Traumatic Anterosuperior Dislocation of the Intact Mandibular Condyle into the Temporal Fossa
Abstract
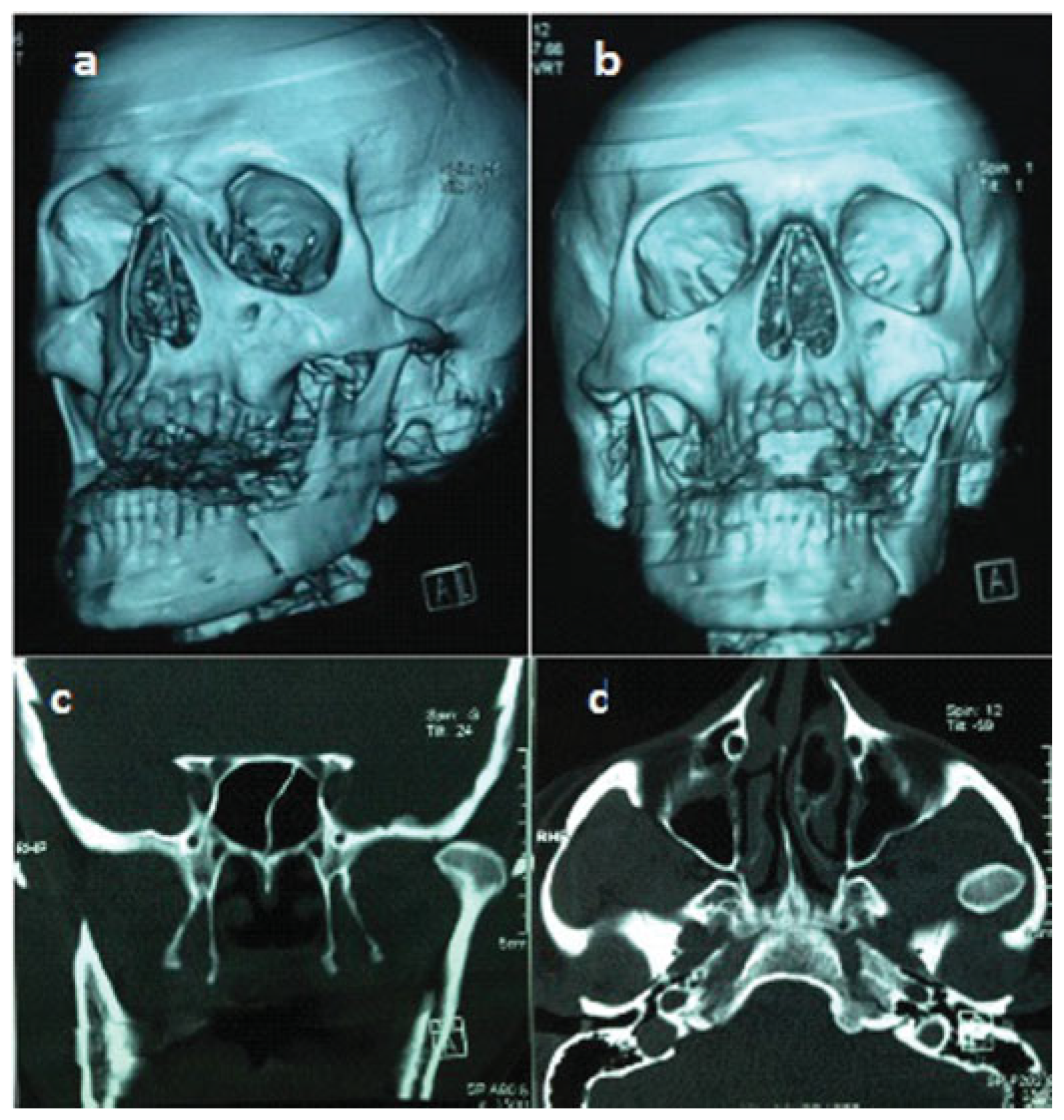
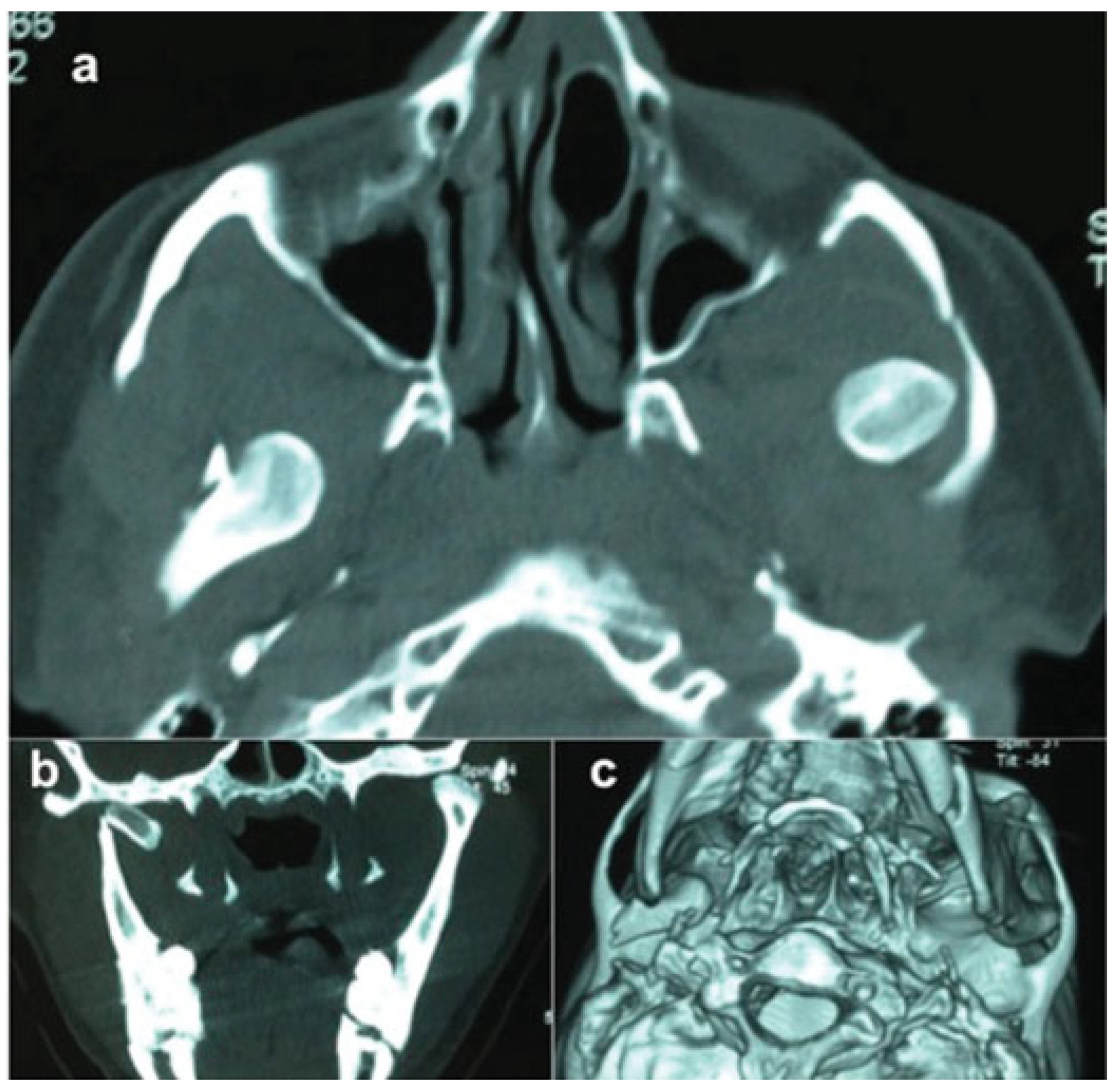
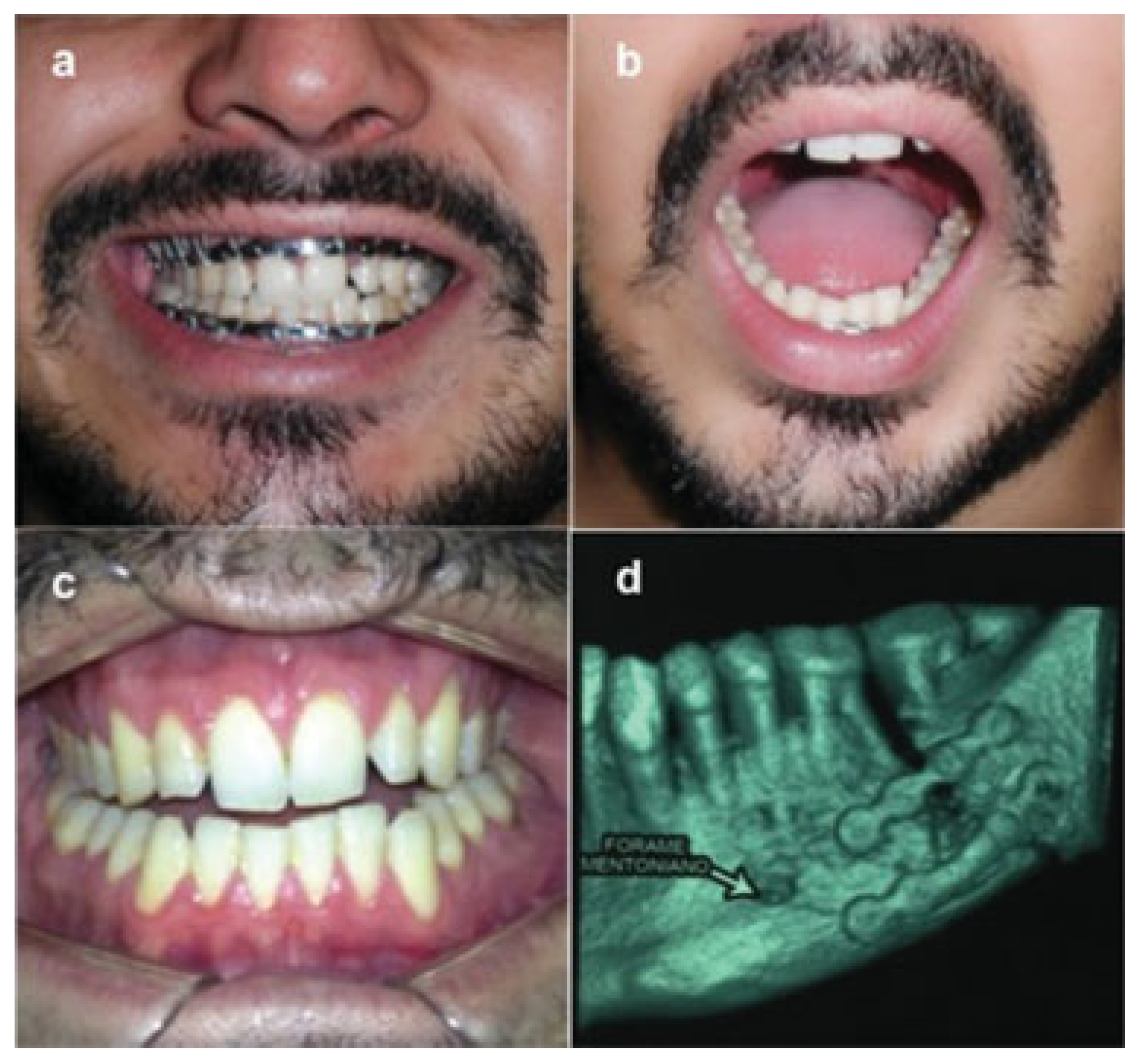
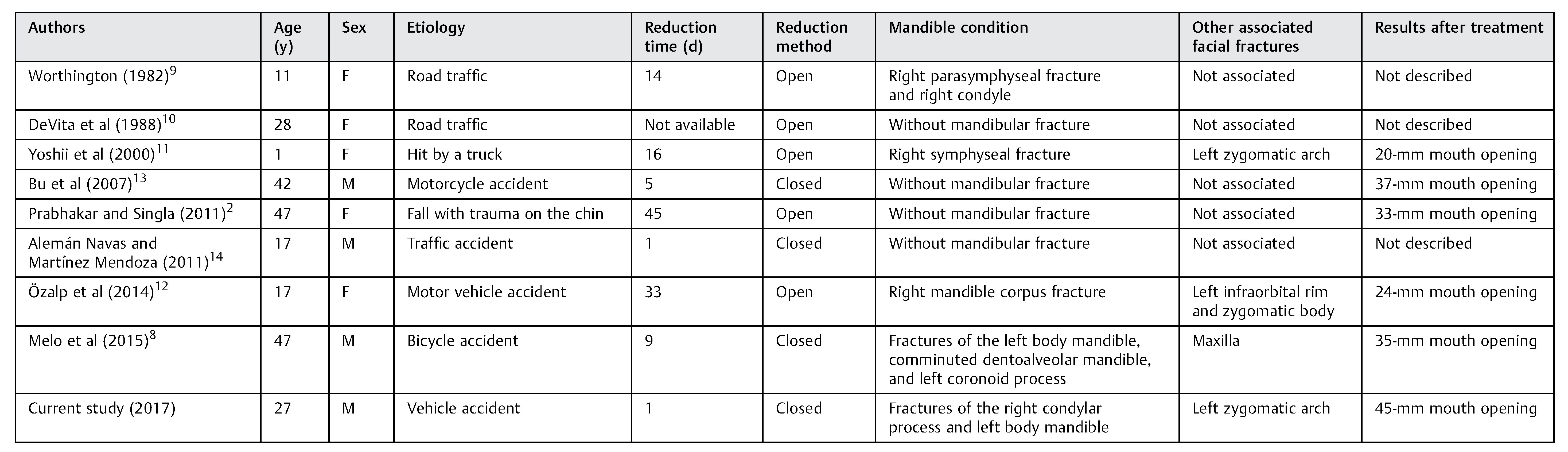
:Case Report
Conclusion
References
- He, Y.; Zhang, Y.; Li, Z.L.; An, J.G.; Yi, Z.Q.; Bao, S.D. Treatment of traumatic dislocation of the mandibular condyle into the cranial fossa: development of a probable treatment algorithm. Int J Oral Maxillofac Surg 2015, 44, 864–870. [Google Scholar] [CrossRef]
- Prabhakar, V.; Singla, S. Bilateral anterosuperior dislocation of intact mandibular condyles in the temporal fossa. Int J Oral Maxillofac Surg 2011, 40, 640–643. [Google Scholar] [CrossRef] [PubMed]
- Vaezi, T.; Rajaei, S.A.; Hosseini Abrishami, M.; Erfanian Taghvaei, M. Dislocation of the mandibular condyle into the middle cranial fossa: a case report. Oral Maxillofac Surg 2014, 18, 69–73. [Google Scholar] [CrossRef]
- Oberman, B.; Setabutr, D.; Goldenberg, D. Traumatic dislocation of intact mandibular condyle into middle cranial fossa. Am J Otolaryngol 2014, 35, 251–253. [Google Scholar] [CrossRef] [PubMed]
- Rahman, T. Unusual superolateral dislocation of mandibular condyle. Craniomaxillofac Trauma Reconstr 2017. [CrossRef] [PubMed]
- Allen, F.J.; Young, A.H. Lateral displacement of the intact mandibular condyle. A report of five cases. Br J Oral Surg 1969, 7, 24–30. [Google Scholar] [CrossRef]
- Satoh, K.; Suzuki, H.; Matsuzaki, S. A type II lateral dislocation of bilateral intact mandibular condyles with a proposed new classification. Plast Reconstr Surg 1994, 93, 598–602. [Google Scholar] [CrossRef]
- Melo, M.F.S.; Oliveira, R.B.; Silveira, R.L.; Amaral, M.B.F. Anterosuperior dislocation of the intact condyles into the temporal fossa. J Craniofac Surg 2015, 26, 990–991. [Google Scholar] [CrossRef]
- Worthington, P. Dislocation of the mandibular condyle into the temporal fossa. J Maxillofac Surg 1982, 10, 24–27. [Google Scholar] [CrossRef]
- DeVita, C.L.; Friedman, J.M.; Meyer, S.; Breiman, A. An unusual case of condylar dislocation. Ann Emerg Med 1988, 17, 534–536. [Google Scholar] [CrossRef]
- Yoshii, T.; Hamamoto, Y.; Muraoka, S.; Teranobu, O.; Shigeta, Y.; Komori, T. Traumatic dislocation of the mandibular condyle into the temporal fossa in a child. J Trauma 2000, 49, 764–766. [Google Scholar] [CrossRef] [PubMed]
- Özalp, B.; Elbey, H.; Durgun, M.; Selçuk, C.T. An alternative surgical procedure for anterosuperior dislocation of intact mandibular condyle. J Craniofac Surg 2014, 25, e382–e384. [Google Scholar] [CrossRef] [PubMed]
- Bu, S.S.; Jin, S.L.; Yin, L. Superolateral dislocation of the intact mandibular condyle into the temporal fossa: review of the literature and report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007, 103, 185–189. [Google Scholar] [CrossRef]
- Alemán Navas, R.M.; Martínez Mendoza, M.G. ‘Inverse’ temporo-mandibular joint dislocation. Int J Oral Maxillofac Surg 2011, 40, 877–879. [Google Scholar] [CrossRef]
- Chan, T.C.; Harrigan, R.A.; Ufberg, J.; Vilke, G.M. Mandibular reduction. J Emerg Med 2008, 34, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Myrhaug, H. A new method of operation for habitual dislocation of the mandible; review of former methods of treatment. Acta Odontol Scand 1951, 9, 247–260. [Google Scholar] [CrossRef]
- Young, A.L.; Khan, J.; Thomas, D.C.; Quek, S.Y. Use of masseteric and deep temporal nerve blocks for reduction of mandibular dislocation. Anesth Prog 2009, 56, 9–13. [Google Scholar] [CrossRef]
- Li, Z.; Li, Z.B.; Shang, Z.J.; Wu, Z.X. An unusual type of superolateral dislocation of mandibular condyle: discussion of the causative mechanisms and clinical characteristics. J Oral Maxillofac Surg 2009, 67, 431–435. [Google Scholar] [CrossRef]
- Ogawa, M.; Kanbe, T.; Kano, A.; et al. Conservative reduction by lever action of chronic bilateral mandibular condyle dislocation. Cranio 2015, 33, 142–147. [Google Scholar] [CrossRef]
- Shorey, C.W.; Campbell, J.H. Dislocation of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000, 89, 662–668. [Google Scholar] [CrossRef]
- Tutela, J.P.; Verbist, D.E.; Kelishadi, S.; Little, J.A. Traumatic dislocation of the mandibular condyle into the middle cranial fossa in an elderly patient. J Craniofac Surg 2013, 24, 1703–1705. [Google Scholar] [CrossRef]
- Shen, L.; Li, P.; Li, J.; Long, J.; Tian, W.; Tang, W. Management of superolateral dislocation of the mandibular condyle: a retrospective study of 10 cases. J Craniomaxillofac Surg 2014, 42, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Sharma, D.; Khasgiwala, A.; Maheshwari, B.; Singh, C.; Shakya, N. Superolateral dislocation of an intact mandibular condyle into the temporal fossa: case report and literature review. Dent Traumatol 2017, 33, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Tauro, D.; Lakshmi, S.; Mishra, M. Superolateral dislocation of the mandibular condyle: report of a case with review of literature and a proposed modification in the classification. Craniomaxillofac Trauma Reconstr 2010, 3, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Kapila, B.K.; Lata, J. Superolateral dislocation of an intact mandibular condyle into the temporal fossa: a case report. J Trauma 1996, 41, 351–352. [Google Scholar] [CrossRef]
- Amaral, M.B.; Bueno, S.C.; Silva, A.A.; Mesquita, R.A. Superolateral dislocation of the intact mandibular condyle associated with panfacial fracture: a case report and literature review. Dent Traumatol 2011, 27, 235–240. [Google Scholar] [CrossRef]
- Huang, I.Y.; Chen, C.M.; Kao, Y.H.; Chen, C.M.; Wu, C.W. Management of long-standing mandibular dislocation. Int J Oral Maxillofac Surg 2011, 40, 810–814. [Google Scholar] [CrossRef]
- Lello, G.E. Treatment of long-standing mandibular dislocation. J Oral Maxillofac Surg 1987, 45, 893–896. [Google Scholar] [CrossRef]


 |
© 2017 by the author. The Author(s) 2017.
Share and Cite
Silveira, R.L.; Ranuzia, I.; Melo, M.F.S.; de Oliveira, R.A.; de Brito, A.A.; Vidigal, V.L. Traumatic Anterosuperior Dislocation of the Intact Mandibular Condyle into the Temporal Fossa. Craniomaxillofac. Trauma Reconstr. 2018, 11, 296-301. https://doi.org/10.1055/s-0037-1607067
Silveira RL, Ranuzia I, Melo MFS, de Oliveira RA, de Brito AA, Vidigal VL. Traumatic Anterosuperior Dislocation of the Intact Mandibular Condyle into the Temporal Fossa. Craniomaxillofacial Trauma & Reconstruction. 2018; 11(4):296-301. https://doi.org/10.1055/s-0037-1607067
Chicago/Turabian StyleSilveira, Roger Lanes, Ivan Ranuzia, Marcelo Fernandes S. Melo, Rogerio Araujo de Oliveira, Antonio Alburquerque de Brito, and Victor Laviola Vidigal. 2018. "Traumatic Anterosuperior Dislocation of the Intact Mandibular Condyle into the Temporal Fossa" Craniomaxillofacial Trauma & Reconstruction 11, no. 4: 296-301. https://doi.org/10.1055/s-0037-1607067
APA StyleSilveira, R. L., Ranuzia, I., Melo, M. F. S., de Oliveira, R. A., de Brito, A. A., & Vidigal, V. L. (2018). Traumatic Anterosuperior Dislocation of the Intact Mandibular Condyle into the Temporal Fossa. Craniomaxillofacial Trauma & Reconstruction, 11(4), 296-301. https://doi.org/10.1055/s-0037-1607067



