Abstract
Management of condylar fractures is a highly controversial and debatable area. Open reduction and internal fixation (ORIF) using an extraoral approach has certain benefits over the nonsurgical treatment. Risk of damage to the facial nerve and an extraoral scar remains constant deterrents. An endoscopic-assisted ORIF offers an intraoral approach, thus eliminating consequences such as scarring. Though this technique offers unparalleled advantages, it is associated with a steep learning curve. Surgical results improve only with patience and experience. Patients with condylar fractures reported to SDM Craniofacial Unit, Dharwad, India, from 2013 to 2015 are included. Patients were treated with endoscopic-assisted ORIF and were evaluated for functional outcomes that included occlusion, maximal interincisal opening, and deviation of mouth and complications such as facial nerve pareses, postsurgical infection, and morbidity. Fifteen patients included in the study: 4 left sided and 11 right sided fractures. Nine patients had associated other mandibular fracture. Mean age of the patients was 28.2 years. Mean mouth opening at the end of 1 week, 6 weeks, and 6 months was 32.6, 37.8, and 40.5 mm, respectively. Transient facial nerve pareses were noted in one patient, and an extraoral draining sinus was noted in another. Endoscopic-assisted ORIF has a definite scope in management of condylar fractures. Results are more predictable with appropriate case selection due to a steep learning curve and intraoperative technical challenges. An initial experience in ORIF using extraoral approaches would greatly benefit a surgeon in utilizing this novel and alternate tool.
Mandibular condylar fractures account for 29 to 40% of all facial fractures. Though goals of management are common, treatment options differ, making this a topic of endless discussion. Management of condylar fractures is still subjective. Complications are not infrequent irrespective of the type of treatment or approach used.[1,2,3] Nonsurgical management is popular in many centers due to zero risk of facial nerve damage or scarring.[4] Though in any case, a fractured displaced condyle when managed nonsurgically mostly heals by malunion, various adaptations help achieve the treatment objectives grossly, if not precisely.[5] Factors such as surgeons’ choice, experience, rigid protocols, surgical skill, or a negative attitude in view of complications[6,7] do govern decision making in the management of condylar fractures.
A technique that combines the advantages of open reduction and internal fixation (ORIF) and avoids its associated complications is preferred. Endoscopic-assisted ORIF has emerged as an alternative, which provides both of these benefits. Since its application, endoscopic-assisted ORIF has been accepted as one of the mainstays in the management of condylar fractures.[8]
Materials and Methods
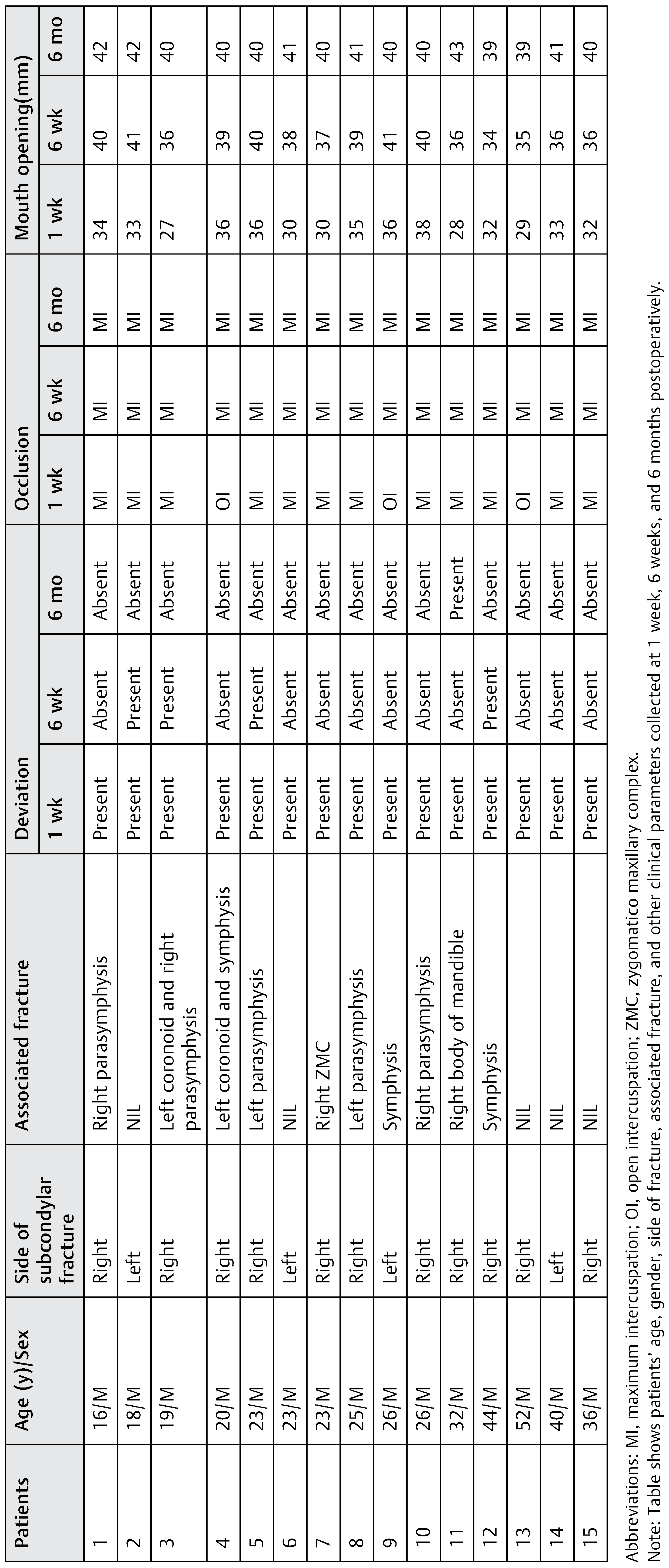
This study was performed at the department of oral and maxillofacial surgery, SDM Craniofacial Unit, Dharwad, India. Approval for the study was obtained from the ethics committee of the institute (SDMCDS/IRB 2014/OS/02) and all participants signed an “informed consent agreement.” A total of 178 patients with mandible fractures reported to us between January 2013 and January 2016. Sixty-seven of them had condylar fractures. Fifty-four of the 67 patients had unilateral fractures, while 13 had bilateral condylar fractures. Based on the anatomic location of fracture, out of the 54 unilateral condylar fractures, subcondylar fractures (Figure 1 and Figure 2) were noted in 24 individuals and intracapsular fractures were noted in 30 individuals.
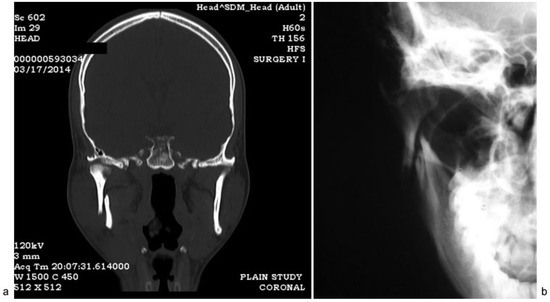
Figure 1.
(a) Coronal section through temporomandibular joint, (b) PA mandible shows laterally displaced condyle.
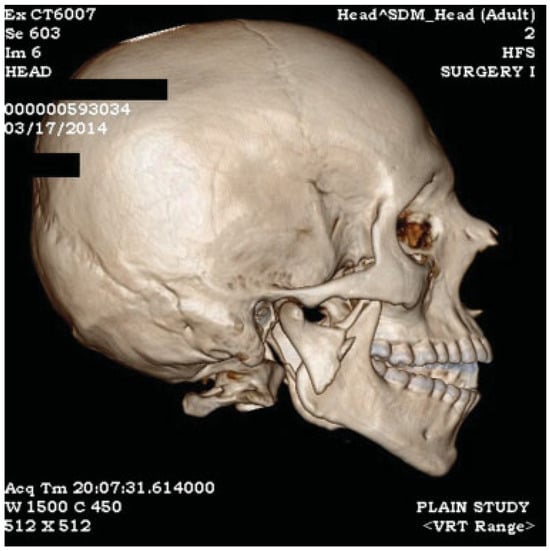
Figure 2.
3D reconstruction image showing laterally displaced condyle with shortening of posterior ramal height with premature occlusion of posterior teeth resulting in anterior open bite.
All patients with unilateral subcondylar fractures in whom ORIF was indicated were explained the necessity for surgery. Out of 24 patients, 20 agreed for surgical intervention and 4 did not. Furthermore, patients who opted for ORIF were given the choice of fixation: conventional extraoral Risdon’s approach versus endoscopic approach. A total of 15 patients opted for endoscopic ORIF approach and 5 patients opted for conventional ORIF approach (Figure 3).
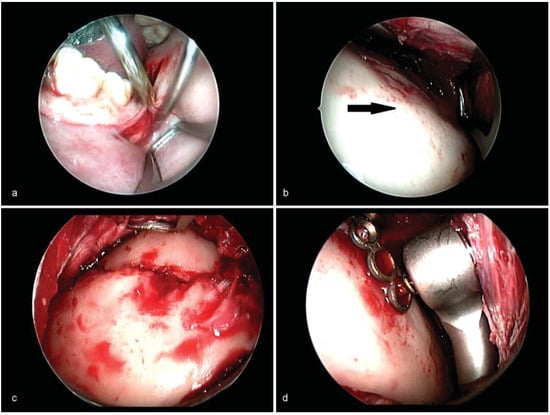
Figure 3.
(a) “S”-shaped curvilinear incision along the anterior border of ramus for transoral approach. (b) Optical cavity created in the subperiosteal plane over lateral surface of ramus. Arrow shows the lateral surface of the ramus. (c) Endoscopic visualization of reduced laterally displaced fracture. (d) Endoscopic visualization of placement of screws using right angled driver.
The mandible and temporomandibular joint (TMJ) were evaluated after 1 week, 6 weeks, and 6 monthspostoperatively for functional outcomes, side effects, and general patient satisfaction. Parameters for functional outcomes were based on occlusion, maximal incisal opening, and deviation on mouth opening. Parameters for side-effects included signs and symptoms related to facial nerve, scars, and sinus tracts. Thirty-five patients who either refused surgery or in whom surgery was not indicated were managed nonsurgically.
Endoscopic Equipment and Surgical Technique
Associated mandibular fractures were reduced and fixed first. To access the condyle-ramus unit intraorally, a standard incision was placed over the ascending ramus in all patients. Optical cavity was created using Howarth’s long raspatories and periosteal elevators. A 30-degree angle, 4-mm-diameter endoscope (Karl Storz, Tuttlingen, Germany) was introduced within the optical cavity and advanced superiorly toward the fracture. Reduction was achieved by forced gentle distraction of the mandible in a downward, forward, and superior direction. This created adequate space to accommodate the fractured fragment in the glenoid fossa and achieve reduction. Maxillomandibular fixation (MMF) was achieved using Erich’s arch bars. The endoscope was used for inspection of the posterior border and lateral ramus. In three patients, miniplate fixationwas donevia a transbuccal approach using a single stab incision in the preauricular region. Remaining 12 patients underwent a transoral procedure using a right angle screwdriver with plate holder. In all patients, fractured fragments were fixed using two standard 2.0 miniplates. The first plate was fixed along the posterior ramal border, while the second was fixed closer to the sigmoid notch. MMF was released after fixation. Occlusion and complete range of mandibular movements were confirmed.
Results
A total of 15 patients underwent endoscopic-assisted ORIF. All belonged to the group of unilateral condylar fractures. Out of 15 patients, 12 had subcondylar fractures and 3 had low condylar neck fractures. Four patients were left sided fractures and remaining 11 were right sided. Additional mandibular fractures were seen in nine patients (Table 1), while six patients had isolated condylar fractures. Transbuccal approach via a preauricular stab incision was used in 3 out of the 15 patients. Right angle screwdriver with plateholder was used in the remaining 12 patients. Three out of the 12 subcondylar fractures and 2 condylar neck fractures received single 2.0 AOASIF miniplates. Two 2.0 AO-ASIF miniplates were used to fix the remaining nine subcondylar fractures (Figure 4). Procedure was abandoned in one low condylar neck fracture, which was medially displaced. The patient had not consented for an extraoral incision prompting us to adopt a nonsurgical line of management by using elastic MMF.

Table 1.
Clinical details of the patients.
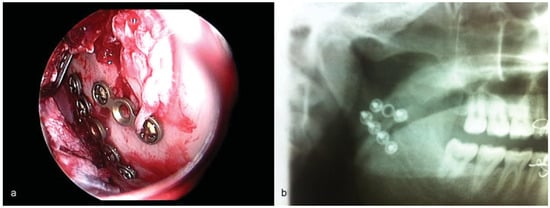
Figure 4.
(a) Endoscopic visualization of plates along the posterior aspect of lateral surface of subcondyle and another plate along the sigmoid notch. (b) Postoperative OPG shows the miniplate fixation.
Postoperative elastic MMF was used in all patients. Mean period of this MMF was 4.2 days. All patients were assessed for occlusion, maximum interincisal mouth opening, deviation during mouth opening, facial nerve weakness, scars, sinus tracts, and patient satisfaction. Postoperative Orthopantomograph and reverse Towne’s radiographs were used to confirm the fixation and condylar position in the glenoid fossa.
The mean age of patients was 28.2 years with a standard deviation (SD) of 10.71. The mean mouth opening at the end of first week postoperatively was 32.6 mm with a standard deviation of 3.29. At the end of 6 weeks, it increased to 37.8 mm with a SD of 2.29. At the 6-month follow-up, the mean mouth opening was 40.5 with a SD of 1.12 (Figure 5).
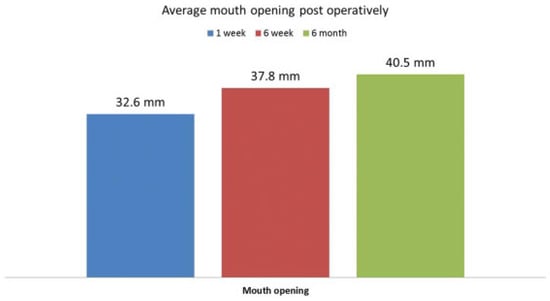
Figure 5.
Bar diagram shows progressive improvement in the average mouth opening.
Maximum intercuspation (MI) was observed in all patients except two who had occlusal interferences at the end of 1 week. Guiding elastics were continued in these two patients. Follow-ups of 6 weeks and 6 months showed MI in all patients. Deviation of jaw was assessed by residents as independent observers who were blinded about the side of surgery. Deviation of varying degrees was noted in all patients at the end of first postoperative week. At the end of 6 weeks, four patients continued to have mild deviation. One patient had deviation at the end of 6 months which was minimal compared with earlier. Facial nerve weakness was observed in one patient. One patient reported back with an extraoral draining sinus in the sixth month postoperatively. The sinus corresponded to the stab incision utilized for transbuccal fixation. The plate and screws were removed subsequently and the sinus tract excised. Generally, all patients were satisfied with the treatment at the end of 6 weeks (Figure 6).
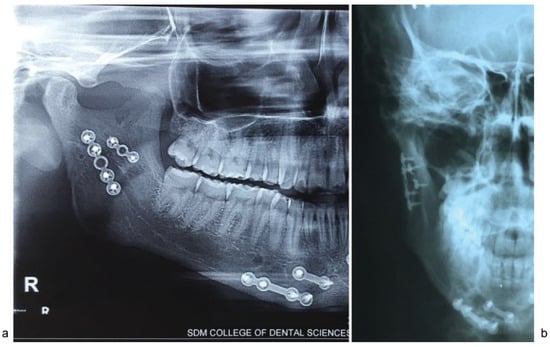
Figure 6.
(a) Two-year postoperative OPG showing restoration of posterior ramal height and healed fracture. (b) PA mandible shows restoration of mediolateral position of proximal segment.
Discussion
Open versus Nonsurgical versus Endoscope:
The Debate
In the past, decisions, philosophy, anecdotal experience, and retrospective case series with short follow-up governed actions determining management of condylar fractures.[9] This considerable debate that got tagged with condylar fractures resulted in a lack of consensus which made these fractures distinct. The management is also situation specific. There has been much satisfaction expressed by many surgeons with the results of closed treatment of subcondylar fractures. Proponents of nonsurgical management offer simplicity, reduced morbidity, prevention of facial scar, and facial nerve damage as benefits of closed treatment. You et al[10] have specifically enlisted the complications of nonsurgical management as follows: open-bite deformity, deviation during mouth opening, disc displacement, habitual luxation of the TMJ on the contralateral side, and malocclusion due to shortening of the ascending ramus. Mueller et al[11] has mentioned that the significant percentage of adults managed conservatively suffered from long-term aesthetic and functional problems. Benefits of ORIF include immediate function, restoration of mandibular vertical dimension, facial symmetry and projection, and improved jaw motion resulting from immediate anatomic restoration. Complications are facial scars, hemorrhage due to rupture of an internal maxillary artery, avascular necrosis of the proximal segment, and associated morbidity.[10] The single biggest concern remains facial nerve damage. The reported incidence of facial nerve damage with different extraoral approaches ranges from 0 to 24%, while long-term injuries range from 0% to just 4%.[12,13] Between temporary and permanent facial nerve pareses, temporary pareses is more.[2,13]
Choice of extraoral approach also affects the incidence of facial nerve paresis. Among the approaches, the mini-retromandibular approach and retromandibular approaches have been described as easy and quick with least risk of transient or permanent facial nerve damage.[12,14] The extraoral approach thus shows very high standard results with low morbidity. Though encouraging, this is still associated with some psychological burden, considering scar and varying periods of facial nerve pareses.
The transoral endoscopic-assisted condylar fixation has gained grounds due to the advantages offered, including direct visualization of a magnified and illuminated operative field for the surgeon and unobstructed views for the assistant and no extraoral scar.[15]
Boehle and colleagues mentioned that the most important benefit of the transoral approach is certainly the avoidance of any facial nerve injury.[12] We may not entirely agree with that since one of our patients did have a transient facial nerve pareses postoperatively. The optical cavity is entirely subperiosteal; hence, the risk of direct injury to the facial nerve is minimal. But again, the optical cavity by itself is a closed and restricted space and can offer resistance to manipulation in displaced fractures. The traction of tissues due to this can cause transient facial nerve pareses.
Endoscopic Approaches: Intraoral versus Extraoral
Approaches for introduction of the endoscope are transoral, transoral with transbuccal trochar-assisted fixation, and transoral with submandibular incision.
Troulis and Kaban[16] and Miloro[17] approached the condyle via the Risdon’s incision and used the endoscope to reduce and fix the condyle. The optic cavity created via transoral was smaller compared with an extraoral approach. The extraoral incision of 1.5 cm was placed higher toward the angle, which minimized risk to facial nerve. Aboelatta et al[18] comprehensively reviewed preferences of surgeons toward these approaches. These authors stated that most of the surgeons tend to use an external approach or a combined intraoral/external approach for endoscope-assisted ORIF. Though a transoral approach is ideal, Aboelatta and colleagues mentioned difficulties such as inappropriate reduction in up to 80% of their cases and difficulty in maintenance of the reduced segments which necessitates an additional submandibular incision. In our experience, we faced similar difficulties. A submandibular incision may be used to introduce the endoscope or allow for the introduction of an interosseus wires that facilitate both the reduction and its maintenance till the plate and screws are applied.[18]
Schön et al[19] have rationalized this debate by providing adequate indications for each. The authors stated that endoscope offers superior visibility extrapolating from limited incisions. Intraoral approaches are better suited for condylar fractures with lateral over-ride and undisplaced or minimally displaced fractures. Extraoral approach can be reserved for a severely comminuted or condylar fractures with medial override.[19] After 5 years of experience, Schön et al recommended using the transoral approach even for fractures with medial override.[4] González-Garcíaetal[20] concluded in their study that the intraoral approach constituted a valid alternative compared with a transcutaneous submandibular access. While Troulis has reported incidence of damage to marginal mandibular nerve as 4.5%[15] with an intraoral approach, the risk of damage to the marginal mandibular nerve is completely negated. Besides, the transoral approach is minimally invasive when compared with extraoral. In our series, one of our patients returned with a draining sinus in relation to the extraoral transbuccal port 6 months postoperative. The plates were retrieved intraorally using the angulated screw driver. We did not consider use of an additional submandibular incision in any of our patients. In our short experience, we believe that the true benefits of the endoscope can be realized to its fullest when used transorally.
Morbidity
When performed intraorally, dissection is restricted mostly to creation of a subperiosteal optic cavity. This minimal tissue dissection results in less edema and morbidity for the patient.[15,21] Reduced immediate postsurgical morbidity
allows early return to function. This was evident in our series. In the first week, all patients had varying degrees of deviation and malocclusion. The kinematic characteristics of free mandibular movements improved with subsequent regression of the edema. There was an improvement in deviation, range of motions, and occlusion. Haug et al[22] in their conclusion stated that “The endoscope-assisted approach currently takes longer than the traditional approach.” The longer operative time and costs for the initial outlay of equipment make the endoscopic approach more expensive than the traditional. Thus, according to Lee et al’s standards, the endoscopic approach currently used is more costly, takes longer to perform than traditional techniques, and offers no better frequency of patient morbidity. Haug et al in 2004 had stated that “for universal acceptance, surgery with the endoscope must be cost-effective, quicker than standard techniques, and decrease patient morbidity.”[22]
Displacement Direction of Condylar Fragment
Lo and Cheung[23] stated, “In cases of condylar fracture with medially dislocated condyle, an intraoral reduction is considered very difficult or virtually impossible.” We share a similar experience with all the medially displaced fractures when compared with laterally displaced fractures. Inexperience is an important factor, but this difficulty is in accordance with a more general observation.[10,11,23,24] Comparing medially displaced condylar fractures with lateral, Mueller in 2006 stated reasons for ease in the reduction of lateral override fractures, that is, better fragment visualization, manipulation, and hardware fixation. Reasons contributing to difficulty in a medially displaced fractures are “obscured access of lateral surface of condylar segment due to telescoped ascending ramus and subsequent difficulty in manipulation because of physical obstruction.”[11] In one of our patients who had a near 90-degree medially displaced condylar neck fracture, we found it extremely difficult to reduce the fragment. Enthusiasm notwithstanding, the procedure was abandoned after a long struggle and closed reduction was performed for the patient. For reduction of medial overrides, Mueller advocated first reducing them to the lateral override category and then stabilizing.
In sharp contrast, while You et al stated that subcondylar fractures with lateral override are easier to treat than those with medial override, they refute any relation between displacement direction and results. Therefore, the downward traction of the distal segment using a wire is a very important step. Hackenberg et al[24] reserved the endoscopic option for mildly displaced fractures and for the patient with multiple injuries who cannot tolerate closed reduction. In our experience, endoscopic repair was valuable in all the laterally displaced subcondylar fractures and low subcondylar fractures.
Angulated Drill versus Trocar
Trocar systems are used for placement of screws in the condylar fractures through a stab incision after fractures are reduced. The trocar system has potential to damage branches of facial nerve and blood vessels, infection, and sinus tract along the trocar wound and stab incision. Use of angled drills and screwdrivers eliminate these possible adverse events. Limitations of using angled drills and screwdrivers are manipulation of instruments within the closed optical cavity[4,25] and also good coordination between operating surgeon and other members of the team is needed. These limitations are transient and eliminated with intense training and practice.[26] When we started using the angulated screwdriver, we faced numerous problems in adapting to the system. This was largely related to the factors mentioned previously.
The Learning Curve
Knowledge or skills are learned in particular pattern based on its difficulty and repetition. Learning curve gives us the patterns in which particular skills are mastered. Use of endoscope in reduction and fixation of condylar fracture has steep learning curve which means that initial use of EAORIF technique is difficult, but with experience operating time is reduced and it is comparable to the conventional transparotid ORIF of condyle.[26,27]
Factors influencing the learning curves include the following:
- Skill of the surgeon to perform ORIF of condyle fracture.
- Skill to use the endoscopic instruments.
- Skill to use the right angle instruments or transbuccal system.
- Theater team coordination in setting up endoscopic unit and their coordinated use.
As mentioned earlier, it is the concept of team effort which will reduce the operating time and make the learning curve steeper.
Conclusion
In our nascent experience, we found the use of endoscope challenging but worthwhile at the same time. Technically, the endoscopic-assisted ORIF is complex and requires training. Prerequisites, which add as determinants to success, are a steep learning curve, patience, coordination of hand and eye, and coordination with the assistant. Difficulty increases with the level of fracture and the endoscope could be better used in subcondylar and low subcondylar fractures. The challenges we faced in this part of the world included the costof acquisition of equipment, related hardware, and maintenance. Increased operating time with the use of endoscope, more so during the initial days, adds to the financial burden either on the hospital or on the patient which again is a deterrent. Patients from a poor socioeconomic status and without financial support still cannot afford ORIF.
Though our experiences have not been unique when compared with other centers, it is noteworthy as it would suggest that new technologies can be successfully introduced into emerging health care systems. We intend to continue the study and also understand the biologic behavior, anatomic positional changes, and bite forces in our services.
Conflicts of Interest
None.
Financial Disclosure
The authors have no financial interest to declare in relation to the content of this article.
Declaration
Ethical approval was given by SDMCDS, reference number: SDMCDS/IRB 2014/OS/02. Written patient consent has been obtained to publish clinical photographs. All authors have viewed and agreed to the submission.
Acknowledgments
We thank Dr. Niranjan Kumar, medical director, SDM College of Medical Sciences and Hospital, and Dr. Srinath Thakur, principal of SDM College of Dental Sciences and Hospital for their constant support and encouragement and also Dr. Alexander Schramm for his surgical tips and advice.
References
- Ellis, E., III. Complications of mandibular condyle fractures. Int J Oral Maxillofac Surg 1998, 27, 255–257. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E., III; McFadden, D.; Simon, P.; Throckmorton, G. Surgical complications with open treatment of mandibular condylar process fractures. J Oral Maxillofac Surg 2000, 58, 950–958. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.H.; Choi, E.J.; Kim, H.W.; Kim, H.J.; Cha, I.H.; Nam, W. Complications in endoscopic-assisted open reduction and internal fixation of mandibular condyle fractures. Oral Surg Oral Med Oral Pathol Oral Radiol 2012, 113, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Schön, R.; Fakler, O.; Gellrich, N.C.; Schmelzeisen, R. Five-year experience with the transoral endoscopically assisted treatment of displaced condylar mandible fractures. Plast Reconstr Surg 2005, 116, 44–50. [Google Scholar] [CrossRef]
- Ellis, E.; Throckmorton, G.S. Treatment of mandibular condylar process fractures: biological considerations. J Oral Maxillofac Surg 2005, 63, 115–134. [Google Scholar] [CrossRef]
- Zide, M.F.; Kent, J.N. Indications for open reduction of mandibular condyle fractures. J Oral Maxillofac Surg 1983, 41, 89–98. [Google Scholar] [CrossRef]
- Eckelt, U.; Schneider, M.; Erasmus, F.; et al. Open versus closed treatment of fractures of the mandibular condylar process-a prospective randomized multi-centre study. J Craniomaxillofac Surg 2006, 34, 306–314. [Google Scholar] [CrossRef]
- Lee, C.H.; Lee, C.; Trabulsy, P.P.; Alexander, J.T.; Lee, K. A cadaveric and clinical evaluation of endoscopically assisted zygomatic fracture repair. Plast Reconstr Surg 1998, 101, 333–345, discussion 346. [Google Scholar] [CrossRef]
- Martin, M.; Lee, C. Endoscopic mandibular condyle fracture repair. Atlas Oral Maxillofac Surg Clin North Am 2003, 11, 169–178. [Google Scholar] [CrossRef]
- You, H.J.; Moon, K.C.; Yoon, E.S.; Lee, B.I.; Park, S.H. Clinical and radiological outcomes of transoral endoscope-assisted treatment of mandibular condylar fractures. Int J Oral Maxillofac Surg 2016, 45, 284–291. [Google Scholar] [CrossRef]
- Mueller, R.V.; Czerwinski, M.; Lee, C.; Kellman, R.M. Condylar fracture repair: use of the endoscope to advance traditional treatment philosophy. Facial Plast Surg Clin North Am 2006, 14, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Colletti, G.; Battista, V.M.; Allevi, F.; Giovanditto, F.; Rabbiosi, D.; Biglioli, F. Extraoral approach to mandibular condylar fractures: our experience with 100 cases. J Craniomaxillofac Surg 2014, 42, e186–e194. [Google Scholar] [CrossRef] [PubMed]
- Boehle, A.P.; Herrmann, E.; Ghanaati, S.; Ballon, A.; Landes, C.A. Transoral vs. extraoral approach in the treatment of condylar neck fractures. J Craniomaxillofac Surg 2015, 43, 224–231. [Google Scholar] [CrossRef]
- Kanno, T.; Sukegawa, S.; Tatsumi, H.; et al. Does a retromandibular transparotid approach for the open treatment of condylar fractures result in facial nerve injury? J Oral Maxillofac Surg 2016, 74, 2019–2032. [Google Scholar] [CrossRef]
- Troulis, M.J. Endoscopic open reduction and internal rigid fixation of subcondylar fractures. J Oral Maxillofac Surg 2004, 62, 1269–1271. [Google Scholar] [CrossRef] [PubMed]
- Troulis, M.J.; Kaban, L.B. Endoscopic approach to the ramus/condyle unit: clinical applications. J Oral Maxillofac Surg 2001, 59, 503–509. [Google Scholar] [CrossRef]
- Miloro, M. Endoscopic-assisted repair of subcondylar fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003, 96, 387–391. [Google Scholar] [CrossRef]
- Aboelatta, Y.A.; Elbarbary, A.S.; Abdelazeem, S.; Massoud, K.S.; Safe, I.I. Minimizing the submandibular incision in endoscopic subcondylar fracture repair. Craniomaxillofac Trauma Reconstr 2015, 8, 315–320. [Google Scholar] [CrossRef]
- Schön, R.; Gutwald, R.; Schramm, A.; Gellrich, N.C.; Schmelzeisen, R. Endoscopy-assisted open treatment of condylar fractures of the mandible: extraoral vs intraoral approach. Int J Oral Maxillofac Surg 2002, 31, 237–243. [Google Scholar] [CrossRef]
- González-García, R.; Sanromán, J.F.; Goizueta-Adame, C.; RodríguezCampo, F.J.; Cho-Lee, G.Y. Transoral endoscopic-assisted management of subcondylar fractures in 17 patients: an alternative to open reduction with rigid internal fixation and closed reduction with maxillomandibular fixation. Int J Oral Maxillofac Surg 2009, 38, 19–25. [Google Scholar] [CrossRef]
- Williams, W.B.; Abukawa, H.; Shuster, V.; Kaban, L.B.; Troulis, M.J. A comparison of postoperative edema after intraoral vs. endoscopic mandibular ramus osteotomy. J Oral Maxillofac Surg 2003, 61, 61–62. [Google Scholar] [CrossRef]
- Haug, R.H.; Brandt, M.T. Traditional versus endoscope-assisted open reduction with rigid internal fixation (ORIF) of adult mandibular condyle fractures: a review of the literature regarding current thoughts on management. J Oral Maxillofac Surg 2004, 62, 1272–1279. [Google Scholar] [CrossRef] [PubMed]
- Lo, J.; Cheung, L.K. Endoscopic-assisted rigid fixation of condylar fracture: a technical note. J Oral Maxillofac Surg 2006, 64, 1443–1446. [Google Scholar] [CrossRef]
- Hackenberg, B.; Lee, C.; Caterson, E.J. Management of subcondylar mandible fractures in the adult patient. J Craniofac Surg 2014, 25, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Veras, R.B.; Kriwalsky, M.S.; Eckert, A.W.; Schubert, J.; Maurer, P. Longterm outcomes after treatment of condylar fracture by intraoral access: a functional and radiologic assessment. J Oral Maxillofac Surg 2007, 65, 1470–1476. [Google Scholar] [CrossRef]
- Loukota, R.A. Endoscopically assisted reduction and fixation of condylar neck/base fractures–the learning curve. Br J Oral Maxillofac Surg 2006, 44, 480–481. [Google Scholar] [CrossRef]
- Foletti, J.M.; Bruneau, S.; Meningaud, J.P.; Berdah, S.V.; Guyot, L. Endoscopic treatment of mandibular condylar fractures in live minipigs: benefits of the operative learning curve. Br J Oral Maxillofac Surg 2013, 51, 630–633. [Google Scholar] [CrossRef]
© 2017 by the author. The Author(s) 2017.