Analysis of the Changing Patterns of Midface Fractures Using 3D Computed Tomography: An Observational Study
Abstract
:Subjects and Method
- Similar to Le Fort fracture patterns.
- Combination of Le Fort fracture patterns.
- Deviation from Le Fort fracture patterns.
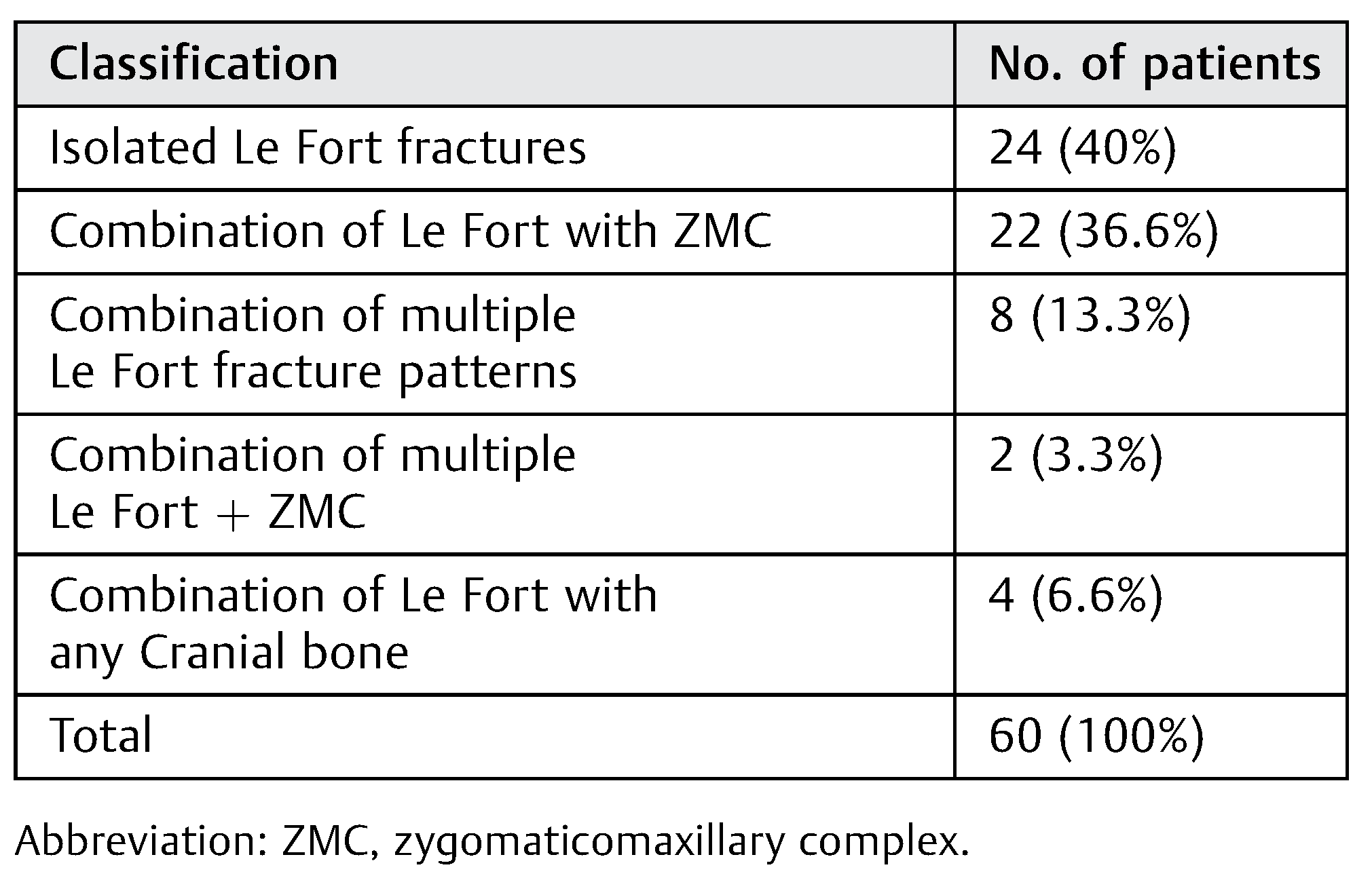
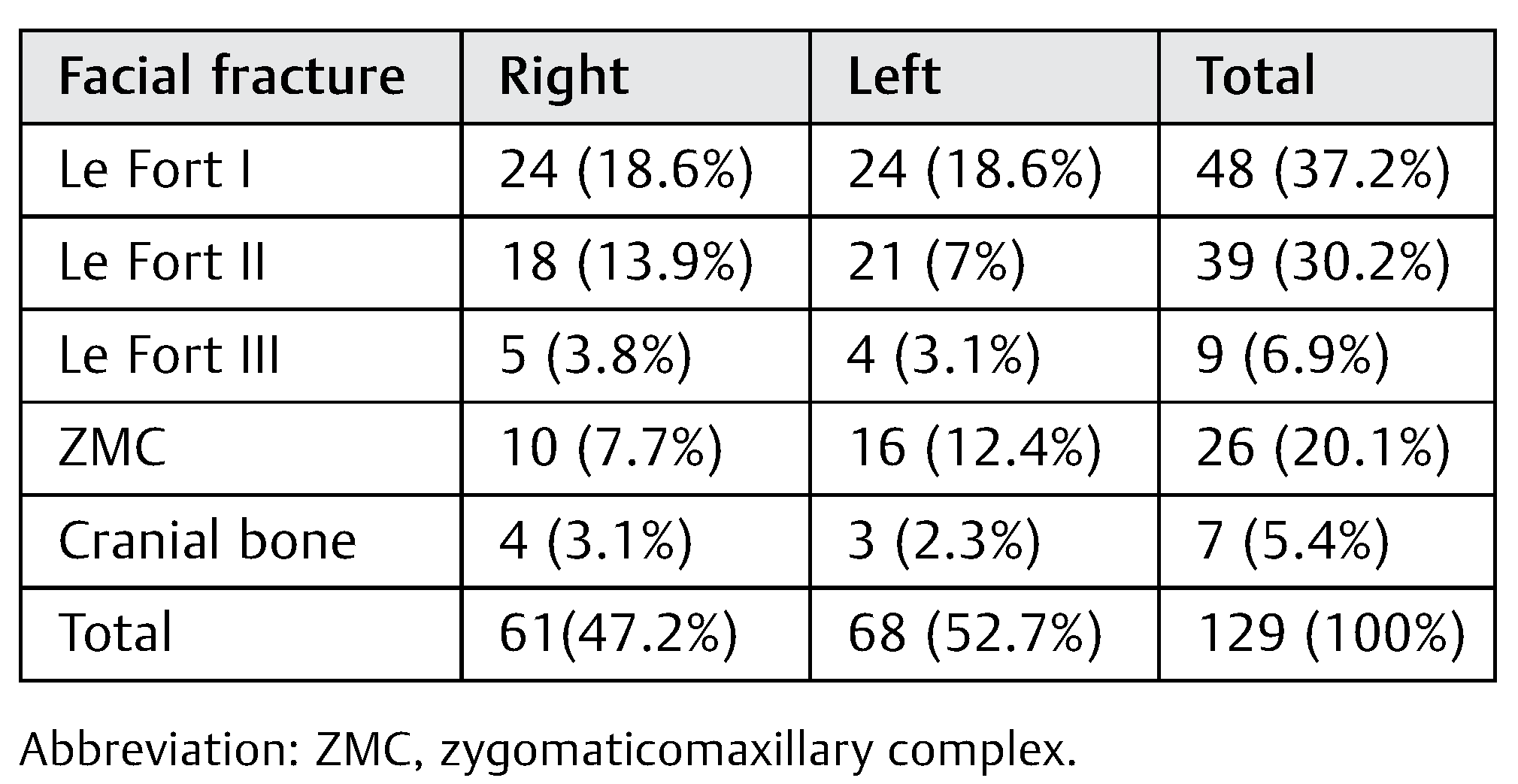
Results
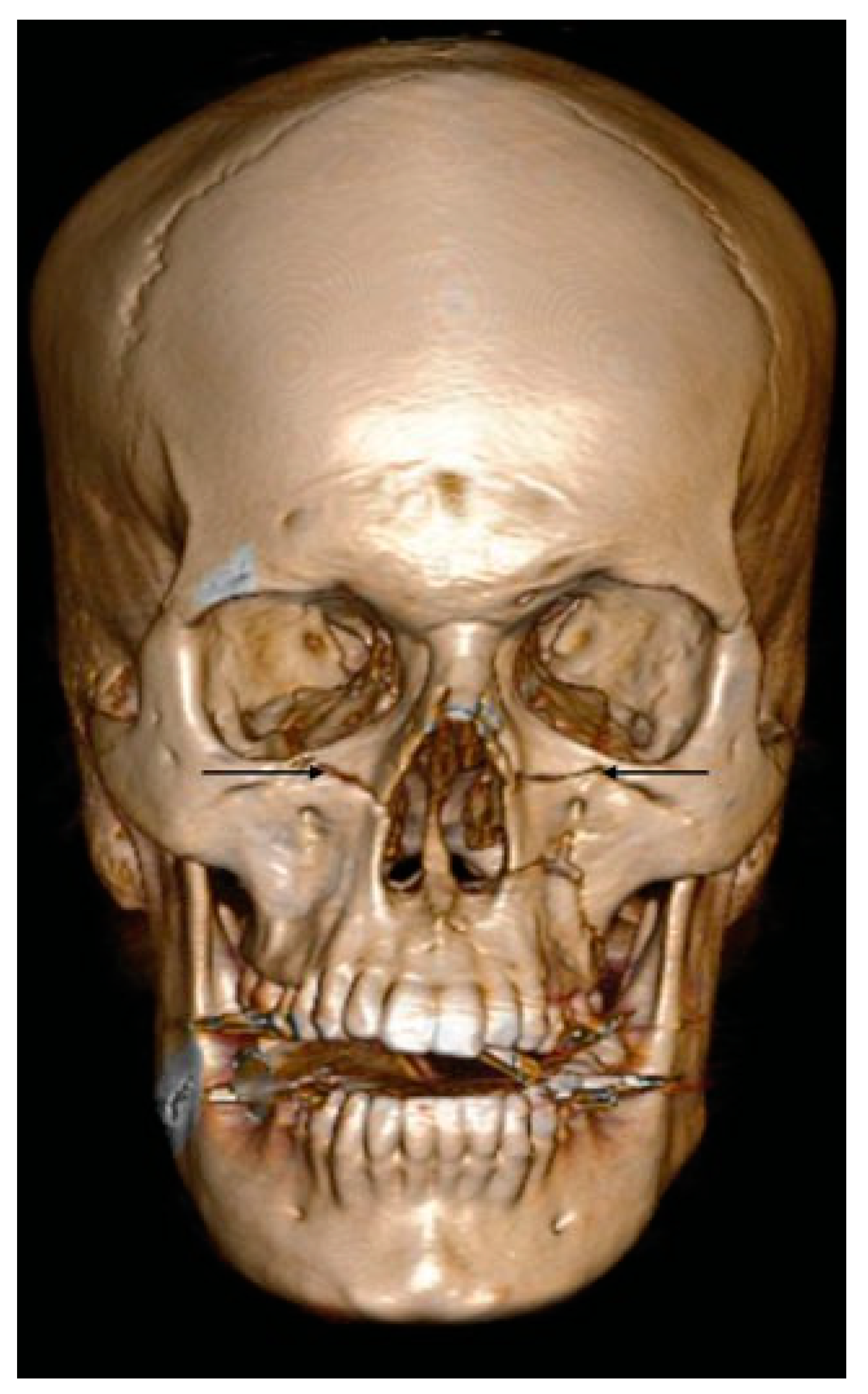
- D1:
- Additional line extending from the pyriform aperture to the infraorbital rim of the same side (60%).
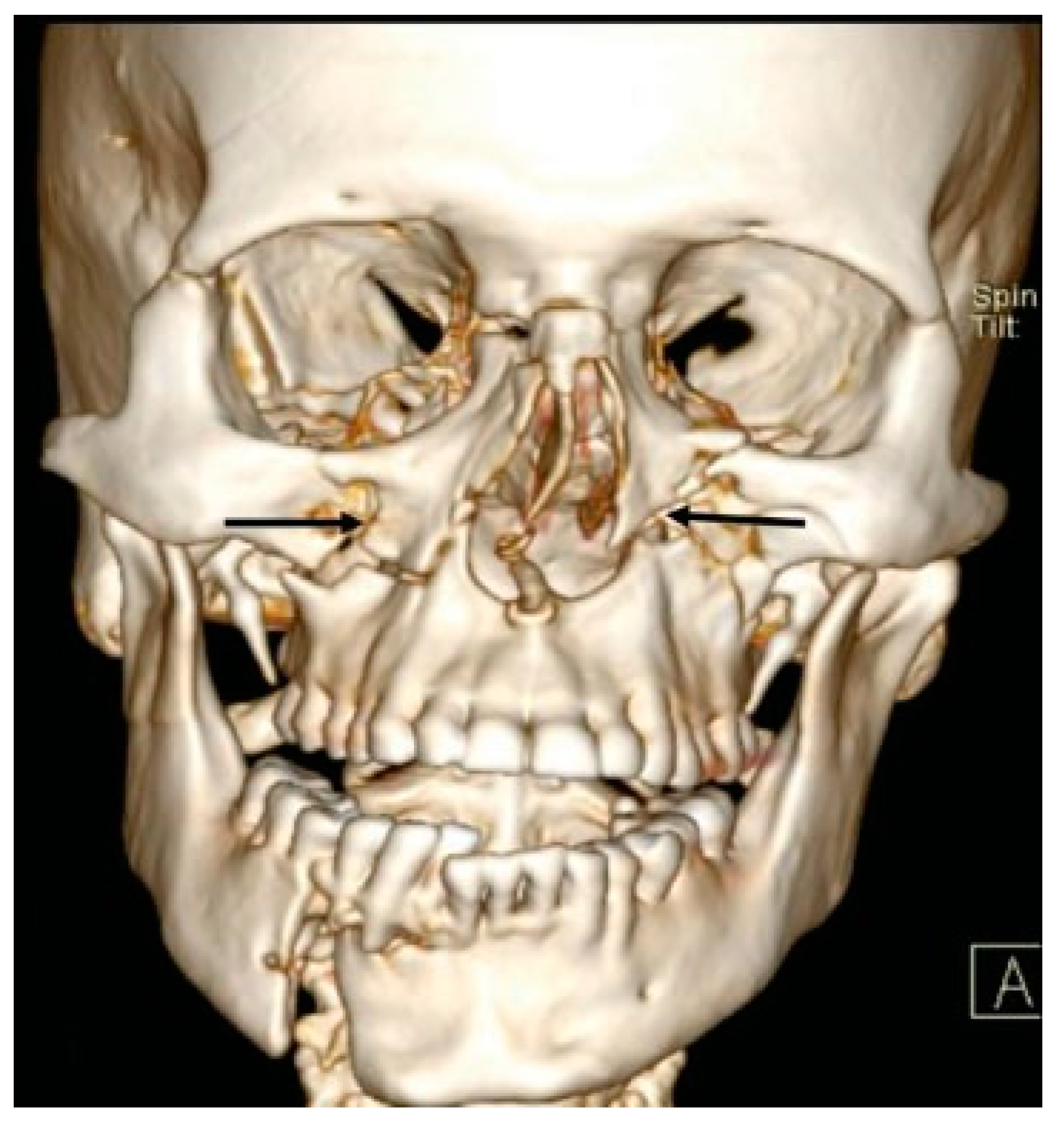
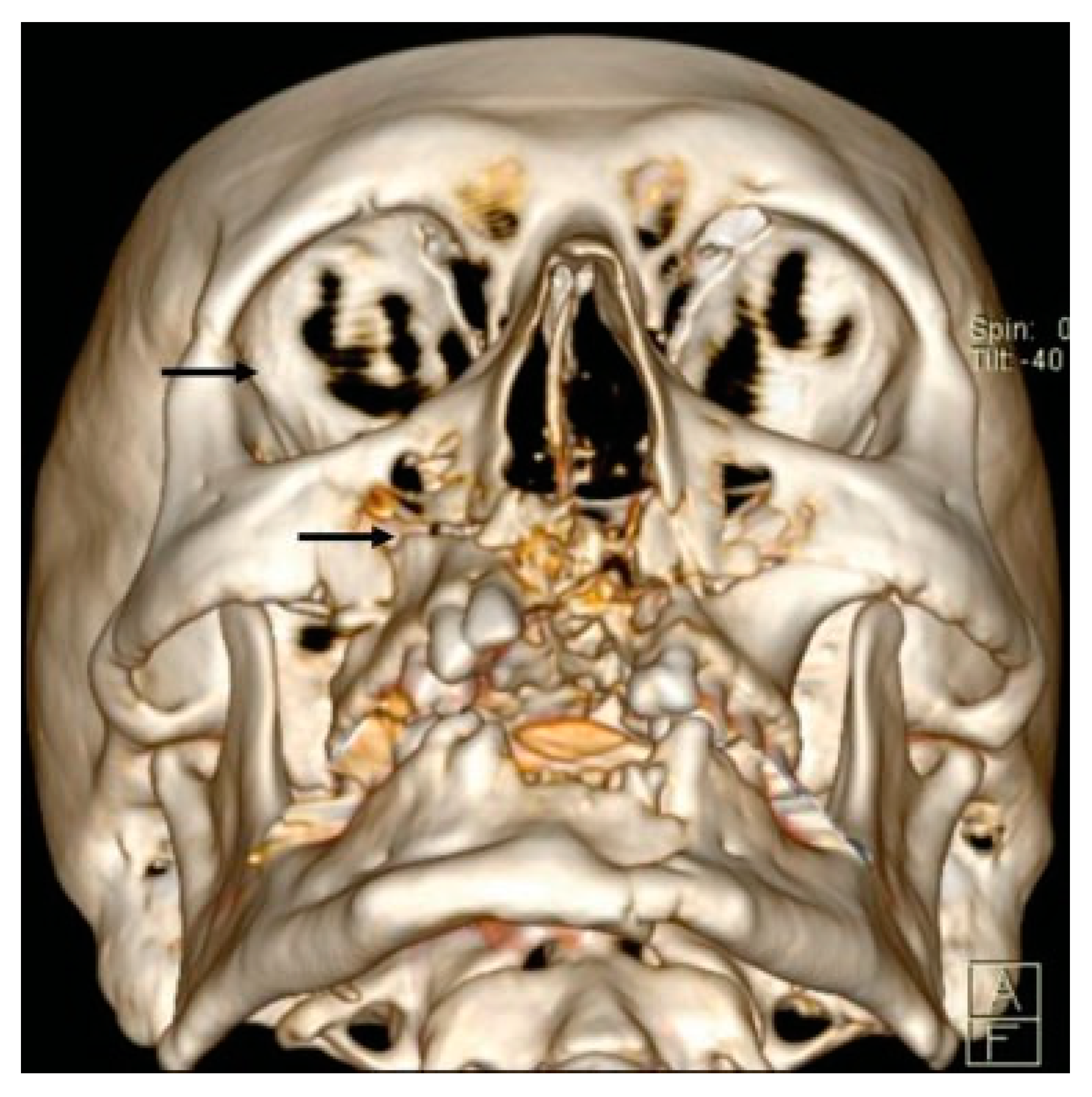
- D2:
- Additional line extending from the infraorbital rim to the Le Fort fracture line.
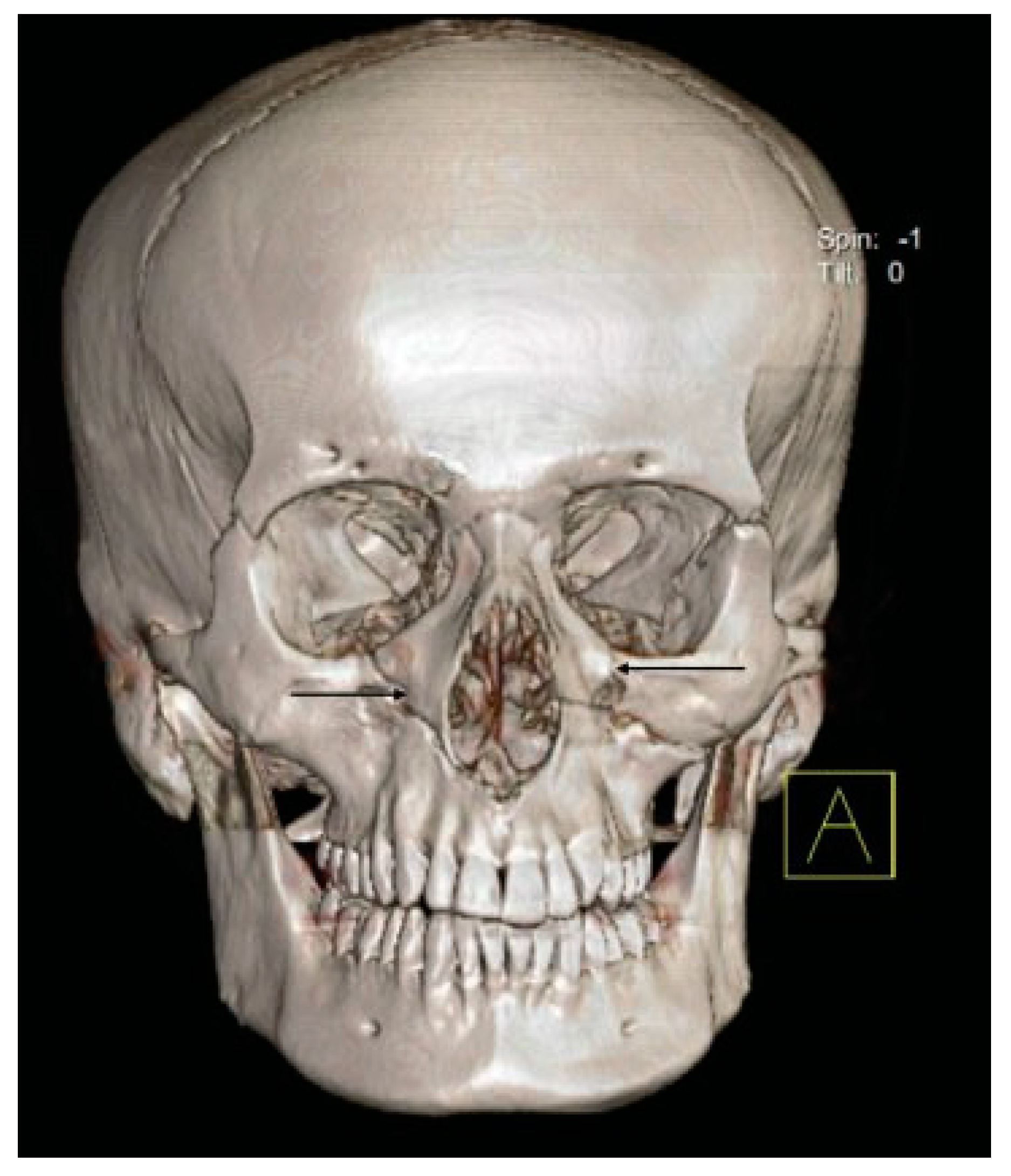
- D3:
- Additional line extending from the pyriform aperture to the lateral wall of orbit, without breaking the infraorbital rim of the same side (5.4%).
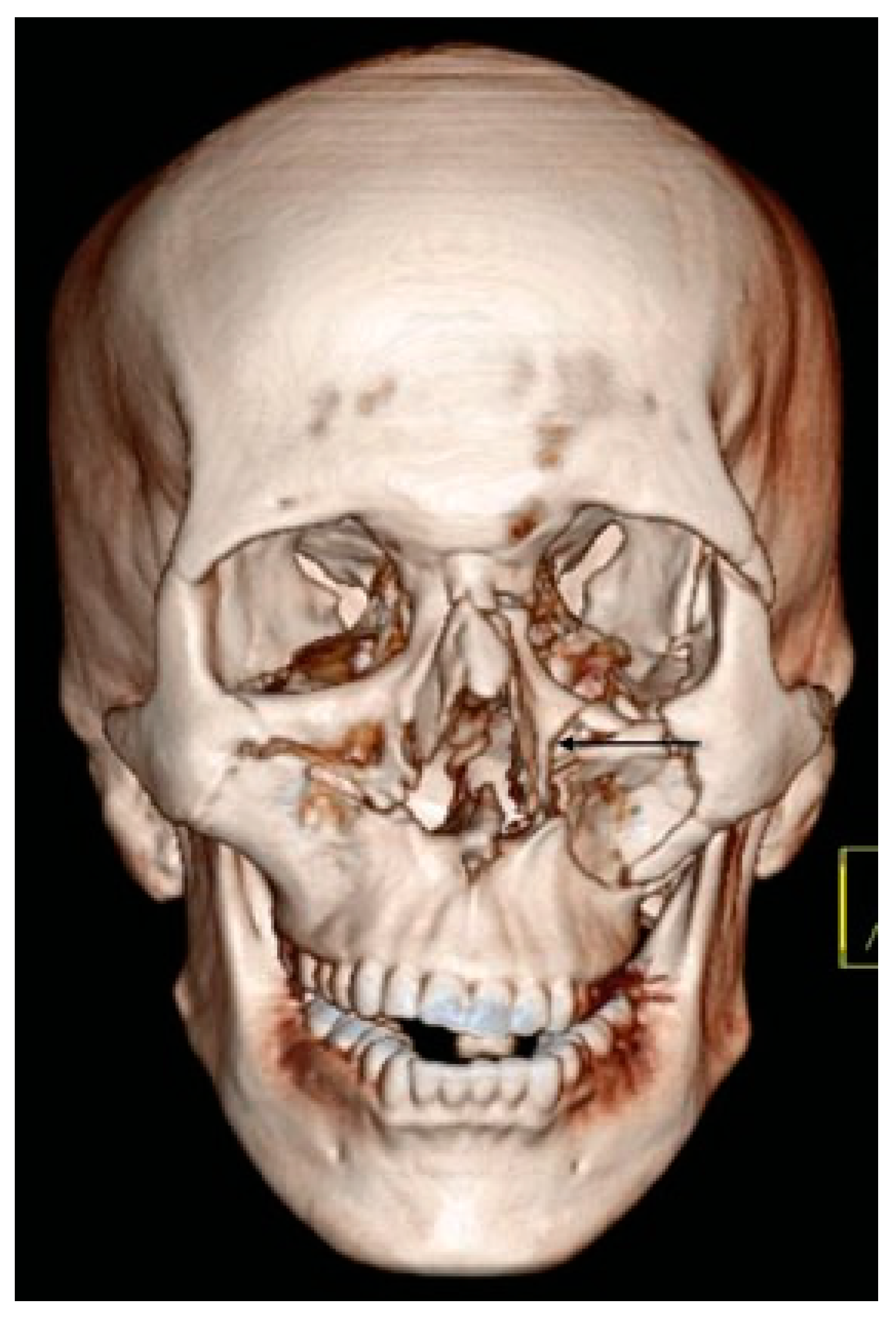
- D4:
- Additional line extending from the infraorbital rim through the canine fossa to terminate as a fractured dentoalveolar segment of the same side, involving the fractured segment (10.9%).
- D5:
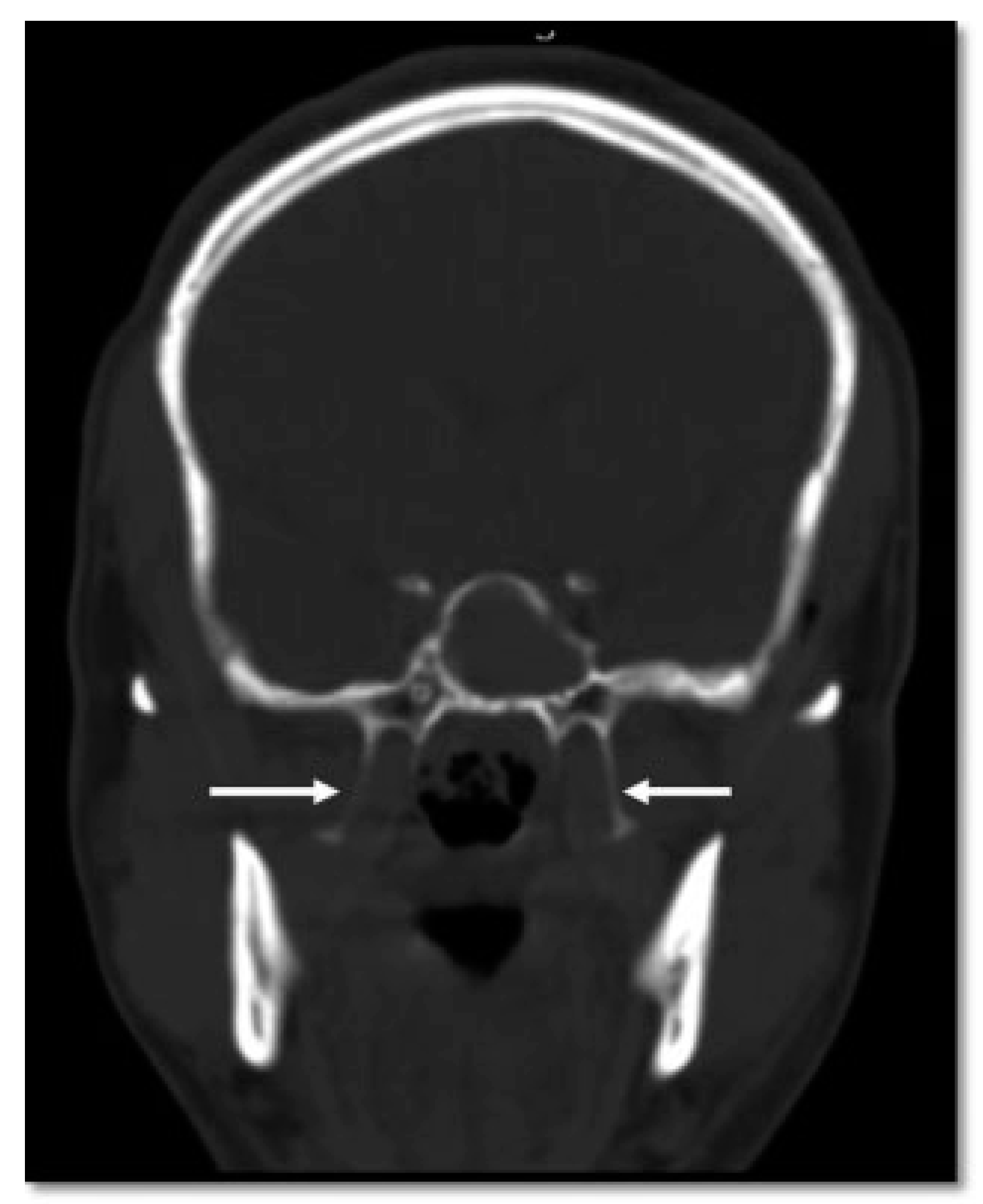
- Pterygoid plates are not fractured (23.6%).
Discussion
Case Discussions
- D1: Additional Line Extending from the Pyriform Aperture to the Infraorbital Rim of the Same Side (34.5%)
- D2: Additional Line Extending from Infraorbital Rim to the Le Fort Fracture Line (25.4%)
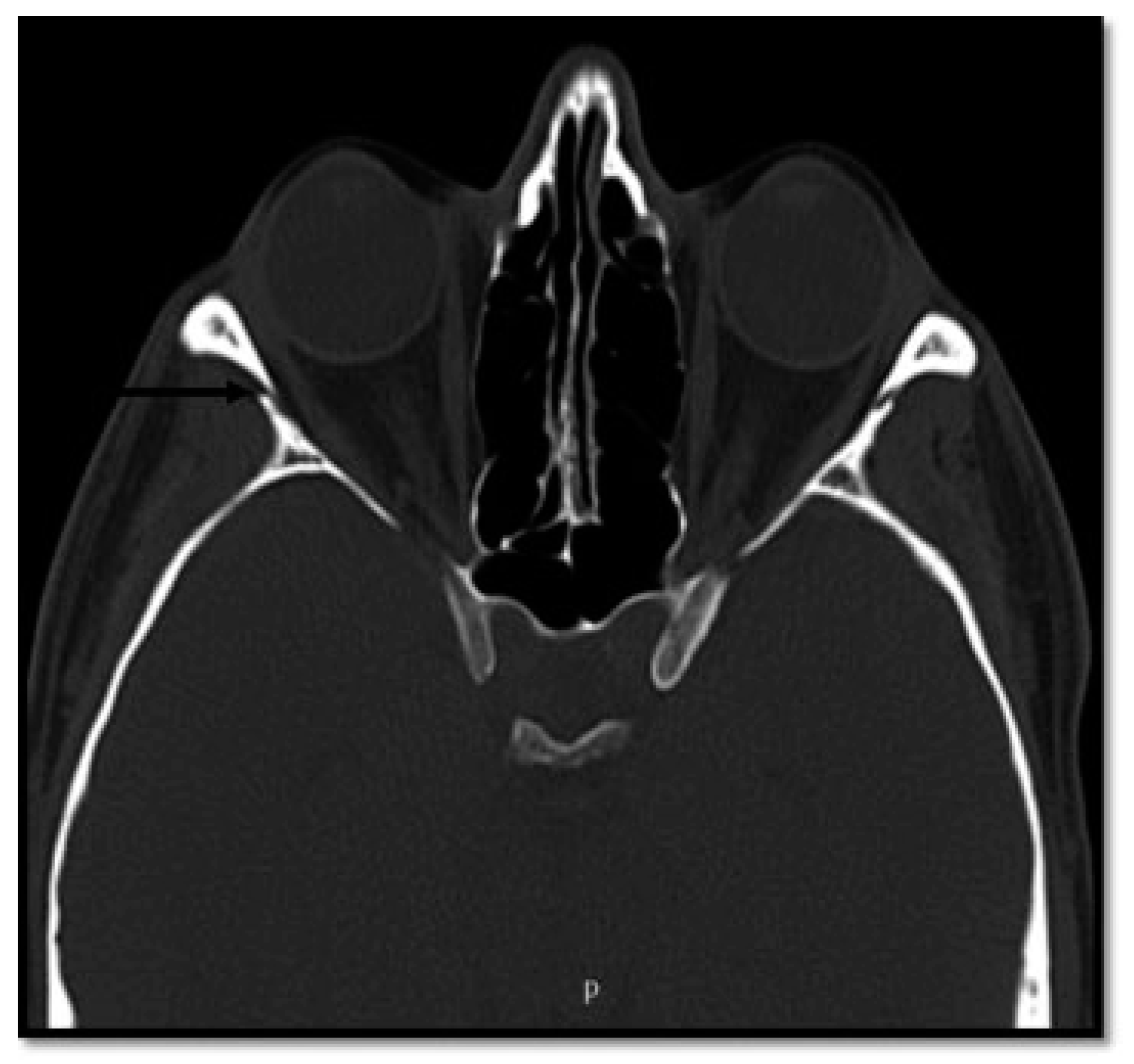
- D3: Additional Line Extending from Pyriform Fossa to Lateral Wall of Orbit, without the Fracture of the Infraorbital Rim of the Same Side (5.4%)
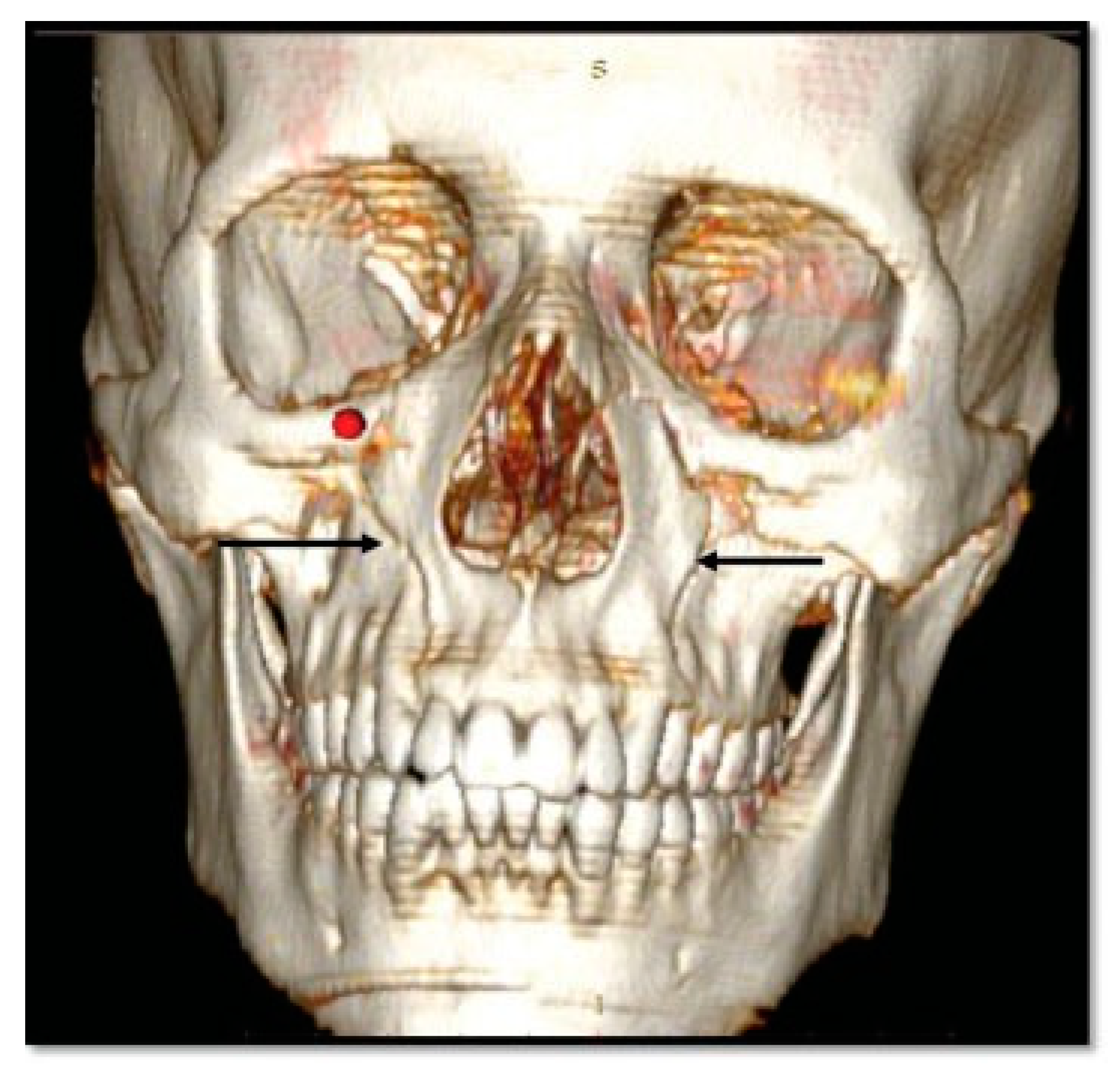
- D4: Additional Line Running from the Infraorbital Rim through the Canine Fossa to Terminate as a Fractured Dentoalveolar Segment of the Same Side (10.9%)
- D5: Pterygoid Plates Are Not Fractured (23.6%)
Conclusion
Funding
References
- Gartshore, L. A brief account of the life of René Le Fort. Br J Oral Maxillofac Surg 2010, 48, 173–175. [Google Scholar] [CrossRef] [PubMed]
- Noffze, M.J.; Tubbs, R.S. René Le Fort 1869-1951. Clin Anat 2011, 24, 278–281. [Google Scholar] [CrossRef] [PubMed]
- Rowe, N.L.; Williams, J.L.; Hobbs, J.A. Williams, J.L., Ed.; Etiology of injury. In Rowe and Williams Maxillofacial Injuries, 2nd ed.; Churchill Livingstone: New York, NY, USA, 1994; Volume 1, pp. 34–36. [Google Scholar]
- Simpson, D.A.; McLean, A.J. Mechanisms of injury. In Craniomaxillofacial Trauma; David, D.J., Simpson, D.A., Eds.; Churchill Livingstone: New York, NY, USA, 1995; Volume 101. [Google Scholar]
- Marciani, R.D.; Gonty, A.A. Principles of management of complex craniofacial trauma. J Oral Maxillofac Surg 1993, 51, 535–542. [Google Scholar] [CrossRef]
- Doi, Y.; Tomitsuka, S.; Asano, K.; Sakai, E.; Sasaki, T.; Imai, Y. A study on the classification of the maxillary fractures—new proposal for revised Le Fort classification. Int J Oral Maxillofac Surg 2005, 34, 159–160. [Google Scholar] [CrossRef]
- Zhang, Y.; Gu, X.M.; Cai, Y.J.; Duan, D.H. [A revised scheme for LeFort classification of upper jaw fractures]. Zhonghua Kou Qiang Yi Xue Za Zhi 2005, 40, 134–136. [Google Scholar]
- Roccia, F.; Servadio, F.; Gerbino, G. Maxillofacial fractures following airbag deployment. J Craniomaxillofac Surg 1999, 27, 335–338. [Google Scholar] [CrossRef]
- Kadkhodaie, M.H. Three-year review of facial fractures at a teaching hospital in northern Iran. Br J Oral Maxillofac Surg 2006, 44, 229–231. [Google Scholar] [CrossRef]
- Al Ahmed, H.E.; Jaber, M.A.; Abu Fanas, S.H.; Karas, M. The pattern of maxillofacial fractures in Sharjah, United Arab Emirates: a review of 230 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004, 98, 166–170. [Google Scholar] [CrossRef]
- Patil, R.S.; Kale, T.P.; Kotrashetti, S.M.; Baliga, S.D.; Prabhu, N.; Issrani, R. Assessment of changing patterns of Le fort fracture lines using computed tomography scan: an observational study. Acta Odontol Scand 2014, 72, 984–988. [Google Scholar] [CrossRef]
- Hächl, O.; Tuli, T.; Schwabegger, A.; Gassner, R. Maxillofacial trauma due to work-related accidents. Int J Oral Maxillofac Surg 2002, 31, 90–93. [Google Scholar] [CrossRef]
- Maladière, E.; Bado, F.; Meningaud, J.P.; Guilbert, F.; Bertrand, J.C. Aetiology and incidence of facial fractures sustained during sports: a prospective study of 140 patients. Int J Oral Maxillofac Surg 2001, 30, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Ajike, S.O.; Adebayo, E.T.; Amanyiewe, E.U.; Ononiwu, C.N. An epidemiologic survey maxillofacial fractures and concomitant injuries in Kaduna, Nigeria. Niger J Surg Res 2005, 7, 251–255. [Google Scholar] [CrossRef]
- Subhashraj, K.; Nandakumar, N.; Ravindran, C. Review of maxillofacial injuries in Chennai, India: a study of 2748 cases. Br J Oral Maxillofac Surg 2007, 45, 637–639. [Google Scholar] [CrossRef] [PubMed]
- Toivari, M.; Suominen, A.L.; Lindqvist, C.; Thorén, H. Among patients with facial fractures, geriatric patients have an increased risk for associated injuries. J Oral Maxillofac Surg 2016, 74, 1403–1409. [Google Scholar] [CrossRef]
- Olasoji, H.O.; Tahir, A.; Arotiba, G.T. Changing picture of facial fractures in northern Nigeria. Br J Oral Maxillofac Surg 2002, 40, 140–143. [Google Scholar] [CrossRef]
- Cook, L.J.; Kerns, T.; Burch, C.; et al. Motorcycle Helmet Use and Head and Facial Injuries: Crash Outcomes in CODES-Linked Data; National Highway Traffic Safety Administration: Washington, DC, USA, 2009. [Google Scholar]
- Yu, W.Y.; Chen, C.Y.; Chiu, W.T.; Lin, M.R. Effectiveness of different types of motorcycle helmets and effects of their improper use on head injuries. Int J Epidemiol 2011, 40, 794–803. [Google Scholar] [CrossRef]
- Tsai, Y.J.; Wang, J.D.; Huang, W.F. Case-control study of the effectiveness of different types of helmets for the prevention of head injuries among motorcycle riders in Taipei, Taiwan. Am J Epidemiol 1995, 142, 974–981. [Google Scholar] [CrossRef]
- Hoeffner, E.G.; Quint, D.J.; Peterson, B.; Rosenthal, E.; Goodsitt, M. Development of a protocol for coronal reconstruction of the maxillofacial region from axial helical CT data. Br J Radiol 2001, 74, 323–327. [Google Scholar] [CrossRef]
- Hopper, R.A.; Salemy, S.; Sze, R.W. Diagnosis of midface fractures with CT: what the surgeon needs to know. Radiographics 2006, 26, 783–793. [Google Scholar] [CrossRef]
- Daffner, R.H. Imaging of facial trauma. Semin Musculoskelet Radiol 1998, 2, 65–82. [Google Scholar] [CrossRef]
- Bernhardt, T.M.; Rapp-Bernhardt, U.; Fessel, A.; Ludwig, K.; Reichel, G. Grote RCTscanning of the paranasal sinuses: axial helical CTwith reconstruction in the coronal direction versus coronal helical, CT. Br J Radiol 1998, 71, 846–851. [Google Scholar] [CrossRef] [PubMed]
- Reuben, A.D.; Watt-Smith, S.R.; Dobson, D.; Golding, S.J. A comparative study of evaluation of radiographs, CT and 3D reformatted CT in facial trauma: what is the role of 3D? Br J Radiol 2005, 78, 198–201. [Google Scholar] [CrossRef] [PubMed]
- Shankar, A.N.; Shankar, V.N.; Hegde, N.; Prasad, R. The pattern of the maxillofacial fractures: a multicentre retrospective study. J Craniomaxillofac Surg 2012, 40, 1–5. [Google Scholar]
- Salentijn, E.G.; van den Bergh, B.; Forouzanfar, T. A ten-year analysis of midfacial fractures. J Craniomaxillofac Surg 2012, 40, 51–54. [Google Scholar] [CrossRef]






 |
 |
 |
 |
© 2017 by the author. The Author(s) 2017.
Share and Cite
Satish, P.; Prasad, K.; Lalitha, R.M.; Ranganath, K.; Sagar, P. Analysis of the Changing Patterns of Midface Fractures Using 3D Computed Tomography: An Observational Study. Craniomaxillofac. Trauma Reconstr. 2018, 11, 265-272. https://doi.org/10.1055/s-0037-1606250
Satish P, Prasad K, Lalitha RM, Ranganath K, Sagar P. Analysis of the Changing Patterns of Midface Fractures Using 3D Computed Tomography: An Observational Study. Craniomaxillofacial Trauma & Reconstruction. 2018; 11(4):265-272. https://doi.org/10.1055/s-0037-1606250
Chicago/Turabian StyleSatish, Preeti, Kavitha Prasad, R. M. Lalitha, Krishnappa Ranganath, and Parimala Sagar. 2018. "Analysis of the Changing Patterns of Midface Fractures Using 3D Computed Tomography: An Observational Study" Craniomaxillofacial Trauma & Reconstruction 11, no. 4: 265-272. https://doi.org/10.1055/s-0037-1606250
APA StyleSatish, P., Prasad, K., Lalitha, R. M., Ranganath, K., & Sagar, P. (2018). Analysis of the Changing Patterns of Midface Fractures Using 3D Computed Tomography: An Observational Study. Craniomaxillofacial Trauma & Reconstruction, 11(4), 265-272. https://doi.org/10.1055/s-0037-1606250



