Abstract
Obtaining postoperative images of maxillofacial fractures does not affect the clinical management of asymptomatic patients; however, few studies have evaluated the role of postoperative imaging in the context of orbital floor fractures. In this study, we evaluate current practice techniques and the role of postoperative imaging in the management of orbital floor fractures in isolation and with concomitant facial fractures. Retrospective review of patients who underwent open reduction and internal fixation of orbital floor fractures between 2005 and 2015 at a single medical institution. Operative and perioperative records were reviewed to characterize postoperative imaging as routine or as indicated by concerning clinical symptoms, and to correlate clinical outcomes to postoperative imaging patterns across all identified orbital floor fractures. A total of 139 patients underwent open reduction and internal fixation of orbital floor fractures. Of these, 75 (54%) had zygomaticomaxillary (ZMC) involvement. The remaining 64 (46%) were isolated orbital floor fractures. Overall, 54 (39%) patients underwent postoperative imaging. Of these, 38 (70%) had postoperative imaging in the absence of concerning clinical symptoms. There was no observed difference in complication rates in those who underwent postoperative imaging, and those who did not. Patients with orbital + ZMC fractures underwent a significantly higher number of postoperative imaging studies (p < 0.001); however, there was no observed difference in complications between isolated orbital and orbital + ZMC fractures. Routine post-operative imaging is not warranted in the absence of persistent clinical symptoms following open reduction and internal fixation of orbital floor fractures.
Postoperative imaging is routinely performed in the absence of clinical symptoms for maxillofacial fractures despite evidence that this practice does not affect the clinical management of asymptomatic patients [1,2,3,4,5,6,7]. Reports of postoperative imaging in the context of zygomatic fractures [3,6], mandibular fractures [4], and all maxillofacial fractures [1,2,5,7] have uniformly demonstrated that postoperative imaging unaccompanied by concerning clinical symptoms does not influence whether revision surgery is performed. To date, no studies have examined the clinical utility of postoperative imaging in the context of orbital floor fractures with or without zygomaticomaxillary (ZMC) complex involvement. A lack of high-quality studies, combined with the absence of standardized guidelines to direct the management of orbital floor fractures has led to highly varied practice patterns across institutions and providers [8,9,10]. This study sought to evaluate current practice techniques and the role of postoperative imaging in the management of orbital floor fractures. It is hypothesized that, as demonstrated for other maxillofacial fractures, postoperative imaging is not warranted in the absence of concerning clinical symptoms for orbital floor fractures.
Methods
After receiving Institutional Review Board approval (Pro00066190), records were reviewed for patients seen at a single medical institution from 2005 to 2015 who under-went operative management of orbital floor fractures. Patients who experienced involvement of the ZMC were also included in this study. Patients were excluded if they either experienced concurrent craniomaxillofacial trauma beyond orbital floor and ZMC involvement, or underwent nonoperative management.
Variables of interest included patient demographic data, mechanism of injury, days from initial presentation to fracture repair, surgical specialty of the attending provider, pre- and postoperative imaging data, operative and postoperative complications, and revision surgery rates within 30 days of the initial operation. Imaging studies included in the analysis were limited to those that involved the maxillofacial bones. No definitive clinical protocol exists at this institution for obtaining postoperative imaging following the repair of orbital floor fractures. Thus, to determine if postoperative imaging was routine versus symptomatically indicated, operative records were reviewed and the reasoning behind the request for postoperative imaging was assessed. Time from initial presentation to fracture repair was categorized as ≤2, >2 to ≤14, or >14 days, as per orbital fracture management guidelines that address indications for surgery prior to resolution of local edema [11]. All intra- and postoperative complications were compared across the presence and absence of postoperative imaging. Concerning postoperative complications included blurred vision, persistent diplopia, enophthalmos, eye pain, limited ocular motility, fever, and mental status change. In the absence of a defined institutional protocol, the decision whether to obtain postoperative imaging and/or revision surgery was made by the attending surgeon (Figure 1).
Statistical Analysis
Orbital floor fracture cases were separated into two pairs of cohorts based on fracture type (i.e., isolated orbital floor and ZMC involvement) and the presence and absence of post-operative imaging. Both cohorts were analyzed with respect to the following factors: patient demographics, mechanism of injury, time from presentation to operation, specialty of the attending surgeon, and number of preoperative images obtained. Continuous factors were analyzed between cohorts using logistic regression, and categorical factors using chi-squared analysis with Fisher’s exact test at α = 0.05.
Results
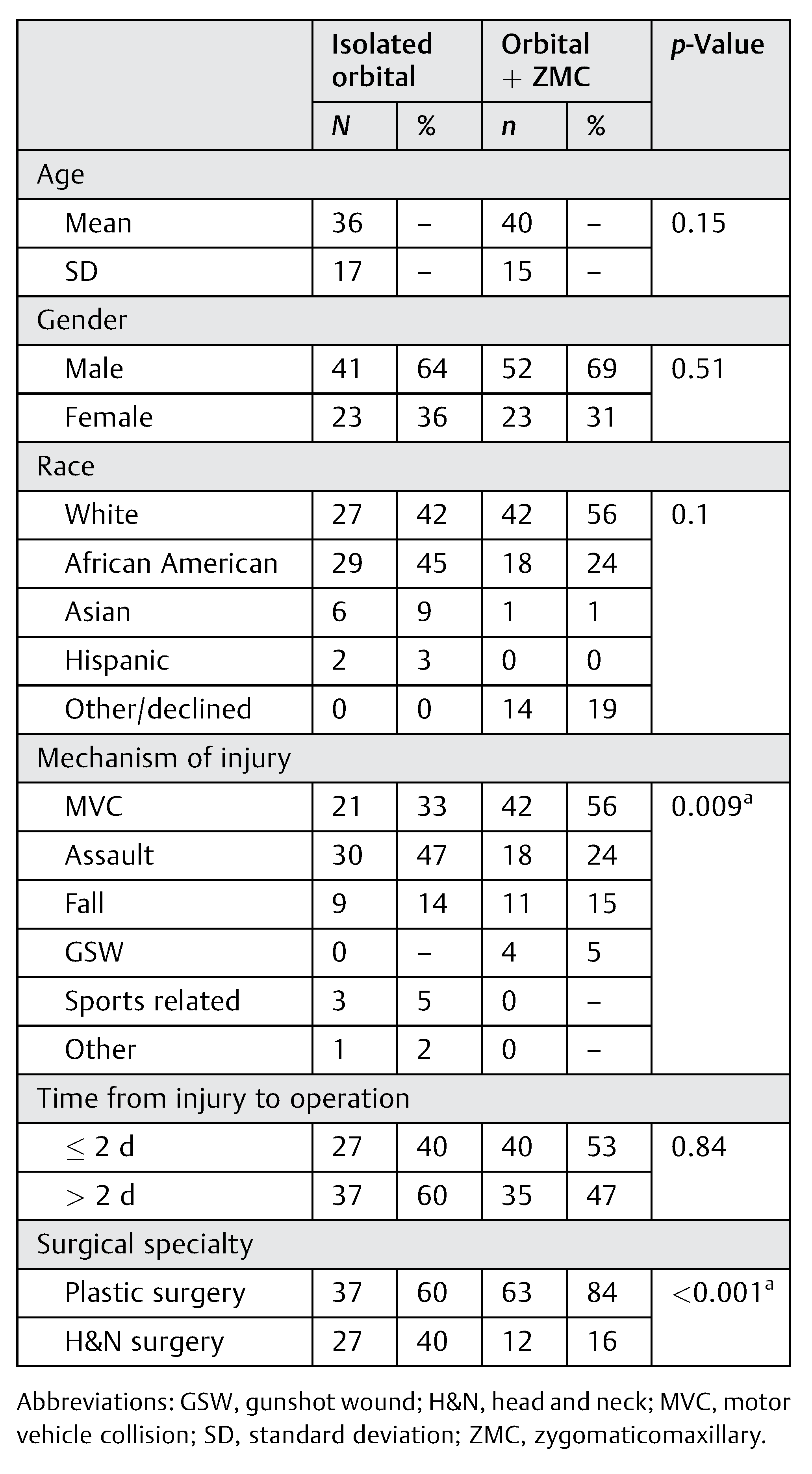
A total of 139 patients met inclusion criteria. Of these, 64 patients (46%) presented with isolated orbital floor fractures, and 75 patients (54%) presented with orbital floor fractures with ZMC involvement. Overall, patients were predominately male (67%), with a mean age of 38 years (range, 5–82). Racial demographics are shown in Table 1. On average, each patient underwent 1.8 (range, 1–3) preoperative imaging studies of the facial skeleton. The majority of cases with multiple pre-operative images of the facial skeleton consisted of facial computed tomography (CT) scans ordered in addition to an initial trauma work-up that included a head CT scan. Motor vehicle collision (MVC) and assault were the two most common mechanisms of injury, comprising 80% of all orbital floor fractures. Regarding the timing of surgical repair following the injury, 67 (48%) patients underwent surgical repair of their injury within 2 days of their initial presentation, 64 (46%) had surgery 3 to 14 days after presentation, and 8 (6%) received surgery more than 2 weeks after presentation.
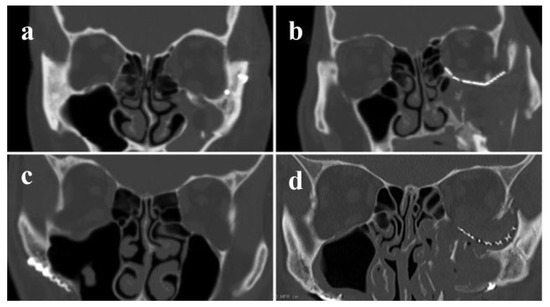
Figure 1.
Coronal views of postoperative computed tomography facial scans are shown for patients without (a,b) and with (c,d) postoperative complications.

Table 1.
Comparison of patient demographics in cases that did
and did not use postoperative imaging.
Table 1.
Comparison of patient demographics in cases that did
and did not use postoperative imaging.
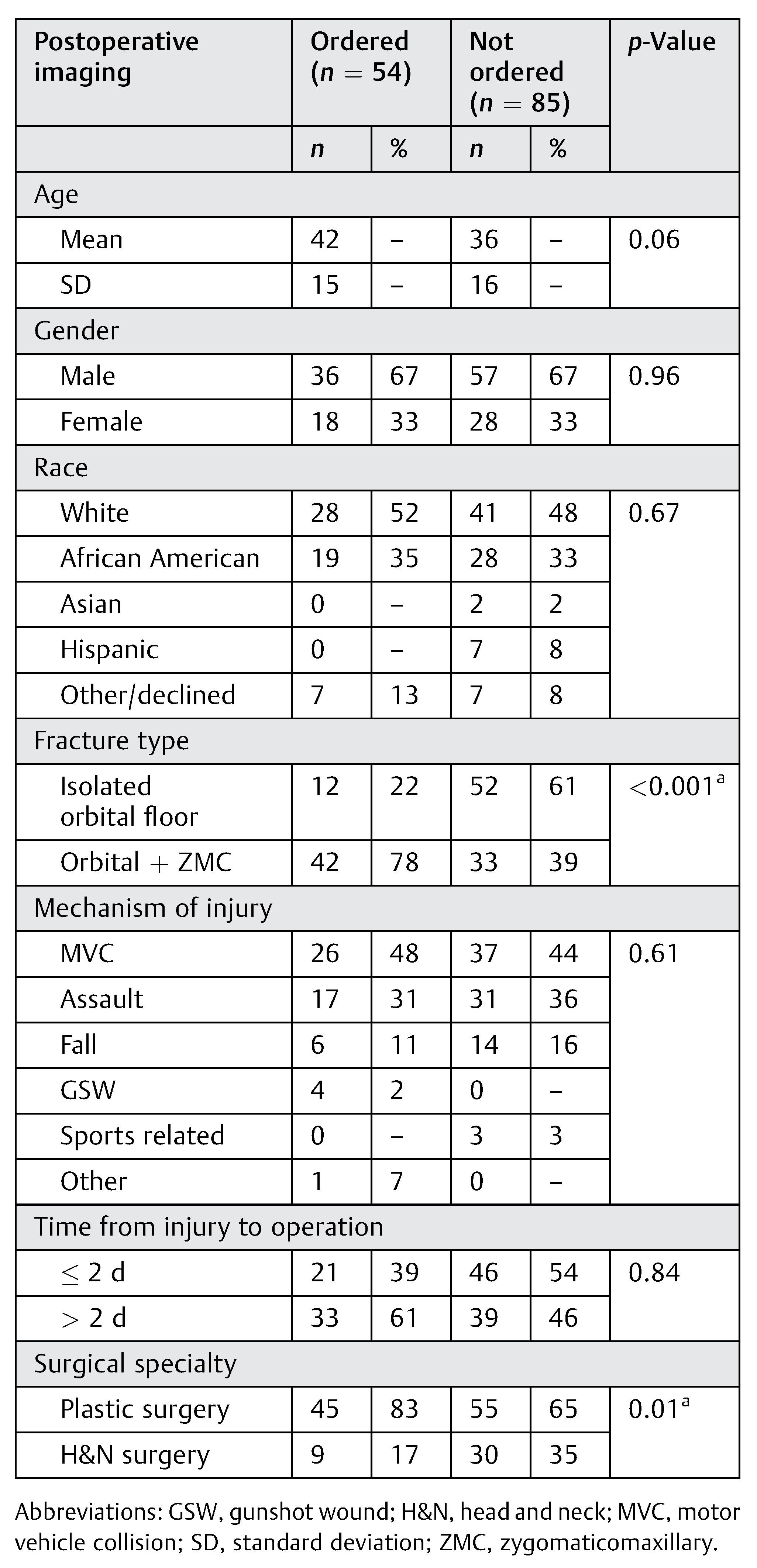 |
Postoperative imaging was ordered for 54 (39%) patients. The most common postoperative imaging study ordered was facial CT (n = 42), followed by brain CT (n = 15), skull X-ray (n = 7), magnetic resonance imaging (MRI) of the orbit (n = 1), and orthopantomogram imaging (n = 1). The single case of postoperative MRI orbital imaging was obtained to visualize the soft tissues of the orbital cavity in the context of limited ocular motility concerning for entrapment. Post-operative imaging was obtained secondary to concerning clinical symptoms in 16 of 54 (30%) cases. As shown in Table 2, concerning clinical symptoms included oculomotor dysfunction (n = 6), persistent edema (including enophthalmos; n = 3), altered mental status (n = 3), visual field deficits (n = 2), lagophthalmos (n = 2), persistent pain with ocular motion (n = 1), and malocclusion in the setting of ZMC involvement (n = 1). The remaining 38 (70%) cases that received postoperative imaging did so with no clear clinical indication. Two of these 38 (5%) cases revealed concerning findings in the absence of postoperative symptoms: one previously undetected left zygomatic arch fracture and one instance concerning for interval increase of intraorbital hematoma. Neither case resulted in a second surgery. The decision to obtain postoperative imaging was not significantly associated with age, gender, race, mechanism of injury, time from presentation to operative, or the number of preoperative imaging studies obtained (Table 1 and Table 3).

Table 2.
Reasons for obtaining postoperative imaging (n = 54).
Table 2.
Reasons for obtaining postoperative imaging (n = 54).
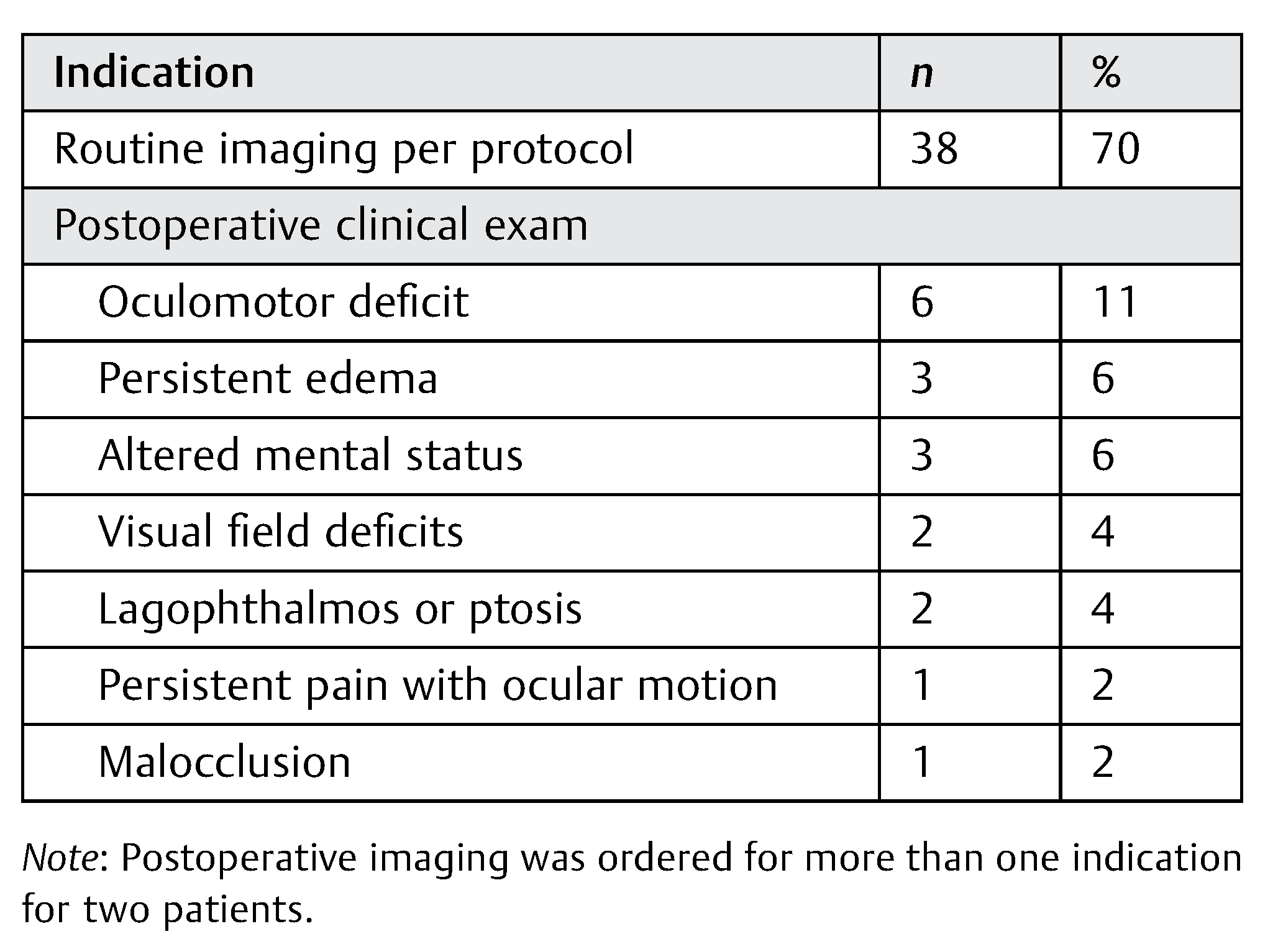 |

Table 3.
Comparison of imaging practices and outcomes in
cases that did and did not use postoperative imaging.
Table 3.
Comparison of imaging practices and outcomes in
cases that did and did not use postoperative imaging.
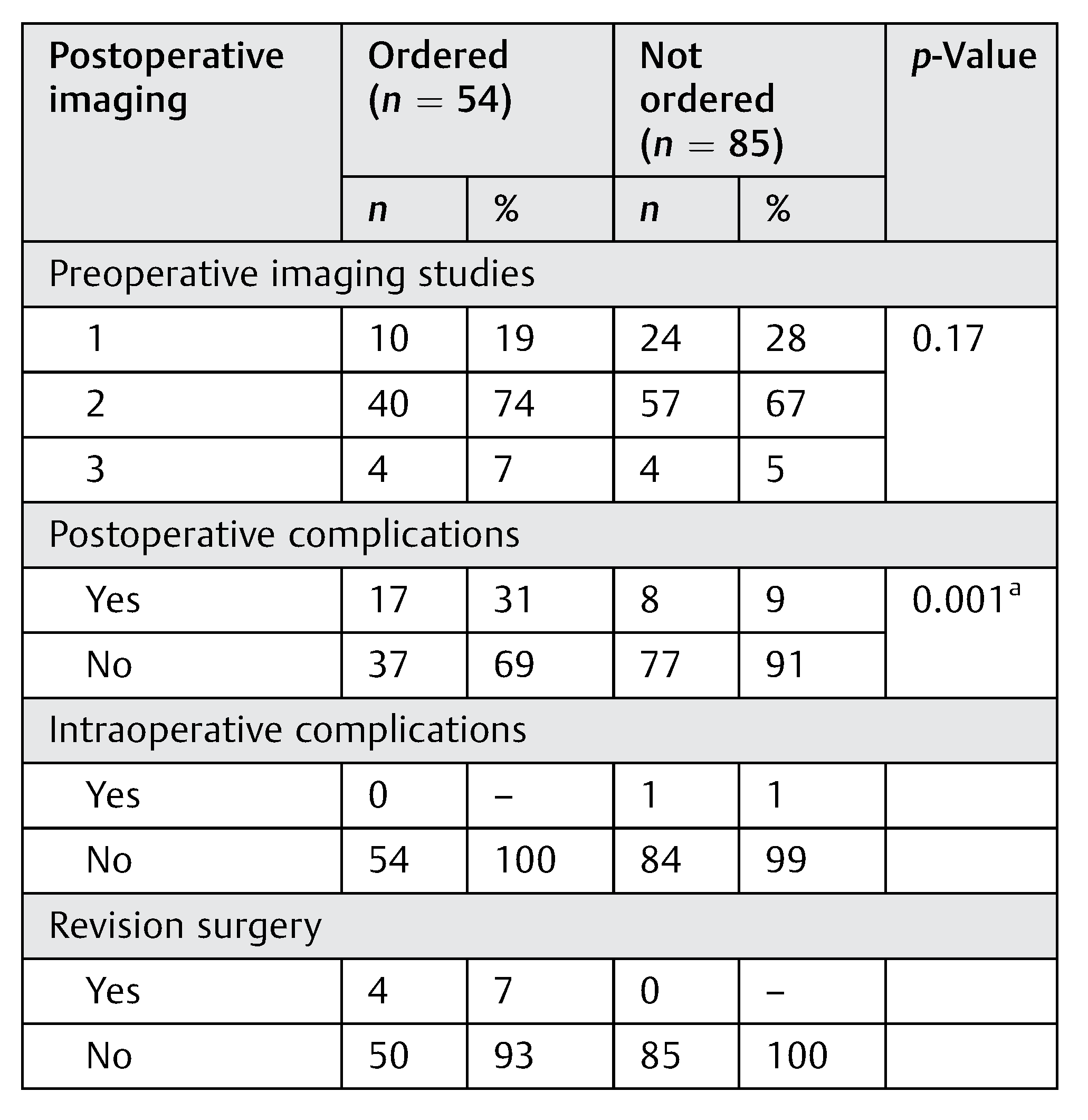 |
Out of 54 patients who underwent postoperative imaging, 4 (7%) patients underwent subsequent surgical revision within 30 days of the initial operation (Table 3). In the first case, postoperative enophthalmos and visual field deficits prompted CT imaging that revealed herniation of the inferior rectus muscle into theleft maxillary sinus. Open reduction was subsequently performed and the orbital floor was reconstructed using an iliac crest bone graft. In the second case, postoperative enophthalmos and lagophthalmos prompted CT imaging that revealed no entrapment but showed lateral displacement of the ZMC attributed to significant edema during the original operation. Revision open reduction and internal fixation of the orbital floor fracture and ZMC complex fracture were performed. The third case involved postoperative medial rectus dysfunction on clinical exam with subsequent CT imaging that showed impingement of the left medial and inferior rectus muscles by the medial flange of the orbital implant. Re-exploration of the orbital floor fracture with repositioning of the implant was performed, with postrevision positioning confirmed by a low-dose CT orbit scan. The fourth case involved postoperative ocular pain with severely limited ocular range of motion. A CT scan demonstrated transection of the inferior rectus muscle by the orbital plate, which was removed during a revision orbitotomy procedurethat included inferior rectus muscle repair.
Postoperative imaging was more commonly obtained for orbital floor fractures involving the ZMC than isolated fractures (p < 0.001) (Table 3). Despite the significantly higher number of postoperative imaging studies obtained for orbital + ZMC fractures (p < 0.001), there were no observed differences in postoperative complications or patient demographics between isolated orbital floor and orbital + ZMC fractures (Table 4 and Table 5). Isolated orbital floor fractures were more often secondary to assault, whereas ZMC involvement was more commonly associated with MVC (p = 0.009) (Table 4).
When examining differences in practice patterns by specialty, postoperative imaging was more frequently obtained by plastic surgeons, as compared with head and neck surgeons (p < 0.01). Plastic surgeons performed 100 orbital fracture repairs compared with 39 by head and neck surgeons. From plastic surgery, 20 (20%) cases developed post-operative complications. Of these, 13 (65%) had imaging obtained. Comparatively, head and neck surgeons noted postoperative complications in five (13%) cases, and three (60%) had postoperative imaging.
Of the 67 (48%) patients who underwent surgical repair within 2 days of their initial presentation, 10 of 67 (15%) experienced postoperative complications with 2 patients requiring revision surgery. Postoperative imaging was ordered in 21 of 67 (31%) patients. Comparatively, post-operative complications were present in 15 of 64 (23%) of patients who underwent surgical repair 3 to 14 days after presentation with 1 patient requiring revision surgery. Post-operative imaging was ordered in 30 of 64 (47%) patients. None of the eight patients who underwent surgery more than 14 days following initial presentation experienced postoperative complications or revision surgery. Postoperative imaging was ordered in three of eight (38%) patients.

Table 4.
Comparison of patient demographics across isolated
and complex orbital fractures.
Table 4.
Comparison of patient demographics across isolated
and complex orbital fractures.
 |
Discussion
Postoperative imaging of maxillofacial fractures has been shown to offer no additional benefits in the clinical management of asymptomatic patients. However, the clinical utility of postoperative imaging has never been evaluated in the context of orbital floor fractures. This study found that postoperative imaging does not affect the clinical management of asympto-matic patients following orbital floor fracture repair.
The study shows that postoperative imaging was most commonly ordered in the absence of concerning clinical symptoms such as oculomotor dysfunction or persistent edema. Furthermore, of those patients who underwent postoperative imaging, there were no subsequent surgical revisions or changes in clinical management as a result of the imaging obtained. The majority of patients who underwent orbital floor fracture repair were asymptomatic after surgery. By limiting postoperative imaging to patients who demonstrate concern-ing clinical symptoms, providers may help reduce patient costs, better allocate health care resources, and prevent unnecessary exposure to radiation [12]. In the context of symptomatic patients, the discretion of the surgeon should continue to guide the decision to pursue orbital fracture repair.

Table 5.
Comparison of imaging practices and outcomes across
isolated and complex orbital fractures.
Table 5.
Comparison of imaging practices and outcomes across
isolated and complex orbital fractures.
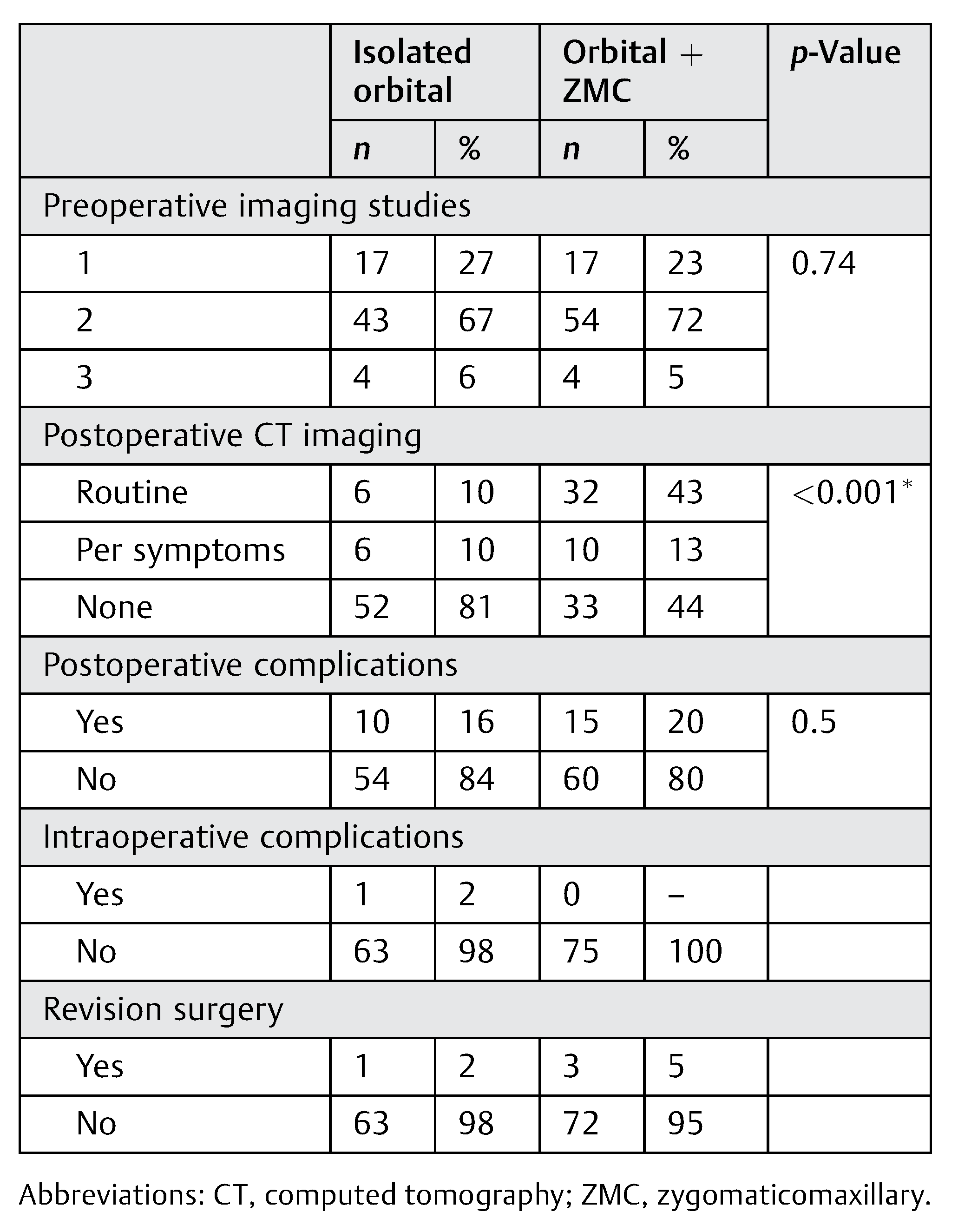 |
The potential overuse of postoperative imaging should also be addressed for orbital floor fractures with ZMC involvement, which represents the largest group of complex orbital fractures [13]. The larger proportion of postoperative imaging observed in the orbital + ZMC cohort may be explained by a greater concern to evaluate plate placement in complex orbital floor fractures. However, it should be noted that the increased incidence of postoperative imaging in the orbital + ZMC cohort did not correspond to an increase in complications or surgical revisions. Previous studies have shown that complex mandibular fractures with ZMC involvement demonstrate similar rates of postoperative complications to isolated mandibular fractures, and that the decision to pursue postoperative surgical revision is not influenced by postoperative imaging in the absence of clinical symptoms. Uniformly, these studies recommend against routine postoperative imaging in asymptomatic patients [2,3,4]. As isolated and complex orbital floor fractures have been shown to demonstrate similar outcomes, the findings of this study—and previous studies—suggest that in bothsettings, a restricted approach be takento postoperative imaging of the asymptomatic patient [2,3,4,7].
Current guidelines for the management of orbital floor fractures do not address postoperative imaging [14,15]. However, differences in the management (i.e., operative thresholds) of orbital floor fractures among surgical specialties have been addressed [16,17]. Plastic surgeons and head and neck surgeons have demonstrated similar diagnostic accuracy when assessing CT scans for maxillofacial trauma [18], further supporting the feasibility of standardizing postoperative imaging guidelines for orbital floor fractures across surgical specialties.
A review of intraoperative imaging practices demonstrated intraoperative revision reduction rates for orbital and ZMC fractures of 9 and 18%, respectively [19], with a recent report showing a 44% intraoperative revision rate for orbital fractures [20]. Reported intraoperative reduction rates are higher than the revision surgery rates in reports of post-operative imaging following facial fracture repair [1,2,3,4,5,6,7], which are consistent with the revision surgery rate of the current report (3%). Postoperative imaging findings in asymptomatic patients did not account for this discrepancy.
Preoperative imaging practices may representan additional area where unnecessary imaging can be mitigated, as multiple preoperative imaging studies of the maxillofacial bones including radiographs and MRI are likely redundant. When obtained without concurrent facial CTs, head CTs have a 90% sensitivity and 95% specificity when screening trauma patients for maxillofacial fractures [21], and are the preferred method of imaging for providers managing orbital floor fractures [10,22,23]. Head CTs and facial CTs are commonly obtained together per institutional trauma protocols that recommend whole-body CT (WBCT) imaging at specified trauma levels [24]. In meta-analysis, WBCT imaging reduced all-cause mortality (pooled odds ratio, 0.66) and duration of emergency room stay (mean difference, 28 minutes) as compared with selective CT imaging [25], however, whether WBCT was directly responsible for this difference in mortality remains debated. Predictive factors for the presence of maxillofacial fractures have been determined in the setting of WBCT for trauma [26]. Identifying predictive factors for orbital fracture types may prove similarly useful. Further studies of the significant associations of isolated orbital floor fractures to assault, and orbital + ZMC fractures to MVCs, may help maintain accurate pretest probabilities for orbital fracture types in the absence of multiple preoperative imaging studies of the maxillofacial bones.
Limitations
This study has limitations, many of which are inherent to its retrospective design. Providers who routinely order postoperative imaging might have done so in the presence of concerning clinical symptoms without denoting specific indications in the imaging orders. To limit this potential source of error, all perioperative records were reviewed to search for concerning symptoms noted elsewhere. Postoperative assessment of structural (e.g., enophthalmos) and direct visual (diplopia, blurred vision, etc.) can be subjective as a means to assess the anatomic correctness of orbital fracture repair. In addition, these data were obtained at a single institution where ophthalmic surgeons do not routinely manage orbital floor fractures, limiting the generalizability of these findings to such settings. This series spans a 10-year period and may be prone to evolving pattern sin patient selection and clinical practice not captured herein. Regarding the statistical analysis, this study is not adequately powered for stratification across patient cohorts, and institutional bias may be present. This analysis primarily showed where “positive” CT scans changed postoperative clinical management. The clinical utility of postoperative imaging may be understated because the degree to which “negative” CT scans might have prevented revision surgery cannot be retrospectively determined. Moreover, the educational benefits and clinical indications beyond orbital floor fractures that might influence a provider’s decision to obtain postoperative imaging were beyond the scope of this study.
Conclusion
Postoperative imaging is likely indicated in the presence of concerning clinical symptoms. In the absence of concerning postoperative symptoms, however, imaging alone does not appear to influence the postoperative clinical management of orbital floor fractures.
Note
We have no competing interests.
Disclosure
Research reported in this article was supported by the National Institutes of Health under Award Numbers 5T32 DC013018-03 and UL1TR001117. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Portions of this work were presented at the American Academy of Otolaryngology–Head and Neck Surgery Annual Meeting (September 18–21, 2016).
References
- Bali, N.; Lopes, V. An audit of the effectiveness of postoperative radiographs–do they make a difference? Br J Oral Maxillofac Surg 2004, 42, 331–334. [Google Scholar] [CrossRef] [PubMed]
- Chandramohan, J.; McLoughlin, P.M. Fractures of the mandible and zygomatic complex: Postoperative radiographs are not necessary. Br J Oral Maxillofac Surg 2007, 45, 90. [Google Scholar] [CrossRef]
- Crighton, L.A.; Koppel, D.A. The value of postoperative radiographs in the management of zygomatic fractures: Prospective study. Br J Oral Maxillofac Surg 2007, 45, 51–53. [Google Scholar] [CrossRef]
- Durham, J.A.; Paterson, A.W.; Pierse, D.; et al. Postoperative radiographs after open reduction and internal fixation of the mandible: Are they useful? Br J Oral Maxillofac Surg 2006, 44, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Jain, M.K.; Alexander, M. The need of postoperative radiographs in maxillofacial fractures–a prospective multicentric study. Br J Oral Maxillofac Surg 2009, 47, 525–529. [Google Scholar] [CrossRef]
- Ogden, G.R.; Cowpe, J.G.; Adi, M. Are post-operative radiographs necessary in the management of simple fractures of the zygomatic complex? Br J Oral Maxillofac Surg 1988, 26, 292–296. [Google Scholar] [CrossRef]
- van den Bergh, B.; Goey, Y.; Forouzanfar, T. Postoperative radio-graphs after maxillofacial trauma: Sense or nonsense? Int J Oral Maxillofac Surg 2011, 40, 1373–1376. [Google Scholar] [CrossRef]
- Aldekhayel, S.; Aljaaly, H.; Fouda-Neel, O.; Shararah, A.W.; Zaid, W.S.; Gilardino, M. Evolving trends in the management of orbital floor fractures. J Craniofac Surg 2014, 25, 258–261. [Google Scholar] [CrossRef] [PubMed]
- Sloan, B.H. Orbital floor blow-out fractures. Clin Experiment Ophthalmol 2004, 32, 3–4. [Google Scholar] [CrossRef]
- Christensen, B.J.; Zaid, W. Inaugural survey on practice patterns of orbital floor fractures for American Oral and Maxillofacial Surgeons. J Oral Maxillofac Surg 2016, 74, 105–122. [Google Scholar] [CrossRef]
- Jordan, D.R.; Allen, L.H.; White, J.; Harvey, J.; Pashby, R.; Esmaeli, B. Intervention within days for some orbital floor fractures: The white-eyed blowout. Ophthal Plast Reconstr Surg 1998, 14, 379–390. [Google Scholar] [PubMed]
- Council, N.R. Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2; National Academies Press: Washington, DC, USA, 2006; Volume 7. [Google Scholar]
- Hwang, K.; You, S.H.; Sohn, I.A. Analysis of orbital bone fractures: A 12-year studyof 391 patients. J Craniofac Surg 2009, 20, 1218–1223. [Google Scholar] [CrossRef] [PubMed]
- Gart, M.S.; Gosain, A.K. Evidence-based medicine: Orbital floor fractures. Plast Reconstr Surg 2014, 134, 1345–1355. [Google Scholar] [CrossRef] [PubMed]
- Burnstine, M.A. Clinical recommendations for repair of isolated orbital floor fractures: An evidence-based analysis. Ophthalmology 2002, 109, 1207–1210. [Google Scholar]
- Lelli, G.J., Jr.; Milite, J.; Maher, E. Orbital floor fractures: Evaluation, indications, approach, and pearls from an ophthalmologist’s perspective. Facial Plast Surg 2007, 23, 190–199. [Google Scholar]
- Anderson, O.A.; Lee, V.; Singh, R.; Ford, R.L.; Rose, G.E.; Thuau, H. Orbital fractures: Ophthalmic or maxillofacial? Br J Oral Maxillofac Surg 2007, 45, 90–91. [Google Scholar]
- Jarrahy, R.; Vo, V.; Goenjian, H.A.; et al. Diagnostic accuracy of maxillofacial trauma two-dimensional and three-dimensional computed tomographic scans: Comparison of oral surgeons, head and neck surgeons, plastic surgeons, and neuroradiologists. Plast Reconstr Surg 2011, 127, 2432–2440. [Google Scholar]
- van Hout, W.M.; Van Cann, E.M.; Muradin, M.S.; Frank, M.H.; Koole, R. Intraoperative imaging for the repair of zygomaticomaxillary complex fractures: A comprehensive review of the literature. J Craniomaxillofac Surg 2014, 42, 1918–1923. [Google Scholar]
- Borad, V.; Lacey, M.S.; Hamlar, D.D.; Dresner, H.S.; Yadava, G.K.; Schubert, W. Intraoperative imaging changes management in orbital fracture repair. J Oral Maxillofac Surg 2017, 75, 1932–1940. [Google Scholar] [CrossRef]
- Marinaro, J.; Crandall, C.S.; Doezema, D. Computed tomography of the head as a screening examination for facial fractures. Am J Emerg Med 2007, 25, 616–619. [Google Scholar]
- Exadaktylos, A.K.; Sclabas, G.M.; Smolka, K.; et al. The value of computed tomographic scanning in the diagnosis and management of orbital fractures associated with head trauma: A prospective, consecutive study at a level I trauma center. J Trauma 2005, 58, 336–341. [Google Scholar] [PubMed]
- Nguyen, P.N.; Sullivan, P. Advances in the management of orbital fractures. Clin Plast Surg 1992, 19, 87–98. [Google Scholar] [PubMed]
- Tillou, A.; Gupta, M.; Baraff, L.J.; et al. Is the use of pan-computed tomography for blunt trauma justified? A prospective evaluation. J Trauma 2009, 67, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Ma, Y.; Jiang, S.; et al. Comparison of whole-body computed tomography vs selective radiological imaging on outcomes in major trauma patients: A meta-analysis. Scand J Trauma Resusc Emerg Med 2014, 22, 54. [Google Scholar] [CrossRef]
- Whitesell, R.T.; Steenburg, S.D.; Shen, C.; Lin, H. Facial fracture in the setting of whole-body CT for trauma: Incidence and clinical predictors. AJR Am J Roentgenol 2015, 205, W4–W10. [Google Scholar]
© 2018 by the author. The Author(s) 2018.