should have high rate of infection than two-plate fixation in the angle region of mandible.[4,12,13] The study of Ellis[14] contradicts the results of such biomechanical tests because he observed increased rate of infection in patients with two-plate fixation.
Levy et al.[15] have provided clinical evidence that paired miniplate fixation may provide superior fixation of angle fractures over single miniplate. They reported high complication percentage in patients treated with a single miniplate across the oblique line.
Ellis and Walker[14,16] have reported that the complication rate was much higher in two points of fixation than one point of fixation in mandibular angle fracture. Danda[17] performed similar trial; he reported no significant differences in postoperative complication rates in both the groups. In a similar study performed by Schierle et al.,[18] they concluded that no significant differences were found between the groups in terms of postoperative infection and occlusal disturbances. The findings of our study also showed that there was no significant difference in complication rates (malocclusion, infection, wound dehiscence, and plate exposure) between the two groups. In our study, we achieved functionally stable occlusion in all the cases postoperatively. Ellis[14] also attained normal occlusal relationship in all the patients without MMF, except three patients who had malocclusion and who responded to MMF with elastics for 1 to 2 weeks.
We observed a sharp decrease in intensity of postoperative pain in the initial first postoperative week. There was no significant difference in postoperative pain score between both the groups.
Saikrishna et al.[19] observed postoperative swelling with transbuccal approach due to blunt dissection of the masseter muscle to approach surgical site, 65% of the cases had operative edema for 4 days while 35% of cases had operative edema for 6 days. Persistence of the swelling was noted for 2 weeks postoperatively in 70% of cases. In our study, we found that postoperative swelling was present in 65% of the total cases for first week which subsided gradually in the subsequent postoperative period in both the groups. Only 15% of the total cases had swelling in the second week postoperatively.
Studies provide evidence that the main reason for infection associated with rigid fixation is the failure to achieve stability even after placement of plates and screws.[12,20,21] In such case, the single-miniplate group should have had more infections than the two-miniplate group. However, the process of fixing the second miniplate at the lower border also means increased periosteal stripping, bacterial contamination, and additional miniplate on the mandible, which theoretically increase the possibility of infection.[13] Ellis[14] treated most of the infected cases with intraoral incision and drainage, removal of plate, and antibiotics; only two patients required hospitalization, intravenous antibiotics, and surgery. In our study, infection was reported in two cases in Group I and in one case in Group II and these findings support the previous studies. Patients reported with infection were treated conservatively by antibiotics on the basis of pus culture and sensitivity test and plate removal was not required in any patient.
Siddiqui et al.[13] reported patients presented with weakness of the marginal mandibular nerve postoperatively and also involves the risk of scarring due to transbuccal instrumentation. Transbuccal instrumentation does have potential adverse consequences for the patient and should be avoided. In our study, no patient reported for facial nerve injury and facial scar was inconspicuous.
Gerlach and Schwarz[22] stated that the maximal bite force in patients with mandibular fractures treated with miniplate osteosynthesis had reached only 31% at 1 week postoperatively compared with a healthy control group. These values had increased to 58% at 6 weeks postoperatively. Tate et al.[9] also evaluated vertical bite forces after treatment of angle fractures using two miniplates. They found 52% of molar forces obtained within a control group at 6 weeks postoperatively (nonfractured individual). In our study, bite force significantly improved in the subsequent postoperative periods in comparison to the preoperative bite force in both the groups individually, but it was insignificant when both groups are compared.
The duration of MMF in the treatment of mandibular angle fractures is still controversial.[23,24,25] The study by Bolourian et al.[23] showed a 4.2% complication rate in 44 fractures treated with a single noncompression miniplate at the superior border of the mandible and postsurgical MMF for 2 weeks, but in our study no major complications were noted.
Single-miniplate fixation has advantages such as less periosteal stripping, less morbidity, less time consuming, economic, and less postoperative complications with aesthetic results with possible. Two-miniplate fixation technique has certain advantages such as more stable fixation, more adequate bone contact with early regaining of masticatory load but not statistically significant. Disadvantages of two-miniplate fixation technique are more periosteal stripping, requirement of special armamentarium (trocar and cannula), increased operating time, increased operative cost, technique sensitive, chance of facial nerve injury, and extraoral scar.
Conclusion
A noncomminuted mandibular angle fracture can be successfully treated with both the fixation techniques. The results of our study showed that the use of two noncompression miniplates does not seem to have major advantage over the use of a single noncompression miniplate in the treatment of mandibular angle fracture. There was no statistically significant difference in postoperative complications (malocclusion, pain, swelling, infection) between the two groups. In this study, both the fixation techniques seem to be effective and reliable. Further clinical studies are required to determine the ideal treatment modality for mandibular angle fractures.
References
- Michelet, F.X.; Deymes, J.; Dessus, B. Osteosynthesis with miniaturized screwed plates in maxillo-facial surgery. J. Maxillofac. Surg. 1973, 1, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Champy, M.; Loddé, J.P.; Schmitt, R.; Jaeger, J.H.; Muster, D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J. Maxillofac. Surg. 1978, 6, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Kroon, F.H.; Mathisson, M.; Cordey, J.R.; Rahn, B.A. The use of miniplates in mandibular fractures. An in vitro study. J. Craniomaxillofac. Surg. 1991, 19, 199–204. [Google Scholar] [CrossRef]
- Choi, B.H.; Yoo, J.H.; Kim, K.N.; Kang, H.S. Stability testing of a two miniplate fixation technique for mandibular angle fractures. An in vitro study. J. Craniomaxillofac Surg. 1995, 23, 123–125. [Google Scholar] [CrossRef]
- Barber, H.D.; Woodbury, S.C.; Silverstein, K.E. Mandibular fractures. In Oral and Maxillofacial Trauma, 2nd ed; Fonseca, R.F., Walker, R.V., Betts, N.J., Powers, M.P., Eds.; Saunders: Philadelphia, PA, USA, 1997; pp. 473–526. [Google Scholar]
- Gear, A.J.; Apasova, E.; Schmitz, J.P.; Schubert, W. Treatment modalities for mandibular angle fractures. J. Oral. Maxillofac. Surg. 2005, 63, 655–663. [Google Scholar] [CrossRef]
- Myles, P.S.; Troedel, S.; Boquest, M.; Reeves, M. The pain visual analog scale: Is. it linear or nonlinear? Anesth. Analg. 1999, 89, 1517–1520. [Google Scholar] [CrossRef]
- Pöllmann, L. Wound healing–A study on circaseptan reactive periodicity. Chronobiol. Int. 1984, 1, 151–157. [Google Scholar] [CrossRef]
- Tate, G.S.; Ellis, E., III; Throckmorton, G. Bite forces in patients treated for mandibular angle fractures: Implications for fixation recommendations. J. Oral. Maxillofac. Surg. 1994, 52, 734–736. [Google Scholar] [CrossRef] [PubMed]
- Shetty, V.; McBrearty, D.; Fourney, M.; Caputo, A.A. Fracture line stability as a function of the internal fixation system: An in vitro comparison using a mandibular angle fracture model. J. Oral. Maxillofac. Surg. 1995, 53, 791–801; discussion 801–802. [Google Scholar] [CrossRef]
- Alkan, A.; Çelebi, N.; Özden, B.; Baş, B.; İnal, S. Biomechanical comparison of different plating techniques in repair of mandibular angle fractures. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2007, 104, 752–756. [Google Scholar] [CrossRef]
- Rudderman, R.H.; Mullen, R.L. Biomechanics of the facial skeleton. Clin. Plast. Surg. 1992, 19, 11–29. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, A.; Markose, G.; Moos, K.F.; McMahon, J.; Ayoub, A.F. One miniplate versus two in the management of mandibular angle fractures: A prospective randomised study. Br. J. Oral. Maxillofac. Surg. 2007, 45, 223–225. [Google Scholar] [CrossRef]
- Ellis, E., III. Treatment methods for fractures of the mandibular angle. Int. J. Oral. Maxillofac. Surg. 1999, 28, 243–252. [Google Scholar] [CrossRef]
- Levy, F.E.; Smith, R.W.; Odland, R.M.; Marentette, L.J. Monocortical miniplate fixation of mandibular angle fractures. Arch. Otolaryngol. Head. Neck Surg. 1991, 117, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E. III, Walker, L. Treatment of mandibular angle fractures using two noncompression miniplates. J. Oral. Maxillofac. Surg. 1994, 52, 1032–1036. [Google Scholar] [CrossRef] [PubMed]
- Danda, A.K. Comparison of a single noncompression miniplate versus 2 noncompression miniplates in the treatment of mandibular angle fractures: A prospective, randomized clinical trial. J. Oral. Maxillofac. Surg. 2010, 68, 1565–1567. [Google Scholar] [CrossRef]
- Schierle, H.P.; Schmelzeisen, R.; Rahn, B.; Pytlik, C. Oneor two-plate fixation of mandibular angle fractures? J. Craniomaxillofac. Surg. 1997, 25, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Saikrishna, D.; Shetty, S.K.; Singh, V.K. A clinical study on transbuccal fixation of mandibular angle fractures. J. Maxillofac. Oral. Surg. 2008, 7, 371–373. [Google Scholar]
- Assael, L.A. Treatment of mandibular angle fractures: Plate and screw fixation. J. Oral. Maxillofac. Surg. 1994, 52, 757–761. [Google Scholar] [CrossRef]
- Iizuka, T.; Lindqvist, C.; Hallikainen, D.; Paukku, P. Infection after rigid internal fixation of mandibular fractures: A clinical and radiologic study. J. Oral. Maxillofac. Surg. 1991, 49, 585–593. [Google Scholar] [CrossRef]
- Gerlach, K.L.; Schwarz, A. Bite forces in patients after treatment of mandibular angle fractures with miniplate osteosynthesis according to Champy. Int. J. Oral. Maxillofac. Surg. 2002, 31, 345–348. [Google Scholar] [CrossRef] [PubMed]
- Bolourian, R.; Lazow, S.; Berger, J. Transoral 2.0-mm miniplate fixation of mandibular fractures plus 2 weeks’ maxillomandibular fixation: A prospective study. J. Oral. Maxillofac. Surg. 2002, 60, 167–170. [Google Scholar] [CrossRef] [PubMed]
- Chritah, A.; Lazow, S.K.; Berger, J.R. Transoral 2.0-mm locking miniplate fixation of mandibular fractures plus 1 week of maxillomandibular fixation: A prospective study. J. Oral. Maxillofac. Surg. 2005, 63, 1737–1741. [Google Scholar] [CrossRef] [PubMed]
- Mehra, P.; Murad, H. Internal fixation of mandibular angle fractures: A comparison of 2 techniques. J. Oral. Maxillofac. Surg. 2008, 66, 2254–2260. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2018 by the author. The Author(s) 2018.