Nasal septum perforation represents a frequent challenge facing the reconstructive surgeon. Causes of perforation are diverse and include acquired injuries caused by trauma or septal surgery, systemic disease, or medication. The sizes of septal perforations vary, as do their associated subjective and objective patient complaints. Nasal airflow dysfunction such as obstruction and inspiratory whistling, crusting, pain, infection, and epistaxis may all co-occur and can be debilitating and refractory to conservative treatment, including nasal irrigations, emollients, humidifiers, applications of antibiotic salves, and nasal septal prosthesis such as a septal button[
1,
2] and.[
3]
The thin and malleable temporoparietal fascia (TPF) pedicled or free flap is an excellent tool in head and neck reconstruction. Extending laterally from the galea aponeurotica, the TPF is continuous with the superficial musculoaponeurotic system inferiorly; the flap has consistent vascular anatomy and is well suited to accept skin grafts.[
4] Numerous uses for the TPF pedicled or free flap have been characterized in the literature; here we present the use of a TPF free flap for the repair of a nasal septal perforation. To our knowledge, this is the first description of this technique for this indication.
Case Report
Case Patient
A 37-year-old woman presented with a history of remote intranasal cocaine use and developed a nasoseptal perforation with concomitant loss of anterior aspects of bilateral inferior turbinates. The perforation measured 3.5 cm in length and 3.0 cm in height. The patient’s complaints of nasal crusting, dryness, bleeding, and chronic pain worsened by cold air which were all refractory to medical management. No other prior surgical interventions were attempted and the patient requested complete repair for relief of her symptoms. After extensive discussion regarding the available reconstructive options given the paucity of local tissues, free tissue transfer, using a temporoparietal free flap, of the full-thickness septal defect was planned.
Surgical Approach
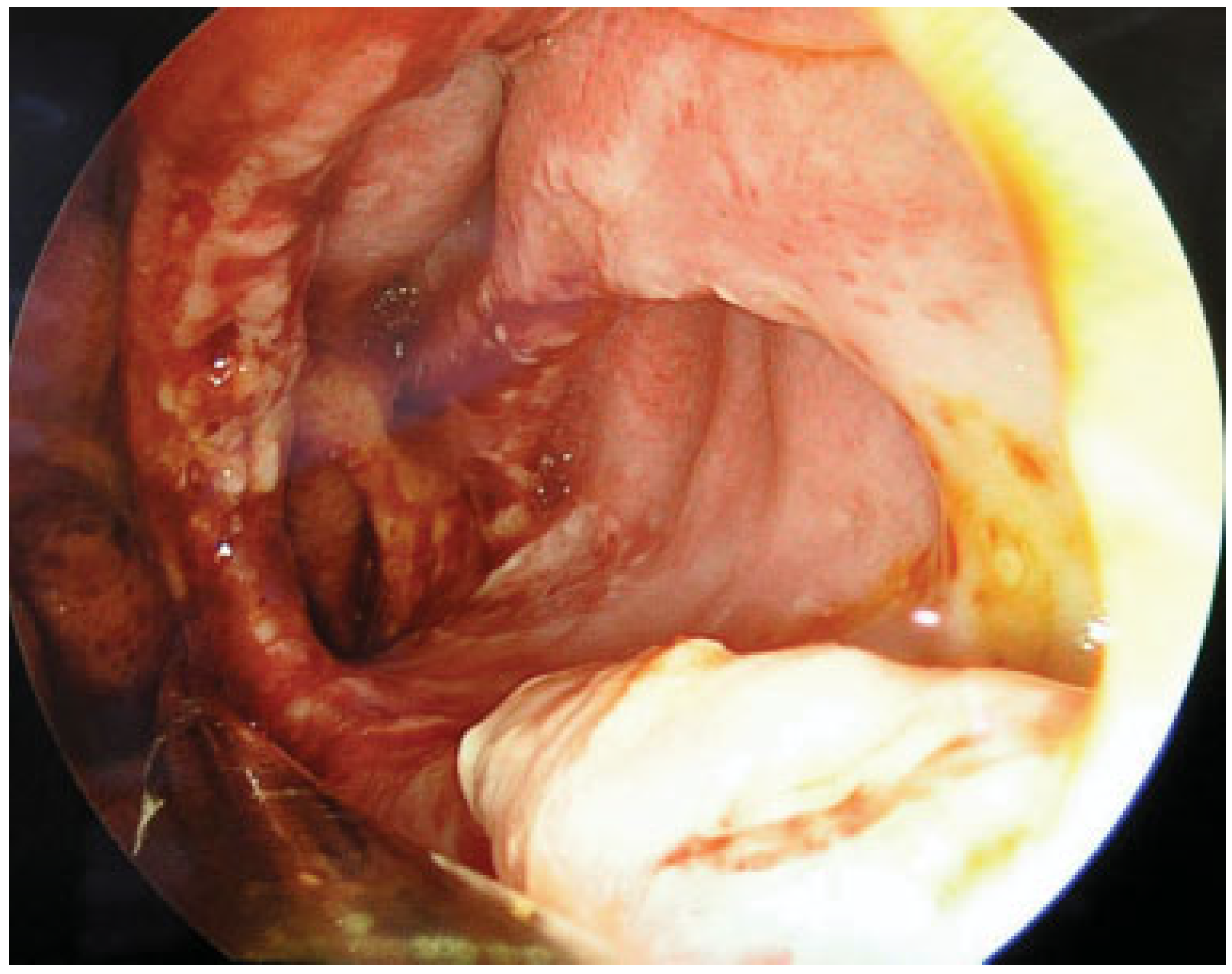
Prior to the procedure on the day of surgery, the patient presented to the hospital and initially had a toxicology screen, which was negative for the presence of cocaine or opiates. Following evaluation by anesthesia and review of the medical clearance, the patient was deemed safe for surgery. A TPF free flap based on the superficial temporal artery was identified using Doppler ultrasound and marked on the skin anterior to the left auricle. Similarly, the facial artery and vein were also marked. A hemitransfixion incision was performed to elevate a mucoperichondrial flap anterior, superior, and inferior to the septal defect. A 3.0 cm × 4.0 cm advancement rotation flap was elevated from the nasal floor in anticipation of accommodating tissue from the left temporal region and was left for a later portion of the operation. Afrin-soaked pledgets were left intranasally and attention was then given to the elevation of the TPF free flap demonstrated in
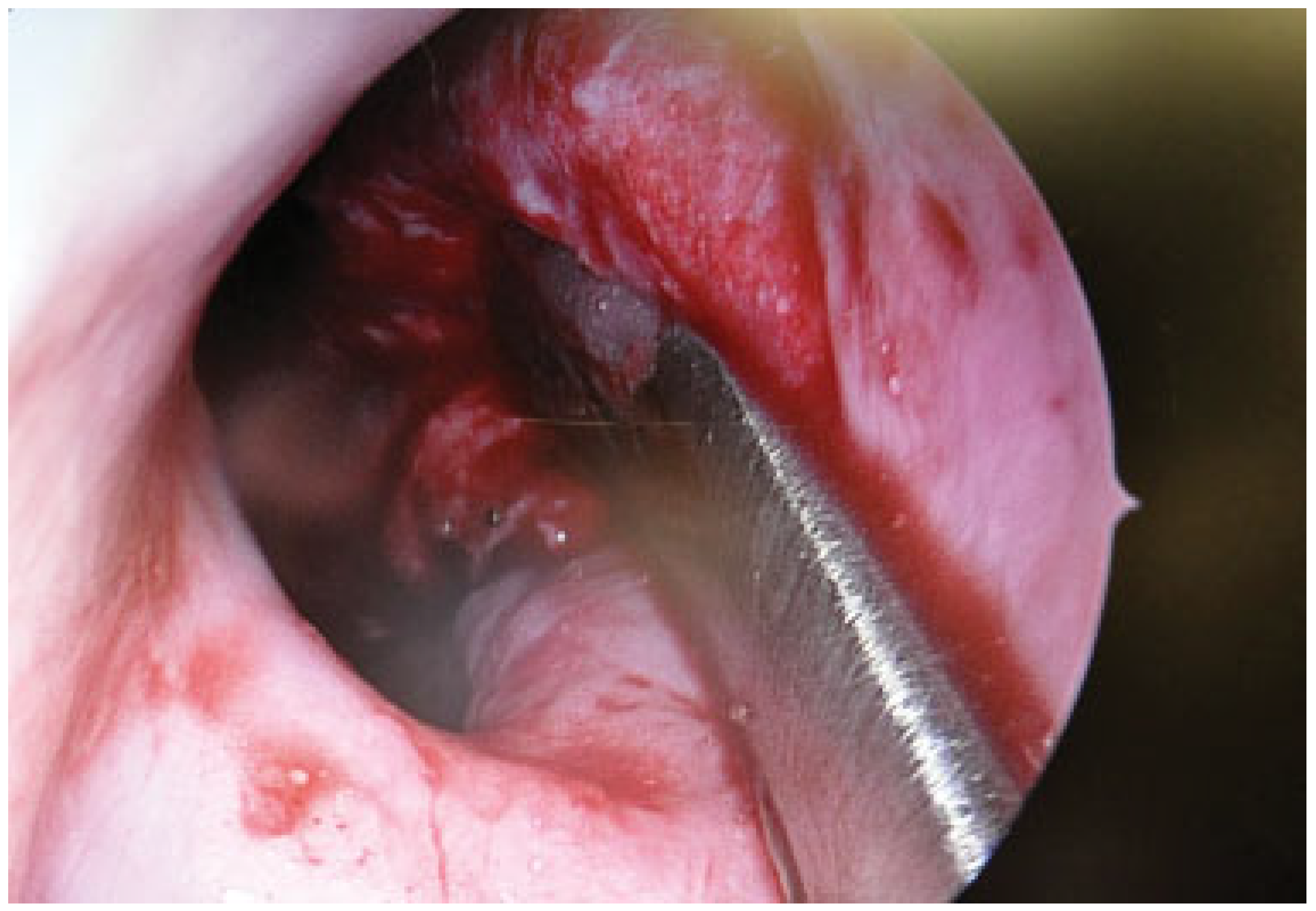
Figure 1, which was made to accommodate the intranasal defect, measuring 3.5 cm in length and 3.0 cm in height noted in
Figure 2; inset is seen in
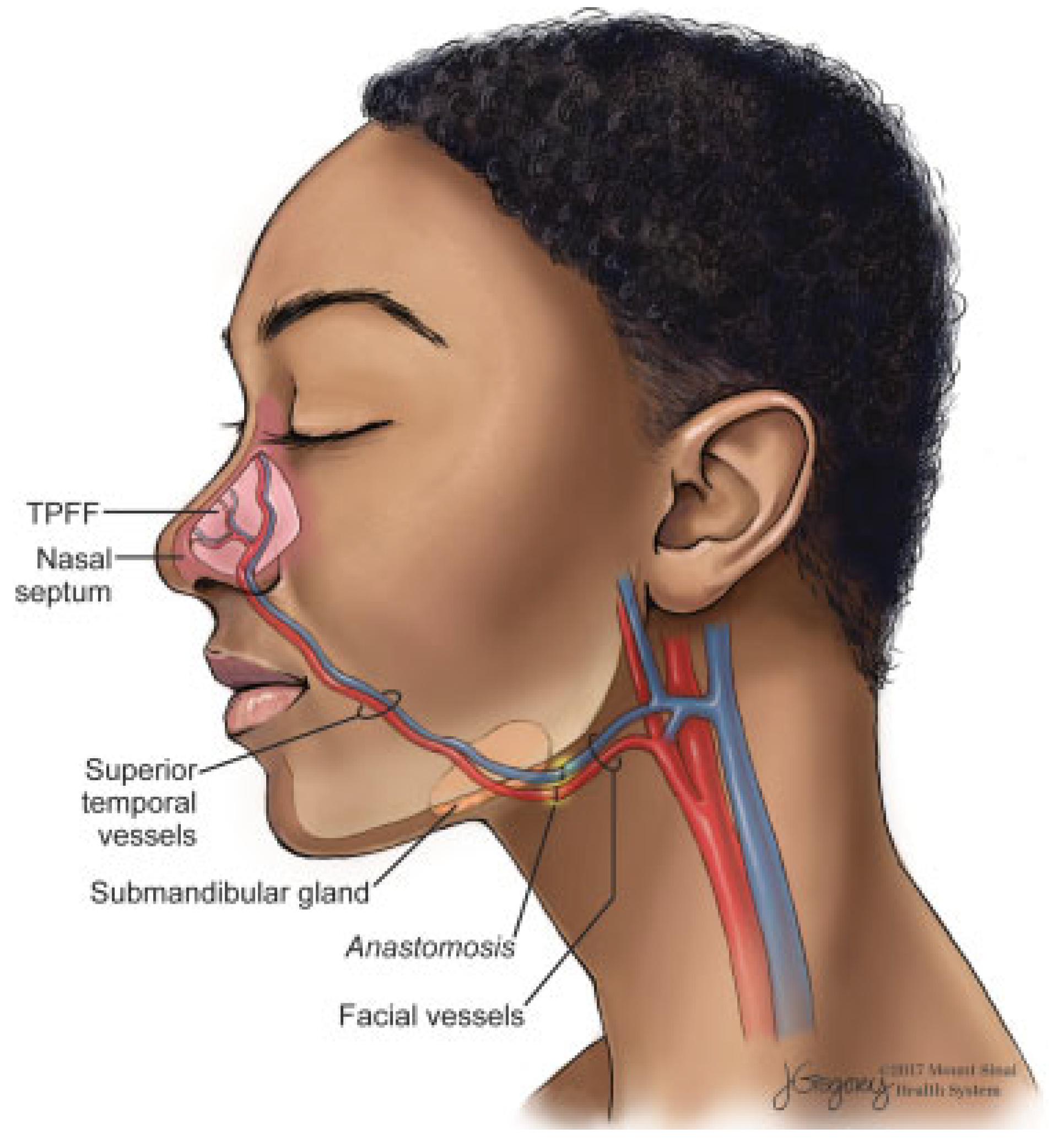
Figure 3. The ipsilateral facial artery and vein were identified and traced proximally with concomitant use of a facial nerve monitor until they could be circumferentially isolated. The free flap pedicle was placed into a subcutaneous tunnel through the floor of the nose into the nasolabial fold and down into the neck, and microvascular anastomosis was performed in the usual fashion.
Figure 4 shows an illustration of this inset and anastomosis. The flap was monitored postoperatively by evaluating Doppler signals of the vein and artery that were marked by an external skin stitch. A drain was placed underneath the tissues and secured to the posterior scalp. Silastic stents were placed intranasally with modification of the left silastic stent to avoid compression over the free tissue.
Results
The postoperative course was uncomplicated. A nasal hygiene regimen was implemented, consisting of three-timesdaily nasal saline irrigation and daily bacitracin to the intranasal incision. Nasal silastic stents were removed at 2 weeks from the index procedure. The patient reports complete symptom resolution, with no complaint of dryness, bleeding, crusting, or pain which had chronically plagued the patient. Notably, the patient’s preoperative sensitivity to changes in heat and cold also resolved postoperatively. Although a symptom-specific outcome score was not utilized in this case, the complete resolution of symptoms served as a strong indicator that the patient had derived improvement from surgical therapy. At 6 months, the reconstructed nasal septum was intact, with pink and viable nasal mucosa. The wound edges of the TPF flap incision were clean and intact, with no signs of incisional alopecia. Facial nerve function was additionally intact. Although the patient was requested and advised to return for further follow-up appointments, given the lack of symptoms and satisfaction with the procedure the patient opted to return on an as-needed basis.
Discussion
Surgical reconstruction may offer definitive symptom relief, and there exist several modalities for repair depending on surgeon’s skillset and the nature of the perforation. Despite the absence of comprehensive randomized controlled trials, a wealth of nonrandomized retrospective studies and literature review exist to aid in prognosticating septal perforation repair. Determinants of successful repair include the size of the septal perforation, complete bilateral flap coverage, and the successful interposition of grafting material.[
5] Poor consensus exists regarding classification of perforation size, although defects exceeding 2.0 cm are generally considered to be large and are intrinsically more difficult to close due to the paucity of associated mucosa, with complete successful closure obtained in approximately 78% of patients.[
2,
5] Notably, posterior perforations are more difficult to repair; thankfully these perforations are less likely to be symptomatic.[
6]
Surgical repair does not always guarantee relief of symptoms. Indeed, more bulky flaps and destruction of nasal mucosa may together and independently affect nasal airflow in spite of perforation repair.[
1,
5] Reconstructive modalities vary, with smaller to medium perforations, loosely defined as 5.0 mm to less than 2.0 cm, more often amenable to local advancement flaps and/or concomitant interposition grafts with remnant septal cartilage, septal bone, auricular cartilage, dermal allograft, titanium membrane, and bioactive glass among other modalities.[
5,
7] These interpositional grafts appear to reduce reperforation. Nonetheless, there is evidence to suggest that factors such as tension-free flap approximation may be more critical for closure.[
5]
It is important to understand, however, that cartilage is not a required portion of the reconstruction of septal defects. Given that the patient has an adequate dorsal and caudal septal cartilaginous strut, the presence of cartilage in the reconstructed perforation does not necessarily add much value; however, the literature is divided regarding this subject. Patients undergoing routine septoplasty have large portions of cartilage removed without any untoward consequences so long as the mucosal flaps are intact bilaterally. Uni- or bipedicled advancement flaps, inferior turbinate flap, nasolabial flap, labiobuccal flap, and skin flaps have been characterized in closing septal defects. Regional flaps, such as pericranial and facial artery musculomucosal flaps, have also been cited in the literature as a potential option for reconstruction.[
8,
9]
Ideally, the trilaminated nature of the nasal septum, namely, cartilage interposed between mucosal tissues, should be reapproximated during repair. Free flaps, including radial forearm free flap and fascia lata, are well suited for this task and are particularly useful in defects too large for regional flaps.[
3,
10] The free flap requires adequate exposure for the treatment of larger perforations. External septorhinoplasty, lateral alotomy, and historically even midface degloving have all been described for exposure of large septal perforations.[
11]
Myriad reconstructive options exist for nasal septal perforations and the location, size, and the intrinsic threelayered nature of the nasal septum add complexity to its repair. Larger perforations are typically more technically difficult to close, and may render local tissue advancement ineffective. Moreover, remnant native vasculature and the native mucosal bed may be inadequate and damaged. In this way, adjacent tissue rearrangement or, in this case, free flap placement represents a tenable option to close larger septal defects. The free flap’s “external” blood supply is of particular usefulness, as it precludes the need for intact native septal vasculature, which may be compromised. Not all free flaps are created alike, indeed radial forearm free flaps are often more bulky, requiring thinning and patients frequently complain of donor-site scar. Bank et al described prelaminating a fascia lata free flap with buccal mucosa and elevating and positioning in a two-stage procedure with excellent results.[
3]
In this case study, the TPF flap was harvested with ease and had minimal donor-site morbidity with a well-hidden scar. Unlike the two-stage procedures needed to mucosalize the fascia lata flap, the TPF flap is mucosalized without exogenous intervention in approximately 3 weeks, with no crusting or desquamation. This case study serves as a proof of concept regarding the use of a TPF free flap to repair large septal defects that would otherwise not be amenable to local flaps or septal prosthesis. It is important to recognize that patients with a history of cocaine abuse need to be scrutinized more closely prior to undertaking surgery, given not only the cardiac concerns from anesthesia but also the potential limitations posed by poorly vascularized mucosa. The authors in this study typically recommend waiting for 4 to 6 months following cessation of cocaine abuse before undertaking reconstruction.
A clear limitation of the study is its single case, and that its findings, while assuring, cannot represent a generalizable option, as there need to be more studies to validate the use of our approach as a safe alternative. Disadvantages of using a free flap include the need for a skilled microvascular surgeon, specialized instrumentation, donor-site morbidity, and the potential need for several operative stages. The TPF free flap obviates the concern of significant donor-site morbidity and can be completed as a single stage. This study codifies a novel approach for nasal septal perforation closure by use of the TPF free flap.