The zygomatic bone is a strong buttress of the middle third of the facial skeleton that is responsible for facial contour and protection of orbital contents.[
1] It gives the cheek its prominence, forms part of the orbital lateral wall and fltoor, houses the globes and maxillary sinus, and also forms a part of the boundaries of the temporal and infratemporal fossae. Fracture and dislocation of zygoma not only cause adverse cosmetic defects but also disrupts ocular and mandibular functions.[
2]
Despite the high frequency of the zygomaticomaxillary (zygomaticomalar) complex (ZMC) fractures, there is no consensus among facial reconstructive surgeons regarding the best surgical management. Thus, surgical choice for ZMC fractures is still challenging. Basically, four basic principles must be considered when undertaking the repair of a facial fracture: adequate exposure, proper reduction, stable fixation, and minimal complications. Multiple methods were described to approach to and fix the ZMC fracture.[
3]
Few prospective clinical studies compare the results of two-point and three-point rigid plate fixation in patients with fractured zygoma.[
4] This study was conducted to address this particular aspect in the management of ZMC fractures, so as to formulate an operative strategy that will achieve the surgical objective of stable fixation with better clinical results and minimizing the morbidity of the procedure.
Patients and Methods
This study was performed in the Department of Otorhinolaryngology—Head and Neck Surgery, Zagazig University Hospital, from March 2014 to February 2016 on patients with isolated displaced ZMC fracture. Medically unfit patients for surgery, patients with infected fractures, patients with history of TMJ dysfunction, and patients with previously operated ZMC fractures were excluded from this study.
From a total of 60 patients who were admitted in the Zagazig University Hospital in the mentioned period, 40 patients were included in this study and the remaining 20 patients were excluded. Informed written consent was signed by all patients. This study was also approved by the Zagazig University Institutional Review Board (IRB).
Those 40 patients who fulfilled the selection criteria were divided into two groups. Group A: 20 patients were treated with open reduction and internal fixation (OR/IF) using two-point fixation technique (at infraorbital margin and zygomaticofrontal buttress region). Group B: 20 patients were treated with OR/IF using three-point fixation technique (at frontozygomatic suture, infraorbital margin, and zygomatico maxillary buttress).
All patients were subjected to detailed history, photographic assessment, radiological assessment (CT facial bones; axial, coronal, and 3D views), and electromyography (EMG) examination.
Surgery was performed under general anesthesia (nasotracheal intubation). After disinfection and draping, 1:200,000 epinephrine was infiltrated at the site of incisions and dissection. Inferior orbital margin was performed through subciliary approach in 33 cases (82.5%), transconjunctival approach in 6 cases (15%), and subtarsal approach in 1 case (2.5%). Frontozygomatic buttress was addressed using preexisting lacerations in 5 cases (12.5%), lateral eyebrow incision approach in 21 cases (52.5%), and extended subciliary incision in 14 cases (35%). Intraoral superior gingivobuccal sulcus was done in 20 cases (50%). Finally, coronal approach was used in one case to address associated frontal fracture.
Zygomatic bone was reduced using either J-shape zygomatic hook in 37 cases (92.5%) or Allis’ or Kocher’s forceps in three cases (7.5%).
Orbital fltoor exploration was required in two cases (5%) in which clinical picture suggesting orbital fltoor injuries includes enophthalmos, extraocular muscle dysfunction with an abnormal forced duction test, and diplopia. CT confirms the presence of significant orbital fltoor fracture.
Mini titanium plates (1.5 mm thickness) were used for fixation of inferior orbital rim and frontozygomatic buttress, either straight or C shape in two-point fixation group. In three-point fixation, another mini L-shape plate was fixed at zygomaticomaxillary buttress.
The soft tissue overlying the malar prominence was returned via facial sling suture to prevent soft-tissue descent in which the zygomatic periosteum can be lifted and secured to the orbital rim by a preexisting plate. If a lateral canthotomy was performed, reanchoring the lateral canthus at the appropriate height and depth is also critical for maintaining symmetry and lid position. Each incision was closed in subcutaneous layers using Vicryl and in cutaneous layers using silk. Orbital mobility and visual acuity were documented during follow-up.
Patients in each group have same hospital stay (5-day postoperative care) with the same medical regimen.
Assessment Parameters
Aesthetic (Photographic) Assessment
Each patient is assessed via photos 3 months postoperatively to judge on malar eminence projection in different views, including frontal (Frankfort) view, right–left (RT-LT) lateral view, RT-LT oblique view, basal “worm” view, and cephalic “sky bird” view.[
4] Photos were reviewed by three authors who were blinded observers. Cosmetic results were categorized as follows:
Grade I: Excellent cosmetic result, no malar asymmetry.
Grade II: Good cosmetic result, malar asymmetry on careful inspection.
Grade III: Poor cosmetic result, noticeable malar asymmetry.
Grade IV: Gross malar asymmetry.
Radiological Assessment
Facial bone CT scan (axial, coronal, 3D reconstruction) was done for each patient preoperatively to confirm diagnosis and assess type of ZMC fracture and 3 months postoperatively to judge on postreduction of displacement of zygoma.
Figure 1.
Radiological assessment of zygomatic position in axial view at the level of clivus. Distance A—Zygomatic projection: anteroposterior projection of zygoma forms interpterygoid line (reference line) and center of zygoma (distance A; measurements in cm). Distance B— Zygomatic width: lateral presentation of zygoma from nasal septum (reference line) and center of zygoma (measurements in cm).
Figure 1.
Radiological assessment of zygomatic position in axial view at the level of clivus. Distance A—Zygomatic projection: anteroposterior projection of zygoma forms interpterygoid line (reference line) and center of zygoma (distance A; measurements in cm). Distance B— Zygomatic width: lateral presentation of zygoma from nasal septum (reference line) and center of zygoma (measurements in cm).
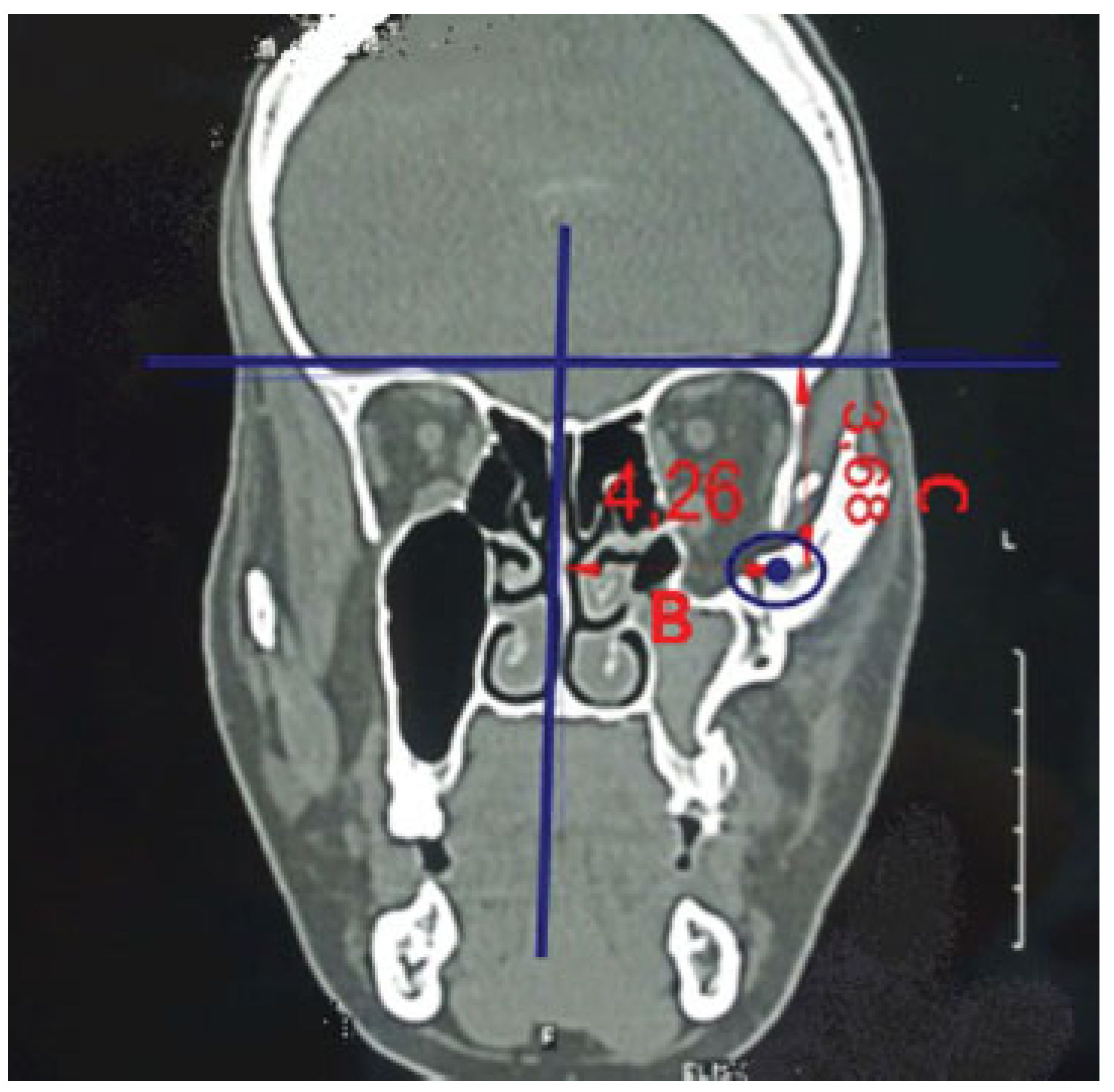
Figure 2.
Radiological assessment of zygomatic position in coronal view at the level of OMC. Distance B—Zygomatic width: lateral presentation of zygoma from nasal septum (reference line) and center of zygoma (measurements in cm). Distance C—Zygomatic height: superoinferior distance forms roof of the bony orbit (reference line) and center of zygoma (measurements in cm).
Figure 2.
Radiological assessment of zygomatic position in coronal view at the level of OMC. Distance B—Zygomatic width: lateral presentation of zygoma from nasal septum (reference line) and center of zygoma (measurements in cm). Distance C—Zygomatic height: superoinferior distance forms roof of the bony orbit (reference line) and center of zygoma (measurements in cm).
3D View
Vertical change of inferior orbital rim (vertical step): Measure distance between two parallel lines drawn over inferior orbital rim on both sides (distance D; measurements in mm; modification from Kim et al[
7]).
Angle of displacement of zygoma: Angle between two parallel lines drawn over lateral surface of zygoma is estimated to assess medial and lateral displacement of zygoma (angle E; modification from Thiagarajan et al;[
2]
Figure 3).
Muscle Power (EMG) Assessment
All patients were subjected to surface EMG to both masseter and temporalis muscles preoperatively and 6 weeks postoperatively by using surface round plate electrodes acting as active reference electrodes and ground electrode.
For temporalis muscle, the active round plate electrode (black) was applied on the motor point of the muscle and thereference electrode (red) was applied on zygomatic bone.
For masseter muscle, the active round plate electrode (black) was applied on the motor point of the muscle and the reference electrode (red) was applied on the angle of mandible.
The ground electrode in both muscles was applied on the neck.
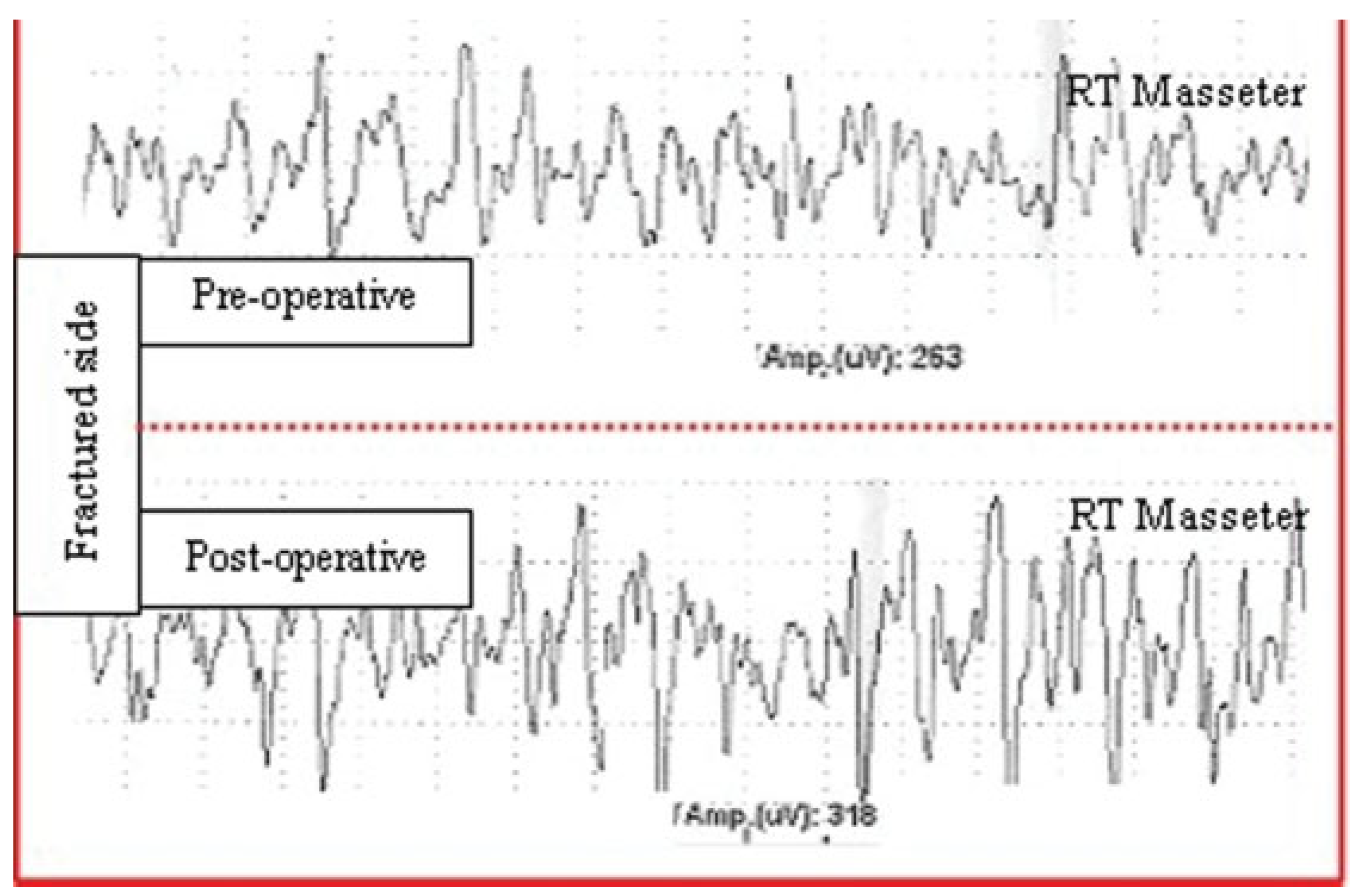
The activity was recorded at rest (to detect any spontaneous activity), at minimal contraction (to detect motor unit action at voluntary contraction) and at maximal contraction (to detect the interference pattern by recording the contraction of the muscle against resistance). The mean of 20 MUAP of the muscles was calculated (in ~10 seconds of contraction, on both sides).This is done by using Nihon Kohden Neuropack S1 MEB-9400K EMG EP System preoperatively and 6 weeks postoperatively to evaluate the degree of improvement of the muscle power (
Figure 4).
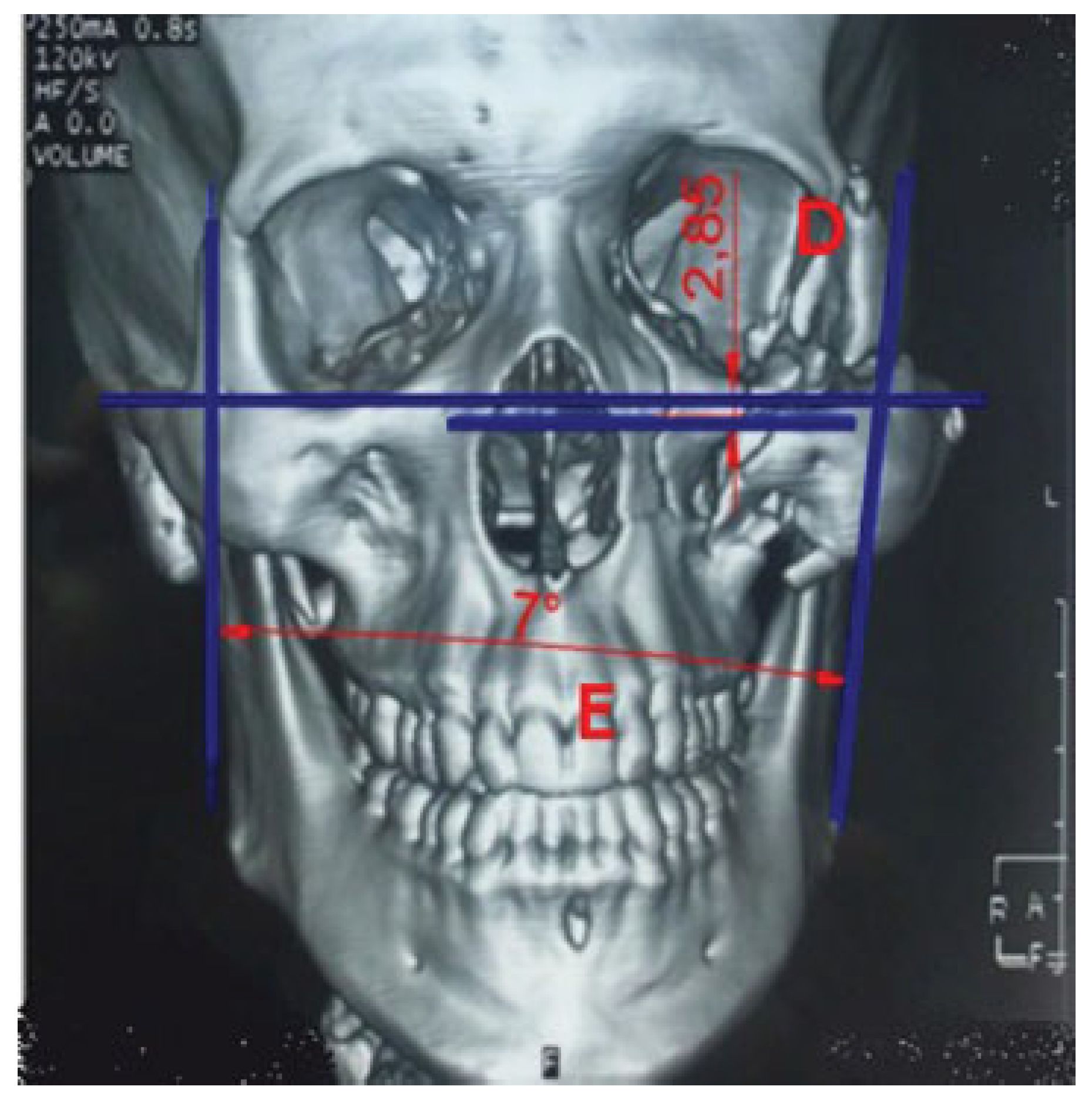
Figure 3.
Radiological assessment of zygomatic position in 3D view. Distance D—vertical change of inferior orbital rim. Vertical step: distance between two parallel lines drawn over inferior orbital rim on both sides (measurements in mm). Angle E—Angle of displacement of zygoma. Angle between two parallel lines drawn over lateral surface of zygoma is estimated to assess medial and lateral displacement of zygoma.
Figure 3.
Radiological assessment of zygomatic position in 3D view. Distance D—vertical change of inferior orbital rim. Vertical step: distance between two parallel lines drawn over inferior orbital rim on both sides (measurements in mm). Angle E—Angle of displacement of zygoma. Angle between two parallel lines drawn over lateral surface of zygoma is estimated to assess medial and lateral displacement of zygoma.
Figure 4.
Muscle activity assessment (EMG): pre- and postoperative EMG of right masseter muscle in right-sided ZMC fracture.
Figure 4.
Muscle activity assessment (EMG): pre- and postoperative EMG of right masseter muscle in right-sided ZMC fracture.
Other Parameters
Actual operation time needed for management of isolated fracture zygoma in both groups which refltects anesthesia time/cost.
Patient satisfaction questionnaire for malar symmetry, scars, enophthalmos, diplopia.
Cost of the plate and screws used in fixation of displaced zygomatic fracture in both groups which can be used as an indicator for cost-effectiveness of both procedures.
Statistical Analysis
Results of preoperative and postoperative evaluations were compared statistically using tests from the SPSS program version 17.0 (Chicago, IL). When p-value is ≤0.05, it is considered statistically significant.
Results
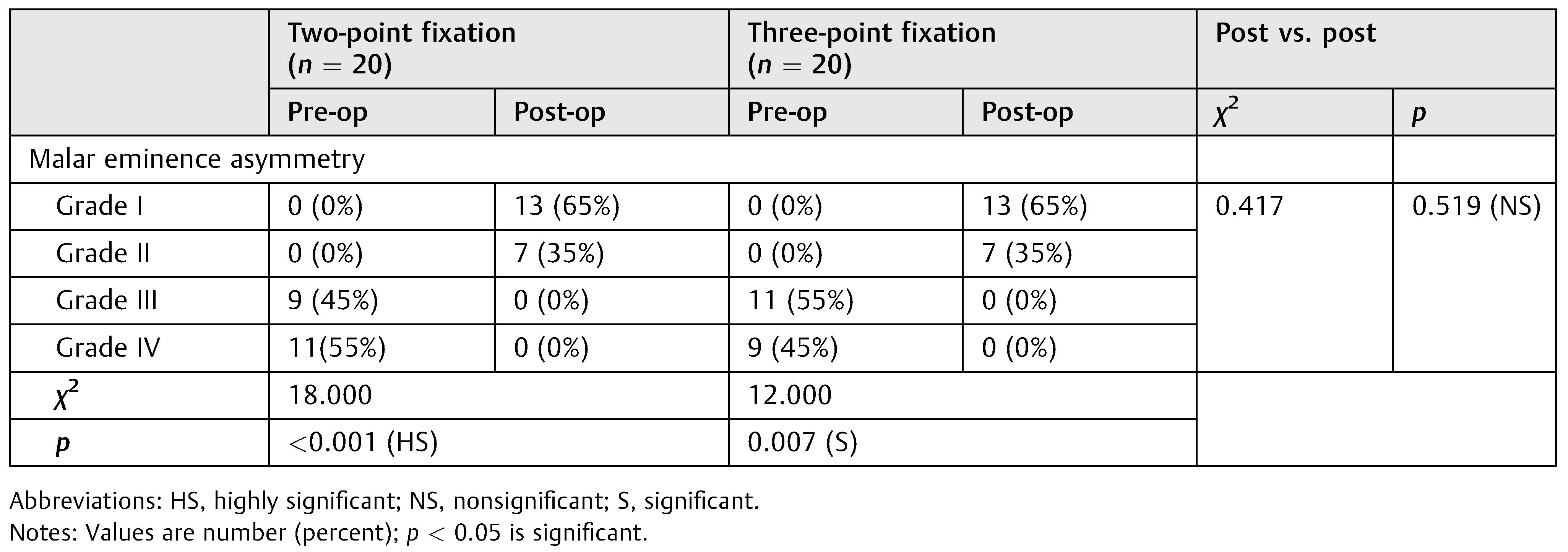
In this study, 40 patients were randomly divided into two study groups (groups A and B). Epidemiological data of the included patients are summarized in
Table 1. Comparison between studied groups was conducted. Malar eminence asymmetry revealed significant improvement in malar prominence with both two-point (
p < 0.001) and three-point (
p = 0.007) groups without statistically significant difference between both modalities (
p = 0.519;
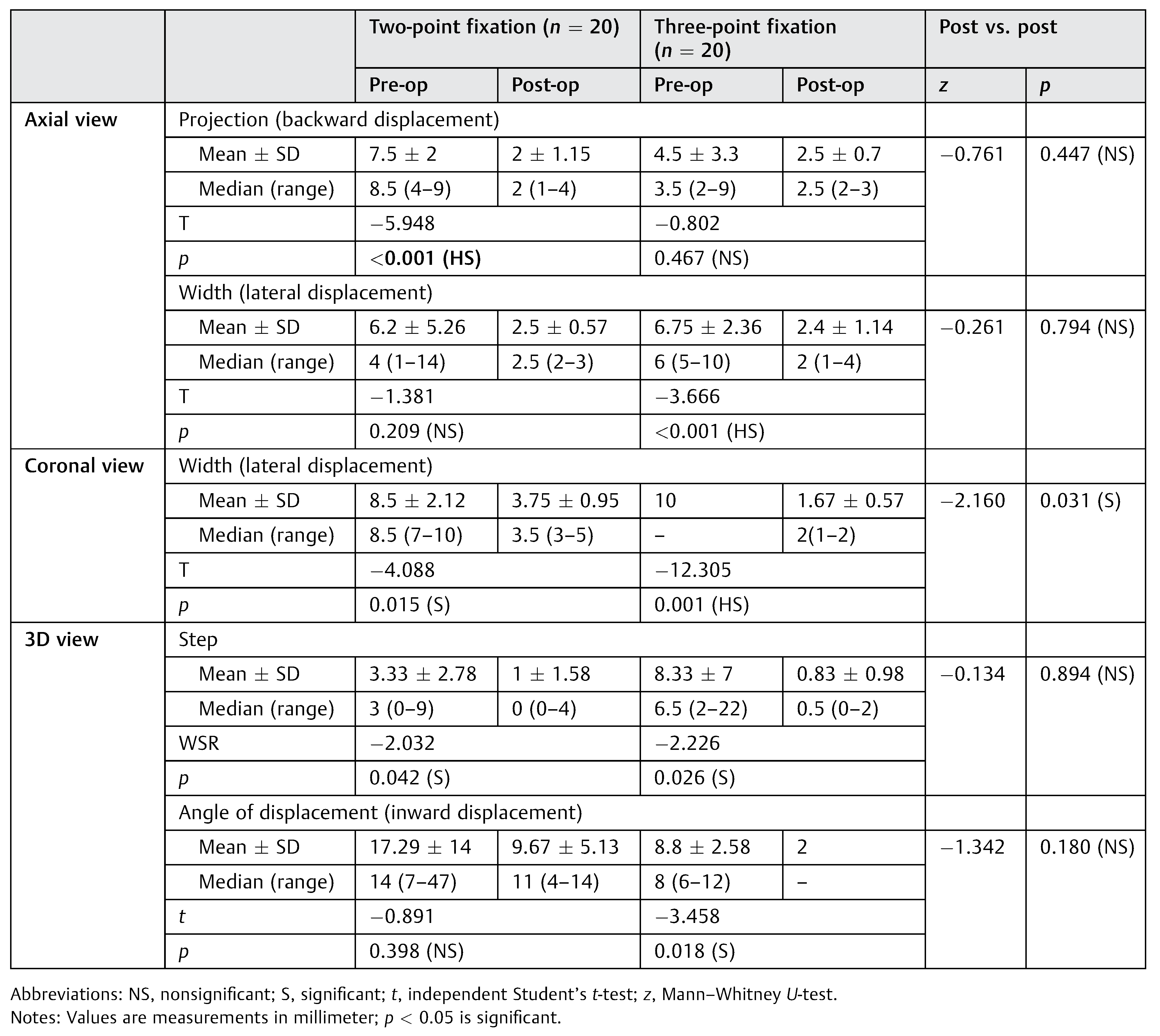
Table 2). Regarding radiological assessment (
Table 3), more perfect reduction without postreduction displacement is obtained by three-point fixation treatment modality (group B) than two-point fixation modality (group A) with statistically significant results in the following items.
Degree of good displacement reduction in laterally displaced zygoma in both axial and coronal views is statistically more significant in group B than in group A (p-value is <0.001, 0.209, respectively), also degree of good displacement reduction in inward angle displacement in 3D view is statistically more significant in group B than in group A (p-value is 0.018, 0.398, respectively).
Both treatment modalities (groups A and B) show statistically significant results between preoperative zygomatic displacement and postoperative zygomatic reduction in coronal view measuring lateral displacement of the zygoma (p-value is 0.015, 0.001, respectively) but with statistically significant results in postoperative results in group B (p-value is 0.0031).
Degree of good displacement reduction in backward displaced zygoma in axial views is statistically more significant in group A than in group B (p-value is <0.001, 0.467, respectively).
Otherwise, there are no statistically significant results in radiological comparison between both modalities in other items: anterior–posterior displacement reduction, medial displacement reduction, superior–inferior displacement reduction, and medial angle displacement in all CT facial bone views.
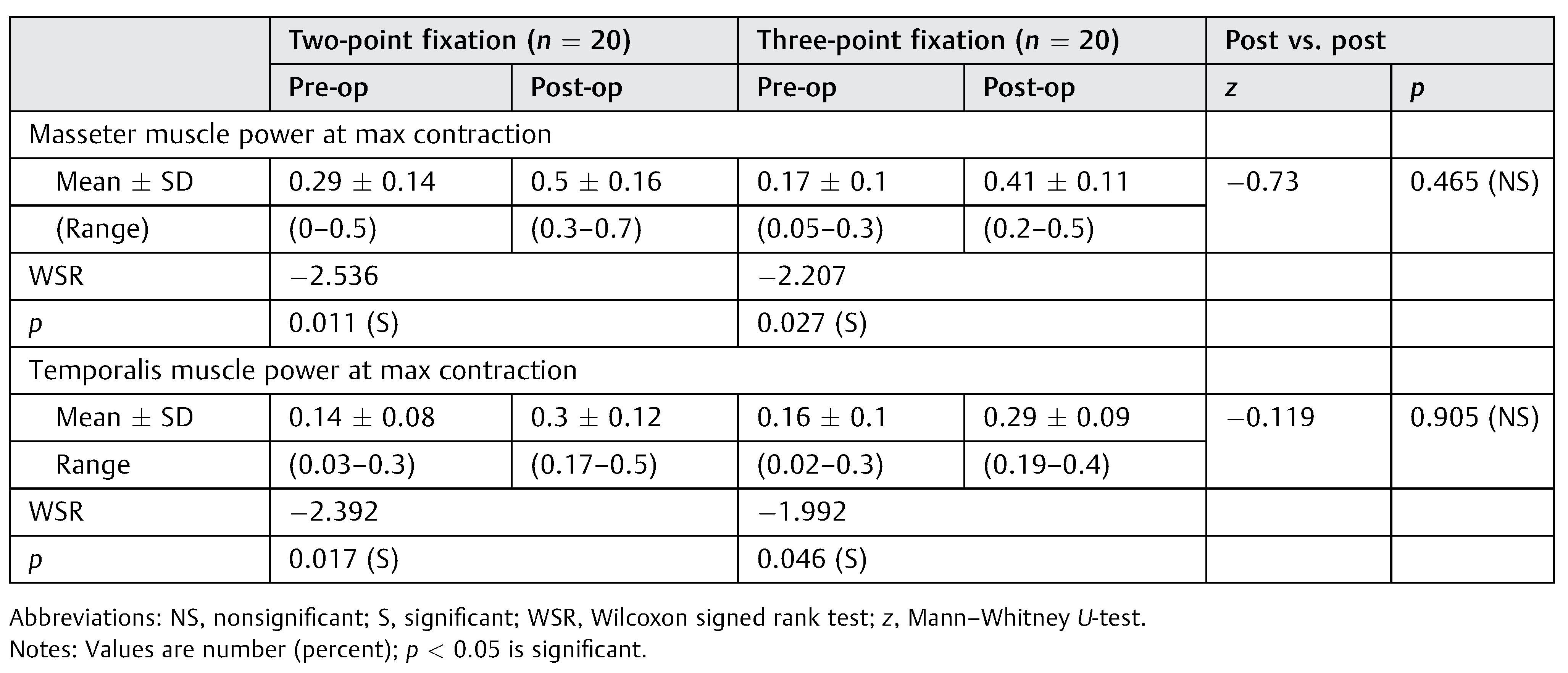
Masseter and temporalis muscles power (EMG) increased significantly after fixation with nonsignificant difference between both groups (
Table 4).
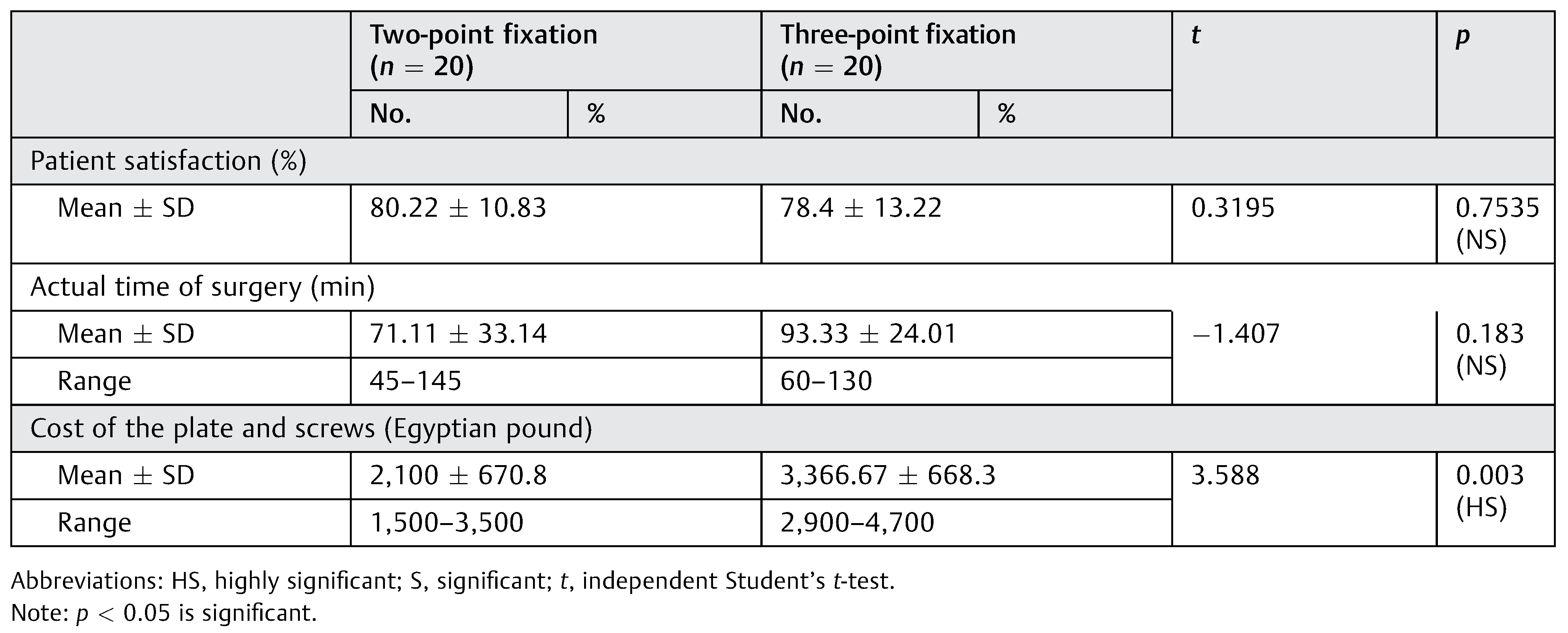
Actual duration of surgery was less in two-point fixation, which was nonsignificant (p = 0.183).
Patient satisfaction did not vary significantly between both types of fixations (p = 0.785).
Cost of the used plates and screws was significantly higher with three-point repair than with two-point repair (
p = 0.003;
Table 5).
No reported postoperative retrobulbar hematoma, diplopia, plate exposure or infection or intolerability, or gross malar asymmetry. But there is true postoperative enophthalmos in one case in group B (2.5%) and one apparent enophthalmos due to rupture globe preoperatively. Also, lower eyelid abnormalities, ectropion with scleral, occur in four cases in group A (20%) and in two cases in group B (5%). All these abnormalities occur with subciliary incision. Also, infraorbital paraesthesia occurs in approximately six cases in group A (30%) and in four cases in group B (10%). All these patients show sensation improvement completely within 6 months postoperatively except in one case in group A (2.5%). In addition, plate palpability occurs in one patient in group A (2.5%) in inferior orbital margin who undergoes conservative management without surgical intervention.
Discussion
Displaced zygoma fractures are vulnerable to secondary malposition caused by masticatory forces even after some types of fixation. These forces must be overcome at fracture sites by optimum stabilization because any postreduction displacement of zygoma can result in delayed development of malar asymmetry and vertical dystopia. Therefore, the goal of treatment of ZMC fractures is to restore and maintain preinjury facial skeletal configuration.[
4] Many experimental biophysical studies have been performed to find out rotational stability of ZMC fracture after OR/IF with miniplate. Davidson et al[
8] analyzed different combinations of miniplate fixation for stabilizing fractured ZMC in human skulls and found that three-point fixation at frontozygomatic suture, inferior orbital rim, and zygomaticomaxillary buttress conferred maximum stability against forces matching physiological stresses. Similar results were found by O’Hara et al[
9] in another experimental biophysical study. Despite these experimental studies, there are no prospective clinical studies.[
4]
Regarding esthetic (malar symmetry) assessment, both treatment modalities (two-point and three-point fixations) had statistically significant retrieve malar symmetry postoperatively (
p < 0.001, 0.007, respectively) without significant difference between both methods. This is a subjective method and these results are in agreement with the results of Parasher et al,[
5] who explained this nonsignificant difference to subjective nature of assessment, thickness of the skin, and subcutaneous tissue edema.
Radiologically speaking, perfect reduction without postreduction displacement was obtained by three-point fixation more than two-point fixation without statistically significant results. This is clear in number of cases with good reduction of displacement in
y-axis (superior–inferior displacement) and is statistically more significant in group B than in group A (
p = 0.049, 0.299, respectively). The number of cases with good reduction of lateral angle displacement in 3D view is statistically significant in group B rather than in group A (
p = 0.049, 0.118, respectively), and the degree of good displacement reduction in laterally displaced zygoma in both axial and coronal views is statistically significant in group B rather than in group A (
p < 0.001, 0.209, respectively). Otherwise, there are no statistically significant results in radiological comparison between both modalities in other items: anterior–posterior displacement reduction, medial displacement reduction, and superior–inferior displacement reduction. These results are similar to that of Pearl,[
10] who reported that it is essential to reposition the zygoma at a minimum of three locations to achieve correction in three dimensions. He further opined that reduction at the frontozygomatic suture and inferior orbital rim can still leave persistent lateral rotation in the region of the anterior maxillary buttress leading to intraorbital volume expansion behind the axis of globe. And according to Parasher et al,[
5] they reported similar result regarding malar height displacement reduction.
Regarding muscle activity (EMG) assessment, both treatment modalities had significantly improved masticatory muscle activity (masseter and temporalis) function postoperatively. Also, with regard to preoperative muscle function, there is statistically significant result between nonfractured side and fractured side in both the groups, which indicate the need of the surgical intervention to improve masticatory muscle activity.
Similarly, Campolongo et al[
11] described electromyographic study in patients with surgically treated facial fractures. The mean values of the masseter activity, in descending order, were from the zygomatic complex, mandibular, maxillary, and associated fractures. The unilateral mandibular fractures showed higher values than the bilateral fractures in most of the evaluations. There was a highly significant difference in the comparison of the evolution of the masseter activity on both sides, for mandibular and zygomatic complex fractures, and the pairwise comparison showed significant difference between most groups. It was concluded that facial fractures and surgical procedures had negative effects in the muscle activity as observed using EMG. To the best of our knowledge, there is no study correlate between zygomatic fracture-surgical interference and masticatory muscle activity.
Regarding patient satisfaction assessment, both treatment modalities show patient satisfaction with the surgical intervention without statistically significant result.
The main factors affecting total satisfaction of the patients in both groups are lower eyelid abnormalities, paraesthesia, and residual malar asymmetry in descending manner. This result was correlated with various studies and techniques used for the management of zygomatic fracture, as Kurita et al[
12] reported that the ultimate goal of plastic surgery should be to attain the maximal degree of satisfaction for the patient. Treatment strategies should thus be optimized not only toward evaluation using objective measures but also toward subjective evaluations from patients. They rated total satisfaction of surgically treated zygomatic patients as 72.5% ± 21.6%; they also rated annoyances with deformity, pain, paraesthesia, and trismus as 12.0 ± 20.5%, 14.6 ± 24.3%, 25.6 ± 31.2%, and 9.8 ± 21.0%, respectively. Various techniques were described to minimize annoyance from incision. Hwang[
13] described operative technique for the management of zygomatic fracture via lateral brow incision and one-point fixation of frontozygomatic buttress. Kim et al[
7] described surgical technique of one-point fixation at the zygomaticomaxillary buttress through a buccogingival incision using ultrasonography for judgment on reduction. Carvalho et al[
14] described a modification of the Keen technique that promotes adequate visualization of the infraorbital rim and permits reduction and fixation of this region in cases of zygomatic fractures. Lee et al[
15] described a single transconjunctival incision with lateral canthotomy and two-point (inferior orbital rim and frontozygomatic suture) fixation. Chakranarayan et al[
16] reported two-point fixation of zygomatic complex fracture via double-incision lateral eyebrow and upper gingivobuccal incisions.
The mean actual operation time in group B is more than that in group A but without significant results (mean of operation time: 93 and 71 minutes, respectively). This may be due to insufficient patient number in this study leading to nonsignificant results.
Regarding cost of the plate and screws used in both treatment modalities, three-point fixation modalities show statistically significant high-cost result in relation to the other method (
p = 0.003). These results are similar to that of Parasher and Ramesh.[
5]
Regarding postoperative complication, there is no specific complication related to trauma (rupture globe—postoperative apparentenophthalmos) or incision (ectropionwith subciliary incision) in either of the methods. These results are in contrast with that of Parasher and Ramesh,[
5] who reported that vertical dystopia, enophthalmos, is higher in two-point fixation than in three-point fixation with statistically significant results (
p < 0.01, <0.02, respectively). This difference may be due to insufficient zygomatic bone reduction intraoperatively or missed orbital fltoor fracture after reduction.
Thus, collectively, postoperative CT lateral zygoma displacement was one finding that showed statistically significant better result in three-point fixation (as asymptomatic radiological measurement).
While other CT measurements including projection (forward displacement) and width (medial displacement) in axial CT, inferior displacement, superior displacement and width (medial displacement) in coronal CT, and angle of displacement (outward displacement) in 3D CT showed nonsignificant differences between two- and three-point fixations. Moreover, the clinical assessment with regard to malar eminence asymmetry and patient satisfaction showed nonsignificant differences.
Therefore, although three-point fixation modality is known to exert maximum stability against forces matching physiological stresses,8,9 the results of current clinical comparative study revealed that three-point fixation of ZMC fractures did not add significant difference from two-point fixation regarding most parameters of malar symmetry and radiological reduction, muscle power, and patients’ satisfaction. On the other hand, three-point fixation increases the cost and surgery duration. Current results are in agreement with Lee et al15 and Chakranarayan et al,16 while Parasher and Ramesh[
5] and Rana et al[
4] recommended three-point fixation to obtain stable fixation. So, results of two-point fixation could be achieved on proper fixations at frontozygomatic buttress and inferior orbital rim after adequate disimpaction and reduction of the fractures and using miniplates and screws. However, larger series of patients still need to be studied.
Conclusion
Three-point fixation technique is the standard fixation technique of ZMC fracture. However, apart from asymptomatic and clinically unnoticeable radiological difference, two-point fixation modality for displaced ZMC fractures is almost as effective as three-point fixation and prevents postreduction rotation or clinical displacement with significantly lower cost.