Abstract
Plastic surgical techniques were described in antiquity and the Middle Ages; however, the genesis of modern plastic surgery is in the early 20th century. The exigencies of trench warfare, combined with medical and technological advances at that time, enabled pioneers such as Sir Harold Gillies to establish what is now recognized as plastic and reconstructive surgery. The physicians of Germany, Russia, and the Ottoman Empire were faced with the same challenges; it is fascinating to consider parallel developments in these countries. A literature review was performed relating to the work of Esser, Lanz, Joseph, Morestin, and Filatov. Their original textbooks were reviewed. We describe the clinical, logistical, and psychological approaches to managing plastic surgical patients of these physicians and compare and contrast them to those of the Allies, identifying areas of influence such as Gillies’ adoption of Filatov’s tube pedicle flap.
Aesthetic and reconstructive surgery has existed in several guises since the Egyptian Old Kingdom in 3000 BC, with the advent of modern plastic surgery as a discrete specialty arising shortly prior to the Great War.[1] As with many branches of medicine and surgery, the World Wars catalyzed the development of new techniques and the realization of talent from some driven and intriguing individuals. The most well-known names in the western hemisphere are unquestionably Sir Harold Gillies and Sir Archibald McIndoe; however, physicians of the Central Powers and wider Europe were faced with the same challenges and opportunities. Although Gillies was a tireless innovator, his practice was also inspired and informed by the techniques devised and published by the subjects of this article. With the shadow cast over German surgery by the events of World War Two, there is a risk that the contributors to the art from the Central Powers will fade into ignominy. Therefore, there is scope for a review article discussing the precursors to the emergence of plastic surgery from Germany, Austria, and the Ottoman Empire.
This article will discuss the principle contributors from the Central Powers during in the early 20th century, identify the techniques they pioneered, and describe their contribution to the literary record. In particular, we compare and contrast the circumstances faced by each of the protagonists and reflect on the geographical constraints that affected the dissemination of these ideas in the predigital era.
Methods
A MEDLINE literature search was performed using the names of the authors Lexer, Joseph, Lanz, Esser, Filatov, and Morestin. The original editions of their published works/books were translated and reviewed. Contemporary plastic surgery histories on the subject were read and bibliographies cross-referenced with the aforementioned literature search. Significant contributors from the field of maxillofacial surgery arising from these reviews were also researched and included. Following compilation of these data, a map was drawn of the areas in which each of the surgeons was operating during World War One and a timeline compiled of their most notable achievements.
Results: Biographies
Figure 1 shows the timelines of the life spans of the key protagonists and how they related to the World Wars of the 20th Century.
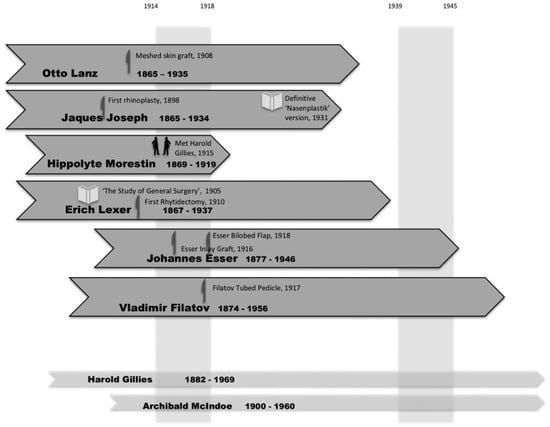
Figure 1.
Life events of the Central Powers Pioneers.
Figure 2 is a map of Central and Western Europe that is annotated with their areas of practice over World War One. Table 1 is a compilation of significant events for each of these surgeons.
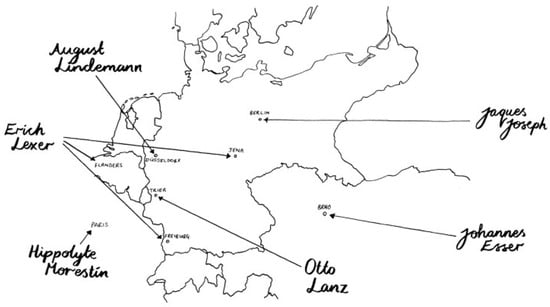
Figure 2.
Geographical locations of the Central Powers Pioneers during the Great War.

Table 1.
Significant contributions of the Central Powers Pioneers.
Any history of the development of plastic surgery requires a discussion of those who set the stage for the development of these pioneers. They influenced this generation through direct tutorship orliterary disseminationof their techniques. Accordingly, we will briefly discuss Von Graefe, Dieffenbach, and Langenbeck. These surgeons had a direct influence on the training or early development of the subjects of this review.[2] They were revered surgeons themselves and practiced reconstructive and aesthetic techniques. The most significant aspect of their influence is their geographical location—they all worked as senior members of the famous Charité Hospital in Berlin, the most advanced hospital in Germany at that time. Karl Ferdinand von Gräfe (1787–1840) was physician to the General Staff of the Prussian Army. While working in the Charité Hospital, he considered the works of his Indian and Italian predecessors and modified these to develop his own method of rhinoplasty. Dieffenbach (1792–1847) fought in the Napoleonic wars as a Jaeger (Light Infantry) where he witnessed the plights of the wounded soldiers; this led to his adoption of reconstructive surgery.[3] He developed many techniques in facial reconstruction, mammaplasty, and cleft palate repair.[4] He was later appointed the Director of the Charité Hospital, where he was succeeded by Bernhard von Langenbeck. Langenbeck (1810–1887) is well known to us for his retractor and the concept of the surgical residency. However, he also continued some of Dieffenbach’s maxillofacial work, developing his own palatoplasty technique. The fact that there was a strong legacy of plastic surgery present in this hospital prior to the World War One is relevant; some of our subjects worked there and this influenced their practice.
Harold Delf Gillies
Although this article concentrates mainly on the Central Powers, no history of plastic surgery of World War One would be complete without the mention of the greatest and most famed of the pioneers. He has been eulogized and studied extensively; as both an originator and developer of techniques, he has no equal. His initial training in otolaryngology was no doubt the grounding for his head and neck surgeries; however, there were three main influences that led to his part in the creation of plastic surgery as a specialty [5]. First, his meeting and partnership with Valadier, the dental surgeon with whom he initially practiced in the World War One. Second, he obtained an essay by Lindemann on jaw reconstruction. Lastly, while on leave in Paris, he met Hippolyte Morestin, which helped to set him on his path.[5,6] Gillies’reputation as a true visionary can be ascribed to identifiable aspects of his practice. In 1915, Gillies was appointed to lead the Plastic Surgery Department in the Cambridge Hospital in Aldershot. He proved himself to be an effective departmental head, and emphasized the need for teamwork and efficiency in the face of the overwhelming number of casualties from the Battle of the Somme. The volume of cases that he encountered there taught him important lessons in logistics and resource management. In his subsequent move to the Queen’s Hospital in Sidcup, London, in 1917, Gillies had a leadership role in the development of the hospital site. This allowed for efficient management of the special requirements of the reconstructive patient, albeit it having come toward the end of the war. This contrasts with the German system, in which the development of plastic surgical techniques in multiple smaller centers at the start of the war permitted a quicker response to large volumes of reconstructive patients. The deliberately open nature of the Queen’s Hospital Unit, where the international surgical community was welcomed, ensured that there was an audience to witness his ingenuity and facilitate dissemination of his techniques. His pensive nature during operations allowed for innovation within the operating theater. He had absolute certainty that plastic surgery should exist as a discrete entity, despite this not being reflected by the medical establishment of that time. Lastly, despite his tireless work ethic, it is clearly evident from descriptive works that he was an infectiously likeable man, an essential component in the development of his legacy. Gillies’ main work from World War One, “Plastic Surgery of the Face,” published in 1920, is the most engaging as a series of case studies. Looking at Esser’s book “Biological Flaps,” it is possible that Esser used this format as inspiration to construct his volume around a similarly large number of cases.[7,8] “Plastic Surgery of the Face” consolidated many of the practices that Gillies adopted, improved upon, and invented himself; it is an invaluable document detailing some of the best work of Sir Harold.
Otto Lanz
One of the earliest contributors to plastic surgery in the Great War, Otto Lanz was a Swiss general surgeon, born in 1865 in Steffisburg, Switzerland. Studying in Geneva, he undertook surgical training under Kocher in Bern, Germany, before settling in Amsterdam. There, he made his impact as a one of the Chairs of General Surgery. He was an imposing man, bearded and ferocious, but one who enjoyed teaching, and he was a keen art collector.[5] During his time in Amsterdam, he was the first to describe the meshed skin graft, publishing on it in 1908 in Zentralblatt fur Chirurgie (Central Sheet for Surgery).[9] This was not published in English for many years. The timing of his inception of this technique was impeccable and allowed for larger areas of skin grafting during the war.[10] At the outbreak of the Great War, he was 49-years-old and situated in neutral Holland, volunteering to treat the German war wounded in the military hospital in Trier.[11] His contribution with respect to the rapid evacuation of personnel from the front line and adherence to Joseph Lister’s aseptic methods demonstrate that he was a highly effective wartime surgeon. This improvement in casualty evacuation timelines was facilitated by the fact that the German Army was anticipating a longer occupation and was fighting on their own ground. This meant that their evacuation chains back to the tertiary centers of the day were less convoluted and they were certainly better at this than the Allied Forces, with the encumbrance of the English Channel. All surgeons today are aware of his eponymous incision, which we know of as a cosmetic improvement to a general surgical procedure; this is indicative of his wider practice, as he remained a predominantly general surgeon.
Hippolyte Morestin
Although not strictly a Central Powers surgeon, the French Surgeon Hippolyte Morestin was an intriguing character who may have attained greater recognition had he lived longer. Originally a maxillofacial surgeon, he published 634 articles during his short life.[12,13] He is under-recognized, despite being famous during his own time for his maverick techniques and his fiery temperament. Thanks to his fiery temperament he was reputedly not well liked by many of his colleagues.[14] One of his more notable feats was the inspiration of Sir Harold Gillies, who travelled to Paris in June 1915 to watch Morestin operate. The jaw reconstruction he witnessed there ignited an enthusiasm in Gillies which led to his subsequent endeavors.[15] At the start of World War One, Morestin was 44 and working in Paris, primarily in the St-Louis Hospital.[16] His lack of interests outside of work may have contributed to his rapid oscillation in mood, which was clearly documented by Gillies on his occasion of meeting him; “In the space of a single moment he can display the gentleness of a kitten and the savagery of a tiger.”[12] Unfortunately, his early deathdue totheinfluenza pandemicof 1919 meant that his contributions were halted, and he is not as appreciated as he might be. His most telling legacy was the inspiration of others: Gillies, Esser, and his other students who became excellent surgeons in their own right during the interwar period.
Jaques Joseph
Sometimes referred to as “the father of modern aesthetics,” Jaques Joseph was also born in 1865, to a Jewish family in Konigsberg, Prussia.[17] After studying medicine in Berlin, his initial career led him along the path of general practice. Hungering for something more specialized, he commenced orthopaedic training at the Berlin University Clinic; it was at this stage that his first mark was made on the world of plastic surgery. Noticing an unhappy 10-year-old boy with protruding ears, he carefully researched the relevant anatomy and proceeded to set back the child’s ears. Although he gained recognition for this, his supervising Professor Julius Wolff was not pleased and relieved him from his service.[17] After returning to private practice, he was approached by a man with a large nose, who had heard of the child’s operation. Once again he researched, meticulously planned the procedure, and practiced on cadavers prior to conducting his first rhinoplasty in 1898.[5] This led to the development of a burgeoning market within his local Jewish population, and cemented his reputation as an aesthetic facial surgeon. Although the psychological benefits of aesthetic surgery had been propounded prior to this by Tagliacozzi, Joseph’s drive in the face of prevailing opinion was the behavior of a true leader. He coined the term “anti-dysplasia” in an effort to dispel the myth of vanity as the indication for his surgery. At the start of World War One, he was 49, working in Berlin in his private practice. His fierce patriotism led him to increase his work rate and he came to the forefront of reconstructive and aesthetic surgery, being recognized by the Prussian Kaiser Wilheim II himself. In 1916, he began working at the Charité Hospital in Berlin and in 1919 was made professor of Plastic Surgery. Von Gräfe’s work on rhinoplastics was about to be improved upon, around a century after he had held the directorship there. For his efforts during the war, Joseph was decorated with the Iron Cross. Over his life he published much, including his book “Nasenplastik” (Nasal Plastic Surgery) and the ensuing volume “Nasenplastik und sonstige Gesichtsplastik nebst einem Anhang über Mammaplastik” (Nasal Plastic Surgery and other Facial Plastic with Mammoplasty); these volumes remain relevant and show that Joseph was a visionary who stood apart in early rhinoplasty.[18] He died in his home from a myocardial infarct in 1934 at the age of 69 years, and although he had suffered at the hands on the changing German political landscape, he was mercifully spared from the worst of what World War Two held. He was much admired by Erich Lexer, who praised his artistic temperament.
Erich Lexer
Erich Lexer was one of the foremost reconstructive surgeons of the Great War, born in 1867 in Freiberg. As a youngster he was a keen student of the arts—particularly sculpting and modeling. After studying medicine at Wurzburg University, in 1892 at the age of 25, he moved to the Berlin University Clinic where he acted as assistant to Ernst Von Bergman.[19] After leaving Berlin in 1905, he set up in Konigsberg, then Jena in 1911—at both sites he was made a professor of surgery. He also continued to pursue engagements in his hometown of Freiburg. He was prolific in this pre-war period, and was granted the title of Admiral in the German Navy as the transition to war occurred. Much of his work over the latter part of the war was concerned with facial reconstruction, for which he set up a center for plastic surgery in Flanders, close to the Western Front.[5] His patients followed him after the war to his clinics back in Jena and Freiburg, where he continued to manage war wounded. He finally moved to Munich, where he died in 1937 from a myocardial infarct. His character was that of a man living life to its fullest, with a love of fast cars and physical exertion.[5] Like Gillies, he was also a lover of practical jokes, once standing stark naked in the middle of his bedroom to surprise a nursing sister who refused to knock before entering.[20] His history of publications is colored by his reticence in being a coauthor; he preferred to allow his juniors to develop their careers. This almost resulted in the loss of much of his legacy, but one of his mentees later compiled a full bibliography of his works.[21] A cursory glance at the assembled titles here is all that is required for a picture of the breadth of his knowledge. It is from here that we may find his true nature as a developer of surgical techniques, for instance, his use of the total palmar fasciectomy for Dupuytren’s was described by one of his trainees in 1902, and was not published by himself until 1931.[20,22] He did publish several books which have stood the test of time, however—including his popular “Principles and Practice of Surgery,” and “Reconstructive Surgery” shortly after the war.[23,24] He also described the pathogenesis of osteomyelitis for the first time in detail, work which still stands today.[25] His other books include “The Complete Reconstructive Surgery.”[22] His description of one of the earliest iterations of the forehead lift shows his revolutionary approach, along with his description of the nipple–alveolar complex approach to mammaplasty, which was far ahead of its time and was rediscovered many years later [26,27].
Johannes Esser
Johannes Frederick Esser was born in 1877 in the Netherlands. After completing his medical degree, he became itinerant, working as a ship’s doctor before his sister’s studies prompted him to experiment in dentistry. He gained work as a general practitioner with a special interest in dentistry, during which time he became dissatisfied professionally, and began to collect art and cultivate relationships with artists. He was also a keen chess player and became the Dutch chess champion. His surgical studies followed thereafter, permitting him some experience before the start of World War One when he was 37 years of age, roughly 10 years younger than the next youngest Central Pioneer.[14] His studies also came under the auspices of Morestin for a 6-month period in Paris, during which time he observed many revolutionary operations; this granted him an opportunity at the advent of World War One. After his offers to work for the French and British were ignored, Esser began work at the Imperial and Reserve Hospital No. 2 in what is now Brno in the Czech Republic. This led to his appointment as Chief Surgeon; the ensuing experience he gained in traumatology led to the development of many of his lasting techniques. These included his eponymous inlay graft, rotational flaps of the check, and “biological arterial flaps”—which contributed greatly to the pedicled facial flaps which we know today.[8] During this time in Brno, he performed over 700 facial plastic operations alone, which gave him sufficient material to develop his book.[28] His landmark work with the inlay graft was later adopted by Gillies, and he recognized the importance of the vascular supply in particular facial flaps.[28] His description of the bilobed nasal flap in 1918 was an important contribution to facial reconstruction.[29] Following the war, Esser was well recognized, which put him in a good position for his passion of developing plastic surgery as a discrete specialty, to which there was strong resistance from the prevailing body of general surgeons. Reading his papers is strongly recommended; the English from a Dutchman is transposed most beautifully into scientific language, more assertive than one sees in the modern era and with delightful economy of speech. His dislike of politics and its influence on the practice of medicine crystallized his ambitious dream—to establish an independent state of plastic surgery, free from interference. This led him to travel the world with staggering endurance over the post war years, operating from one world city to the next in an effort to procure support—at one stage even purchasing a French castle. Unfortunately, no country appeared completely willing to engage with Esser on this, and some element of governmental interference was always imposed. This dream followed him to America shortly prior to World War Two, where he upheld it over the war until his death in 1946 from cardiologic complications of the rheumatic fever that he had contracted as a child. A most comprehensive and detailed review of Esser’s life and influences has been documented by Haeseker in his 1983 publication “Dr. J.F.S. Esser and His Influence on the Development of Plastic and Reconstructive Surgery [30]”.
August Lindemann and Christian Bruhn
Lindemann’s (1880–1970) exploits are not well recorded in the English language, but there are somedetails thatcan begleaned from exploration of German texts. As maxillofacial surgeons operating before, during, and after World War One, he and his mentor Professor Christian Bruhn’s work foreshadowed much of the facial reconstruction that took place throughout the rest of Germany and in Britain. Indeed, Gillies mentioned him as a continuing inspiration during his work at the Queen’s Hospital. The jaw reconstruction facility established in Dusseldorf by the early titan of maxillofacial surgery Bruhn during World War One permitted the development of such techniques as an extraoral approach to the mandibular ramus, iliac crest bone grafting, and mandibular reconstruction.[31] Lindemann published on these after the war, continuing to provide literary contributions to his field.[32,33] He was appointed professor of Oral and Maxillofacial Surgery in Dusseldorf in 1935, and worked until his retirement in 1950 [31].
Vladimir Filatov
Vladimir Filatov (1874–1956) is worthy of mention here; although he was of the Allied powers and not particularly prolific as awar surgeon, heis the original architectof the tubed pedicle flap in 1917,[34] following Snydacker’s description of the pedicle flap.[35] Primeur was hotly disputed at its inception between Gillies and Aymard; with Gillies later affirming that Filatov was the originator, but that the idea had occurred to him independently the same year.[36,37,38,39] It was used extensively and in different areas in the following years by both Hugo Ganzer and Gillies, and was a hallmark procedure of reconstructive surgery of the time and endures to this day, for example, in groin flaps for hand reconstruction. It also has a role in less developed countries where free flaps are not feasible [40].
Maxillofacial Surgeons
The impact of maxillofacial surgery techniques on the fledgling field of plastic surgery cannot be overstated. We have discussed Bruhn’s and Lindemann’s influences, but there are several recurring names arising from the literature reviewed who should be included.
The dental surgeon Hugo Ganzer was something of an unsung hero during this period; due to his lack of a formal medical degree in his early career, ithas been opined that he was at a political disadvantage.[41] Qualifying in dentistry in 1900, he was given the responsibility of a jaw reconstruction service in Berlin in 1915, at the age of 36 years. During his time there, his contributions included description of the tubed pedicle flap at the same time as Filatov,[40] and it may well be that he was the originator of the technique. His use of the nasolabial flap also predated many descriptions, and he was a clear descriptor of many of the early techniques in oculoplastics [41].
In contrast to Ganzer, Hans Pichler was a staunch advocate of having a medical background for a career in maxillofacial surgery. Having initially studied medicine, his severe reaction to carbolic acid during surgical training prompted him to study dentistry. He developed an impressive academic portfolio of 125 articles and was a keen author, writing “Surgery of the Mouth and Jaws” and establishing the use of integrated prosthetics for jaw reconstruction. His work during the Great War in the Dental Institute of the University of Vienna met with great success, and his dexterity became renowned.[42] Famous for his care of Sigmund Freud’s oral cancer after the war, his operations allowed Freud 16 years of life with cancer before he eventually succumbed [43].
George Axhausen was a German maxillofacial surgeon, qualifying in Berlin in 1901. He was 32 years old when he started work at the Charité Hospital in 1909, and is likely to have worked closely with Joseph over this period. His work in orthognathic surgery during the Great War was the foundation for many important techniques and principles, including the use of the bone grafts and the first description of avascular (aseptic from his description) necrosis of the epiphysis.[31] His eponymous operation for cleft palate repair was a milestone within the field.
Further Discussion
During World War One, there was a notable lag in the understanding of the war wounded by the civilian population regarding the psychological issues that presented as a result of their experiences and injuries. Even in World War Two, the RAF pilots who were unable to fly as a result of psychological stresses were referred to as “Lacking Moral Fiber,” a phrase still used in the United Kingdom to this day.[44] This may have increased the appetite for reconstructive aesthetic surgery in the era, acting as a further catalyst for the development of plastic surgery in an effort to restore physical normality.
The contrast between the surgical backgrounds of each side in the war suggests that plastic surgery may have been more established in Germany than in Britain prior to the war, judging by the greater number of influential surgeons who were sympathetic to the discipline. In comparison, Britain centered much of her activity around the drive and focus of a single man. The multitude of dedicated centers for plastic surgery developed by the Central Powers demonstrates this, and these are likely to have been facilitated by the presence of those preliminary surgeons such as Dieffenbach and Langenbeck.
None of the pioneers we have described were active surgically during World War Two. However, their younger apprentices during World War One would have been senior surgeons during World War Two. It is difficult to track down German surgeons within the Nazi regime in enough detail to ascertain what their original training may have been; those pages of the history books have been obscured. The Charité Hospital itself—the spiritual home of German Plastic Surgery—was also a victim of World War Two, with an exodus of most of its senior surgeons and its eventual destruction by bombing.
The literature relevant to this study incorporated archaic foreign language texts, which may not have been included in the original MEDLINE search. Accordingly, much of the source material is from third-party bibliographies, meaning that full capture of the subjects’ less well known literary accomplishments may not have been achieved.
Conclusion
We have discussed some of the World War One surgeons of the Central Powers. It is evident from this brief examination of these individuals that their work in the technical and academic spheres has contributed a great amount to the practice of plastic and reconstructive surgery. We have identified the major developments that they have made and their most famous works, in addition to displaying their relative ages and locations during the war. We have also seen that although Gillies has been rightly lauded for his career, he adopted many techniques from those described earlier—including the Esser inlay, Filatov’s tubed pedicle, and Morestin’s local flaps. It is important that we do not forget that no one person can begiven credit for the development of functional aesthetic surgery, but that a group of individuals from a range of specialties devised the techniques, the tools, and the knowledge to found a school dedicated to the restoration of anatomy and psyche.
Acknowledgments
We would like to thank Surg Lt Cdr Joanne Laird RN for her artistic contribution shown in Figure 2.
References
- Shiffman, M.A.; Di Giuseppe, A. Cosmetic Surgery: Art and Techniques; Springer: Berlin/Heidelberg, Germany; New York, NY, USA, 2013. [Google Scholar]
- Bankoff, G. The Story of Surgery; A. Barker: London, UK, 1947. [Google Scholar]
- Killian, H.; Freidrich, J. Dieffenbach. Neue Deutsche Biographie 1957, 3, 641–643. [Google Scholar]
- Dieffenbach, J. Die operative Chirurgie.—Leipzig, F. A. Brockhaus 1845–1848. Vol. 1 of Die Operative Chirurgie; F.Brockhaus: Munich, Germany, 1845. [Google Scholar]
- Tolhurst, D. Pioneers in Plastic Surgery; Springer International Publishing: Basel, Switzerland, 2015. [Google Scholar]
- Warren, M. Obituary: Sir HAROLD GILLIES, C.B.E., F.R.C.S. Hon.F.R. A.C.S., Hon.F.A.C.S. BMJ 1960, 2, 866–867. [Google Scholar]
- Gillies, H. Plastic Surgery of the Face; Oxford University Press: Oxford, UK, 1920. [Google Scholar]
- Esser, J.F.S. Biological- or Artery Flaps of the Face: With 420 Plates and a List of the Author’s Publications; Institut Esser de Chirurgie Structive: Monaco, 1934. [Google Scholar]
- Lanz, O. Die Transplantation bertreffend. Zentralbl Chir 1908, 35, xx. [Google Scholar]
- Clodius, L. The classic reprint. Die Transplantation Betreffend by Prof. Otto Lanz. Plast Reconstr Surg 1972, 50, 395–397. [Google Scholar] [PubMed]
- Craig, S.C.; Smith, D.C. Glimpsing Modernity: Military Medicine in World War I; Cambridge Scholars Publishing: Cambridge, UK, 2016. [Google Scholar]
- Rogers, B.O. Hippolyte Morestin (1869–1919). Part I: A brief biography. Aesthetic Plast Surg 1982, 6, 141–147. [Google Scholar] [CrossRef]
- Rogers, B.O. Hippolyte Morestin (1968–1919). Part 1: A brief biography. Plast Reconstr Surg 1983, 72, 932. [Google Scholar]
- Haeseker, B. Johannes Fredericus Samuel Esser: Innovative “structive” surgeon (1877–1946). Plast Reconstr Surg 1986, 77, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Gillies, H. Methods of closing the maxillary defect with new tissue. Acta Chir Orthop Traumatol Cech 1957, 24, 440–442. (In Czech) [Google Scholar]
- Lalardrie, J.P. Hippolyte Morestin 1869–1918. Br J Plast Surg 1972, 25, 39–41. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, S. Jacques Joseph: Father of modern aesthetic surgery. Indian J Plast Surg 2008, 41, S3–S8. [Google Scholar] [CrossRef] [PubMed]
- Joseph, J. Nasenplastik und Sonstige Gesichtsplastik Nebst Einem Anhang Über Mammaplastik; Kabitizsch: Liepzig, Germany, 1928. [Google Scholar]
- Hinderer, U.T.; del Rio, J.L. Erich Lexer’s mammaplasty. Aesthetic Plast Surg 1992, 16, 101–107. [Google Scholar] [CrossRef] [PubMed]
- May, H. Erich Lexer, A Biographical Sketch. Plast Reconstr Surg 1962, 29, 141–152. [Google Scholar] [CrossRef]
- May, H. The bibliography of Erich LEXER’s scientific work. Plast Reconstr Surg Transplant Bull 1962, 30, 670–675. [Google Scholar] [CrossRef]
- Lexer, E. Die Gesamte Wiederherstellungschirurgie; J.A. Barth: Leipzig, Germany, 1931. [Google Scholar]
- Lexer, E. Allgemeinen; Chirurgie. F. Enke: Stuttgart, Germany, 1905. [Google Scholar]
- Lexer, E. Wiederherstellungschirurgie; J.A. Barth: Leipzig, Germany, 1918. [Google Scholar]
- Lexer, E. Die Ätiologie Und die Mikroorganismen der Akuten Osteomyelitis; Chirurgie: Leipzig, Germany, 1897. [Google Scholar]
- Gesichtsplastik, L.E. Arch Facial Plast Surg 1910, 92, 749.
- Lexer, E. Correccion de los pechos pendulos (Mastoptose) por medio de la implantacion de grasa. San Sebastian Guipuzcoa Medica 1921, 63, 213. [Google Scholar]
- Esser, J.F. Studies in plastic surgery of the face: I. Use of skin from the neck to replace face defects. II. Plastic operations about the mouth. III. The epidermic inlay. Ann Surg 1917, 65, 297–315. [Google Scholar] [CrossRef]
- Esser, J.F. Gestielte lokale Nasenplastik mit zweizipligem Lappen, Deckung des Sekundaren Defektes vom ersten Zipfel durch den Zweiten. Deutsche Zeitschrilt fiir. Chirurgie 1918, 143, 385–390. [Google Scholar] [CrossRef]
- Haeseker, B. Dr. J. F. S. Esser and His Influence on the Development of Plastic and Reconstructive Surgery; Erasmus University Rotterdam: Rotterdam, The Netherlands, 1983. [Google Scholar]
- Naini, F.G.D. Orthognathic Surgery: Principles, Planning and Practice; Wiley-Blackwell: Hoboken, NJ, USA, 2017. [Google Scholar]
- Lindemann, A. Die Wehrchirurgie des Gesichtsscha dels—Nachbehandlung und Nachoperation. Dtsch Z Zahn Mund Kieferheilk 1936, 3, 105. [Google Scholar]
- Lindemann, A.H.H. Die Kieferosteotomie. Chirurg 1938, 10, 745–770. [Google Scholar]
- Filatov, V. Plastic procedure using a round pedicle. Vestn Oftalmol 1917, 34, 128. [Google Scholar] [CrossRef]
- Snydacker, E. Lidplastik mit gestieltem Lappen von Halse. Klin Monatsbl Augenhlkd 1907, 45, 71–76. [Google Scholar]
- Aymard, J.L. Nasal reconstruction. Lancet 1917, 190, 888–892. [Google Scholar] [CrossRef]
- Aymard, J. The tubed pedicle in plastic surgery. Lancet 1920, 196, 270. [Google Scholar] [CrossRef]
- Gillies, H.D. The tubed pedicle in plastic surgery. Lancet 1920, 196, 320. [Google Scholar] [CrossRef]
- Gillies, H.D. Experiences with tubed pedicle flaps. Surg Gynecol Obstet 1935, 60, 291. [Google Scholar]
- Marck, K.W.; Palyvoda, R.; Bamji, A.; van Wingerden, J.J. The tubed pedicle flap centennial: Its concept, origin, rise and fall. Eur J Plast Surg 2017, 40, 473–478. [Google Scholar] [CrossRef]
- Rittersma, J. The dentist as a plastic surgeon (Hugo Ganzer 1879–1960). J Craniomaxillofac Surg 1988, 16, 51–54. [Google Scholar] [CrossRef]
- Riaud, X. Treatment of Sigmund Freud’s Maxillary Jawbone Cancer by Hans Pichler and Varaztad Kazanjian (1856–1939). Trauma Treatment 2015, 4, 236. [Google Scholar]
- Romm, S.; Luce, E.A. Hans Pichler: Oral surgeon to Sigmund Freud. Oral Surg Oral Med Oral Pathol 1984, 57, 31–32. [Google Scholar] [CrossRef]
- Noakes, L. British Cultural Memory and the Second World War; Bloomsbury: London, UK, 2014. [Google Scholar]
© 2018 by the author. The Author(s) 2018.